Abstract
Health at Every Size® (HAES®) is a weight-neutral approach focused on promoting healthy behaviors in people with different body sizes. This study examined multiple physiological, attitudinal, nutritional, and behavioral effects of a newly developed, intensive, interdisciplinary HAES®-based intervention in obese women. This was a prospective, seven-month, randomized (2:1), controlled, mixed-method clinical trial. The intervention group (I-HAES®; n = 39) took part in an intensified HAES®-based intervention comprising a physical activity program, nutrition counseling sessions, and philosophical workshops. The control group (CTRL; n = 19) underwent a traditional HAES®-based intervention. Before and after the interventions, participants were assessed for physiological, psychological, and behavioral parameters (quantitative data) and took part in focus groups (qualitative data). Body weight, body mass index, and waist and hip circumferences did not significantly differ within or between groups (P > 0.05). I-HAES® showed increased peak oxygen uptake and improved performance in the timed-stand test (P = 0.004 and P = 0.004, between-group comparisons). No significant within- or between-group differences were observed for objectively measured physical activity levels, even though the majority of the I-HAES® participants indicated that they were engaged in or had plans to include physical activity in their routines. I-HAES® resulted in improvements in eating attitudes and practices. The I-HAES® group showed significantly improved all Body Attitude Questionnaire subscale and all Figure Rating Scale scores (P ≤ 0.05 for all parameters, within-group comparisons), whereas the CTRL group showed slight or no changes. Both groups had significant improvements in health-related quality of life parameters, although the I-HAES® group had superior gains in the “physical health,” “psychological health,” and “overall perception of quality of life and health” (P = 0.05, 0.03, and 0.02, respectively, between-group comparisons) domains. Finally, most of the quantitative improvements were explained by qualitative data. Our results show that this new intensified HAES®-based intervention improved participants’ eating attitudes and practices, perception of body image, physical capacity, and health-related quality of life despite the lack of changes in body weight and physical activity levels, showing that our novel approach was superior to a traditional HAES®-based program.
Introduction
The rising rates of obesity and the consequent health-related effects and healthcare costs have highlighted the need for approaches to assist people who are obese. The majority of obesity interventions focus on weight loss through a restrictive diet and physical activity programs. However, the negative effects provoked by interventions of this nature include binge eating and eating disorders, body dissatisfaction, low self-esteem, and culpability and stigmatization of the fat body [1,2,3]. Moreover, the success rate of weight-loss approaches regarding sustainable weight loss, reduction of body fat mass, maintenance of body fat-free mass, and other health benefits (e.g., clinical improvement in blood pressure, lipid profile, physical activity levels, disturbed eating behaviors, self-esteem, and body image) [4,5] is limited. In this context, weight-neutral approaches, such as the Health at Every Size® approach (HAES®), are of increasing interest [6] (Health at Every Size® and HAES® are registered trademarks of the Association for Size Diversity and Health—ASDAH).
HAES® aims to promote healthy behaviors in people with different body sizes, regardless of body weight changes. Overall, the approach encourages the development of a positive body image and the acceptance of different body shapes and sizes; the promotion of eating practices that respect individual nutritional needs and the sensations of hunger, satiety, appetite, and pleasure; the promotion of enjoyable and sustainable physical activities [7].
HAES®-based interventions have been shown to improve participant’s diet, eating patterns, eating behaviors, anthropometric and metabolic parameters, and psychological well-being [8–15]. However, HAES®-based interventions are traditionally characterized by group meetings and fixed discussion topics conducted by a limited number of professionals and do not effectively promote physical activity or assess it as an outcome. Moreover, qualitative evaluation is rarely performed, precluding more comprehensive conclusions regarding participants’ experiences and opinions [8,9,11–17].
In a pilot study, we showed that a 1-year HAES®-based intervention comprising an exercise program, nutrition counseling, and philosophical workshops led to improvements in body composition, body dissatisfaction, perception of body size, and symptoms of binge eating in addition to participants reporting behavioral and attitudinal changes towards eating and physical activity, as well as improved food choices [18,19]. However, the study had a quasi-experimental design, a small sample size, and did not evaluate cardiovascular risk factors. Given the clear potential of non-prescriptive interdisciplinary interventions for the management of obesity, this study aimed to use a mixed-method approach and a randomized controlled design to extensively investigate the effects of an intensive interdisciplinary HAES®-based intervention on multiple physiological, attitudinal, nutritional, and behavioral parameters in obese women. Our hypothesis was that the new HAES®-based intervention would promote greater improvements in overall health-related outcomes (including weight loss, despite the weight-neutral nature of the programs) in comparison to a traditional HAES®-based intervention.
Methods
Study design and participants
The rationale and design of this study have been fully described elsewhere [20]. In brief, this was a prospective, seven-month, randomized, controlled, mixed-methods clinical trial. The sample consisted of 58 women aged between 25 and 50 years with body mass indexes (BMIs) ranging between 30 and 39.9 kg/m2. The exclusion criteria included: a) diagnosis of diabetes mellitus, congestive heart failure, chronic renal disease, or hepatic steatosis; b) use of medications, such as appetite suppressants, thyroid hormones, diuretics or any other “anti-obesity” drug; c) currently engaged in nutritional counseling or in regular supervised physical activity programs elsewhere; e) currently pregnant or nursing. Participants were randomly allocated to the intensified HAES®-based intervention (I-HAES®) or the control (CTRL) groups in a 2:1 ratio using the Research Randomizer software.
The project was approved by the institutional Ethics Committee of the School of Public Health, University of Sao Paulo (protocol 1.738.855). The participants signed an informed consent and all procedures were in accordance with the Declaration of Helsinki as revised in 2008. This study is registered at clinicaltrials.gov (NCT02102061).
I-HAES®-based intervention
The I-HAES® group participated in a program comprising thrice-weekly physical activity sessions, bimonthly individual nutritional sessions, and five philosophical workshops over 7 months. All professionals involved in the intervention were trained in the HAES® concepts.
The physical activity program was supervised by professionals who had a bachelor degree in Physical Education. The sessions lasted for one hour and comprised different approaches aimed at increasing enjoyment and autonomy for engaging in daily physical activities (e.g., playing ludic games, dancing, engaging in different sports, exercising at participant’s preferred intensities). Improvements in physical capacity and weight loss were considered consequences of this process. As this is the first study to use the HAES® principles to design physical activity sessions, our theoretical foundation is fully presented in data in S1 File.
The nutritional intervention was based on nutritional counseling [21], with no prescription of diets. We aimed to promote healthy eating habits by stimulating participants’ sensitivity to hunger and satiety cues, emotional eating, triggers that could lead to automatic behaviors related to food, and methods to neutralize food (i.e., to not classify food as “good” or “bad”). To do so, we used the following strategies: maintaining a food diary, meal planning, and goal setting in accordance with the HAES® principles [20]. Before beginning the nutritional counseling, two 1-h lectures were held to present the nutritional approach and to address sociocultural aspects involving eating and concepts about healthy eating according to the Dietary Guidelines for the Brazilian Population [22]. Finally, participants received a book [23] that addressed the same principles encouraged by the nutritional intervention. The nutritional sessions lasted for 45 minutes and were conducted by dietitians, who had a bachelor degree in Nutrition. A full description of the nutritional intervention may be found elsewhere [18–20].
The philosophical workshops consisted of five 1-h meetings focused on discussion and reflection about topics related to obesity (e.g., concepts of desire and boredom [24], restriction and health [25,26], body and health moralization [27–29], freedom [24,30] and anxiety [31]. The philosophical workshops were conducted by a professional, who had a bachelor degree in Philosophy. The information regarding each component of this intervention is extensively described elsewhere [20].
