Abstract
Background and aims
Although first treatment approaches for Internet Use Disorders (IUDs) have proven to be effective, health care utilization remained low. New service models focus on integrated health care systems, which facilitate access and reduce burdens of health care utilization, and stepped-care interventions, which efficiently provide individualized therapy.
Methods
An integrated health care approach for IUD intended to (a) be easily accessible and comprehensive, (b) cover a variety of comorbid syndromes, and (c) take heterogeneous levels of impairment into account was investigated in a one-armed prospective intervention study on n = 81 patients, who were treated from 2012 to 2016.
Results
First, patients showed significant improvement in Compulsive Internet Use over time, as measured by hierarchical linear modeling. Effect sizes of outcome change from baseline to 6-month follow-up ranged from d = 0.48 to d = 1.46. Second, differential effects were found depending on patients’ compliance, demonstrating that high compliance resulted in significantly higher rates of change. Third, patients referred to minimal interventions did not differ significantly in amount of change from patients referred to intensive psychotherapy.
Discussion
Tailored interventions result in higher efficiency through optimized resource allocation and equal amounts of symptom change in all treatment conditions. Moreover, comprehensive, low-threshold interventions seem to increase health service utilization.
Keywords: integrated health care, mental health, treatment, Internet addiction, Internet Gaming Disorder, stepped-care
Introduction
Internet Gaming Disorder (IGD), which refers to psychological distress caused by uncontrolled Internet and video gaming, has recently been included in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as condition for future research (American Psychiatric Association, 2013). Prevalence rates in a representative German adolescent sample have been found to be 1.2% (Rehbein, Kliem, Baier, Mößle, & Petry, 2015).
Although excessive non-gaming Internet use has not yet been included in the DSM-5 because of insufficient data, research has shown that pathological non-gaming Internet use (such as chatting and surfing) is a growing burden and can lead to similar levels of impairment and thus should also be considered in future diagnostic categories (Strittmatter et al., 2015). Prevalence of any Internet Use Disorder (IUD; i.e., including both excessive gaming and non-gaming Internet activities) is estimated at about 6.0% in a meta-analysis (Cheng & Li, 2014). However, this study may overestimate the IUD prevalence, as it includes only studies which classify IUD by the Internet Addiction Test and the Young Diagnostic Questionnaire (Young, 1998). Furthermore, the meta-analysis includes non-representative convenience samples, which may contribute to a possible overestimation. Subthreshold pathology afflicts 13.3% of adolescent boys and girls (Rumpf, Meyer, & John, 2011).
Individuals with IUD show significant social, physical, and mental complaints (Gentile, 2009; Gentile et al., 2011; Moody, 2001; Müller, Ammerschläger, Freisleder, Beutel, & Wölfling, 2012; Pfeiffer, Mößle, Kleimann, & Rehbein, 2007) and overall reduced quality of life (Alonso et al., 2011; Bischof, Bischof, Meyer, John, & Rumpf, 2013). IUD is marked by severe comorbid mental health problems, such as depressive disorders, anxiety disorders, attention-deficit/hyperactivity disorders, or substance-related disorders (Black, Belsare, & Schlosser, 1999; Carli et al., 2013; Gentile et al., 2011; Morrison & Gore, 2010; Müller et al., 2012; Rehbein, Kleimann, & Mößle, 2009).
Although first treatment approaches for IUD have proven to be highly effective in reducing both IUD symptoms and comorbid psychopathology (King, Delfabbro, Griffiths, & Gradisar, 2011; Kuss & Lopez-Fernandez, 2016; Winkler, Dörsing, Rief, Shen, & Glombiewski, 2013), health care utilization remained disappointingly low. This might be due to several reasons: First, like other addictive disorders, IUD is characterized by low treatment motivation and readiness-to-change (O’Brien, Li, Snyder, & Howard, 2016). The proportion of untreated IUD patients in consequence of missing compliance is alarming (Wölfling, Jo, Bengesser, Beutel, & Müller, 2013). Second, in contrast to physical health care, access to mental health care is often unknown (Gröne & Garcia-Barbero, 2001). Third, treatment accessibility for IUD in Germany is particularly limited and impeded due to inconsistent institutional responsibilities. To date, IUD is not included in the current version of the International Classification of Diseases (ICD-10; Dilling, 2005), which would be necessary for health insurance coverage in the German health care system. Guidelines that indicate IUD treatment settings and requirements do not yet exist. At present, IUD is unsystematically treated (and financed correspondingly) by selected addiction counseling, educational counseling, or psychotherapy treatment institutions. This results in undersupply and treatment gaps for IUD patients.
Thus, it is a public health priority to enhance psychosocial health care systems for IUD, to facilitate access, and to reduce burdens of help-seeking. Specifically, effective health care structures and treatment programs for IUD should be (a) easily accessible and comprehensive (i.e., offering low-threshold services and care management), (b) cover comorbid syndromes, and (c) account for the heterogeneous target group and different levels of impairment.
In recent years, health service research has focused on improving psychosocial health care by developing new treatment models. Integrated health care systems, that focus on collaboration and integration of services, have been found to improve health care, to facilitate access and to reduce burdens of health care utilization, to establish a comprehensive referral system, and to ensure continuity of care (Gröne & Garcia-Barbero, 2001). They benefit from enhanced treatment quality, knowledge transfer, transparency, and cost-effectiveness (Amelung, 2008). Moreover, stepped-care approaches, that offer adaptable intervention types and intensities, following the idea that individual patients need individualized care, have been found to be both highly effective and economic (Haaga, 2000; Lindenberg, 2012). Thus, considering limited resources, stepped-care models result in optimized resource allocation.
In line with the aforementioned ideas, the Integrated Health Care Network for Diagnostics, Counseling and Treatment (IDCT), addressing people suffering from IUD was founded in November 2012 in Heidelberg (Germany). The IDCT consists of 16 institutions covering several health care sectors (addiction counseling, psychotherapy treatment, and educational counseling) and treatment approaches (psychodynamic, cognitive behavioral, and (hypno)-systemic treatment) in multiple treatment settings (inpatient, daycare, and outpatient treatment and counseling).
This study aims to assess the effects of the IDCT network for IUD patients in terms of symptom reduction over 6 months. First, we expect that the targeted referral within the integrated health care system (depending on comorbidities and levels of impairment) ensures specialized treatment and continuity of care, which results in significant symptom change over time. Second, we expect differential effects depending on patients’ compliance, assuming that high treatment compliance results in higher rates of change. Third, we expect that patients referred to addiction counseling do not differ significantly in recovery from patients referred to psychotherapy. The latter hypothesis refers to the idea that tailored interventions should result in higher efficiency through optimized resource allocation and equal effectiveness (non-inferiority) over treatment conditions.
As a contribution to this area of research, this study reports therapy outcomes for IUD patients treated and monitored for a period of 6 months each between 2012 and 2016.
Method
The study was conducted as a one-armed prospective intervention study with two follow-up assessments at 1 and 6 months after referral to specialized treatment.
Participants’ characteristics
In total, N = 120 adolescent and adult patients with a mean age of 19.21 years (SD = 6.46, range: 12–53 years) signed up for diagnostics and treatment at the IDCT health care center in Heidelberg, Germany between November 2012 and September 2016. The majority of these patients (97.5%) was male, 53.3% were underage adolescents and accompanied by a primary caregiver. The patient sample was composed of 46.7% high-school students, 11.7% trainees, 7.5% college students, 2.5% employees, 21.7% unemployed, and 10.0% without information on professional activity. Patients who missed IUD diagnosis were not included in the analysis, because this study focuses on the effects of IUD treatment in patients only. The analysis was done by intent-to-treat, i.e., we based our analyses on the initial treatment assignment and not on the treatment actually received. At baseline, n = 81 (67.5%) of the total sample met the criteria for IUD. The intervention was implemented in a routine care setting.
Procedure
Patients were informed about the IDCT by articles in newspapers, flyers and poster announcements, or directly referred by practitioners. All data were collected at the IDCT health care center, organized in an electronic database (Psycho EQ), and cryptographically secured. Reidentification was only possible through the encryption key. Database access was strictly controlled, automatically documented, and continuously monitored. Follow-up data were collected by sending coded paper–pencil questionnaires including return envelopes. If preferred, follow-up assessments could be completed online using the SoSci Survey platform (www.soscisurvey.de). Patients did not receive any monetary incentive for participation in the study. All treatments at the IDCT health care center were offered free of charge. Treatment costs were covered by the respective IDCT institution. These are financed by either compulsory health insurance or by local public, ecclesiastic, or non-profit organizations. A list of collaborating institutions can be found in the Appendix.
The IDCT health care center was established in November 2012 at the rural district office in Heidelberg, Germany. Clinical management and scientific investigation were realized by the University of Education Heidelberg and the Heidelberg University. The IDCT procedure included initial diagnostics, systematical referral to specific treatment conditions (in line with stepped-care), and symptom monitoring over 6 months.
