Abstract
Background
Many studies investigating the impact of individual risk factors on cord blood immune cell counts may be biased given that cord blood composition is influenced by a multitude of factors. The aim of this study was to comprehensively investigate the relative impact of environmental, hereditary and perinatal factors on cord blood cells.
Methods
In 295 neonates from the prospective Basel-Bern Infant Lung Development Cohort, we performed complete blood counts and fluorescence-activated cell sorting scans of umbilical cord blood. The associations between risk factors and cord blood cells were assessed using multivariable linear regressions.
Results
The multivariable regression analysis showed that an increase per 10μg/m3 of the average nitrogen dioxide 14 days before birth was associated with a decrease in leukocyte (6.7%, 95% CI:-12.1,-1.0) and monocyte counts (11.6%, 95% CI:-19.6,-2.8). Maternal smoking during pregnancy was associated with significantly lower cord blood cell counts in multiple cell populations. Moreover, we observed sex differences regarding eosinophilic granulocytes and plasmacytoid dendritic cells. Finally, significantly increased numbers of cord blood cells were observed in infants exposed to perinatal stress. Cesarean section seems to play a significant role in Th1/Th2 balance.
Conclusions
Our results suggest that all three: environmental, hereditary and perinatal factors play a significant role in the composition of cord blood cells at birth, and it is important to adjust for all of these factors in cord blood studies. In particular, perinatal circumstances seem to influence immune balance, which could have far reaching consequences in the development of immune mediated diseases.
Introduction
It is known that the late prenatal and neonatal period represent a critical window of immune vulnerability and on-going immune maturation [1]. Cellular and soluble markers from infantile cord blood are used as risk biomarkers in many outcome studies investigating the origin of immune mediated disease during this early window of immune maturation. Special interest was paid to immune development in terms of allergy and tolerance. However, a multitude of environmental, hereditary, and perinatal factors can influence the composition of cord blood cells. During fetal life, the immune response is physiologically skewed towards a Type 2 helper T cell (Th2) response [2]. At birth, the infant’s immune system begins a process of re-calibration towards a Type 1 helper T cell (Th1) response [3, 4]. It is known that dendritic cells play an important role in the pathogenesis of asthma and allergic disease influencing Th1/Th2 balance [5], and that these cells are influenced by nitrogen dioxide (NO2),[6] particulate matter (PM) [7] and tobacco smoke in adults [8, 9].
It has been shown that environmental factors, such as prenatal ambient air pollution, have important effects on cord blood cells [10–13] and on cord blood cytokine profiles [14]. Maternal tobacco smoke affects leukocyte counts [15, 16], and reduces natural killer cell activity in umbilical cord blood [17]. Hereditary factors, both hereditary allergy risk [18] and sex [19, 20], have been reported to affect cord blood cells. Finally, the effect of perinatal obstetric factors on cord blood cells [19–22], and cytokines [23, 24] has been reported several times in the last decades.
Each of these studies was limited in that their focus was on subpopulations of cord blood cells [10–13, 21, 22], they investigated high exposure populations [10–12], they did not take into account all potentially known influencing factors in a healthy population [10–13, 18–22], nor they did assess individual exposure to air pollution [10–13]. Given that all cells within cord blood are likely affected by small and interacting effects of varying origin, an examination of cord blood composition accounting for all known confounders and influencing factors is needed. Thus, our aim was to investigate the relative impact of environmental, hereditary and perinatal factors on cord blood cells and on dendritic cells in particular, as master regulators of the Th1/Th2 balance. This investigation was carried out within a prospective birth cohort of healthy unselected term born neonates by way of a comprehensive multivariable statistical approach, using a sophisticated spatio-temporal exposure modeling of air pollutants.
Materials and methods
Ethics statement
The ethics committees of the regions of Bern and Basel approved the study and written informed consent of the parents was obtained at enrolment.
Study design
Between April 1999 and July 2014, 295 subjects were enrolled from the prospective Basel-Bern Infant Lung Development Cohort (BILD). The study design, exclusion and inclusion criteria, and detailed questionnaires are reported in Fuchs et al. [25]. In brief, we investigated whether prenatal environmental exposures, hereditary and perinatal risk factors were associated with alterations in cord blood cell numbers in unselected middle European population of healthy new-borns prenatally recruited at the four major maternity hospitals and obstetric practices in the agglomeration of Bern, Switzerland. Exclusion criteria for this study were preterm delivery at <37 weeks of gestation, ethnicity other than European white, severe maternal health problems, maternal drug abuse other than nicotine, birth defects, major respiratory disease after birth, and/or significant perinatal disease.
Outcome assessment
Cord blood was taken by venipuncture from the umbilical cord directly after birth and collected in sterile Ethylenediaminetetraacetic acid tubes. Blood analysis was performed within 12h after birth. Complete blood counts with correction for nucleated red blood cells were performed by the haematological laboratory of the University Hospital of Berne using a Cell-Dyn 3500R (Abbott, Baar, Switzerland). Dendritic cells as well as basophilic and eosinophilic granulocytes were, as previously described [16], flowcytometrically identified using a fluorescence-activated cell sorting scan (FACS-scan) (BD Bioscience, Franklin Lakes, NJ). The following monoclonal mouse anti-human antibodies, purchased from BD Bioscience, were used: anti-CD11c allocyanin (APC), anti-CD123 phycoerythrin (PE), lineage cocktail (lin 1) FITC (anti-CD3, CD14, CD16, CD19, CD20, and CD56), and anti-HLA-DR peridinin chlorophyll protein (PerCP). Mouse anti-human IgG2a APC, PerCP, FITC, and mouse anti-human IgG1 PE were used as isotype controls. Cells were identified as follows: Step 1) mononuclear cells were gated based on forward and side scatter signals; Step 2) cells where then selected within the gated population by four color-flowcytometry; myeloid dendritic cells: lin 1 negative, HLA-DR positive and CD11c bright; plasmacytoid dendritic cells: lin 1 negative, HLA-DR positive and CD123 bright; basophilic granulocytes: lin 1 negative, HLA-DR negative and CD123 positive; eosinophilic granulocytes: lin1 dim, HLA-DR dim, CD11c positive, CD123 dim.