CTRL group
The CTRL group attended bimonthly educational lectures, in accordance to the HAES® principles, on the same topics offered to the I-HAES® group (i.e., healthful eating, physical activity and philosophy, and encouraging the adoption of a healthy lifestyle). This “control” intervention was designed to mimic the most traditional HAES®-based interventions [8,9–17], as described elsewhere [20]. Table 1 presents the type and frequency of the activities performed by each group.
Table 1. Type and frequency of the activities performed by the intensified HAES®-based intervention group (I-HAES®) and the control group (CTRL).
| Activity | I-HAES® | CTRL |
|---|---|---|
| Supervised physical activity | 3 times-a-week | none |
| Individual nutritional sessions | 2 times per month | none |
| Philosophical workshops | 5 throughout the intervention | none |
| Lectures on physical activity | none | 1 |
| Lectures on healthy eating | 2 (pre-intervention) | 2 |
| Lectures on philosophy | none | 1 |
| Food diary register | Throughout the intervention | 2 (pre- and post-intervention) |
Quantitative data collection and statistical analysis
As previously described [20], prior to and after the intervention (i.e., pre and post), all participants were assessed for anthropometry measures (body weight, height, and hip and waist circumferences); aerobic condition (using a maximal graded exercise test); spontaneous physical activity levels (objectively measured using an ActiGraph GT3X® accelerometer [ActiGraph®, Pensacola, FL]); muscle function (using the timed-stands test [32] and timed-up-and-go test [33], where the lower the scores the better); psychological and behavioral assessments using validated questionnaires; namely, body perception and dissatisfaction (Figure Rating Scale [34,35]) attitudes towards the body (Body Attitude Questionnaire–BAQ–[36,37]) and health-related to quality of life (WHOQOL-BREF [38,39]). From the food diary data, we also calculated the frequency (considering total and daily intake) of intake of fruits, vegetables and ultra-processed foods, as a post-hoc analysis.
Mixed model analysis was performed for each dependent variable, with group (intervention and control groups) and time (pre and post) as fixed factors and subjects as a random factor. In the case of significant F-values, a post hoc test with Tukey’s adjustment was performed for multiple comparisons. For non-parametric data, independent and dependent samples were compared using Mann-Whitney U- and Wilcoxon tests, respectively. Percent delta changes were compared between groups [(post–pre from I-HAES®)–(post–pre from CTRL)] using unpaired Student’s t-tests. Participants’ baseline characteristics, and baseline characteristics between participants who retained and those who dropped out, were compared using Student’s t- or Chi-square tests. Finally, within-group Cohen’s d effect sizes (ES) were calculated [40]. All data analyses were performed using SAS 8.2 (SAS Institute Inc., Cary, NC, USA) or SPSS Statistics for Windows, version 17.0. The level of significance was set at P ≤ 0.05 and P values between 0.05 and 0.1 were considered to indicate a tendency towards significance. Quantitative data are presented as mean ± standard deviation or median ± interquartile range, estimated mean of differences between pre and post values, 95% confidence interval (CI), and % difference between delta change, except stated otherwise.
Qualitative data collection and analysis
As described previously [20], two focus groups convened to understand participant experiences, feelings, expectations, and opinions regarding the intervention and the interdisciplinary team, aspects related to their eating practices, and quality of life. The I-HAES® and CTRL groups attended separate focus groups. The initial focus groups, each composed of 7 to 10 participants, met one month after the beginning of the intervention and the final focus groups met in the last month of the intervention. Forty-eight and 14 participants in the I-HAES® and CTRL groups, respectively, joined the initial focus groups whereas 32 and 11, respectively, joined the final focus groups.
For qualitative data, an exploratory content analysis was conducted using an inductive approach which revealed themes and codes from the data. Themes were selected by two researchers using the “cutting and sorting” approach and subsequently organized in a structured codebook [41]. Both coders independently applied the codebook to the data set, using phrases as the unit of analysis. Kappa coefficients for inter-rater reliability were calculated using the GraphPad QuickCalcs online software. Themes were analyzed considering their core and peripheral aspects, with attention to their details and co-occurrence [41]. The results of the exploratory content analysis are presented for each group with a detailed description, direct quotes, and paraphrases [41]. Speeches from the I-HAES® group members are identified as “I” whereas those from the CTRL group are indicated as “C”.
Results
Participants
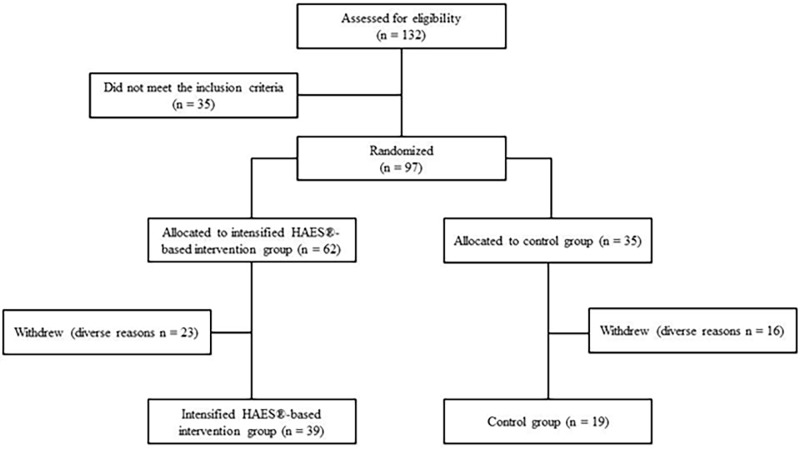
One hundred and thirty-two women were screened for participation. Ninety-seven met the inclusion criteria and were randomly assigned into either the I-HAES® (n = 62) or CTRL (n = 35) groups. Thirty-nine participants withdrew from the study for various reasons (one moved to another country, two because of distance issues, three became pregnant, six because of personal reasons, eight because of health reasons, and 19 were not available). Therefore, 58 subjects completed the trial and were included in the analysis (I-HAES®, n = 39; CTRL, n = 19; maintaining the 2:1 ratio). S1 Table presents the main baseline characteristics between participants who retained and those who dropped out, stratified by groups. The study flowchart is presented in Fig 1.
Fig 1. The “Health and Wellness in Obesity” study flowchart.
Table 2 shows participant demographic characteristics at baseline. No differences were observed between groups at baseline regarding age, weight, BMI, waist and hip circumferences, education, and family income (Table 2).
