Abstract
Despite patients referred to home health having diverse and complex needs, it is unknown how nurses develop personalized visit plans. In this qualitative descriptive study, we interviewed 26 nurses from three agencies about their decision-making process to determine visit intensity and analyzed data using directed content analysis. Following a multifactorial assessment of the patient, nurses relied on their experience and their agency’s protocols to develop the personalized visit plan. They revised the plan based on changes in the patient’s clinical condition, engagement, and caregiver availability. Findings suggest strategies to improve visit planning and positively influence outcomes of home health patients.
Keywords: visit intensity, nurse decision-making, socio-ecological model, qualitative descriptive, directed content analysis, home health care, patient care planning, needs assessment, clinical pathways
Background
The demand for home health (HH) care services is increasing due to the growing aging population, rising rates of chronic conditions, and advances in the provision of health-related services in patients’ homes. In 2014, there were 12,461 HH agencies serving 3.4 million Medicare beneficiaries at a cost of 17.9 billion U.S. dollars (Medicare Payment Advisory Commission [MedPAC], 2016). Patients receiving HH services have complex needs (Murtaugh et al., 2009) and require different levels of care and attention. Visit intensity specifically refers to the number and frequency of visits that patients receive throughout the 60-day care episode (O’Connor et al., 2014). While there is some available data on the impact of visit intensity on outcomes for HH care in the United States (O’Connor, Hanlon, Naylor, & Bowles, 2015; O’Connor et al., 2014), empirical evidence about nurse decision-making regarding visit intensity planning does not exist. Despite this, nurses are required to make such decisions daily for newly admitted patients, which annually equates to 6.6 million decisions (MedPAC, 2016). Therefore, we sought to answer the following question: How do HH nurses decide on visit intensity and what factors influence these decisions?
Visit Planning and Patient Outcomes
The Centers for Medicare and Medicaid Services (CMS) mandates that patients admitted to HH care receive an initial assessment within 48 hours of referral or within 48 hours of their return home (CMS, 2015). However, there are no requirements or recommendations regarding the timing, number, and frequency of subsequent visits. Half of unplanned rehospitalizations among HH patients occur within the first two weeks following admission to HH care (Rosati & Huang, 2007), when patients are at greatest risk for poor health outcomes (Krumholz, 2013). This highlights the critical role of HH nurses who provide personalized care and are attentive to early cues of health decline while a hospital admission is avoidable.
Providing more visits in the first few weeks of the HH episode allows nurses to maximize teaching opportunities, provide surveillance, and identify issues early on, thus contributing to decreased rates of rehospitalization (Rogers, Perlic, & Madigan, 2007). This practice has been referred to in the literature as frontloading, recently defined as providing “at least one nursing visit on the day of or day after hospital discharge and at least three nursing visits (including the first visit) in the first posthospital week” (Murtaugh et al., 2017, p. 5). Although initial intensive assessment is key for early interventions, maintaining a steady pattern of visits can also influence patient outcomes. The total number of skilled nursing visits in a care episode and the HH length of stay also influence the likelihood of hospital readmissions (O'Connor et al., 2015). Therefore, nurses can assist in reducing hospital readmission by providing an adequate number and frequency of skilled nursing visits, otherwise known as visit intensity.
Decision-Making and Nursing Practice
Decision-making is a complex process that involves analysis and intuition, which are inherently connected (Banning, 2008). Nurses routinely use these interrelated patterns of reasoning to make decisions that influence patient care and outcomes (Tanner, 2006). Previous research highlights the importance of knowing the patient and family in order to make appropriate clinical decisions (Egan et al., 2009; Smith Higuchi, Christensen, & Terpstra, 2002; Stajduhar et al., 2011). Decision-making also relies on personal values and professional scope of practice (Gillespie & Paterson, 2009), as well as prior experiences with similar situations, which facilitates the evaluation and weighing of potential decisional alternatives (Tversky & Kahneman, 1974). HH organizational factors such as the level of support from managers and peers influence how nurses engage in decision-making and care delivery (Ellenbecker, Boylan, & Samia, 2006; Flynn, 2007; Tullai-McGuinness, Riggs, & Farag, 2011). Also, HH policy and payment factors influence care delivery. Since the implementation of the prospective payment system in 2000, the number of visits per HH user over a yearlong period was reduced by more than half (MedPAC, 2017). However, it is unclear to what extent this drop in visits is related to the interplay between nurses’ autonomy in developing visit plans and other agency and policy factors that may influence their decisions.