Six children were excluded from further analysis due to technical errors. Of the 289 infants with good quality cord blood samples, in 261 we performed a differential leukocyte blood count, and 246 had a measurement of thrombocytes. In 253 children we were able to perform a FACS-scan determining basophilic granulocytes, eosinophilic granulocytes and dendritic cells. The different numbers in the FACS scan outcomes are due to an updated gating strategy for cord blood dendritic cells implemented after October 2006. Although all original FACS scan analyses (n = 253) were stored on long life compact discs for 51Infants (recruitment 1999–2002), the original data were no longer readable so that a reanalysis according to the new gating strategies was not possible and those measurements had to be excluded from final analysis.
Exposure assessment
Environmental exposure
Maternal NO2 exposure was assessed at the residential addresses of study participants using a spatio-temporal model [26]. The model is based on traffic data, road network, land use, population, and an NO2 dispersion model to account for spatial variability; seasonality, meteorological conditions and a continuous running fixed air quality monitor to capture temporal variability. This method allowed for the estimation of mean NO2 levels at the address of each study participant in the third trimester, at days 30 and 14 prior to delivery. These particular time points were selected as they were shown to be important for lung development and as possibly crucial periods for the influence of air pollution on the immune system [12, 27]. Individual exposure to PM10 was assessed for the same timepoints, averaging the daily PM10 mean values from the background Swiss National Air Pollution Monitoring Network station Payerne, which is located within the study area. As a proxy for long term traffic-related pollution exposure, the distance from the mothers’ homes to the closest major road of ≥6 meters in width was calculated (GIS; ArcGIS, version 9, Environmental System Research Institute, Redlands, USA) and classified into two categories: 0–50 meters and ≥50 meters based on a previous study from our group [14]. Home addresses were geo-coded using the building registry of the Swiss Federal Statistical Office, and street information was obtained from the VECTOR25 map of the Swiss Federal Office of Topography (Wabern).
Maternal and paternal smoking habits during pregnancy were assessed by means of a standardized questionnaire. Maternal smoking habits were validated by chromatographic measured cotinine levels in the first urine of the newborns [25]. In one child the mother’s smoking history (nonsmoker) was contradicted by a high urine cotinine level (93ng/mL), and was therefore reclassified. Maternal passive smoking exposure was determined based on information about smoking exposure at home and at the workplace.
Hereditary factors
Several factors were assessed at enrolment based on a standardized questionnaire: sex, paternal atopic disease history, and maternal atopic disease history (allergic -rhinitis, -eczema, and -asthma), as described [25].
Perinatal factors
Information about perinatal circumstances were recorded by a responsible midwife at birth: parity, vaginal or cesarean delivery, meconium stained amniotic fluid, Apgar-Scores, umbilical vein pH, umbilical artery pH, pathological cardiotocography (CTG), premature rupture of the membranes, and gestational age.
Statistical analysis
Cell counts were inspected for normality and, if necessary, were transformed before analysis (leukocytes, monocytes, lymphocytes, segmented neutrophils, basophils, eosinophils, pDCs, mDCs and pDC/mDC). Univariable, bivariable and multivariable linear regression models were applied to investigate the association between cord blood cell counts and known environmental, hereditary and perinatal risk factors. Covariates of concern were chosen a priori from the literature and included in the model. First we ran a univariable model for each risk factor against blood cells (simple model). Based on results from simple models and to minimize the multiple comparison issues, we focused on the pathological CTG as a main perinatal parameter representing stress during delivery. Subsequently, all cell counts were adjusted for known risk factors: sex, gestational age, birth order (classified as first born and subsequent born infants), mode of delivery, pathological CTG, maternal smoking during pregnancy, maternal atopy, season of birth (cosine term), the concentration of either PM10 or NO2 during the last trimester, the last 30 or 14 days preceding delivery (adjusted model). The cell subtypes measured by FACS were additionally controlled for the change in gating strategy (0 –measurements until October 2006, 1-after that date). We repeated the analysis restricting our sample size to participants without maternal smoking activity during pregnancy to assess the effect of maternal exposure to passive smoking on cord blood cells.
In the sensitivity analysis, we additionally adjusted the models with PM10 exposure for the residential distance to major roads.
Results are expressed as absolute difference in cell counts for untransformed outcomes and as a percent difference for log-transformed outcomes [100 × (exponentiated mean -1)] with 95% confidence interval (CI). Effect estimates for air pollution are presented per standardized increment of 10μg/m3. A p-value <0.05 was considered significant. All statistical analyses were performed using Stata version 11.2 (StataCorp., College Station, TX, USA).
Results
A subgroup of 295 infants of the BILD cohort was included in this study. Anthropometric data, air pollution exposure data, and the distribution of possible risk factors are given in Table 1. Complete blood count analyses as well as FACS analysis results are given in Table 2.