At stage one (admission), all patients underwent a structured diagnostic procedure by means of a semi-structured clinical interview and psychometric self-report questionnaires. The clinical interview was developed by the IDCT group and covered IUD symptoms, such as craving, behavioral, and mental preoccupation, unsuccessful control, and dysfunctional emotion regulation (based on criteria of other behavioral addictions). Furthermore, past clinical history, psychological strain, and past help-seeking behavior were assessed. The clinical diagnosis was primarily justified by the interview and additionally supported by the psychometric questionnaires. All assessments were conducted by graduated clinicians, who were trained in applying the interview. In addition, caregivers or significant others were asked to provide external ratings for underaged patients. The data were analyzed by an independent clinician. Indication for specialized treatment was systematically derived from the diagnostic results and reported to patients 14 days later.
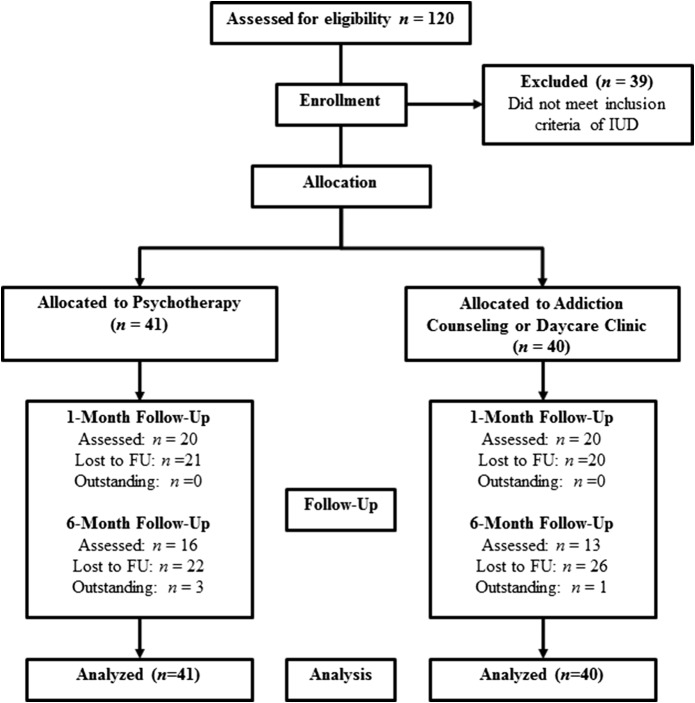
At stage two (14 days after admission), patients were informed about the diagnostic results in a counseling face-to-face appointment and were systematically referred to either addiction counseling, psychotherapy treatment, or educational counseling within the integrated health care network. The specialized treatment recommendation and referral procedure were based on the diagnostic results, following an a priori defined, hierarchical decision tree (Figure 1).
Figure 1.
Stepped-care treatment procedure
At stages three (1-month follow-up) and four (6-month follow-up), patients’ symptom courses were monitored using a coded, psychometric assessment battery.
Measures and covariates
Because IUD is very broadly defined, multiple diagnostic instruments were used covering different aspects of IUD. Specifically, Compulsive Internet Use, Online Addiction Behavior, and Problems Caused by Computer Use were measured using three questionnaires. In addition, Time Spent Online was recorded. Overall, the diagnostic instruments were highly congruent (r = .78 to .82, p < .001 in the present sample). Minor discrepancies between assessment tools resulted from different clinical cut-offs to define cases and from varying phenomenological foci. We decided to use multiple psychometric instruments and not to rely on one outcome measure because of the novelty of the syndrome and of its assessment tools.
Compulsive Internet Use
The Compulsive Internet Use Scale (CIUS; Meerkerk, Van Den Eijnden, Vermulst, & Garretsen, 2009) was used at baseline, 1-month, and 6-month follow-ups. It is a validated and widely used one-dimensional, 14-item questionnaire assessing Compulsive Internet Use on a 5-point Likert scale. It assesses five symptoms of IUD, i.e., (a) problems to control the addictive behavior, (b) withdrawal, (c) dysfunctional coping, (d) mental and behavioral preoccupation, and (e) intra- and interpersonal conflicts. A total score ≥28 is defined as clinically relevant. The instrument shows a high internal consistency (α = .89) as well as a high internal validity. We used the German version for adolescents and adults (Peukert et al., 2012).
Online Addiction Behavior
Data on Online Addiction Behavior were recorded at baseline and 6-month follow-up. Compared with the CIUS, the Scale for the Assessment of Internet and Computer Game Addiction (AICA-S; Wölfling & Müller, 2009; Wölfling, Müller, & Beutel, 2011) is a more conservative instrument for IUD diagnostics. It comprises 15 items that sum up to a total score of 27. The AICA-S shows high internal consistencies (α = .89 to .91), sensitivity (80.5%), and specificity (82.4%) in clinical samples. The AICA-S assesses demographic variables, Time Spent Online on weekdays and weekends, and frequency of different Internet activities, as well as symptoms of IUD on a 5-point Likert scale. The questionnaire allows for classifying (a) normal Internet use (total score < 7 points), (b) high-risk Internet use (total score ≥ 7 points), and (c) Internet addiction (total score ≥ 13.5 points). We used the criteria for high-risk Internet use to define clinical significance.
Problems Caused by Computer Use
The Short Questionnaire Assessing Problems Caused by Computer Use (Kurzfragebogen zu Problemen beim Computergebrauch; Petry, 2010) was used at baseline and 6-month follow-up. It is a widely used instrument in clinical settings (Schwarz, Petry, Flatau, & Beyer, 2013) and assesses Problems Caused by Computer Use using 20 items on a 4-point Likert scale. The reliability amounts to α = .88. Moderate to high validity has been shown (Schwarz et al., 2013). In contrast to the CIUS and the AICA-S, the KPC does not focus on symptoms of excessive computer use, but on its consequences, such as bad conscience and need for help, dominance of the virtual life, immersion into virtual experiences, experienced disadvantages of excessive computer use, social withdrawal, physical problems, and respect in the virtual world. In addition, the KPC assesses Time Spent Online and type of computer-related activity. A total score ≥28 is defined as clinically relevant.
Time Spent Online
Data on Time Spent Online were derived from AICA-S ratings at baseline and 6-month follow-up separately for (a) average time per day spent online on weekdays, (b) average time per day spent online on weekends, and (c) total average time per day spent online [(5 × average time weekdays + 2 × average time weekends)/7].
Comorbid psychopathology
General psychopathology was measured at baseline and 6-month follow-up using the Brief Symptom Inventory (BSI; Franke, 2000) for adult patients and the Youth Self Report 11–18 (YSR 11–18; Döpfner, Berner, & Lehmkuhl, 1994) for adolescent patients. This was complemented by the Child Behavior Checklist 4–18 (CBCL 4–18; Döpfner, Schmeck, & Berner, 1994), which was rated by caregivers. The BSI (Franke, 2000) is a short form of the Symptom Checklist-90-Revised (SCL-90-R; Franke & Derogatis, 1995) and comprises 53 items. It assesses nine symptom scales, i.e., (a) somatization, (b) obsession–compulsion, (c) interpersonal sensitivity, (d) depression, (e) anxiety, (f) hostility, (g) phobic anxiety, (h) paranoid ideation, and (i) psychoticism. Moreover, it provides three global indices, among others the Global Severity Index (GSI), which serves to measure the overall psychological distress. Clinical significance is defined as T ≥ 63. An examination of the psychometric qualities of the symptom scales has shown internal consistencies of α = .39 to .89 and a high reliability for the GSI (α = .92 to .96). The retest reliability after 1 week ranges between r = .68 and .91 and validity has been confirmed (Franke & Derogatis, 1995). The CBCL 4–18 (Döpfner, Schmeck, et al., 1994) is a parental (or other primary caregivers) report questionnaire to identify emotional, social, and behavioral problems of children aged 4–18 years. The YSR 11–18 (Döpfner, Berner, et al., 1994) is the adolescent self-report version of the CBCL 4–18. Both versions consist of 118 items and allow for the calculation of T-scores, separately normed for girls and boys, in eight different behavioral domains: (a) withdrawn, (b) somatic complaints, (c) anxious/depressed, (d) social problems, (e) thought problems, (f) attention problems, (g) delinquent behavior, and (h) aggressive behavior. The syndrome scales are assigned to three global scales: internalizing problems (G1), externalizing problems (G2), and other problems (G3) and one total score. Clinical significance is defined as T ≥ 63 on the global scales and T ≥ 70 on the syndrome scales. The reliability and validity of both screening tools have been confirmed in various studies (Döpfner, Berner, & Lehmkuhl, 1995; Remschmidt & Walter, 1990; Walter & Remschmidt, 1999).
Compliance
Compliance with the advised individualized treatment was assessed as moderator variable to predict the outcome. Patients were asked at 1-month and 6-month follow-ups if they actually utilized the health services and treatments as recommended or if alternative treatment was used (self-report). We assumed that patients were compliant if they stated that they had received treatment (i.e., made use of the offered intervention) at the recommended health service institution.