Table 2. General characteristics of women participating in a randomized controlled trial based on the Health at Every Size® approach.
| Intensified HAES®-based intervention group (n = 39) | Control group (n = 19) |
P | |
|---|---|---|---|
| Age (yr), mean, ± SD | 33.4 ± 6.7 | 37.1 ± 7.8 | 0.065 |
| Anthropometry | |||
| Body weight (kg), mean, ± SD | 90.7 ± 10.9 | 90.0 ± 10.5 | 0.912 |
| Body mass index (kg/m2), mean, ± SD | 34.5 ± 2.7 | 33.9 ± 3.1 | 0.552 |
| Waist circumference (cm), mean, ± SD | 108.6 ± 8.6 | 109.0 ± 10.2 | 0.248 |
| Hip circumference (cm), mean, ± SD | 119.4 ± 8.9 | 118.2 ± 7.0 | 0.431 |
| Relationship status, n (%) | |||
| Single | 21 (54) | 5 (26) | 0.177 |
| Married | 13 (33) | 10 (53) | |
| Common-law marriage | 2 (5) | 1 (5) | |
| Divorced | 3 (8) | 3 (16) | |
| Education, n (%) | |||
| Graduated from high school | 6 (15) | 1 (5) | 0.292 |
| Incomplete high school graduation | 0 (0) | 0 (0) | |
| Graduated from college | 18 (46) | 7 (37) | |
| Incomplete college graduation | 7 (18) | 2 (11) | |
| Postgraduate-level studies | 8 (21) | 9 (47) | |
| Monthly family income (value in Dollars), n (%) | |||
| ≤ 541.0 | 5 (13) | 1 (5) | 0.502 |
| 541.01–1,143.0 | 6 (15) | 1 (5) | |
| 1,143.01–2,705.0 | 17 (44) | 11 (58) | |
| 2,705.01–5,410.0 | 9 (23) | 6 (32) | |
| ≥ 5,410.01 | 1 (3) | 0 (0) | |
| Did not know | 1 (3) | 0 (0) |
Data are expressed as means ± SD, except when identified. No significant differences were found. (nonpaired t-test or chi-square test).
Qualitative data analysis
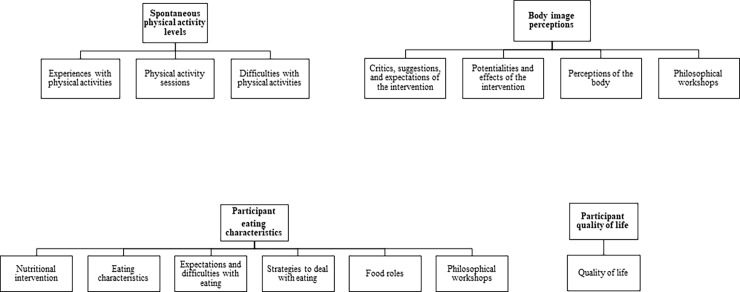
The thirteen emerging codes (Table 3) which resulted from participants’ statements revealed experiences that influenced their involvement with physical activity, eating-related aspects, body image, and quality of life. The kappa values showed a satisfactory strength of agreement between coders [42]. Codes that referred to similar topics were grouped and are shown in Fig 2. Notably, some of the resultant topics (spontaneous physical activity levels and participant eating, body image perceptions, and quality of life) were articulated by both quantitative and qualitative data, as presented in some of the following topics.
Table 3. Codes and kappa coefficients from focus groups with participants in the “Health and Wellness in Obesity” study.
| Code | Kappa |
|---|---|
| Potentialities and effects of the intervention | 0.854 |
| Critics, suggestions, and expectations of the intervention | 0.772 |
| Quality of life | 0.979 |
| Perceptions of the body | 0.662 |
| Nutritional intervention | 0.901 |
| Eating characteristics | 0.853 |
| Expectations and difficulties with eating | 0.738 |
| Strategies to deal with eating | 0.721 |
| Food roles | 0.652 |
| Experiences with physical activities | 0.608 |
| Physical activity sessions | 0.766 |
| Difficulties with physical activities | 0.978 |
| Philosophical workshops | 1.000 |
Kappa result is interpreted as follows: 0.61 to 0.80 as “good” agreement, and 0.81 to 1.00 as “very good” agreement [42].
Fig 2. Representation of the codes that composed some of the resultant topics.
Anthropometry
Body weight, BMI, waist and hip circumferences, and waist to hip ratio did not significantly differ within or between groups (Table 4). Eight out of 39 participants from the I-HAES® group and 1 out of 19 participants from the CTRL group achieved ≥ 5% weight loss, but this difference did not reach statistical significance (P = 0.246).
Table 4. Anthropometric, maximal aerobic capacity, muscle function, and physical activity assessments before and after the intervention.
| Intensified HAES®-based intervention group (n = 39) | Control group (n = 19) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Pre | Post | CI (95%) | ES | Pre | Post | CI (95%) | ES | % Difference between delta change | P value |
| Anthropometry | ||||||||||
| Body weight (kg) | 90.7 (10.9) | 90.1 (12.1) | -1.09 to 1.45 | -0.06 | 90.0 (10.5) | 91.0 (11.1) | -2.69 to 0.81 | 0.09 | -0.87 | 0.301 |
| Body mass index (kg/m2) | 34.5 (2.7) | 34.5 (3.2) | -0.42 to 0.56 | 0.01 | 33.9 (3.1) | 34.3 (3.3) | -1.04 to 0.32 | 0.12 | -0.83 | 0.309 |
| Waist circumference (cm) | 108.6 (8.6) | 106.8 (8.1) | -0.66 to 4.19 | -0.21 | 109.0 (10.2) | 107.8 (9.6) | -2.18 to 4.54 | -0.12 | 0.54 | 0.779 |
| Hip circumference (cm) | 119.4 (8.9) | 119.0 (8.3) | -2.96 to 1.42 | -0.04 | 118.2 (7.0) | 118.3 (8.6) | -3.14 to 2.94 | 0.01 | 0.08 | 0.722 |
| Waist to hip ratio | 0.9 (0.06) | 0.9 (0.06) | -0.006 to 0.031 | -0.19 | 0.9 (0.07) | 0.9 (0.08) | -0.017 to 0.034 | -0.13 | 0.53 | 0.788 |
| Maximal aerobic capacity | ||||||||||
| Time-to-VAT (sec) | 222.3 (70.1) | 226.3 (56.1) | -30.35 to 22.45 | 0.06 | 243.3 (107.4) | 203.4 (64.3) | 2.67 to 79.73 | -0.37 | 19.70ǒ | 0.058 |
| Time-to-RCP (sec) | 454.7 (90.5) | 502.6 (109.5)# | -86.96 to -9.10 | 0.53 | 463.3 (105.0) | 446.6 (101.9) | -38.55 to 74.05 | -0.16 | 15.02ǒ | 0.059 |
| Time-to-exhaustion (sec)* | 625.4 (124.4) | 671.4 (98.6) | -79.19 to -12.76 | 0.37 | 656.7 (91.4) | 678.7 (108.0) | -71.18 to 26.01 | 0.24 | 3.84 | 0.429 |
| VO2 VAT (mL/kg/min) | 11.9 (3.0) | 12.8 (2.7) | -1.82 to 0.02 | 0.30 | 12.2 (4.1) | 11.2 (2.1) | -0.18 to 2.51 | -0.26 | 17.83ǒ | 0.014 |
| VO2 RCP (mL/kg/min) | 18.4 (2.9) | 19.6 (3.6)# | -2.39 to -0.19 | 0.44 | 18.6 (3.6) | 17.3 (2.4)# | -0.29 to 2.89 | -0.34 | 14.65ǒ | 0.010 |
| VO2peak (mL/kg/min)* | 22.0 (3.8) | 24.0 (3.9)ø | -2.89 to -1.07 | 0.52 | 22.5 (3.7) | 22.2 (3.8) | -0.93 to 1.74 | -0.09 | 10.91ǒ | 0.005 |
| Muscle function tests | ||||||||||
| Timed Stands test (sec) | 19.6 (4.0) | 18.1 (4.3)# | 0.29 to 3.10 | -0.37 | 18.5 (4.4) | 20.3 (5.8) | -3.62 to 0.27 | 0.41 | 0.51ǒ | 0.007 |
| Timed-up-and-go test (sec)*ᶿ | 6.0 (0.8) | 6.4 (1.2) | -0.87 to 0.19 | 0.52 | 7.3 (3.4) | 8.1 (5.6) | 1.54 to -0.08 | 0.24 | -5.58 | 0.300 |
| Physical activity levels | ||||||||||
| Sedentary time (min/day) | 513.5 (88.1) | 501.1 (101.3) | -17.74 to 50.68 | -0.14 | 538.5 (102.0) | 517.0 (138.9) | -45.23 to 55.89 | -0.21 | 2.63 | 0.715 |
| Light PA time (min/day) | 325.0 (57.5) | 325.0 (71.8) | -24.18 to 28.19 | 0.00 | 328.2 (93.4) | 369.2 (92.8) | -74.82 to 2.46 | 0.44 | -8.34 | 0.106 |
| Total MVPA (min/day) | 39.3 (20.7) | 39.8 (20.7) | -6.97 to 5.71 | 0.02 | 37.3 (21.6) | 34.3 (23.5) | -7.53 to 11.22 | -0.14 | 5.11 | 0.662 |
Data are expressed as mean (SD), estimated mean of differences between pre and post values, 95% confidence interval (CI), Cohen’s d effect sizes (ES), and % delta differences [(post–pre from intervention)–(post–pre from control)]; expressed as mean ± SD). VAT, ventilatory anaerobic threshold; RCP, respiratory compensation point; VO, oxygen uptake; VO2peak, peak oxygen uptake; PA, physical activity; MVPA, moderate-to-vigorous physical activity.