Table 1. Population characteristics.
| Mean(±SD) / n(%) | n | |
|---|---|---|
| Demographic Characteristics | ||
| Gestational age, weeks | 39.8 (±1.1) | 278 |
| Air pollution exposure | ||
| Outdoor | ||
| Mean PM10, last 14 days before delivery, μg/m3 | 18.4 (±8.0) | 278 |
| Mean PM10, last 30 days before delivery, μg/m3 | 19.1 (±7.1) | 278 |
| Mean PM10, third trimester of pregnancy, μg/m3 | 19.1 (±5.3) | 278 |
| Mean NO2, last 14 days before delivery, μg/m3 | 18.5 (±7.4) | 265 |
| Mean NO2, last 30 days before delivery, μg/m3 | 18.5 (±7.4) | 265 |
| Mean NO2, third trimester of pregnancy, μg/m3 | 18.5 (±7.2) | 265 |
| Distance to major roads, m | 327 (±484) | 276 |
| Indoor | ||
| Maternal smoking during pregnancy, yes | 25 (9%) | 278 |
| Passive smoking during pregnancy, yes | 53 (19.1%) | 277 |
| Hereditary Factors | ||
| Sex, male | 153 (55%) | 278 |
| Maternal atopy, yes | 94 (33.8%) | 278 |
| Perinatal Factors | ||
| Mode of delivery, cesarean section | 42 (15.1%) | 278 |
| Pathological CTG, yes | 27 (9.7%) | 278 |
| Meconium within amniotic fluid, yes | 37 (13.4%) | 277 |
| Older siblings, yes | 169 (60.8%) | 278 |
| Premature rupture of the fetal membranes, yes | 16 (5.9%) | 270 |
Abbreviations: PM10, Particulate matter <10 μm in diameter; NO2, nitrogen dioxide; CTG, Cardiotocogramm
Table 2. Cord blood cell counts and FACS analysis.
| Mean (±SD) | n | |
|---|---|---|
| Total Leukocytes (x109/l) | 13.7 (±4.4) | 289 |
| Banded neutrophils (x109/l) | 0.8 (±0.7) | 260 |
| Segmented neutrophils (x109/l) | 5.9 (±2.7) | 261 |
| Monocytes (x109/l) | 1.3 (±0.6) | 260 |
| Lymphocytes (x109/l) | 4.9 (±1.9) | 261 |
| Eosinophilic granulocytes (x109/l) | 0.39 (±0.4) | 253 |
| Basophilic granulocytes (x109/l) | 0.05 (±0.04) | 252 |
| mDCs (x109/l) | 0.007 (±0.005) | 199 |
| pDCs (x109/l) | 0.010 (±0.008) | 199 |
| Thrombocytes (x109/l) | 283 (±66.4) | 246 |
Abbreviations: mDC, myeloid dendritic cells; pDC, plasmacytoid dendritic cells
Environmental exposure
Results for environmental exposures are summarized in Table 3. In general, the statistical associations were less significant in the simple models. Due to a high correlation between predicted NO2 values (Pearson correlation coefficient r = 0.91–0.99) (S1 Table) we observed similar effects of NO2 on cord blood cell counts at all studied time intervals. Given that the strongest effect of NO2 was mainly observed during the last 14 days before birth (S1 Fig), we are reporting results obtained from the models adjusted for this time period. PM10 and NO2 showed a moderate correlation (Pearson correlation coefficient r = 0.37–0.59, depending on the time period) (S1 Table).
Table 3. Simplea and adjustedb associations of cord blood cells with environmental risk factors.
| Maternal smoking during pregnancy | NO2 during the last 14 days before deliveryc | |||||||
|---|---|---|---|---|---|---|---|---|
| Simple model | Adjusted model | Simple model | Adjusted model | |||||
| β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | |
| Leukocytes d | -17.5 [-27.9, -5.4] |
0.006 | -18.6 [-28.8, -7.0] |
0.003 | -4.9 [-9.8, 0.3] |
0.064 | -6.7 [-12.1, -1.0] |
0.023 |
| Banded neutrophils e | -11.4 [-39.3, 29.3] |
0.528 | -9.3 [-37.8, 32.0] |
0.609 | -9.3 [-21.8, 5.1] |
0.195 | -15.5 [-28.6, 0.1] |
0.052 |
| Segmented neutrophils d | -1.07 [-1.90, -0.24] |
0.011 | -1.17 [-2.05, -0.29] |
0.009 | -0.24 [-0.72, 0.24] |
0.326 | -0.43 [-0.98, 0.12] |
0.128 |
| Monocytes d | -25.0 [-39.7, -6.7] |
0.010 | -24.6 [-39, -6.7] |
0.009 | -8.4 [-16.0–0.2] |
0.046 | -11.6 [-19.6, -2.8] |
0.012 |
| Lymphocytes d | -24.3 [-37.3, -8.5] |
0.004 | -16.9 [-29.7; 2] |
0.029 | -1.7 [-8.2, 5.2] |
0.618 | -4 [-11; 3.4] |
0.280 |
| Eosinophilic granulocytes d | -14.4 [-44.4, 31.6] |
0.477 | -15.0 [-44.9, 30.0] |
0.463 | -3.3 [-18.3, 14.3] |
0.691 | -2.9 [-20.7, 10.1] |
0.777 |
| Basophilic granulocytes d | -38.0 [-56.6, -11.6] |
0.009 | -37.3 [-56.3, -11.2] |
0.009 | -0.7 [-13.7, 14.3] |
0.922 | -1.0 [-16.2, 16.8] |
0.900 |
| pDCs d | -40.6 [-62.7, -5.5] |
0.028 | -42.9 [-63.3, -11.1] |
0.013 | -0.3 [-16.4, 19.0] |
0.980 | 2.6 [-16.0, 25.2] |
0.799 |
| mDCs d | -36.4 [-59.1, -1.2] |
0.044 | -36.6 [-59.6, -0.80] |
0.046 | -9.1 [-23.1, 7.5] |
0.264 | -11.3 [-27.6, 8.6] |
0.245 |
| pDC/mDC d | -7.8 [-36.9, 34.8] |
0.676 | -10.7 [-38.5, 30.3] |
0.555 | 7.8 [-6.6, 23.4] |
0.300 | 14.0 [-4.0, 35.2] |
0.133 |
| Thrombocytes e | -38.3 [-69.5, -7.00] |
0.017 | -45.9 [-77.0, -14.7] |
0.004 | 6.0 [-6.5, 18.5] |
0.344 | 9.65 [-4.46, 23.8] |
0.179 |
Abbreviations: NO2, nitrogen dioxide; β, coefficient; CI, confidence interval; mDC, myeloid dendritic cell; pDC, plasmacytoid dendritic cell
a basophilic granulocytes, eosinophilic granulocytes, pDCs, mDCs, and the pDCs/mDCs ratio were additionally adjusted for the change in gating strategy; for other cells, univariable associations are presented.