Treatment condition
The treatment procedure at the IDCT comprised three specialized treatment conditions (Figure 1; psychotherapy treatment, addiction counseling, and educational counseling) in various settings (outpatient, daycare, and inpatient). However, educational counseling was intended only for individuals, who missed diagnosis for any mental disorder (i.e., IUD as well as other mental disorder) but reported family conflicts. Consequently, patients meeting IUD diagnosis were referred to either psychotherapy treatment (if any comorbid psychopathology was present) or addiction counseling.
Research design
In this one-armed intervention study, patients received specialized treatment depending on initial diagnostics (stages one and two) and were followed up at 1 month (stage three) and at 6 months after referral (stage four).
Outcome criteria
In addition to the clinical diagnoses based on the interview at baseline, IUD was defined by clinical significance for either (a) Compulsive Internet Use, (b) Online Addiction Behavior, or (c) Problems Caused by Computer Use. Specifically, individuals were classified as IUD patients if meeting at least one the following criteria: (a) CIUS total score ≥28 or (b) KPC total score ≥28 or (c) AICA-S total score ≥7. The described criteria would receive a diagnosis for Other Habit and Impulse Disorder (F63.8) according to ICD-10 (Dilling, 2005). Due to limited resources, the diagnostic interview could not be repeated at 6-month follow-up.
Statistical methods
The main objective was the reduction of IUD symptoms over a 6-month period due to specialized treatment. Therefore, symptom changes over 6 months of (a) Compulsive Internet Use, (b) Online Addiction Behavior, (c) Problems Caused by Computer Use, and (d) Time Spent Online were chosen as primary outcome variables. Correspondingly, hierarchical linear models (HLM), that allow to model change in nested data, were used as statistical method. In this study, multiple observations were nested within individuals. Prior to specifying linear growth curve models for the change of IUD symptoms over time, primary outcome data were tested for meeting statistical assumptions. Kolmogorov–Smirnov and Shapiro–Wilk tests were used to test for normality. We log-transformed [ln(x)] Time Spent Online because the variable distribution was positively skewed. Univariate and multivariate outliers (none in Compulsive Internet Use, five in Problems caused by Computer Use, two in Online Addiction Behavior, and two in Time Spent Online) were identified and removed using boxplots and Mahalanobis distance. Missing values were not imputed. For the random-intercept-random-slope-models (Compulsive Internet Use), cases were only included if information on compliance (i.e., at least data of two measurement observations) was available. For random-intercept-fixed-slope models, we included all cases in the analysis if baseline data did not significantly differ between patients who were lost to follow-up and complete datasets. This was the case for Problems Caused by Computer Use and Online Addiction Behavior. Because baseline data in Time Spent Online significantly differed between completers and patients lost to follow-up, we only included patients with complete data sets. The final sample for HLM analyses consisted of n = 44 (Compulsive Internet Use), n = 80 (Problems Caused by Computer Use), n = 81 (Online Addiction Behavior), and n = 25 (Time Spent Online). HLM were tested in three steps. In step one, an unconditional means model (model 0) was computed describing outcome variation as a function of initial status, i.e., we included initial status as a fixed effect parameter (intercept γ00) to predict the outcome. Residual variance components were used to analyze significant systematical variation justifying further model specification. Significant residual variance components at level 1 indicate systematic variation left within-persons ( ) and thus justify the inclusion of additional parameters in step two that might explain intraindividual differences (e.g., symptom change over time caused by treatment). Significant variance components at level 2 indicate systematic variation left between-persons (
) and thus justify the inclusion of additional parameters in step two that might explain intraindividual differences (e.g., symptom change over time caused by treatment). Significant variance components at level 2 indicate systematic variation left between-persons ( ) and justify the inclusion of parameters estimating interindividual differences in step three (moderator variables). Thus, in step two, we modeled unconditional growth models (model 1) including the rate of change (slope γ10) as additional fixed effect parameter to initial status (intercept γ00) to predict the outcome. Changes in Compulsive Internet Use were fitted to a random-intercept-random-slope-model because data were available from three observations. Changes in Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online were fitted to a random-intercept-fixed-slope-model, because data were available from two observations (baseline and 6-month follow-up). In a third step, we computed conditional growth models (model 2) by including potential moderator variables to predict interindividual differences in outcome beyond the predictive value of time. To predict individual differences in symptom changes (between-persons, level 2), we computed preliminary point-biserial correlation analyses to identify moderator candidates. The variables, such as Compliance, Legal Majority, Any Comorbidity, Gaming, Depression/Anxiety/Withdrawn, Aggression, and Social Problems, were included as categorical variables (1 = present and 0 = not present) and correlated to the amount of change in Compulsive Internet Use, Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online. Change was computed by subtracting 6-month follow-up scores from baseline scores. The overall model fit for HLM models was judged by χ2 difference (the log-likelihood of the more complex model subtracted from the value of the more simple model), by the Akaike’s information criterion (AIC), and by the pseudo-R² statistic computed from the variance components (Singer & Willett, 2003).
) and justify the inclusion of parameters estimating interindividual differences in step three (moderator variables). Thus, in step two, we modeled unconditional growth models (model 1) including the rate of change (slope γ10) as additional fixed effect parameter to initial status (intercept γ00) to predict the outcome. Changes in Compulsive Internet Use were fitted to a random-intercept-random-slope-model because data were available from three observations. Changes in Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online were fitted to a random-intercept-fixed-slope-model, because data were available from two observations (baseline and 6-month follow-up). In a third step, we computed conditional growth models (model 2) by including potential moderator variables to predict interindividual differences in outcome beyond the predictive value of time. To predict individual differences in symptom changes (between-persons, level 2), we computed preliminary point-biserial correlation analyses to identify moderator candidates. The variables, such as Compliance, Legal Majority, Any Comorbidity, Gaming, Depression/Anxiety/Withdrawn, Aggression, and Social Problems, were included as categorical variables (1 = present and 0 = not present) and correlated to the amount of change in Compulsive Internet Use, Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online. Change was computed by subtracting 6-month follow-up scores from baseline scores. The overall model fit for HLM models was judged by χ2 difference (the log-likelihood of the more complex model subtracted from the value of the more simple model), by the Akaike’s information criterion (AIC), and by the pseudo-R² statistic computed from the variance components (Singer & Willett, 2003).
Differential effects of intended treatment (psychotherapy vs. addiction counseling) on the amount of outcome change (see above) were analyzed in a one-way analysis of variance including treatment condition (1 = Psychotherapy Treatment and 0 = Addiction Counseling) as independent variable and the amount of change in Compulsive Internet Use, Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online as dependent variables. The analyses were conducted using IBM SPSS version 23.
Ethics
The study was conducted in a routine care setting in collaboration with 16 clinical institutions. We obtained permission by the Institute of Psychology, University of Heidelberg to conduct the study according to the university’s ethical guidelines. Prior to admission, the investigator provided oral and written information about the diagnostics and treatment procedure of the IDCT as well as on the study including follow-up assessments. Informed written consent was obtained from all patients and from legal guardians for underage patients prior to diagnostics. The study was conducted in line with the principles of the Declaration of Helsinki.
Results
From November 2012 to September 2016, N = 120 patients underwent the diagnostics procedure at baseline (stage one). Of these, n = 81 patients (67.5%) met the criteria of IUD as defined above.
Flow of participants
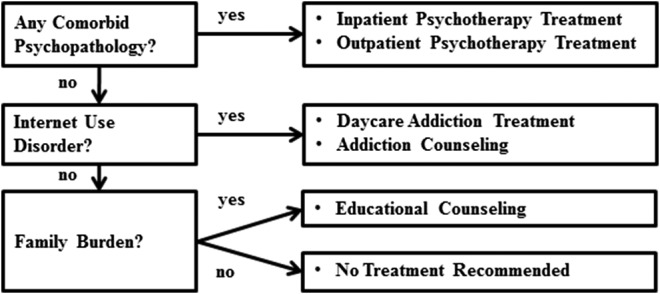
One month after diagnostics, n = 74 IUD patients (91.4%) attended stage two and were referred to specialized treatment. In total, n = 40 patients (49.4%) attended 1-month follow-up (stage three) and n = 29 patients (37.7%) attended 6-month follow-up (stage four). The flow of participants is graphed in Figure 2. By the time of data analysis, 6-month follow-ups were outstanding for four patients (4.9%). At stage three, n = 41 patients (50.6%) and at stage four, n = 48 patients (59.3%) were lost to follow-up. We controlled for effects of age on dropout rate (rpb = .06, p = .589) and on compliance (rpb = −.26, p = .099) but did not find significant associations.
Figure 2.