P-values for group vs. time interaction.
ø Significant difference within group (P ≤ 0.05)
# Tendency for significance within group (P ≤ 0.10)
* Significant main effect of time (P ≤ 0.05)
ᶿ Significant main effect of group (P ≤ 0.05)
ǒ Significant difference between delta changes (P ≤ 0.05)
Aerobic conditioning
Table 4 shows data regarding aerobic capacity. There was a tendency towards an interaction effect in time-to-ventilatory anaerobic threshold (VAT) (P = 0.058) whereas delta analysis revealed a greater increase in time-to-VAT in the I-HAES® group compared to that in the CTRL group (P = 0.04). An interaction effect was observed in VO2 at VAT (P = 0.01), but post hoc analyses did not detect any significant differences. However, delta analysis showed greater increases in VO2 at VAT in the I-HAES® group compared to that in the CTRL group (P = 0.01).
A tendency towards an interaction effect was observed for time-to-respiratory compensation point (RCP) (P = 0.05), with post hoc analysis showing an increasing trend in the I-HAES® group (P = 0.07); delta analysis revealed greater increases in the I-HAES® group compared that in the CTRL group (P = 0.05). In addition, an interaction effect was observed for VO2 at RCP (P = 0.009), with the I-HAES® and CTRL groups increasing and decreasing tendencies, respectively (P = 0.09; P = 0.06), whereas delta analysis showed greater increases in the I-HAES® group compared to that in the CTRL group (P = 0.008).
A significant main effect of time was observed for the increase in time-to-exhaustion (P = 0.02), but no interaction effect was noted. Likewise, no significant differences were evidenced through delta analysis (P = 0.44). Finally, a main effect of time and an interaction effect were observed for VO2peak (P = 0.05 and 0.004, respectively), with the I-HAES® group (P = 0.0003), but not the CTRL group (P > 0.05), showing an increase in this parameter. Furthermore, delta analysis showed greater increases in VO2peak in the I-HAES® group compared to that in the CTRL group (P = 0.004).
Muscle function
An interaction effect was observed in the timed-stand test (P = 0.006), with the I-HAES® (P = 0.08), but not with the CTRL (P > 0.05) group showing an improving trend in this parameter. Similarly, delta analysis showed greater improvements in the timed-stand test in the I-HAES® group compared to that in the CTRL group (P = 0.004). Significant main effects of group and time were observed for the timed-up-and-go test (P = 0.04 and 0.01, respectively), but no interaction effect was noted. No significant differences were evidenced through the delta analysis (P = 0.29) (Table 4).
Physical activity levels
In the final focus groups, the majority of the participants in the I-HAES® group reported being engaged in some physical activity outside the intervention context or having plans to include novel activities in their routines, suggesting that they had gained a willingness and autonomy to practice physical activities. The participants in the CTRL group reported that the lectures on physical activities had stimulated them to become more attentive about how much they moved their bodies and were more aware of its importance. In the final focus group, ten CTRL participants reported having included physical activities in their routines. The participants that did not engage in any physical activity reported that they could not identify which activity they enjoyed and mentioned aspects of their routines that acted as barriers (e.g., unforeseen events in their routines, work demands, caring for their children).
Accelerometry data did not reveal any changes within or between groups in sedentary time, light physical activity levels, or time spent in moderate to vigorous physical activity after the intervention. Likewise, the delta differences showed no significant differences in these parameters (P > 0.05) (Table 4).
Participant eating characteristics
The I-HAES® group showed significant decreases in the total and daily consumption of ultra-processed foods, and significant increases in the total and daily consumption of fruits and vegetables. The CTRL group did not show any difference in total and daily intake of abovementioned food groups (Table 5).
Table 5. Dietary frequency intake of ultra-processed foods, fruits and vegetables of women participating in a randomized controlled trial based on the Health at Every Size® approach.
| Intensified HAES®-based intervention group (n = 39) |
Control group (n = 19) |
|||||
|---|---|---|---|---|---|---|
| Pre | Post | P | Pre | Post | P | |
| Ultra-processed foods (total consumption*), mean, ± SD | 32.0 ± 17.0 | 21.7 ± 13.4 | 0.0001 | 28.3 ± 14.5 | 26.5 ± 14.8 | 0.363 |
| Ultra-processed foods (daily consumption), mean, ± SD | 4.6 ± 2.4 | 3.1 ± 1.9 | 0.0001 | 4.2 ± 2.0 | 3.8 ± 2.1 | 0.133 |
| Fruits (total consumption), mean, ± SD | 8.8 ± 6.7 | 12.0 ± 8.9 | 0.026 | 8.6 ± 4.4 | 9.4 ± 5.8 | 0.291 |
| Fruits (daily consumption), mean, ± SD | 1.3 ± 1.0 | 1.7 ± 1.3 | 0.038 | 1.3 ± 0.8 | 1.4 ± 0.8 | 0.333 |
| Vegetables (total consumption), mean, ± SD | 13.9 ± 9.4 | 18.9 ± 12.6 | 0.018 | 13.7 ± 9.7 | 13.5 ± 7.8 | 0.753 |
| Vegetables (daily consumption), mean, ± SD | 2.0 ± 1.3 | 2.7 ± 1.8 | 0.012 | 2.0 ± 1.4 | 1.9 ± 1.1 | 0.572 |
* At pre-intervention, food diaries were completed 6.9 ± 0.3 days and 6.6 ± 0.7 days in the intensified HAES®-based intervention group and the control group, respectively. At post-intervention, food diaries were completed 6.9 ± 0.5 days and 6.9 ± 0.5 days in the intensified HAES®-based intervention group and the control group, respectively. Data was analyzed by the Wilcoxon test.