b adjusted for sex, gestational age, birth order, gestational age, mode of delivery, CTG, maternal smoking during pregnancy, maternal atopy, season of birth and 14 days average of NO2.
c Effect estimates for NO2 are presented per 10 μg/m3 NO2 increase
d Results are expressed as percent difference
e Results are expressed as a difference in absolute cell counts
Multivariable analysis revealed significant negative associations between exposure to NO2 and leukocyte and monocyte counts (β = -6.7, 95% CI:-12.1,-1.0, and β = -11.6, 95% CI:-19.6,-2.8, respectively) (Table 3 and S1 Fig). There was no association between PM10 exposure and any of the cord blood cells (data not shown).
Cord blood cell numbers, except those for banded neutrophils and eosinophilic granulocytes, were significantly decreased in neonates with maternal smoking exposure during pregnancy (Table 3). When we restricted our sample size to neonates without maternal smoking exposure during pregnancy, we found no evidence for an association between maternal passive smoking exposure and cord blood cell counts (data not shown).
Hereditary risk factors
Eosinophilic granulocyte counts and pDCs were significantly higher in boys compared to girls in adjusted models (S2 Table). We did not observe a significant difference in cord blood cell numbers between neonates with and without maternal atopy or maternal asthma (data not shown).
Perinatal risk factors
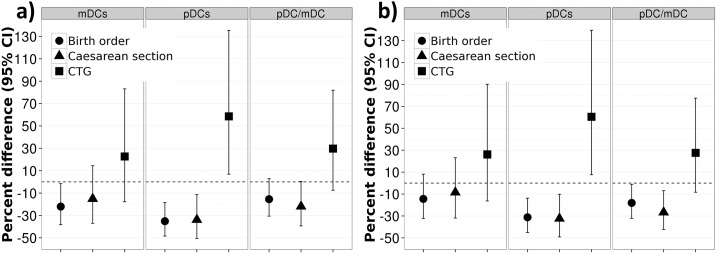
In the simple models, the second and subsequent births (birth order) were associated with decreased monocyte, basophilic granulocyte and pDC counts in neonates (Table 4). Associations were stable after adjustment for other risk factors. In the multivariable model, including exposure to NO2, the effect of birth order was also seen for mDC counts (β = -22.1; 95% CI:-38.3,-1.56). However, we did not observe any significant association between birth order and mDC counts after adjustment for PM10 exposure (Fig 1).
Table 4. Simplea and adjustedb associations of cord blood cells with perinatal risk factors.
| Birth order | Mode of delivery | CTG | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Simple model | Adjusted model | Simple model | Adjusted model | Simple model | Adjusted model | |||||||
| β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | β [95% CI] |
p-value | |
| Leukocytes c | -6.5 [-13.7, 1.3] |
0.102 | -5.5 [-12.8, 2.31] |
0.161 | -10.6 [-20.0, -0.1] |
0.048 | -11.9 [-21.0, -1.7] |
0.024 | 18.2 [3.9, 34.5] |
0.011 | 16.6 [2.7, 32.4] |
0.018 |
| Banded neutrophils d | -19.9 [-35.9; 1.0] |
0.051 | -17.6 [-34.3, 3.3] |
0.094 | -8.3 [-32.5, 24.5] |
0.578 | -9.4 [-33.5, 23.3] |
0.526 | 40.1 [-3.8, 4.1] |
0.078 | 39.1 [-4.6, 102;9] |
0.086 |
| Segmented neutrophils c | -0.4 [-1.2, 0.3] |
0.282 | -0.32 [-1.1, 0.4] |
0.409 | -0.7 [-1.6, 0.2] |
0.129 | -0.76 [-1.7, 0.18] |
0.113 | -0.1 [-1.3, 1.0] |
0.804 | -0.2 [-1.3, 1.0] |
0.754 |
| Monocytes c | -13.6 [-24.1, -1.6] |
0.028 | -13.5 [-23.9, -1.74] |
0.026 | -7.5 [-22.7, 10.8] |
0.399 | -9.6 [-24.2, 7.9] |
0.264 | 40.7 [12.9, 75.6] |
0.003 | 33.9 [7.8, 66.5] |
0.009 |
| Lymphocytes c | -1.3 [-10.9, 9.3] |
0.801 | -1.7 [-11.1, 8.6] |
0.733 | -4.6 [-16.8, 9.4] |
0.499 | -5.6 [-17.8, 8.3] |
0.409 | 46.9 [24.4, 73.5] |
<0.001 | 43.2 [20.8, 69.7] |
<0.001 |
| Eosinophilic granulocytes c | -9.7 [-28.8, 14.5] |
0.398 | -14.6 [-33.3, 9.3] |
0.193 | -18.4 [-41.4, 13.6] |
0.226 | -22.7 [-44.8, 8.1] |
0.221 | 19.1 [-19.7, 76.8] |
0.383 | 8.7 [-27.2, 62.4] |
0.899 |
| Basophilic granulocytes c | -21.8 [-35.8, -4.8] |
0.015 | -21.3 [-35.7, -3.7] |
0.020 | -20.0 [-40.0, 4.1] |
0.094 | -25.4 [-43.3, -1.9] |
0.036 | 42.4 [2.7, 97.6] |
0.034 | 30.7 [-5.7, 81.4] |
0.108 |
| pDCs c | -33.5 [-46.2, -16.2] |
0.001 | -35.1 [-48.4, -18.4] |
<0.001 | -30.3 [-48.6, -5.5] |
0.021 | -33.8 [-50.5, -11.4] |
0.006 | 77.6 [18.4, 166.4] |
0.006 | 58.6 [6.9, 135.4] |
0.022 |
| mDCs c | -19.8 [-36.0, 0.4] |
0.054 | -22.1 [-38.3, -1.56] |
0.036 | -11.7 [-34.3, 18.8] |
0.409 | -15.1 [-37.0, 14.4] |
0.280 | 32.8 [-10.0, 96.1] |
0.152 | 22.7 [-17.7, 83.1] |
0.314 |
| pDC/mDC c | -16.5 [-31.1, 1.1] |
0.065 | -15.5 [-30.6, 3.0] |
0.094 | -21.8 [-39.1; 0.4] |
0.054 | -21.9 [-39.3, 0.4] |
0.054 | 32.1 [-5.1, 84.0] |
0.099 | 29.7 [-7.5, 81.9] |
0.130 |
| Thrombocytes d | 11.6 [-6.4, 29.7] |
0.206 | 10.9 [-7.3, 29.1] |
0.238 | -18.9 [-42.8; 5.0] |
0.120 | -19.7 [-43.5, 4.2] |
0.105 | -36.8 [-65.5, -8.2] |
0.012 | -41.1 [-69.9, -12.2] |
0.005 |
Abbreviations: CTG, Cardiotocogramm; β, coefficient; CI, confidence interval; mDC, myeloid dendritic cell; pDC, plasmacytoid dendritic cell