Flow of participants through each stage of the study
IUD symptoms in adolescents and adults
IUD patients (adolescents and adults) achieved average CIUS scores of M = 29.54 (SD = 9.03) and M = 32.69 (SD = 9.73), respectively. Most frequent symptoms were Intra- and Interpersonal Conflicts in adolescents and Dysfunctional Coping in adults. Mean Time Spent Online on weekdays was 6.03 hr/day (SD = 3.71) in adolescents and 8.16 hr/day (SD = 3.65) in adults. On weekends, mean time spent online was 8.42 hr/day (SD = 4.61) in adolescents and 9.50 hr/day (SD = 4.07) in adults. Most popular Internet activities (defined by indicating often or very often on the respective item) were playing online games (82.6%), chatting (66.3%), and searching for information (65.4%). Table 1 shows IUD symptoms in adolescents and adults at baseline. Adult IUD patients reported higher rates of sick days (M = 20.93, SD = 28.01) within the past 6 months than adolescent IUD patients (M = 10.73, SD = 12.09).
Table 1.
IUD symptoms in adolescents and adults
| Symptoms | Adolescents (n = 38) M (SD) | Adults (n = 43) M (SD) |
|---|---|---|
| Compulsive Internet Use | 29.54 (9.03) | 32.69 (9.73) |
| Reduce/stop | 2.02 (0.95) | 2.35 (0.94) |
| Withdrawal | 1.97 (0.99) | 1.57 (1.09) |
| Dysfunctional coping | 1.89 (1.11) | 2.75 (1.05) |
| Mental and behavioral preoccupation | 2.17 (0.79) | 2.30 (0.79) |
| Inter- and intrapersonal conflicts | 2.29 (0.72) | 2.33 (0.85) |
| Online Addiction Behavior | 11.00 (4.31) | 13.64 (4.39) |
| Problems Caused by Computer Use | 28.79 (6.07) | 35.51 (9.87) |
| Sick days (last 6 months) | 10.73 (12.09) | 20.93 (28.02) |
| Sick days (last month) | 3.75 (5.69) | 5.18 (6.26) |
| Time Spent Online (weekdays) | 6.03 (3.71) | 8.16 (3.65) |
| Time Spent Online (weekends) | 8.42 (4.61) | 9.50 (4.07) |
Note. Compulsive Internet Use displays the CIUS total score. The five symptom scales display mean scores per symptom scale (range: 0–4). Online Addiction Behavior is operationalized by the AICA-S and displays the total score. Problems Caused by Computer Use is measured using the KPC total score. CIUS: Compulsive Internet Use Scale; AICA-S: Scale for the Assessment of Internet and Computer Game Addiction; SD: standard deviation.
Comorbid psychopathology
Tables 2 and 3 display comorbid syndromes of IUD patients. To facilitate comparison across measures, prevalence rates for both T ≥ 63 (liberal criterion) and T ≥ 70 (conservative criterion) are displayed for all measures. In adolescent IUD patients, the most prevalent comorbid syndrome (CBCL, conservative criterion, T ≥ 70) was withdrawn (35.1%), followed by attention problems (27.0%), somatic complaints (24.3%), thought problems (24.3%), and anxious/depressed (21.6%). Aggressive behavior was reported by 18.9%, social problems by 13.5%, and delinquent behavior by 8.1% of all adolescent IUD patients. On the global scales, internalizing problems were much more prevalent (35.1%) than externalizing problems (13.5%). In total, 64.9% of all adolescent IUD patients met criteria for at least one comorbid syndrome (Table 2).
Table 2.
Comorbid psychopathology in adolescents
| Self-report (YSR), n = 37 | Parent-report (CBCL), n = 34 | |||
|---|---|---|---|---|
| CBCL/YSR scale | T ≥ 63 n (%) | T ≥ 70 n (%) | T ≥ 63 n (%) | T ≥ 70 n (%) |
| 1. Withdrawn | 16 (43.2%) | 8 (21.6%) | 27 (73.0%) | 13 (35.1%) |
| 2. Somatic complaints | 11 (29.7%) | 5 (13.5%) | 14 (37.8%) | 9 (24.3%) |
| 3. Anxious/depressed | 9 (24.3%) | 1 (2.7%) | 18 (48.6%) | 8 (21.6%) |
| 4. Social problems | 14 (37.8%) | 4 (10.8%) | 15 (40.5%) | 5 (13.5%) |
| 5. Thought problems | 2 (5.4%) | 0 (0.0%) | 16 (43.2%) | 9 (24.3%) |
| 6. Attention problems | 14 (37.8%) | 4 (10.8%) | 21 (56.8%) | 10 (27.0%) |
| 7. Delinquent behavior | 9 (24.3%) | 0 (0.0%) | 13 (35.1%) | 3 (8.1%) |
| 8. Aggressive behavior | 4 (10.8%) | 0 (0.0%) | 12 (32.4%) | 7 (18.9%) |
| G1: Internalizing problems | 10 (27.0%) | 5 (13.5%) | 26 (70.3%) | 13 (35.1%) |
| G2: Externalizing problems | 3 (8.1%) | 0 (0.0%) | 13 (35.1%) | 5 (13.5%) |
| Total score | 10 (27.0%) | 2 (5.4%) | 21 (56.8%) | 11 (29.7%) |
| Any comorbid syndrome | 26 (70.3%) | 11 (29.7%) | 33 (89.2%) | 24 (64.9%) |
Note. For a better comparison across measures, prevalence rates are displayed for both T ≥ 63 (liberal criterion) and T ≥ 70 (conservative criterion). According to the CBCL and YSR manual, clinical significance is defined as T ≥ 70 on the syndrome scales and T ≥ 63 on the global scales. CBCL: Child Behavior Checklist; YSR: Youth Self Report.
Table 3.
Comorbid psychopathology in adults
| Self-report (BSI), n = 44 | ||
|---|---|---|
| BSI scale | T ≥ 63 n (%) | T ≥ 70 n (%) |
| 1. Somatization | 11 (25.0%) | 5 (11.4%) |
| 2. Obsession–compulsion | 26 (59.1%) | 15 (34.1%) |
| 3. Interpersonal sensitivity | 23 (52.3%) | 19 (43.2%) |
| 4. Depression | 30 (68.2%) | 25 (56.8%) |
| 5. Anxiety | 14 (31.8%) | 9 (20.5%) |
| 6. Hostility | 18 (40.9%) | 7 (15.9%) |
| 7. Phobic anxiety | 15 (34.1%) | 6 (13.6%) |
| 8. Paranoid ideation | 18 (40.9%) | 11 (25.0%) |
| 9. Psychoticism | 22 (50.0%) | 15 (34.1%) |
| Global Severity Index (GSI) | 27 (61.4%) | 19 (43.2%) |
| Any comorbid syndrome | 38 (86.4%) | 31 (70.5%) |
Note. For a better comparison across measures, prevalence rates are displayed for both T ≥ 63 (liberal criterion; equivalent to BSI Test Manual) and T ≥ 70 (conservative criterion). BSI: Brief Symptom Inventory.
Adult IUD patients reported depression (56.8%) as most prevalent comorbid syndrome, followed by interpersonal sensitivity (43.2%). In total, 70.5% of adult IUD patients reported any comorbid syndrome.
Referral to specialized treatment
N = 41 patients (34.2% of total sample) met the criteria for IUD and at least one comorbid psychiatric syndrome (20.3% of all adolescents, n = 13; 50.0% of all adults, n = 28). Thus, referral to psychotherapy treatment was indicated roughly in twice as many cases in adults. N = 40 patients (33.3% of total sample) only met IUD criteria (monomorbid) and were referred to addiction counseling (37.5% of all adolescents, n = 24; 28.6% of all adults, n = 16). N = 12 patients (10% of total sample) only met criteria for any other mental disorder and were referred to psychotherapy treatment (10.9% of all adolescents, n = 7; 8.9% of all adults, n = 5). N = 27 individuals (22.5% of total sample) missed any psychiatric diagnosis but reported severe family conflicts. They were referred to educational counseling (31.3% of all adolescents, n = 20; 12.5% of all adults, n = 7).
IUD symptom change over time
Prior to computing the HLM, we tested for multicollinearity and singularity. Intraclass correlations were estimated at ρ = .36 (Compulsive Internet Use), ρ = .64 (Problems Caused by Computer Use), ρ = .03 (Online Addiction Behavior), and ρ = .13 (Time Spent Online), explaining 36%, 64%, 3%, and 13% of the variance attributed to individual differences, respectively.
First, unconditional means models (model 0) were fitted to Compulsive Internet Use (Table 4), Problems Caused by Computer Use, Online Addiction Behavior, and Time Spent Online (Table 5). Because significant residual variance at level 1 indicated further model specification for all outcome variables, unconditional growth models (model 1) were fitted including time (rate of change) as predictor. Model fit significantly improved in all models according to χ2 statistics (p < .05) and residual variance components decreased. The treatment effect over time (rate of change) explained 23% of within-person variation in Compulsive Internet Use, 53% in Online Addiction Behavior, 36% in Problems Caused by Computer Use, and 15% in Time Spent Online, as displayed by Pseudo-R Statistics  . With regard to moderator variables, Compliance was found to be positively correlated to the amount of change in Compulsive Internet Use (rpb = .39, p < .05). In total, 56.8% (25 out of 44) of IUD patients were compliant with the referred treatment. Thus, we included Compliance as moderator in the conditional growth model (model 2; Table 4). Model fit significantly improved in model 2 (p < .05) and residual variance components decreased. The amount of change in other outcome variables was not correlated to any of the moderator candidates. In other words, potential moderator variables could not be identified for Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online, and therefore the specification of conditional growth models for these outcomes was not indicated.