The qualitative data corroborate these findings. In the I-HAES® group, the initial eating difficulties were related to the eating structure, managing desires and emotional eating, eating in social situations, and knowing what and how much to eat. The participants had previously dealt with these issues by avoiding eating, replacing “high-calorie” foods with “low-calorie” foods, eating alone, and trusting other people to make their food choices. These participants completed food diaries throughout the intervention and reported that this tool led to the improvement of their eating perception and consciousness. This was particularly connected with improvements in sensitivity to hunger and satiety feelings, which allowed them to choose how much and what to eat. The participants were encouraged to increase their attentiveness while eating (i.e., eating without distractions, spending more time at the table, and evaluating what they felt like eating), resulting in changes in their food consumption: “I’ve learned that after I stopped eating in front of the television I stopped nibbling” (I10). Participants reported that they were able to identify when they relied on food to deal with feelings and emotions and were able to manage this situation differently. This gave them a sense of empowerment and responsibility for their own eating behaviors. The philosophical workshops were also reported to contribute to this change. In addition, members of the I-HAES® group reported having a more diversified eating habit, increasing their consumption of in natura or minimally processed foods. Finally, they reported having acquired autonomy to plan their eating: they were able to anticipate and think about their eating, plan their grocery list, and organize their schedule to cook. Regarding cooking, they were stimulated to engage more often in this activity and to diversify the ingredients and spices they used, which resulted in a higher willingness and interest to eat fresh and home-made foods.
In the CTRL group, the initial eating difficulties were related to emotional eating, which they dealt with by avoiding eating or eating alone. The participants received lectures about healthful eating and completed food diaries at the beginning and after the intervention respectively. The participants reported benefits from these diaries: they were able to notice patterns in their eating habits (e.g., by evaluating the reasons why they ate, how they ate, how they felt while eating, identifying when they ate in response to emotions, and gauging their hunger and satiety) and were working to change them. The lectures on healthy eating were reported to be clarifying, helping them to reconsider what they understood as healthy food, to value the importance of planning their eating, and to be more attentive about the quantity and the quality of their eating. Nonetheless, according to their statements, the CTRL group was unable to make concrete changes in their eating habits.
Body image perceptions
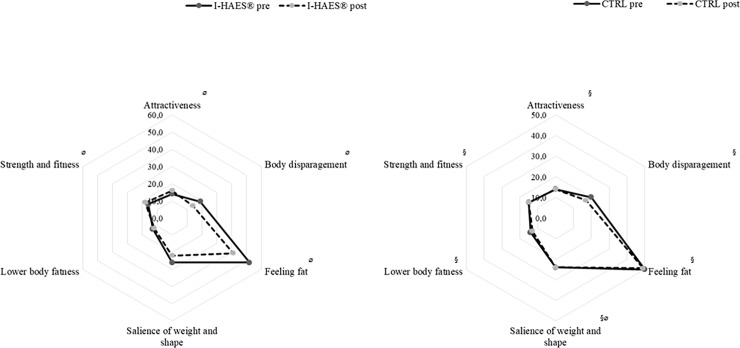
Regarding participants’ attitudes toward their bodies, significant within-group differences were observed for all BAQ subscales post-intervention in the I-HAES® group (P ≤ 0.05) (Fig 3). Compared to those in the CTRL group, the I-HAES® group had significant decreases in the “body disparagement” (P = 0.01) and “feeling fat” (P = 0.01) subscale scores and a significant increase in the “attractiveness” (P = 0.01) and “strength and fitness” (P = 0.001) subscale scores post-intervention. In contrast, the CTRL group showed a decrease only in the “salience of weight and shape” subscale score (P = 0.03). In relation to participants’ body perception and dissatisfaction, the I-HAES® group showed significant within-group differences for all Figure Rating Scale scores (P ≤ 0.05). The I-HAES® group also showed improvements in the “current body size” and “current body size–ideal body size” scores when compared those in the CTRL group post-intervention (P = 0.02 for both parameters). In the “current body size” subscale, the I-HAES® initial and final scores were 5.0 ± 3.0 and 2.0 ± 2.0, respectively (P = 0.001). The initial and final scores in the CTRL group were 3.0 ± 2.0 and 4.0 ± 5.0, respectively (P = 0.098). For “current body size–ideal body size”, the initial and final scores in the I-HAES® group 3.0 ± 1.0 and 2.0 ± 2.0, respectively (P = 0.001) and 3.0 ± 2.0 and 3.0 ± 2.0, respectively in the CTRL group (P = 0.12).
Fig 3.
(Left panel): Results from the intensified HAES®-based intervention group Body Attitude Questionnaire pre- and post-intervention. (Right panel): Results from the control group Body Attitude Questionnaire pre- and post-intervention. I-HAES®, intensified HAES®-based intervention group; CTRL, control group. § Significant difference when compared to the intensified HAES®-based intervention group post-intervention (P ≤ 0.05). ø Significant difference within group (P ≤ 0.05).
The focus groups corroborated these quantitative changes. In the baseline focus group, both groups shared similar perceptions. While some participants reported having positive attitudes toward their bodies, valuing it as part of their personality, others did not: “Losing weight is very important to me: I usually don’t look at myself in the mirror, and when I do I don’t recognize myself” (I5), and “I’d like to lose weight, it disturbs me: I stopped doing things, my social life changed” (C47). Other participants shared a preoccupation with their health and willingness to perform activities or a desire to change certain characteristic of their bodies. In the final focus group, members of the I-HAES® group said that they felt empowered by the activities, highlighting broader gains than nutrition, physical activity, and philosophy (“The intervention changed my life, my conceptions. If I were to define the intervention as my life today, I would define it as life, death and rebirth: I lived, gained weight, died and the intervention rebirth me”–I21). While four participants said that they still did not accept being fat, others said that although they expected to lose more weight, they were happy with their gains (e.g., more willingness, pain relief, etc.), and understood that body change would be a long-term process. Also, their weight was no longer a condition for their happiness (“I used to see myself happy only after [losing weight]. I still want to lose weight, but I’m already happy now”–I16). According to them, their previous focus on weight loss per se was a source of emotional distress that prevented them from keeping healthy habits as they were only sustained during weight loss. The philosophical workshop discussions were reported to have influenced these changes. These quantitative results suggest that, despite not having a significant weight loss, our participants developed a better body image and were more comfortable and less dissatisfied with their current physical condition. Those in the CTRL group stressed that the lectures had an effect on their concepts, making them reflect on the information that was communicated: they started to think and felt more responsible for their body condition and reported feeling more comfortable about it. Despite that, these participants mentioned discontentment: “I have trouble when I’m getting dressed, I want to die because nothing fits me, everything looks hideous” (C47).
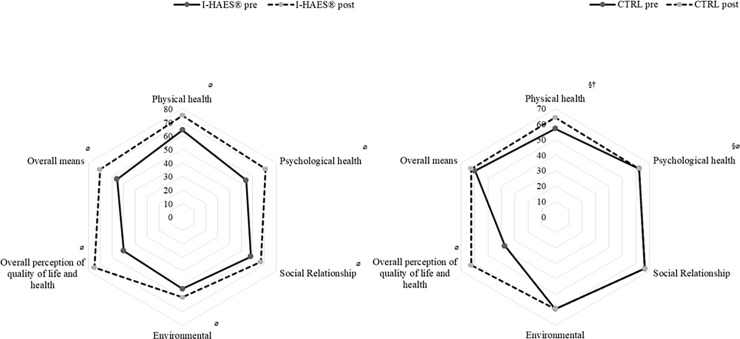
Participant quality of life
In the I-HAES® group, significant within-group differences were observed for all WHOQOL-BREF domains after the intervention (P ≤ 0.05) (Fig 4). Compared to those in the CTRL group, the I-HAES® group showed significant improvements in the “physical health” (P = 0.05), “psychological health” (P = 0.02), and “overall perception of quality of life and health” (P = 0.03) domains. The CTRL group showed improvements only in the “psychological health” (P = 0.04) and “overall perception of quality of life and health” (P = 0.01) domains.
Fig 4.