a basophilic granulocytes, eosinophilic granulocytes, pDCs, mDCs, and the pDCs/mDCs ratio were additionally adjusted for the change in gating strategy; for other cells univariable associations are presented.
b adjusted for sex, gestational age, birth order, gestational age, mode of delivery, CTG, maternal smoking during pregnancy, maternal atopy, season of birth, and 14 days average of NO2
c Results are expressed as percent difference
d Results are expressed as a difference in absolute cell counts
Fig 1. a+b. Adjusteda effect of perinatal stress factors on mDCs, pDCs, and pDCs/ mDCs ratio in multivariable models using a) NO2 and b) PM10 exposure during last 14 days before the birth.
a adjusted for sex, gestational age, birth order, gestational age, mode of delivery, CTG, maternal smoking during pregnancy, maternal atopy, change in the gating strategy, and season of birth.
Neonates delivered via C-section had lower cord blood cell numbers than neonates delivered vaginally (Table 4). The effect of mode of delivery was stronger in adjusted models. Significant associations were found for leukocyte and basophilic granulocyte counts and pDCs. The pDC/mDC ratio was decreased in neonates delivered via C-section with a borderline significance level (β = -21.9; 95% CI:-39.3,04), due to a more pronounced reduction in pDC than in mDC counts (β = -33.8; 95% CI:-50.5,-11.4 and β = -15.1; 95% CI:-37.0,14.4, respectively) (Table 4 and Fig 1a). However, in the multivariable model, which accounted for PM10 exposure, we observed a significant association between the pDC/mDC ratio and the delivery mode (β = -26.7; 95% CI:-42.3, -6.9) (Fig 1b).
Prenatal Stress expressed by pathological CTG tended to increase cord blood cell numbers except for thrombocytes, which showed a decrease (Table 4). Adjustment for other confounders attenuated the magnitude of the associations, but most of them remained significant. Cell numbers associated with pathological CTG include: leukocytes, monocytes, lymphocytes, pDCs, and thrombocytes.
Sensitivity analysis
There was no evidence for an association between distance to major roads and cord blood cell counts (data not shown). Adjusted models suggested statistically significant dose-response trends between the number of cigarettes smoked per day and a decrease in leukocyte-, lymphocyte-, monocyte-, basophilic granulocyte-, pDC-, and thrombocyte-counts (data not shown). Sensitivity analyses revealed only small trend differences between 14 infants (out of 36) delivered by emergency C-section and 22 infants born by elective caesarean section. These borderline trends were not reported due to lack of statistical power.
Discussion
Our results showed that even low level prenatal environmental exposure to NO2 and maternal smoking, but not to PM10, are associated with a significant decrease in multiple cord blood cell types. We showed a pronounced effect of mode of delivery on total leukocyte counts, basophilic granulocytes, and specifically pDC, with significantly lower levels of those cell populations in cesarean-born children. Cesarean-born children showed a borderline significant decrease in the pDC/mDC ratio, suggesting an immunological imbalance in cord blood. Sex specific effects were weak, only eosinophilic granulocytes and pDCs were significantly higher in boys compared to girls in adjusted models.
Comparison with previous air pollution exposure studies
Three studies from a larger project out of the Czech Republic reported a distinct effect of air pollution on cord blood cells. In one study, PM exposure during pregnancy was found to be associated with higher natural killer cell fractions in newborns [11]. A subsequent study found a decrease in T-lymphocyte fractions and an increase in B-lymphocyte fractions in cord blood by higher concentrations of PM2.5 14 days before birth [12]. Finally, a gestational-stage specific significant effect of PM2.5 on cord blood lymphocyte distribution was reported [10]. A French research group showed analogous results with increasing PM10 and NO2 exposure levels three months prior to and during pregnancy [13].
The concentrations of pollutants to which the mothers in our study were exposed are comparable to the French study [13] but differ widely from those in the Czech Republic [10–12]. In contrast to our study, both groups assessed the effect of outdoor pollution on cord blood cells without an individually modelled PM or NO2 exposure. Furthermore, outcomes were a percent of lymphocyte subpopulations which makes it difficult to compare their findings with the absolute cord blood cell values in our study. Moreover, differences in the findings from the Czech studies, in comparison to our study, may also be related to differences in particle size.