. With regard to moderator variables, Compliance was found to be positively correlated to the amount of change in Compulsive Internet Use (rpb = .39, p < .05). In total, 56.8% (25 out of 44) of IUD patients were compliant with the referred treatment. Thus, we included Compliance as moderator in the conditional growth model (model 2; Table 4). Model fit significantly improved in model 2 (p < .05) and residual variance components decreased. The amount of change in other outcome variables was not correlated to any of the moderator candidates. In other words, potential moderator variables could not be identified for Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online, and therefore the specification of conditional growth models for these outcomes was not indicated.
Table 4.
Parameter estimates for HLM analysis examining Compulsive Internet Use as function of time (treatment effect) moderated by compliance
| Compulsive Internet Use | ||||
|---|---|---|---|---|
| Parameter | Model 0 | Model 1 | Model 2 | |
| Fixed effects | ||||
| Initial status | Intercept (γ00) | 28.24 | 35.45 | 30.80 |
| (1.39) | (2.35) | (2.88) | ||
| p < .001 | p < .001 | p < .001 | ||
| Compliance (γ01) | 11.07 | |||
| (4.41) | ||||
| p = .016 | ||||
| Rate of change | Slope (γ10) | −3.94 | −1.84 | |
| (1.10) | (1.33) | |||
| p = .001 | ||||
| Compliance (γ11) | −5.09 | |||
| (2.06) | ||||
| p = .018 | ||||
| Variance components | ||||
| Level 1 | Within-person ( ) ) |
86.49 | 66.59 | 64.58 |
| (14.97) | (16.86) | (15.86) | ||
| p < .001 | p < .001 | p < .001 | ||
| Level 2 | Initial status ( ) ) |
49.66 | 61.31 | 35.67 |
| (18.69) | (64.90) | (57.58) | ||
| p = .008 | ||||
Rate of change ( ) ) |
5.74 | 0.58 | ||
| (13.74) | (12.13) | |||
| Covariance (σ01) | −6.97 | 4.54 | ||
| (27.43) | (24.08) | |||
| Model fit parameters | ||||
 |
.23 | .25 | ||
 |
.42 | |||
 |
.90 | |||
| −2 log-likelihood | 834.10 | 820.56 | 814.21 | |
| AIC | 840.10 | 832.56 | 830.21 | |
Note. Standard errors are displayed in parentheses. The rate of change displays the amount of change per observation.  : estimates the proportion of explained within-person variation (level 1);
: estimates the proportion of explained within-person variation (level 1);  : estimates the proportion of explained between-person variation in the intercept (level 2);
: estimates the proportion of explained between-person variation in the intercept (level 2);  : estimates the proportion of explained between-person variation in the slope (level 2); HLM: hierarchical linear models; AIC: Akaike’s information criterion.
: estimates the proportion of explained between-person variation in the slope (level 2); HLM: hierarchical linear models; AIC: Akaike’s information criterion.
Table 5.
Parameter estimates for HLM analysis in Online Addiction Behavior, Problems Caused by Computer Use, and Time Spent Online as function of time (treatment effect)
| Online Addiction Behavior | Problems Caused by Computer Use | Time Spent Online | |||||
|---|---|---|---|---|---|---|---|
| Parameter | Model 0 | Model 1 | Model 0 | Model 1 | Model 0 | Model 1 | |
| Fixed effects | |||||||
| Initial status | Intercept (γ00) | 10.81 | 18.75 | 31.91 | 37.64 | 1.72 | 2.19 |
| (0.50) | (1.11) | (1.02) | (1.75) | (0.08) | (0.21) | ||
| p < .001 | p < .001 | p < .001 | p < .001 | p < .001 | p < .001 | ||
| Rate of change | Slope (γ10) | −6.32 | −4.85 | −0.31 | |||
| (0.84) | (1.22) | (0.13) | |||||
| p < .001 | p < .001 | p = .026 | |||||
| Variance components | |||||||
| Level 1 | Within-person ( ) ) |
25.98 | 12.09 | 31.77 | 20.41 | 0.26 | 0.22 |
| (6.17) | (3.41) | (8.66) | (5.70) | (0.75) | (0.06) | ||
| p < .001 | p < .001 | p < .001 | p < .001 | p < .001 | p < .001 | ||
| Level 2 | Initial status ( ) ) |
0.67 | 6.54 | 55.41 | 63.10 | 0.04 | 0.07 |
| (5.12) | (3.79) | (14.37) | (13.46) | (0.06) | (0.06) | ||
| p < .001 | p < .001 | ||||||
| Model fit parameters | |||||||
 |
.53 | .36 | .15 | ||||
| −2 log-likelihood | 661.01 | 618.83 | 746.87 | 734.18 | 82.35 | 77.30 | |
| AIC | 667.01 | 626.83 | 752.87 | 742.18 | 88.35 | 85.30 | |
Note. Parameter estimates for Time Spent Online are log-transformed using the ln(x)-function and need to be retransformed using the ex-function for interpretation. Standard errors are displayed in parentheses. The rate of change displays the amount of change per observation.  : estimates the proportion of explained within-person variation (level 1); HLM: hierarchical linear models; AIC: Akaike’s information criterion.
: estimates the proportion of explained within-person variation (level 1); HLM: hierarchical linear models; AIC: Akaike’s information criterion.
Compulsive Internet Use was best predicted by a conditional growth model assuming that patients who were compliant with treatment were significantly more impaired at baseline (i.e., averagely 11.07 points higher on the CIUS, p = .016) than patients who ignored our treatment recommendations (M = 41.87 vs. M = 30.80). Over time, patients who were compliant with treatment significantly improved by averagely −5.09 CIUS points per observation (p = .018), i.e., −10.18 points over a 6-month period. In contrast, patients who ignored our treatment recommendations did not significantly improve.
Online Addiction Behavior was best predicted by an unconditional growth model assuming at baseline AICA-S scores of M = 18.75 and a significant reduction by −6.32 points (p < .001) over 6 months.
Problems Caused by Computer Use was best predicted by an unconditional growth model assuming initial KPC scores of M = 37.64 and a significant reduction by −4.85 (p < .001) points over a 6-month period. Significant residual variance at level 2 indicates systematic variation between persons, which however could not be explained by any potential moderator variable.
Time Spent Online was best predicted by an unconditional growth model fitted to the ln-transformed data. The slope parameter estimate of γ10 = −.31 indicates that Time Spent Online was significantly reduced over time (p = .026). Descriptive statistics show a mean reduction of Time Spent Online of 1.7 hr over 6 months (M = 7.35 hr/day at baseline to M = 5.65 hr/day at 6-month follow-up).
Effect sizes of outcome change from baseline to 6-month follow-up were estimated using Cohen’s d [(μ1 − μ2)/o’]. We found large effects for changes in Compulsive Internet Use (d = 0.83) and Online Addiction Behavior (d = 1.46), a moderate effect for Problems Caused by Computer Use (d = 0.55) and a small to moderate effect for Time Spent Online (d = 0.48).
Reliable change between baseline and 6-month follow-up was computed by the Reliable Change Index (Jacobson & Truax, 1991). On the basis of the standard deviations and the internal consistency scores from an independent representative sample, we found in Compulsive Internet Use (Gürtler et al., 2015) a reliable improvement of 60.7%, a recovery rate of 39.3%, and a reliable deterioration of 10.7%, in Online Addiction Behavior (Müller, Glaesmer, Brähler, Woelfling, & Beutel, 2014) a reliable improvement of 88.9%, a recovery rate of 59.3%, and a reliable deterioration of 3.7%. For Problems Caused by Computer Use, we used the standard deviation and the internal consistency score of an independent clinical sample (Schwarz et al., 2013) due to a missing representative sample and found a reliable improvement of 48.1%, a recovery rate of 33.3%, and a reliable deterioration of 3.7%.
Effects of Treatment Condition
The amount of change did not significantly differ between intended treatment conditions for neither Compulsive Internet Use (MPsychotherapy = 11.34, SD = 14.36, MAddiction Counseling = 5.23, SD = 9.60, t = 1.21, p = .24), nor Online Addiction Behavior (MPsychotherapy = 8.52, SD = 13.53, MAddiction Counseling = 6.05, SD = 7.24, t = 0.57, p = .57), nor Problems Caused by Computer Use (MPsychotherapy = 6.36, SD = 6.05, MAddiction Counseling = 5.19, SD = 3.08, t = 0.65, p = .53), nor Time Spent Online (MPsychotherapy = 0.89, SD = 3.12, MAddiction Counseling = 2.14, SD = 3.76, t = −0.92, p = .37). The analyses included all individuals with data at 6-month follow-up (n = 29).