(Left panel): Results from the intensified HAES®-based intervention group WHOQOL-BREF questionnaire pre- and post-intervention. (Right panel): Results from the control group WHOQOL-BREF questionnaire pre and post intervention. I-HAES®, intensified HAES®-based intervention group; CTRL, control group. § Significant difference when compared to intensified HAES®-based intervention group post-intervention (P ≤ 0.05). ø Significant difference within group post-intervention (P ≤ 0.05). † Significant difference when compared to intensified HAES®-based intervention group pre-intervention (P ≤ 0.05).
The focus groups shed light on the quantitative changes. Initially, in the I-HAES® group, the quality of life was defined as a set of conditions that were not part of the participants’ routine and was related to expectations about their eating, physical activity, physical appearance, and well-being. In the final focus group, the intervention itself was part of the quality of life in the I-HAES® group (“quality of live is to come here and have fun doing the activities”–I14). They reported having included aspects they considered important to their quality of life that were previously only hypothetical: “I said before that quality of life would be to sleep better, eat well, have leisure time. Now I’m trying to sleep better, I’m hanging out more” (I35). The CTRL group reported in both focus groups a general definition of quality of life and did not seem to have incorporated the aspects discussed in the intervention to improve their quality of life or to change their routines to approximate to what they considered to be quality of life.
Discussion
The main finding of this study was that a new intensive, interdisciplinary HAES®-based, non-prescriptive intervention in obese women improved eating attitudes and practices, perception of body image, physical capacity, and health-related quality of life. Moreover, qualitative and quantitative data suggest that this novel intervention was more effective than a traditional HAES®-based one.
Throughout the seven-month follow-up period, both the I-HAES® and CTRL groups showed no change (or slight reductions in the case of waist circumference) in anthropometric measurements. This find might be explained because the current physical activity program, tailored to meet the HAES® principles, was not focused on exercise intensity or even on the adherence to the supervised exercise session; rather, the program was focused on promoting one’s self-engagement in playful, enjoyable activities, which may have been not sufficient to elicit detectable changes in anthropometric variables in such a follow-up period. However, this study was limited by the fact that body composition was not assessed, therefore we cannot rule out the possibility that participants did increase lean mass while decreasing body fat, without affecting body weight or other anthropometric parameters. In contrast, our I-HAES® intervention improved aerobic conditioning and muscle function whereas no changes were observed in the CTRL group. Importantly, poor aerobic conditioning and function are associated with premature mortality in various populations [43,44]. In this context, Ross and Janiszewski [45] argue that anchoring the practice of exercise with weight reduction can mask opportunities to stimulate people to become more physically active [45]. Indeed, our data corroborate previous studies showing that regardless of body weight change, physical activity is associated with increased physical capacity [45–48], reinforcing the protective cardiometabolic effect of physical activity.
Participants in the I-HAES® group were able to overcome their initial eating difficulties, reporting that they were able to better manage their emotional eating, eat in accordance with feelings of hunger and satiety, eat attentively, and improve the quality of food consumed. These gains are in accordance to those reported by previous traditional HAES®-based interventions [8,49,50]. In this study, we also showed that an intensive HAES®-based intervention led to improvements in participants’ autonomy to plan their eating and increased engagement with cooking, which might be important for maintenance of the habits acquired during the intervention. Notably, the CTRL group reported being stimulated to think about their eating, which did not provide them with autonomy to deal with their eating or result in sustainable changes. While traditional HAES®-based interventions have been shown in quantitative assessments to stimulate eating changes [9,12], no studies have qualitatively explored the participants’ likelihood to maintain these changes.
Our findings revealed that members of the I-HAES® group developed a better perception of their bodies and were more comfortable and less dissatisfied with their current physical condition. Importantly, these changes were independent of any change in anthropometric measurements. In contrast, the CTRL group showed small or no changes in these perceptions. Altogether, these results suggest that the positive effects on participants’ body image observed in traditional HAES®-based interventions [16,17] were expanded by this novel intensive and interdisciplinary HAES®-based intervention, which may have provided an atmosphere of mutual empathy, encouraged self-worthiness, and promoted positive changes in participants’ body attitudes, perception, and dissatisfaction.
This intervention also improved the health-related quality of life, which might be a result of the abovementioned improvements. To our knowledge, this is the first intervention to use qualitative data to explore aspects of quality of life in a HAES®-based intervention. Brown et al. [51] explored obese patients’ experiences and perceptions of support in primary care and found that stigma-related thoughts were detrimental to participant quality of life and negatively affected interactions with health services. Our intervention was seemingly able to tackle numerous issues in a supportive way, helping to create a positive and welcoming environment for the participants and positively affecting their interactions with the intervention. The discussions promoted by the philosophical workshops were important for the promotion of reflection among our participants. These workshops are innovative in a HAES®-based intervention and should be considered in further studies. It is important to note that the CTRL group also showed improved “overall perception of quality of life and health”, suggesting that even small efforts regarding changes in health habits might improve the quality of life in this population.
Despite the aforementioned improvements, the accelerometry data did not show increases in physical activity levels in the I-HAES® group. This was observed even though the participants reported having fun during physical activity classes and feeling empowered once they realized they could move their bodies in a number of ways; in addition, most reported engagement in some physical activity outside the intervention context or having plans to include novel activities in their routines. A possible explanation for this outcome is that structured exercise contributes only a minor daily physical activity energy expenditure, suggesting that exercise acts as a supplement to spontaneous physical activities [52]. Corroborating this notion, Turner et al. [53] provided healthy participants with significant amounts of prescribed exercise (almost 4 hours of exercise per week at 65% of their VO2max), which represented only 15% of the physical activity energy expenditure after 18 weeks of the intervention. Furthermore, there is data indicating that the adoption of structured exercise training may induce compensatory changes in behavior or physiology that could lead to decreased energy expenditure and spontaneous physical activity [54–61]. Therefore, it is necessary to test the efficacy and feasibility of programs focused primarily on the promotion of autonomy for physical activity and/or in reducing sedentary behavior in obese populations.
This study had some limitations. First, not all participants attended the focus groups (77% and 73% of adherence in the I-HAES® and CTRL groups at pre-intervention, and 82% and 58% of adherence in the I-HAES® and CTRL groups at post-intervention). However, the participants who attended the discussions expressed different ideas and, at some point, most of them were reinforced, indicating that the focus groups had reached saturation. Second, we did not evaluate body composition, which could have revealed a beneficial effect of exercise on lean and fat mass. Third, we were not able to evaluate participants who dropped out of the intervention and the relatively low retention may have contributed to some null findings. Finally, the major practical issue with lifestyle modifications lies in the long-term ability to sustain the short-term benefits. Although the current findings are promising, long-term studies should re-examine the feasibility, efficacy and effectiveness of this intervention.
Conclusion
This novel seven-month intensive interdisciplinary HAES®-based non-prescriptive intervention in obese women improved participants’ eating attitudes and practices, perception of body image, physical capacity, and health-related quality of life despite no changes in body weight and spontaneous physical activity levels. Importantly, these results were corroborated through qualitative analysis showing that our novel approach was superior to that of a traditional HAES®-based program.
Supporting information
(DOC)
(DOCX)
Data are expressed as mean ± SD or n (%) of total sample per group. Significance level defined as p ≤ 0.05 (nonpaired t-test or chi-square test).
(DOCX)
Acknowledgments
The authors acknowledge Professors Nágila Raquel Teixeira Damasceno e Marly Augusto Cardoso for technical support, the professionals involved in the design of the intervention, the monitors (Rafaela Faria Lemos, Jhessica Campos Victor, Victoria Lima, Felipe Gregório, Stefan Tanabe, Leticia Pironato, Cristiane Siqueira), and the professor Dra. Sophie Deram and her editor Christian Sperli for providing the book [23] for material support.