Several toxicology studies have described the effect of short-term exposure to NO2, presenting mixed results and hypotheses. Two independent studies showed a significant decrease of peripheral blood cells after NO2 exposure [28, 29]. 80–90% of inspired NO2 is absorbed in humans as nitrite, metabolized and then excreted in the urine [30]. Steenhof et al. [29] concluded that nitrite, as well as secondary oxidation products, may induce the observed systemic effects of NO2 exposure on peripheral blood cells in adults. Translating those findings to our study population we presume that nitrite and secondary oxidation products circulating in the mother’s blood can pass the placental barrier and generate the observed effects in the offspring’s blood.
Regarding the effect of maternal smoking on the cord blood cells of the infants, we were able to confirm the results of a previous publication [16]. One of our novel findings was the demonstration of a significant decrease in cord blood pDC, and in thrombocyte numbers, in infants of smoking mothers.
The effects of acute and chronic smoking on DCs are highly complex. A study in adult smokers showed in vivo a strong increase in mDC in bronchoalveolar lavage fluid, and a subsequent decrease in mDC in blood shortly after the onset of active smoking [8]. On the other hand, in chronic smokers, increased absolute DC values and an altered pDC/mDC ratio were found, compared to healthy controls [31]. The authors postulate that smoking may directly alter the immune response. As is well known, pDC and mDC are related to Th1 and Th2 immune responses, respectively. Thus, the hypothesis of tobacco induced immune modulation is also supported by other studies showing that in utero and postnatal exposure to environmental tobacco smoke skews the immune response towards a Th-2 phenotype [4, 9]. Despite the fact that smoking induced a significant decrease in cord blood dendritic cells in our study, the pDC/mDC ratio was not significantly polarized. We hypothesize that this finding may be affected by the relatively low dose tobacco exposure in participating mothers (<20 cigarettes/day) of our cohort. Smoking affects platelet activation [32]. The literature is, however, controversial about the effect of smoking on platelet counts in peripheral blood. The observed decrease of platelet counts in our population could possibly be explained through a higher aggregation under perinatal stress conditions of the pre-activated platelets.
Effects of hereditary and perinatal factors
There remains a lack in literature on hereditary influences on cord blood cells [18]. To our knowledge, no study to date has analyzed the influence of maternal atopy or asthma on absolute values of cord blood cells in offspring. Given our sample size, we were unable to detect any significant difference in cord blood cell levels in relation to maternal atopy or asthma. Sex differences in multiple aspects of immune development and immune response have been previously published [19, 20, 33]. As a novel finding, our study showed significantly higher pDCs in boys.
The effect of perinatal factors on cord blood cellular composition [19–22, 24] and on cytokines [23, 24] has been investigated in the past. Our results are in line with previous studies showing significantly lower total leukocyte numbers in children born via C-section compared to vaginal delivery [19, 20, 24], and higher numbers of cord blood cells in infants exposed to higher perinatal stress [21]. As a novel finding, we describe a borderline significant decrease in the pDC/mDC ratio in cesarean-born, compared to vaginally born, children. This suggests a potential selective effect of mode of delivery on pDC. Since dendritic cells play an important role in immune regulation, and influence the Th1/Th2 balance in the development of asthma and allergies, [5] further studies are needed to explore the potential modifying role of C-sections on DCs, the Th1/Th2 balance in early infancy, and the association of these findings to the subsequent risk of chronic immune disorders (e.g. asthma) later in life [34].
Methodological considerations
This is the first study, to our knowledge, investigating the effect of individually modeled outdoor air pollution, hereditary, and perinatal factors on absolute cord blood cell counts; and, in particular, on dendritic cells in cord blood.
A major strength of our study is the comprehensive approach accounting for the influence of multiple factors (environmental, hereditary, and perinatal) on cord blood cell counts. Our study distinguishes itself from previous studies investigating the effect of prenatal NO2 exposure on immunologic parameters of offspring due to our use of a time-space regression model to assess individual exposure for relevant time periods.
A major limitation of our study was that blood samples were assessed subsequently. In October 2006, due to the updated standards in the gating of DC in FACS, a new gating strategy was applied. Although all the available original FACS analyses prior to this date were re-gated according to the new gating strategies, a trend in higher dendritic cell values before the new gating strategy persisted. We adjusted for this in our final statistical models. PM10 exposure was not individually sampled; rather we used a simpler model to estimate levels from a background sampling station. This provides a good picture regarding temporal variability, which is known to be much more relevant for PM [35], but is weak in representing spatial variability. Due to the fact that total leukocyte counts consist of the sum of analyzed white blood cell subsets, some reported associations between total leukocytes and the different exposures might be influenced by specific subsets. On the other hand, considering that there is a common progenitor cell for all white blood cells, the association between multiple cell subsets and different exposures could be traced back to an effect on a common progenitor cell.
Conclusion
In conclusion, our results suggest that environmental, hereditary and perinatal factors play a significant role in the composition of cord blood cells at birth. Research studies involving cord blood cell counts need to be adjusted for all of these factors. Furthermore, this dataset may serve as a well characterized normative dataset for a Central-European population. In particular, avoidable factors such as NO2, even at low levels, and tobacco smoke seem to play an important role in cord blood cell composition. Moreover, perinatal circumstances seem to influence the immune balance, which could be important to explain of the association between C-sections and the subsequent risk of immune mediated diseases later in life [34].
Supporting information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors would like to thank all the study participants and their families for participation in the study. We would especially like to thank the BILD study team for the professional management of the study, and Karine Hugentobler for proof-reading the manuscript.
Data Availability
According to the ethics Committees of the Canton of Berne (http://www.gef.be.ch/) and North-Western Switzerland (https://www.eknz.ch/), data must be presented in a de-identified and protected form. To enforce data protection, the authors are thus able to make the anonymized minimal dataset only available on request. Raw data will be made available on request to the BILD executive committee, via the Data Request Form on http://www.bild-cohort.ch/en/data-repository/.