Discussion
Most importantly, IUD patients who signed up at the IDCT showed significantly lower symptom severity after 6 months. Overall symptom reduction could be found for all tested outcome variables, i.e., large effects for Compulsive Internet Use and Online Addiction Behavior, a moderate effect for Problems Caused by Computer Use and a small to moderate effect for Time Spent Online. On average, IUD patients reduced the time they spent online by 1.7 hr, which is a reduction of 23%. It is encouraging that treatment of this novel syndrome at a multidisciplinary, integrated health care network results in clinically and statistically significant outcome change.
An examination of differential effects showed that symptom change in Compulsive Internet Use was primarily driven by Compliance, revealing that only patients who actually utilize the intended treatment benefit from treatment, whereas patients who refuse further treatment do not change significantly in symptom severity. In other words, IUD treatment is highly effective if patients are compliant with treatment, which, however, was only the case for 56.8%. The compliance rate was alarmingly low, although we intended to enhance accessibility by offering a low-threshold, transparent, comprehensive, and individualized approach. This was unexpected because previous findings showed that patients rated the IDCT as helpful, therapeutic relationships as positive and were satisfied with the overall concept. And, encouragingly, we could show in our previous study that treatment motivation increased over time (Lindenberg, Schoenmaekers, Szász-Janocha, Wehrmann, & Vonderlin, 2017). Nonetheless, we must assume that initial treatment motivation does not necessarily lead to sufficient compliance. This highlights a major challenge in addiction treatment and may be associated with the lack of perceived impairment of affected individuals (Petersen & Thomasius, 2010). Another important finding was that except for Compliance, none of the moderator variable candidates included in the analysis (Legal Majority, Any Comorbidity, Gaming, Depression/Anxiety/Withdrawn, Aggression, and Social Problems) predicted differential effects on outcomes. A possible explanation is that all IUD patients profited from treatment, irrespective of associated comorbidities, age, or IUD subtype. This is important because about two thirds reported at least one comorbid syndrome. It is assumable that this might be an indicator for the adequacy of our matching procedure (matching treatment condition to syndrome profile), which, however, needs to be confirmed in future studies using randomized control conditions to draw conclusions on the causes of effect. A different interpretation would be that any kind of treatment was helpful, if a patient agreed to use it. More research is needed on specific process variables that actually lead to significant change.
According to the matching procedure, patients meeting a monomorbid IUD diagnosis did not receive psychotherapy. Instead, they were referred to a less-intensive treatment in addiction counseling. It is possible that this was not meeting their expectations and might have contributed to their low compliance. There is some evidence that psychotherapy is strongly indicated in patients with severe IUD independent of any existing comorbid disorder. Thus, it needs to be explored in future research whether IUD patients without comorbidities would profit even more, if they receive psychotherapy treatment.
On the other hand, results show that all treatment conditions (high- vs. low-intensive treatment) produced effects on IUD and did not significantly differ in the amount of symptom change. Of course, this does not imply that effects of psychotherapy and addiction counseling are generally equal. Yet, it is encouraging that low-intensive counseling also produced effects in monomorbid IUD patients for three reasons. First, evidence-based, specified psychotherapy treatments, such as the cognitive-behavioral intervention developed by Wölfling et al. (2013) were not available in routine care in 2012 and thus at that time, IUD-specific treatment alternatives were not available. Second, even at present, addiction counseling institutions serve as relevant first-line assistance for patients with IUD. And third, it was our objective to distribute limited resources efficiently and to equalize benefits over patients. Future randomized efficacy studies need to investigate how limited resources can be allocated optimally in a stepped-care procedure.
It was unique that the IDCT provided individualized treatments, which were adapted to various syndrome ranges and severity levels. Following the principles of stepped-care (Haaga, 2000), multimorbid patients were assigned to high-intensive psychotherapy, and monomorbid patients with IUD pathology were assigned to low-intensive addiction counseling. The findings show that individualized therapy for IUD patients has the potential to be highly cost-effective and efficient, which is crucial in regard to limited resources. This result needs to be validated in a randomized controlled trial. It should be compelling in public health policies to ensure optimized resource allocation.
Interesting results were found concerning the distribution of comorbidities, gender, and IUD subtypes. Supporting previous findings, we found that the IUD sample showed high rates of comorbid psychopathology (Carli et al., 2013). The fact that 64.9% of adolescent and 70.5% of adult patients reported at least one comorbid syndrome, which indicates that in the majority of IUD cases, it is important to simultaneously address comorbid psychiatric disorders. It is noteworthy that treatment of comorbid psychiatric disorders is not covered by addiction counseling in Germany. Pertaining to gender and IUD subtypes, it was salient that the majority of our IUD patients (97.5%) were male and diagnosed with a gaming-subtype IUD (82.6%). This is important in light of the scientific debate whether IGD and Internet addiction display distinct disorders or subtypes of IUD. Although epidemiological studies in non-clinical samples have found that Internet addiction patients (non-gaming subtypes) show similar levels of impairment and that males and females are equally affected (Strittmatter et al., 2015), we did not find many female and non-gaming patients in our clinical data. The discrepancy between epidemiological and clinical findings may be explained by distribution properties. The spread of IUD symptoms may be roughly equal for the predictor variables Gender and Subtype around epidemiological cut-offs (less conservative, e.g., 1 SD, percentile rank of 84.2); however, extreme values of the distribution (as typically present in clinical samples, e.g., 2 SD, percentile rank of 97.5) are found predominantly in males and gamers. Another explanation is that non-gaming Internet activities, such as chatting or social networking, may be less stigmatized than video gaming. The latter is frequently associated with violence in the media and thus may be perceived as more pathological.
In sum, it has been previously shown that the IDCT achieved its aims to be easily accessible and comprehensive, to reduce burdens of help-seeking and to increase treatment motivation. In line with previous research, our findings indicate that IUD treatment within an integrated health care network leads to significant symptom reduction. However, the lack of patients’ compliance remains an unresolved challenge and calls for further research focusing on compliance enhancement. In addition, it will be vital to target adolescents at high risk for IUD onset with preventive interventions.
Limitations
The study has several limitations. First, we relied on a simple, one-armed prospective design, because randomization was not possible due to structural reasons. To validate the explorative finding that the matching procedure (matching treatment condition to syndrome profile) is appropriate, future studies will need a control condition in which patients are randomly matched to treatment conditions. Second, many patients were lost to follow-up. Although we found that most data were missing at random, this is a source of potential bias. Possibly, high rates of comorbidity might have contributed to dropout rates. Third, although the quality of assessments was highly prioritized at study planning (i.e., we chose clinical interviews and validated psychometric assessments), over the course of the study, DSM-5 criteria defining IGD and an international consensus on how to assess these criteria were published (Petry et al., 2014). Because at that time, more than 50% of our patients were already enrolled, we decided to keep the assessment battery as originally envisaged. We measured several aspects of IUD pathology; however, IGD was not assessed precisely. A methodological limitation concerns the fact that the KPC and the AICA-S were only assessed at two observations. This limits the applicability of HLM to random-intercept-fixed-slope models. Furthermore, the follow-up period of 6 months is relatively short. Therefore, predictions about long-term effects of the IDCT treatment cannot be made. Finally, we do not have any information about therapeutic processes and their effects on outcome, i.e., the number of sessions, the models of treatment, or the psychotherapy techniques used, because only referral was standardized within the IDCT but not the treatment itself. Future trials should use a randomized controlled design to assess treatment effectiveness, standardize the treatment conditions, control for comorbidities, e.g., by implementing a SCID module, and assess IGD as recommended by the international consensus.
Clinical and methodological significance of this article
This study is unique because it targets treatment outcome of IUD, a novel and highly challenging mental disorder. It assesses the effects of an innovative approach in a large patient sample. To our knowledge, integrated health care for IUD has not been investigated elsewhere.
Implications for future research
The present findings imply that it is crucial to enhance compliance, because this was the strongest predictor for therapy success. The lack of compliance is a major challenge in addiction therapy. Future trials should test whether implementation of a supportive case manager, who accompanies the therapy process using in-person, telephone-based, mail-based, or Internet-based contacts, can lead to improved compliance.
Although this study provides evidence that integrated health care is effective for IUD treatment, it will be important for future trials to identify the mechanisms, which actually led to the effective reduction of pathological behavior. An improved understanding of moderator variables associated with therapy response is indispensable for developing optimally effective treatment programs and for tailoring interventions individually to specific and associated characteristics of IUD.
Recent policies have consistently argued that addictive disorders are mental disorders and correspondingly require psychotherapeutic treatment. However, German health care sectors are rigidly fragmented and psychotherapeutic treatment of addictive behavior is still uncommon. Although we tried to overcome this separation in the IDCT, future research should investigate more systematically under which conditions addiction counseling might be sufficient (e.g., subthreshold pathology or absence of comorbidities), and when psychotherapy must be indicated.
Generally, it is important to initiate efforts targeting the challenges of IUD treatment, i.e., enhancing pathways to mental health care, increasing treatment motivation, and increasing compliance. Because approximately only 10% of individuals with IUD pathology seek treatment, preventive interventions for high-risk populations on a large-scale basis should be a public health priority to reduce the overall prevalence of IUD.