Conceptual Framework
To guide this study, a model of decision-making (Johansen & O’Brien, 2016) was adapted and superimposed with a socio-ecological lens (McLeroy, Bibeau, Steckler, & Glanz, 1988) that illustrates the contextual factors influencing visit plan development and implementation (see Figure 1). Decision-making is a cyclical and recursive process whereby decisions are reevaluated to be reaffirmed or replaced with other options by engaging in a new decision-making process (Johansen & O’Brien, 2016). The addition of a socio-ecological lens provides the ability to account for multidimensional interactions that are nonlinear and/or reciprocal among several factors—micro-level (nurse and patient), meso-level (agency), and macro-level (policy/payer) —that influence the processes of developing and implementing a visit plan.
Figure 1. Initial Model of Nurse Decision-Making Regarding Visit Intensity Planning in Home Health Care.
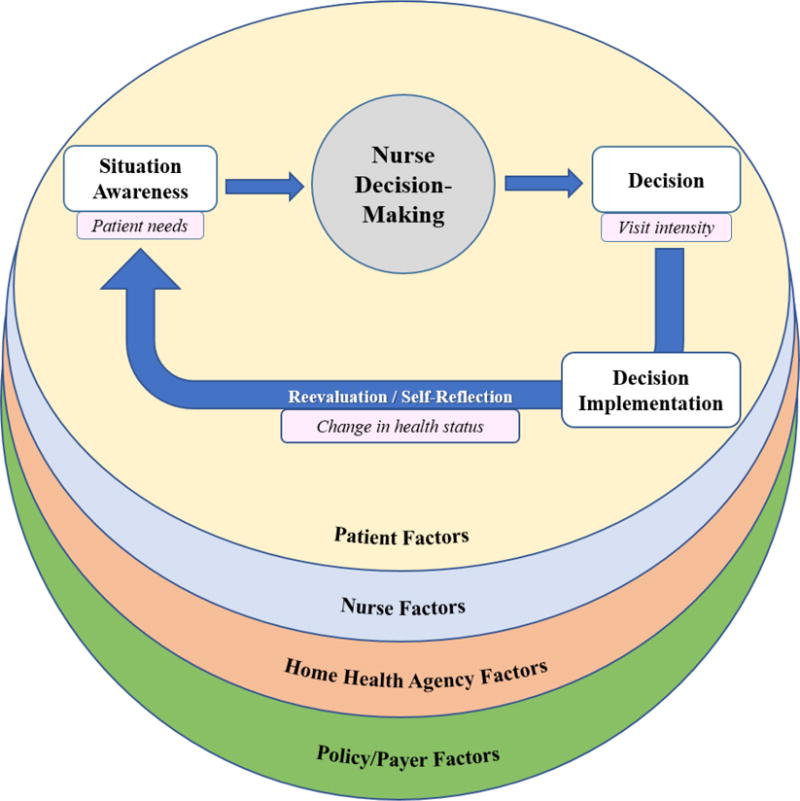
Adapted from “Model of Decision Making” by Johansen and O’Brien (2016) [Copyright 2015 by John Wiley & Sons] with a superimposed socio-ecological lens (McLeroy et al., 1988).
Purpose
Despite the use of a standardized assessment tool to assess patient needs upon admission to HH care, there is no empirical evidence regarding how nurses determine visit intensity based on their assessment. To address this gap, this study explored HH nurses’ decision-making regarding nursing visit intensity planning. Specifically, we aimed to describe the decision-making process and influencing factors through which nurses determine visit intensity and revise the visit plan over the HH episode for newly admitted patients.
Methods
Study Design
A qualitative descriptive design was used in this study to describe the complex decision-making process embedded in nursing practice (Sandelowski, 2000). We used data from semi-structured interviews with HH nurses and conducted a directed content analysis guided by an adapted decision-making model (Figure 1). This study was reviewed and approved by each participating site’s institutional review board (IRB).
Sample and Recruitment Procedures
We recruited a convenience sample of visiting nurses from three large urban agencies located in three Mid-Atlantic States. We sought nurses with at least two years of experience in HH care, a current Registered Nurse license, and a full-time employment status at one of the participating agencies. An e-mail announcement that included the study purpose, eligibility criteria, and the first author’s contact information was sent to potentially eligible participants by nurse managers or research coordinators at each site. Nurses expressing interest were further screened over the phone to verify eligibility and continued interest in the study. In addition, these nurse participants were asked to present the study to potentially interested colleagues. This snowball sampling approach was used to ensure an adequate number of participants until achieving data saturation (Sandelowski, 1995). Following initial recruitment and based on the preliminary findings, the sampling frame was expanded beyond visiting nurses to include nurse managers and nurses holding other administrative positions who served critical roles related to visit intensity planning. Nurses were offered a $50 gift card as compensation for their time participating in the study.