Funding Statement
Funding was provided by Schweizerischer Nationalfonds zur Förderung der Wissenschaftlichen Forschung (324730_144280 and 320030_163311) to Dr. Urs Frey. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Dietert RR, Etzel RA, Chen D, Halonen M, Holladay SD, Jarabek AM, et al. Workshop to identify critical windows of exposure for children’s health: immune and respiratory systems work group summary. Environ Health Perspect. 2000;108 (Suppl 3):483–90. Epub 2000/06/15. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prescott SL, Macaubas C, Holt BJ, Smallacombe TB, Loh R, Sly PD, et al. Transplacental Priming of the Human Immune System to Environmental Allergens: Universal Skewing of Initial T Cell Responses Toward the Th2 Cytokine Profile. The Journal of Immunology. 1998;160(10):4730–7. [PubMed] [Google Scholar]
- 3.Hertz-Picciotto I, Park H-Y, Dostal M, Kocan A, Trnovec T, Sram R. Prenatal Exposures to Persistent and Non-Persistent Organic Compounds and Effects on Immune System Development. Basic & Clinical Pharmacology & Toxicology. 2008;102(2):146–54. 10.1111/j.1742-7843.2007.00190.x [DOI] [PubMed] [Google Scholar]
- 4.Wang L, Joad JP, Abel K, Spinner A, Smiley-Jewell S, Liu H, et al. Effects of environmental tobacco smoke on the developing immune system of infant monkeys. Journal of Allergy and Clinical Immunology. 2007;120(2):445–51. 10.1016/j.jaci.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Lambrecht BN, Hammad H. The role of dendritic and epithelial cells as master regulators of allergic airway inflammation. The Lancet. 2010;376(9743):835–43. 10.1016/S0140-6736(10)61226-3. [DOI] [PubMed] [Google Scholar]
- 6.Hodgkins S, Ather J, Paveglio S, Allard J, Whittaker LeClair L, Suratt B, et al. NO2 inhalation induces maturation of pulmonary CD11c+ cells that promote antigen-specific CD4+ T cell polarization. Respiratory Research. 2010;11(1):102 10.1186/1465-9921-11-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porter M, Karp M, Killedar S, Bauer SM, Guo J, Williams DA, et al. Diesel-Enriched Particulate Matter Functionally Activates Human Dendritic Cells. American Journal of Respiratory Cell and Molecular Biology. 2007;37(6):706–19. 10.1165/rcmb.2007-0199OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lommatzsch M, Bratke K, Knappe T, Bier A, Dreschler K, Kuepper M, et al. Acute effects of tobacco smoke on human airway dendritic cells in vivo. European Respiratory Journal. 2010;35(5):1130–6. 10.1183/09031936.00090109 [DOI] [PubMed] [Google Scholar]
- 9.Vassallo R, Tamada K, Lau JS, Kroening PR, Chen L. Cigarette Smoke Extract Suppresses Human Dendritic Cell Function Leading to Preferential Induction of Th-2 Priming. The Journal of Immunology. 2005;175(4):2684–91. 10.4049/jimmunol.175.4.2684 [DOI] [PubMed] [Google Scholar]
- 10.Herr C, Dostal M, Ghosh R, Ashwood P, Lipsett M, Pinkerton K, et al. Air pollution exposure during critical time periods in gestation and alterations in cord blood lymphocyte distribution: a cohort of livebirths. Environmental Health. 2010;9(1):46 10.1186/1476-069X-9-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hertz-Picciotto I, Dostál M, Dejmek J, Selevan SG, Wegienka G, Gomez-Caminero A, et al. Air Pollution and Distributions of Lymphocyte Immunophenotypes in Cord and Maternal Blood at Delivery. Epidemiology. 2002;13(2):172–83. [DOI] [PubMed] [Google Scholar]
- 12.Hertz-Picciotto I, Herr CE, Yap P-S, Dostál M, Shumway RH, Ashwood P, et al. Air pollution and lymphocyte phenotype proportions in cord blood. Environmental health perspectives. 2005:1391–8. 10.1289/ehp.7610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baiz N, Slama R, Bene M-C, Charles M-A, Kolopp-Sarda M-N, Magnan A, et al. Maternal exposure to air pollution before and during pregnancy related to changes in newborn’s cord blood lymphocyte subpopulations. The EDEN study cohort. BMC Pregnancy and Childbirth. 2011;11(1):87 10.1186/1471-2393-11-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Latzin P, Frey U, Armann J, Kieninger E, Fuchs O, Röösli M, et al. Exposure to Moderate Air Pollution during Late Pregnancy and Cord Blood Cytokine Secretion in Healthy Neonates. PLoS ONE. 2011;6(8):e23130 10.1371/journal.pone.0023130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mercelina-Roumans PEAM, Breukers RBGE, Ubachs JMH, van Wersch JWJ. Hematological variables in cord blood of neonates of smoking and nonsmoking mothers. Journal of Clinical Epidemiology. 1996;49(4):449–54. 10.1016/0895-4356(95)00542-0. [DOI] [PubMed] [Google Scholar]
- 16.Pachlopnik Schmid JM, Kuehni CE, Strippoli M-PF, Roiha HL, Pavlovic R, Latzin P, et al. Maternal Tobacco Smoking and Decreased Leukocytes, Including Dendritic Cells, in Neonates. Pediatr Res. 2007;61(4):462–6. 10.1203/pdr.0b013e3180332d02 [DOI] [PubMed] [Google Scholar]
- 17.Castellazzi AM, Maccario R, Moretta A, De Amici M, Gasparoni A, Chirico G, et al. Effect of active and passive smoking during pregnancy on natural killer–cell activity in infants. Journal of Allergy and Clinical Immunology. 1999;103(1):172–3. 10.1016/S0091-6749(99)70542-7. [DOI] [PubMed] [Google Scholar]