This study provides data from Germany on improving health care services for patients suffering from IUD. To generalize the findings, politicians should elaborate on the extent to which the German model is comparable with other health care systems.
Appendix: Collaborating institutions of the IDCT in alphabetical order
| 1 | AGJ Fachverband für Prävention und Rehabilitation in der Erzdiözese Freiburg e.V. Suchtberatung Heidelberg, Psychosoziale Beratungsstelle | AGJ Professional Association for Prevention and Rehabilitation in the Archdiocese Freiburg e.V., Addiction Counseling Heidelberg |
| 2 | AHG Klinik im Odenwald | AHG Clinic Odenwald |
| 3 | bwlv Fachstelle Sucht Wiesloch für Drogen-, Alkohol- und Medikamentenprobleme | bwlv Specialist Addiction Unit for Drug and Alcohol Problems Wiesloch |
| 4 | Caritasverband Mannheim e.V., Suchtberatung | Caritas Association Mannheim e.V., Addiction Counseling |
| 5 | Institut für Analytische Kinder- und Jugendlichen-Psychotherapie Heidelberg e.V. | Institute for Analytical Children’s and Adolescents’ Psychotherapy Heidelberg e.V. |
| 6 | Klinik in der Plöck der Evangelischen Stadtmission Heidelberg | Clinic in the Plöck, Protestant City Mission Heidelberg |
| 7 | Landratsamt Rhein-Neckar-Kreis, – Gesundheitsamt | Rural District Office Rhine Neckar, Public Health Department |
| 8 | Pädagogische Hochschule Heidelberg | University of Education Heidelberg |
| 9 | Psychologische Beratungsstelle für Erziehungs-, Partnerschafts- und Lebensfragen Evangelischer Kirchenbezirk Neckargemünd – Eberbach | Psychological Counseling for Educational, Partnership and Vital Problems, Protestant Church District Neckargemünd – Eberbach |
| 10 | Rhein-Neckar-Kreis | Rhine Neckar District |
| 11 | Suchtberatung der evangelischen Stadtmission Heidelberg | Addiction Counseling, Protestant City Mission Heidelberg |
| 12 | Suchtberatung Weinheim e.V. | Addiction Counseling Weinheim e.V. |
| 13 | Stadt Heidelberg | Heidelberg Local Government |
| 14 | Stadt Mannheim | Mannheim Local Government |
| 15 | Universität Heidelberg | Heidelberg University |
| 16 | Universitätsklinikum Heidelberg | University Hospital Heidelberg |
Funding Statement
Funding sources: The IDCT project has partially been funded by the Rural District Office Rhine Neckar, Public Health Department.
Authors’ contribution
KL: principle investigator, initiation of the IDCT, study concept and design, data collection, analysis and interpretation of data, statistical analysis, study supervision, and writing. CS-J: clinical diagnostics, data collection, analysis and interpretation of data, and writing. SS: writing and literature review. UW and EV: initiation and coordination of the IDCT and proof reading. All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare no conflict of interest.
References
- Alonso J. Petukhova M. Vilagut G. Chatterji S. Heeringa S., & Ustun T. B. (2011). Days out of role due to common physical and mental conditions: Results from the WHO World Mental Health surveys. Molecular Psychiatry, 16(12), 1234–1246. doi:10.1038/mp.2010.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amelung V. E. (2008). Integrierte Versorgung und medizinische Versorgungszentren: Von der Idee zur Umsetzung. Schriftenreihe des Bundesverbandes Managed Care [Integrated health care and medical care centers. From idea to implementation. Publication series of the federal association for managed care]. Berlin, Germany: Medizinische Wissenschafts Verlag Gesellschaft. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Bischof G. Bischof A. Meyer C. John U., & Rumpf H.-J. (2013). Prävalenz der Internetabhängigkeit– Diagnostik und Risikoprofile (PINTA-DIARI) [Prevalence of Internet dependency – Diagnostics and risk profiles]. Bonn, Germany: Bericht an das Bundesministerium für Gesundheit. [Google Scholar]
- Black D. W. Belsare G., & Schlosser S. (1999). Clinical features, psychiatric comorbidity, and health-related quality of life in persons reporting compulsive computer use behavior. The Journal of Clinical Psychiatry, 60(12), 839–844. doi:10.4088/JCP.v60n1206 [DOI] [PubMed] [Google Scholar]
- Carli V. Durkee T. Wasserman D. Hadlaczky G. Despalins R. Kramarz E. Wasserman C. Sarchiapone M. Hoven C. W. Brunner R., & Kaess M. (2013). The association between pathological Internet use and comorbid psychopathology: A systematic review. Psychopathology, 46(1), 1–13. doi:10.1159/000337971 [DOI] [PubMed] [Google Scholar]
- Cheng C., & Li A. Y (2014). Internet addiction prevalence and quality of (real) life: A meta-analysis of 31 nations across seven world regions. Cyberpsychology, Behavior, and Social Networking, 17(12), 755–760. doi:10.1089/cyber.2014.0317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilling H. (Ed.). (2005). Internationale Klassifikation psychischer Störungen: ICD-10 Kapitel V (F) [International Classification of Mental Diseases: ICD-10, Chapter V]. Bern, Switzerland: Huber. [Google Scholar]
- Döpfner M. Berner W., & Lehmkuhl G. (1994). Handbuch: Fragebogen für Jugendliche. Forschungsergebnisse zur deutschen Fassung der Youth Self-Report Form (YSR) der Child Behavior Checklist [Handbook: Youth Self-Report of the German version of the Child Behavior Check List]. Köln, Germany: Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD). [Google Scholar]
- Döpfner M. Berner W., & Lehmkuhl G. (1995). Reliabilität und faktorielle Validität des Youth Self-Report der Child Behavior Checklist bei einer klinischen Stichprobe [Reliability and factorial validity of the Youth Self-Report of the Child Behavior Checklist in a clinical sample]. Diagnostica, 41(3), 221–244. [PubMed] [Google Scholar]
- Döpfner M. Schmeck K., & Berner W. (1994). Elternfragebogen über das Verhalten von Kindern und Jugendlichen: Forschungsergebnisse zur deutschen Fassung der Child Behavior Checklist (CBCL) [Parent report to child and adolescent behavior: Empirical results to the German version of the Child Behavior Check List]. Köln, Germany: Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD). [Google Scholar]
- Franke G. H. (2000). Brief Symptom Inventory von L.R. Derogatis (Kurzform der SCL-90-R) [Brief Symptom Inventory by L.R. Derogatis (Short version of the SCL-90-R)] (Deutsche Version). Göttingen, Germany: Beltz Test. [Google Scholar]
- Franke G. H., & Derogatis L. R. (1995). Die Symptom-Checkliste von Derogatis: Manual. SCL-90-R [Symptom checklist by Derogatis (SCL-90): Manual]. Göttingen, Germany: Beltz Test. [Google Scholar]
- Gentile D. (2009). Pathological video-game use among youth ages 8 to 18: A national study. Psychological Science, 20(5), 594–602. doi:10.1111/j.1467-9280.2009.02340.x [DOI] [PubMed] [Google Scholar]
- Gentile D. A. Choo H. Liau A. Sim T. Li D. Fung D., & Khoo A. (2011). Pathological video game use among youths: A two-year longitudinal study. Pediatrics, 127(2), e319–e329. doi:10.1542/peds.2010-1353 [DOI] [PubMed] [Google Scholar]
- Gröne O., & Garcia-Barbero M. (2001). Integrated care: A position paper of the WHO European Office for Integrated Health Care Services. International Journal of Integrated Care, 1, e21 Retrieved from http://www.ijic.org/ [PMC free article] [PubMed] [Google Scholar]
- Gürtler D. Rumpf H.-J. Bischof A. Kastirke N. Meerkerk G.-J. John U., & Meyer C. (2015). Psychometrische Eigenschaften und Normierung der deutschen Version der Compulsive Internet Use Scale (CIUS) [Psychometric properties and norm values of the German version of the Compulsive Internet Use Scale (CIUS)]. Diagnostica, 61(4), 210–221. doi:10.1026/0012-1924/a000127 [Google Scholar]
- Haaga D. A. (2000). Introduction to the special section on stepped care models in psychotherapy. Journal of Consulting and Clinical Psychology, 68(4), 547–548. doi:10.1037/0022-006X.68.4.547 [PubMed] [Google Scholar]
- Jacobson N. S., & Truax P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. doi:10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- King D. L. Delfabbro P. H. Griffiths M. D., & Gradisar M. (2011). Assessing clinical trials of Internet addiction treatment: A systematic review and CONSORT evaluation. Clinical Psychology Review, 31(7), 1110–1116. doi:10.1016/j.cpr.2011.06.009 [DOI] [PubMed] [Google Scholar]