Data Availability
All relevant data are within the paper and its Supporting Information files. The design and rationale of the study was published in the journal Nutrition and Health (DOI: 10.1177/0260106017731260).
Funding Statement
We acknowledge the support by the Research Support Foundation of the State of São Paulo (FAPESP), grant number 2015/03878-2. Finally, each author received a fellowship grant. FBS was supported by CNPq (grant number 311357/2015-6) and FAPESP (grant number 2017/17424-9), AJP, PdMS, and RFU by FAPESP (grants numbers 2015/26937-4, 2017/05651-0, and 2015/12235-8, respectively), BG has a productivity grant by CNPq and is also supported by CAPES, and MDU by CAPES. The funding sources had no involvement in study design and in the collection, analysis and interpretation of data.
References
- 1.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7 [DOI] [PubMed] [Google Scholar]
- 2.ten Have M, de Beaufort I, Teixeira P, Mackenbach J, van der Heide A. Ethics and prevention of overweight and obesity: an inventory. Obes Rev. 2011; 12: 669–679. doi: 10.1111/j.1467-789X.2011.00880.x [DOI] [PubMed] [Google Scholar]
- 3.Leske S, Strodl E, Hou X. A qualitative study of the determinants of dieting and non-dieting approaches in overweight/obese Australian adults. BMC Public Health. 2012;12(1). doi: 10.1186/1471-2458-12-1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai A, Wadden T. Systematic Review: An Evaluation of Major Commercial Weight Loss Programs in the United States. ACC Current Journal Review. 2005;14(5):15 doi: 10.1016/j.accreview.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 5.Aphramor L. Validity of claims made in weight management research: a narrative review of dietetic articles. Nutr J. 2010;9(1). doi: 10.1186/1475-2891-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fulwiler C, Siegel JA, Allison J, Rosal MC, Brewer J, King JA. Keeping Weight Off: study protocol of an RCT to investigate brain changes associated with mindfulness-based stress reduction. BMJ Open. 2016; 6(11):e012573 doi: 10.1136/bmjopen-2016-012573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.(ASDAH) Association for Size Diversity and Health. Available at: https://www.sizediversityandhealth.org/. (2006)
- 8.Carbonneau E, Bégin C, Lemieux S, Mongeau L, Paquette M, Turcotte M et al. A Health at Every Size intervention improves intuitive eating and diet quality in Canadian women. Clin Nutr. 2017;36(3):747–754. doi: 10.1016/j.clnu.2016.06.008 [DOI] [PubMed] [Google Scholar]
- 9.Mensinger J, Calogero R, Stranges S, Tylka T. A weight-neutral versus weight-loss approach for health promotion in women with high BMI: A randomized-controlled trial. Appetite. 2016;105:364–374. doi: 10.1016/j.appet.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 10.Mensinger J, Calogero R, Tylka T. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite. 2016a;102:32–43. doi: 10.1016/j.appet.2016.01.033 [DOI] [PubMed] [Google Scholar]
- 11.Borkoles E, Carroll S, Clough P, Polman R. Effect of a non-dieting lifestyle randomised control trial on psychological well-being and weight management in morbidly obese pre-menopausal women. Maturitas. 2016;83:51–58. doi: 10.1016/j.maturitas.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 12.Leblanc V, Provencher V, Bégin C, Corneau L, Tremblay A, Lemieux S. Impact of a Health-At-Every-Size intervention on changes in dietary intakes and eating patterns in premenopausal overweight women: Results of a randomized trial. Clin Nutr. 2012;31(4):481–488. doi: 10.1016/j.clnu.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 13.Provencher V, Bégin C, Tremblay A, Mongeau L, Corneau L, Dodin S et al. Health-At-Every-Size and Eating Behaviors: 1-Year Follow-Up Results of a Size Acceptance Intervention. J Am Diet Assoc. 2009;109(11):1854–1861. doi: 10.1016/j.jada.2009.08.017 [DOI] [PubMed] [Google Scholar]
- 14.Provencher V, Bégin C, Tremblay A, Mongeau L, Boivin S, Lemieux S. Short-Term Effects of a “Health-At-Every-Size” Approach on Eating Behaviors and Appetite Ratings*. Obesity. 2007;15(4):957–966. doi: 10.1038/oby.2007.638 [DOI] [PubMed] [Google Scholar]
- 15.Carroll S, Borkoles E, Polman R. Short-term effects of a non-dieting lifestyle intervention program on weight management, fitness, metabolic risk, and psychological well-being in obese premenopausal females with the metabolic syndrome. Appl Physiol Nutr Metab. 2007;32(1):125–142. doi: 10.1139/h06-093 [DOI] [PubMed] [Google Scholar]
- 16.Bacon L, Stern J, Van Loan M, Keim N. Size Acceptance and Intuitive Eating Improve Health for Obese, Female Chronic Dieters. J Am Diet Assoc. 2005;105(6):929–936. doi: 10.1016/j.jada.2005.03.011 [DOI] [PubMed] [Google Scholar]
- 17.Gagnon-Girouard M, Bégin C, Provencher V, Tremblay A, Mongeau L, Boivin S et al. Psychological Impact of a “Health-at-Every-Size” Intervention on Weight-Preoccupied Overweight/Obese Women. J Obes. 2010;2010:1–12. doi: 10.1155/2010/928097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ulian MD, Benatti F, de Campos-Ferraz P, Roble O, Unsain R, de Morais Sato P et al. The Effects of a “Health at Every Size®”-Based Approach in Obese Women: A Pilot-Trial of the “Health and Wellness in Obesity” Study. Front Nutr. 2015a; doi: 10.3389/fnut.2015.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ulian M, Gualano B, Benatti F, de Campos-Ferraz P, Roble O, Modesto B et al. “Now I Can Do Better”: A Study of Obese Women's Experiences following a Nonprescriptive Nutritional Intervention. Clin Med Insights Womens Health. 2015b;8:CMWH.S23163 doi: 10.4137/CMWH.S23163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ulian M, Gualano B, Benatti F, de Campos-Ferraz P, Coelho D, Roble O et al. The design and rationale of an interdisciplinary, non-prescriptive, and Health at Every Size®-based clinical trial: The “Health and Wellness in Obesity” study. J Nutr Health. 2017;23(4):261–270. doi: 10.1177/0260106017731260 [DOI] [PubMed] [Google Scholar]
- 21.Motta DG. Aconselhamento nutricional In: Motta DG. Educação nutricional & diabetes tipo 2. Piracicaba: Jacintha, 2009. pp. 27–33. [Google Scholar]
- 22.Brasil. Ministério da Saúde (MS). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Guia Alimentar para a população brasileira. 2ed. Brasília: MS; 2014.
- 23.Deram S. O peso das dietas. 1st ed. São Paulo: Sensus; 2014. [Google Scholar]
- 24.Schopenhauer A. O mundo como vontade e representação. São Paulo: Unesp; 2005. [Google Scholar]
- 25.Platão (2011) Fédon. Belém: EDUFPA.
- 26.Espinosa B. Ética. Lisboa: Relógio D’água; 1992.
- 27.Nietzsche F. Aurora. São Paulo: Companhia das Letras; 2004a.