- 18.Hrdý J, Kocourková I, Prokešová L. Impaired function of regulatory T cells in cord blood of children of allergic mothers. Clinical & Experimental Immunology. 2012;170(1):10–7. 10.1111/j.1365-2249.2012.04630.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang Y-H, Yang S-H, Wang T-F, Lin T-Y, Yang K-L, Chen S-H. Complete Blood Count Reference Values of Cord Blood in Taiwan and the Influence of Gender and Delivery Route on Them. Pediatrics & Neonatology. 2011;52(3):155–60. 10.1016/j.pedneo.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Glasser L, Sutton N, Schmeling M, Machan JT. A comprehensive study of umbilical cord blood cell developmental changes and reference ranges by gestation, gender and mode of delivery. J Perinatol. 2015. 10.1038/jp.2014.241 [DOI] [PubMed] [Google Scholar]
- 21.Lim FTH, Scherjon SA, van Beckhoven JM, Brand A, Kanhai HHH, Hermans JMH, et al. Association of stress during delivery with increased numbers of nucleated cells and hematopoietic progenitor cells in umbilical cord blood. American Journal of Obstetrics and Gynecology. 2000;183(5):1144–51. 10.1067/mob.2000.108848. [DOI] [PubMed] [Google Scholar]
- 22.Samelson R, Larkey DM, Amankwah KS, McConnachie P. Effect of Labor on Lymphocyte Subsets in Full-Term Neonates. American Journal of Reproductive Immunology. 1992;28(2):71–3. 10.1111/j.1600-0897.1992.tb00761.x [DOI] [PubMed] [Google Scholar]
- 23.Protonotariou E, Chrelias C, Kassanos D, Kapsambeli H, Trakakis E, Sarandakou A. Immune response parameters during labor and early neonatal life. In Vivo. 2010;24(1):117–23. . [PubMed] [Google Scholar]
- 24.Almanzar G, Schonlaub J, Hammerer-Lercher A, Koppelstaetter C, Bernhard D, Prelog M. Influence of the delivery modus on subpopulations and replication of lymphocytes in mothers and newborns. Early Hum Dev. 2015;91(12):663–70. 10.1016/j.earlhumdev.2015.09.010 . [DOI] [PubMed] [Google Scholar]
- 25.Fuchs O, Latzin P, Kuehni CE, Frey U. Cohort Profile: The Bern Infant Lung Development Cohort. International Journal of Epidemiology. 2012;41(2):366–76. 10.1093/ije/dyq239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Proietti E, Delgado-Eckert E, Vienneau D, Stern G, Tsai MY, Latzin P, et al. Air pollution modelling for birth cohorts: a time-space regression model. Environ Health. 2016;15(1):61 10.1186/s12940-016-0145-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Latzin P, Röösli M, Huss A, Kuehni CE, Frey U. Air pollution during pregnancy and lung function in newborns: a birth cohort study. European Respiratory Journal. 2009;33(3):594–603. 10.1183/09031936.00084008 [DOI] [PubMed] [Google Scholar]
- 28.Frampton MW, Boscia J, Roberts NJ, Azadniv M, Torres A, Cox C, et al. Nitrogen dioxide exposure: effects on airway and blood cells. American Journal of Physiology—Lung Cellular and Molecular Physiology. 2002;282(1):L155–L65. 10.1152/ajplung.2002.282.1.L155 [DOI] [PubMed] [Google Scholar]
- 29.Steenhof M, Janssen NAH, Strak M, Hoek G, Gosens I, Mudway IS, et al. Air pollution exposure affects circulating white blood cell counts in healthy subjects: the role of particle composition, oxidative potential and gaseous pollutants—the RAPTES project. Inhalation Toxicology. 2014;26(3):141–65. 10.3109/08958378.2013.861884 . [DOI] [PubMed] [Google Scholar]
- 30.Ewetz L. Absorption and metabolic fate of nitrogen oxides. Scandinavian Journal of Work, Environment and Health. 1993;19:21–7. [PubMed] [Google Scholar]
- 31.Chen X-Q, Liu X-F, Liu W-H, Guo W, Yu Q, Wang C-Y. Comparative analysis of dendritic cell numbers and subsets between smoking and control subjects in the peripheral blood. International journal of clinical and experimental pathology. 2013;6(2):290 [PMC free article] [PubMed] [Google Scholar]
- 32.Blache D, Bouthillier D, Davignon J. Acute influence of smoking on platelet behaviour, endothelium and plasma lipids and normalization by aspirin. Atherosclerosis. 1992;93(3):179–88. [DOI] [PubMed] [Google Scholar]
- 33.Pennell LM, Galligan CL, Fish EN. Sex affects immunity. Journal of Autoimmunity. 2012;38(2–3):J282–J91. 10.1016/j.jaut.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 34.Sevelsted A, Stokholm J, Bønnelykke K, Bisgaard H. Cesarean Section and Chronic Immune Disorders. Pediatrics. 2015;135(1):e92–e8. 10.1542/peds.2014-0596 [DOI] [PubMed] [Google Scholar]
- 35.Proietti E, Röösli M, Frey U, Latzin P. Air Pollution During Pregnancy and Neonatal Outcome: A Review. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2012;26(1):9–23. 10.1089/jamp.2011.0932 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
According to the ethics Committees of the Canton of Berne (http://www.gef.be.ch/) and North-Western Switzerland (https://www.eknz.ch/), data must be presented in a de-identified and protected form. To enforce data protection, the authors are thus able to make the anonymized minimal dataset only available on request. Raw data will be made available on request to the BILD executive committee, via the Data Request Form on http://www.bild-cohort.ch/en/data-repository/.