- Kuss D. J., & Lopez-Fernandez O. (2016). Internet addiction and problematic Internet use: A systematic review of clinical research. World Journal of Psychiatry, 6(1), 143–176. doi:10.5498/wjp.v6.i1.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindenberg K. (2012). Gestufte Prävention von Essstörungen mit YoungEs[s]prit – Wirksamkeit eines Internet-vermittelten Präventionsprogramms bei Schülern [Stepwise prevention of eating disorders with YoungEs[s]prit – Efficacy of an Internet-delivered prevention program in high-school students]. Retrieved from http://archiv.ub.uni-heidelberg.de/volltextserver/13048/
- Lindenberg K. Schoenmaekers S. Szász-Janocha C. Wehrmann U., & Vonderlin E. (2017). Verbesserung der Zugangs- und Versorgungswege für junge Menschen mit Pathologischem Internetgebrauch: Früherkennung, Frühintervention und integrierte Versorgung [Improving access to mental health care systems and specialized treatment for young people with pathological Internet use: Early detection, early intervention and integrated health care]. Sucht Aktuell, 1, 5–10. [Google Scholar]
- Meerkerk G.-J. Van Den Eijnden R. Vermulst A., & Garretsen H. (2009). The Compulsive Internet Use Scale (CIUS): Some psychometric properties. CyberPsychology & Behavior, 12(1), 1–6. doi:10.1089/cpb.2008.0181 [DOI] [PubMed] [Google Scholar]
- Moody E. J. (2001). Internet use and its relationship to loneliness. CyberPsychology & Behavior, 4(3), 393–401. doi:10.1089/109493101300210303 [DOI] [PubMed] [Google Scholar]
- Morrison C. M., & Gore H. (2010). The relationship between excessive Internet use and depression: A questionnaire-based study of 1,319 young people and adults. Psychopathology, 43(2), 121–126. doi:10.1159/000277001 [DOI] [PubMed] [Google Scholar]
- Müller K. W. Ammerschläger M. Freisleder F. J. Beutel M. E., & Wölfling K. (2012). Suchtartige Internetnutzung als komorbide Störung im jugendpsychiatrischen Setting: Prävalenz und psychopathologische Symptombelastung. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie, 40(5), 331–339. doi:10.1024/1422-4917/a000190 [DOI] [PubMed] [Google Scholar]
- Müller K. W. Glaesmer H. Brähler E. Woelfling K., & Beutel M. E. (2014). Prevalence of Internet addiction in the general population: Results from a German population-based survey. Behaviour & Information Technology, 33(7), 757–766. doi:10.1080/0144929X.2013.810778 [Google Scholar]
- O’Brien J. E. Li W. Snyder S. M., & Howard M. O. (2016). Problem Internet overuse behaviors in college students: Readiness-to-change and receptivity to treatment. Journal of Evidence-Informed Social Work, 13(4), 373–385. doi:10.1080/23761407.2015.1086713 [DOI] [PubMed] [Google Scholar]
- Petersen K. U., & Thomasius R. (2010). Beratungs- und Behandlungsangebote zum pathologischen Internetgebrauch in Deutschland [Counseling and treatment offers for pathological Internet use in Germany]. Lengerich, Germany: Pabst. [Google Scholar]
- Petry J. (2010). Dysfunktionaler und pathologischer PC- und Internet-Gebrauch [Dysfunctional and pathological use of Internet and video games]. Göttingen, Germany: Hogrefe. [Google Scholar]
- Petry N. M. Rehbein F. Gentile D. A. Lemmens J. S. Rumpf H.-J. Mossle T. Bischof G. Tao R. Fung D. S. Borges G. Auriacombe M. González Ibáñez A. Tam P., & O’Brien C. P. (2014). An international consensus for assessing Internet gaming disorder using the new DSM-5 approach. Addiction (Abingdon, England), 109(9), 1399–1406. doi:10.1111/add.12457 [DOI] [PubMed] [Google Scholar]
- Peukert P. Steffen S. ElKasmi J. Barth G. M. Meerkerk G.-J., & Batra A. (2012). Faktorielle Struktur der deutschen Version der Compulsive Internet Use Scale (CIUS) nach konfirmatorischer Faktorenanalyse [Factorial structure of the German version of the Compulsive Internet Use Scale (CIUS)]. Zeitschrift für Klinische Psychologie und Psychotherapie: Forschung und Praxis, 41(2), 101–108. doi:10.1026/1616-3443/a000137 [Google Scholar]
- Pfeiffer C. Mößle T. Kleimann M., & Rehbein F. (2007). Die PISA-Verlierer– Opfer ihres Medienkonsums. Eine Analyse auf der Basis verschiedener empirischer Untersuchungen [The PISA losers – Victims of their media consumption. An analysis on the basis of various empirical studies]. Hannover, Germany: Kriminologisches Forschungsinstitut Niedersachsen e.V. [Google Scholar]
- Rehbein F. Kleimann M., & Mößle T. (2009). Computerspielabhängigkeit im Kindes- und Jugendalter: Empirische Befunde zu Ursachen, Diagnostik und Komorbiditäten unter besonderer Berücksichtigung spielimmanenter Abhängigkeitsmerkmale (Forschungsbericht Nr. 108) [Computer game dependency in childhood and adolescence: Empirical findings on causes, diagnostics and comorbidities, with particular focus on gaming-related dependency symptoms (Research Report No. 108)]. Hannover, Germany: Kriminologisches Forschungsinstitut Niedersachsen e.V. [Google Scholar]
- Rehbein F. Kliem S. Baier D. Mößle T., & Petry N. M. (2015). Prevalence of Internet gaming disorder in German adolescents: Diagnostic contribution of the nine DSM-5 criteria in a state-wide representative sample. Addiction, 110(5), 842–851. doi:10.1111/add.12849 [DOI] [PubMed] [Google Scholar]
- Remschmidt H., & Walter R. (1990). Psychische Auffälligkeiten bei Schulkindern: Eine epidemiologische Untersuchung. Mit deutschen Normen für die Child Behavior Checklist [Psychopathological symptoms in school children: An epidemiological study using German norms for the Child Behavior Checklist]. Göttingen, Germany: Hogrefe. [Google Scholar]
- Rumpf H. J. Meyer C., & John U. (2011). Prävalenz der Internetabhängigkeit (PINTA) [Prevalence of Internet dependency (PINTA)]. Berlin, Germany: Bundesministerium für Gesundheit. [Google Scholar]
- Schwarz S. Petry J. Flatau M., & Beyer L. (2013). Vergleich der Testgütekriterien des KPC und der CIUS [Comparing psychometric properties of KPC and CIUS]. SuchtAktuell, 2013(3), 24–27. [Google Scholar]
- Singer J. D., & Willett J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, UK: Oxford University Press. [Google Scholar]
- Strittmatter E. Kaess M. Parzer P. Fischer G. Carli V. Hoven C. W. Wasserman C. Sarchiapone M. Durkee T. Apter A. Bobes J. Brunner R. Cosman D. Sisask M. Värnik P., & Wasserman D. (2015). Pathological Internet use among adolescents: Comparing gamers and non-gamers. Psychiatry Research, 228(1), 128–135. doi:10.1016/j.psychres.2015.04.029 [DOI] [PubMed] [Google Scholar]
- Walter R., & Remschmidt H. (1999). Untersuchungen zur Reliabilität, Validität und Faktorenstruktur einer deutschsprachigen Version der Child Behavior Checklist [Studies on the reliability, validity, and factor structure of a German version of the Child Behavior Checklist]. Zeitschrift für Klinische Psychologie und Psychotherapie, 28(3), 177–184. doi:10.1026//0084-5345.28.3.177 [Google Scholar]
- Winkler A. Dörsing B. Rief W. Shen Y., & Glombiewski J. A. (2013). Treatment of Internet addiction: A meta-analysis. Clinical Psychology Review, 33(2), 317–329. doi:10.1016/j.cpr.2012.12.005 [DOI] [PubMed] [Google Scholar]
- Wölfling K. Jo C. Bengesser I. Beutel M. E., & Müller K. W. (2013). Computerspiel- und Internetsucht: Ein kognitiv-behaviorales Behandlungsmanual. Störungsspezifische Psychotherapie [Videogame and Internet dependency: A cognitive-behavioral treatment manual]. Stuttgart, Germany: Kohlhammer. [Google Scholar]
- Wölfling K., & Müller K. (2009). Computerspielsucht [Internet dependency]. In Batthyany D., Pritz A. (Eds.), Rausch ohne Drogen – Substanzungebundene Süchte [Intoxication without drugs: Substance-free addictions] (pp. 291–307). New York, NY/Wien, Germany: Springer. [Google Scholar]
- Wölfling K. Müller K. W., & Beutel M. (2011). Reliabilität und Validität der Skala zum Computerspielverhalten (CSV-S) [Reliability and validity of the scale for the assessment of pathological computer-gaming (CSV-S)]. Psychotherapie Psychosomatik Medizinische Psychologie, 61(5), 216–224. doi:10.1055/s-0030-1263145 [DOI] [PubMed] [Google Scholar]
- Young K. S. (1998). Internet addiction: The emergence of a new clinical disorder. CyberPsychology & Behavior, 1(3), 237–244. doi:10.1089/cpb.1998.1.237 [Google Scholar]