- 28.Nietzsche F. Genealogia da moral. São Paulo: Companhia das Letras; 2004b. [Google Scholar]
- 29.Nietzsche F. Humano, demasiado humano. São Paulo: Companhia das Letras; 2004c. [Google Scholar]
- 30.Sartre J-P. O ser e o nada. Petrópolis: Vozes; 2005. [Google Scholar]
- 31.Kierkegaard S. The concept of anxiety. Princenton: Princenton University, 2013. [Google Scholar]
- 32.Podsiadlo D, Richardson S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 33.Newcomer KL, Krug HE and Mahowald ML. Validity and reliability of the timed-stands test for patients with rheumatoid arthritis and other chronic diseases. J Rheumatol. 1993; 20:21–7. [PubMed] [Google Scholar]
- 34.Stunkard AJ, Sorenson T, Schulsinger F. Use of Adaption Registry for the study of obesity and thinness In: The Genetics of Neurological and Pshychiatric Disorders. Raven Press, New York, 1983, pp. 115–120. [Google Scholar]
- 35.Scagliusi F, Alvarenga M, Polacow V, Cordás T, de Oliveira Queiroz G, Coelho D et al. Concurrent and discriminant validity of the Stunkard's figure rating scale adapted into Portuguese. Appetite. 2006;47(1):77–82. doi: 10.1016/j.appet.2006.02.010 [DOI] [PubMed] [Google Scholar]
- 36.Ben-Tovim D, Walker M. The development of the Ben-Tovim Walker Body Attitudes Questionnaire (BAQ), a new measure of women's attitudes towards their own bodies. Psychol Med. 1991;21(03):775 doi: 10.1017/s0033291700022406 [DOI] [PubMed] [Google Scholar]
- 37.Scagliusi F, Polacow V, Coelho D, Philippi S, Cordás T, Alvarenga M et al. Psychometric Testing and Applications of the Body Attitudes Questionnaire Translated into Portuguese. Percept Mot Skills. 2005;101(1):25–41. doi: 10.2466/pms.101.1.25-41 [DOI] [PubMed] [Google Scholar]
- 38.WHOQOL Group (The). Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667 [DOI] [PubMed] [Google Scholar]
- 39.Fleck MPA. O instrumento de avaliação de qualidade de vida da Organização Mundial da Saúde (WHOQOL-100): características e perspectivas. Cien Saude Colet. 2000; 5(1): 33–38. [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, USA: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 41.Bernard R, Ryan GW. Analyzing Qualitative Data: Systematic Approaches. Thousand Oaks: Sage; 2010. [Google Scholar]
- 42.Cohen J. A Coefficient of Agreement for Nominal Scales. Educ Psychol Meas. 1960;20(1):37–46. doi: 10.1177/001316446002000104 [Google Scholar]
- 43.Lee D, Artero E, Sui Xuemei, Blair S. Review: Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24(4_suppl):27–35. doi: 10.1177/1359786810382057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blair S. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–1098. doi: 10.1001/jama.273.14.1093 [PubMed] [Google Scholar]
- 45.Ross R, Janiszewski P. Is weight loss the optimal target for obesity-related cardiovascular disease risk reduction?. Can J Cardiol. 2008;24:25D–31D. doi: 10.1016/s0828-282x(08)71046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee S. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without Type 2 diabetes. J Appl Physiol. 2005;99(3):1220–1225. doi: 10.1152/japplphysiol.00053.2005 [DOI] [PubMed] [Google Scholar]
- 47.Dekker M, Lee S, Hudson R, Kilpatrick K, Graham T, Ross R et al. An exercise intervention without weight loss decreases circulating interleukin-6 in lean and obese men with and without type 2 diabetes mellitus. Metabolism. 2007;56(3):332–338. doi: 10.1016/j.metabol.2006.10.015 [DOI] [PubMed] [Google Scholar]
- 48.Slentz C, Duscha B, Johnson J, Ketchum K, Aiken L, Samsa G et al. Effects of the Amount of Exercise on Body Weight, Body Composition, and Measures of Central Obesity. Arch Intern Med. 2004;164(1):31 doi: 10.1001/archinte.164.1.31 [DOI] [PubMed] [Google Scholar]
- 49.Schaefer J, Magnuson A. A Review of Interventions that Promote Eating by Internal Cues. J Acad Nutr Diet. 2014;114(5):734–760. doi: 10.1016/j.jand.2013.12.024 [DOI] [PubMed] [Google Scholar]
- 50.O'Reilly G, Cook L, Spruijt-Metz D, Black D. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–461. doi: 10.1111/obr.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006; 56(530):666–672. [PMC free article] [PubMed] [Google Scholar]
- 52.Thompson D. Physical activity for physiologists. Physiol News. 2013:32–5 [Google Scholar]
- 53.Turner J, Markovitch D, Betts J, Thompson D. Nonprescribed physical activity energy expenditure is maintained with structured exercise and implicates a compensatory increase in energy intake. Am J Clin Nut. 2010;92(5):1009–1016. doi: 10.3945/ajcn.2010.29471 [DOI] [PubMed] [Google Scholar]
- 54.Di Blasio A, Ripari P, Bucci I, Di Donato F, Izzicupo P, D’Angelo E et al. Walking training in postmenopause. Menopause. 2012;19(1):23–32. doi: 10.1097/gme.0b013e318223e6b3 [DOI] [PubMed] [Google Scholar]
- 55.Goran M, Poehlman E. Total energy expenditure and energy requirements in healthy elderly persons. Metabolism. 1992;41(7):744–753. doi: 10.1016/0026-0495(92)90315-2 [DOI] [PubMed] [Google Scholar]
- 56.Manthou E, Gill JM, Wright A, Malkova D. Behavioural Compensatory Adjustments to Exercise Training In Overweight Women. Med Sci Sports Exerc. 2009;42(6):1121–8. doi: 10.1249/mss.0b013e3181c524b7 [DOI] [PubMed] [Google Scholar]
- 57.Meijer E, Westerterp K, Verstappen F. Effect of exercise training on total daily physical activity in elderly humans. Eur J Appl Physiol Occup Physiol. 1999;80(1):16–21. doi: 10.1007/s004210050552 [DOI] [PubMed] [Google Scholar]
- 58.Meijer G, Janssen G, Westerterp K, Verhoeven F, Saris W, ten Hoor F. The effect of a 5-month endurance-training programme on physical activity: evidence for a sex-difference in the metabolic response to exercise. Eur J Appl Physiol Occup Physiol. 1991;62(1):11–17. doi: 10.1007/bf00635626 [DOI] [PubMed] [Google Scholar]
- 59.Morio B, Montaurier C, Pickering G, Ritz P, Fellmann N, Coudert J et al. Effects of 14 weeks of progressive endurance training on energy expenditure in elderly people. Br J Nutr. 1998;80(06):511–519. doi: 10.1017/s0007114598001603 [DOI] [PubMed] [Google Scholar]
- 60.Westerterp K, Meijer G, Janssen E, Saris W, Hoor F. Long-term effect of physical activity on energy balance and body composition. Br J Nutr. 1992;68(01):21 doi: 10.1079/bjn19920063 [DOI] [PubMed] [Google Scholar]
- 61.Melanson E, Keadle S, Donnelly J, Braun B, King N. Resistance to Exercise-Induced Weight Loss. Med Sci Sports Exerc. 2013;45(8):1600–1609. doi: 10.1249/MSS.0b013e31828ba942 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
Data are expressed as mean ± SD or n (%) of total sample per group. Significance level defined as p ≤ 0.05 (nonpaired t-test or chi-square test).
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files. The design and rationale of the study was published in the journal Nutrition and Health (DOI: 10.1177/0260106017731260).