Data Collection
The participants completed an online survey about their demographic and professional information, then participated in a semi-structured interview either in-person or via a web-based video conferencing tool approved by the IRB. The first author conducted in-person interviews in private rooms at the study sites and asked nurses participating in video interviews to use a private room to avoid distractions and maintain confidentiality. The first author used a semi-structured interview guide consisting of open-ended questions and probes developed based on the categories of the conceptual framework (see Table 1). Before data collection, the first author pre-tested the interview guide with an experienced HH nurse to determine if it was suitable to obtain rich data that answered the study purpose (Elo et al., 2014). The interview guide was revised as new patterns emerged in the concurrent process of data collection and analysis. Interviews continued until analysis failed to yield new information, indicating data saturation (Sandelowski, 1995). Interviews lasted an average of 45 minutes, were digitally recorded, and transcribed verbatim. The first author verified all transcripts against the audio files for accuracy and replaced participant identifiers with pseudonyms to protect their confidentiality.
Table 1.
Exemplar Questions and Probes from the Semi-Structured Interview Guide
| Category | Question | Probe |
|---|---|---|
| Visit plan development | Guide me through the process you use to develop the visit plan. |
|
| What makes it easy or difficult for you to choose how many visits a patient should receive? |
|
|
| Visit plan reevaluation | What situations lead you to change your visit intensity? |
|
| Patient-level factors | What patient factors do you consider when determining visit intensity? |
|
| Nurse-level factors | How does your experience in home health influence your thought process about determining visit intensity? |
|
| Agency-level factors | How does your home health agency influence your decision regarding visit intensity? |
|
If nurses referred to agency protocols:
| ||
| Policy/Payer-level factors | How do different payers influence your visit plan? |
|
Data Analysis
Transcribed interviews were analyzed using directed content analysis (Graneheim & Lundman, 2004; Hsieh & Shannon, 2005) via Atlas.ti 7 (Berlin, Germany). Directed content analysis allows for a structured approach and occurs through coding, data reduction, and identification of findings in relation to predetermined categories; the main concepts of the model served as the predetermined categories. The list and definitions of predetermined categories are presented in Table 2. After obtaining a sense of the data by reading and immersing in all the transcripts, the first six interviews (two from each agency) were reviewed line-by-line and coded to create the preliminary expanded list of codes. Then, first-level codes were collapsed according to commonalities and assessed for fit with the categories derived from the conceptual framework. All codes were aligned with the predetermined categories and no emerging categories were identified. As part of the iterative analysis process, the initial predetermined categories were substantiated and subcategories were created based on the data until redundancy was reached. The two coders (EI, KBH) met regularly to discuss the analysis process and reach agreement regarding data interpretation. All team members reviewed and approved the final codes and findings.
Table 2.
Categories Derived from the Conceptual Framework
| Nurse Decision-Making Model | |
|---|---|
| Category | Operational Definition* |
| Nurse decision-making | Using intuitive and/or analytical strategies. |
| Situation awareness | Assessing the patient and becoming aware of their needs. |
| Decision | Visit plan (or visit patterns), including the number and frequency of skilled nursing visits. |
| Decision implementation** | Steps taken by the nurse to follow the initial visit plan. |
| Reevaluation/Self-reflection | Reevaluating the visit plan during the episode based on unanticipated changes. |
| Socio-Ecological Lens | |
| Category | Operational Definition* |
| Patient-level factors | Information-based variables or sources of information used to make decisions such as pre-encounter data and patient assessment data. |
| Nurse-level factors | Knowing the self, including personal values and professional scope of practice. Prior experiences with similar situations. Knowledge and training necessary to evaluate the situation and weigh potential alternatives. |
| Agency-level factors | Culture of practice and work environment, including support from managers and colleagues, adequate staffing, agency policies, and degree of collaborative practice. |
| Policy/Payer-level factors | Home health regulations and payment system. |
Notes:
The review of the literature led to initial operational definitions for these categories.
Decision implementation is not discussed in this manuscript.
Rigor
Methodological rigor of this study was ensured through the following strategies: keeping a reflexive journal and an audit trail to preserve the integrity of ongoing data collection and analysis (Koch, 2006; Milne & Oberle, 2005), engaging in peer debriefing about methodological concerns and alternative interpretation of the data (Abboud et al., 2017; Graneheim & Lundman, 2004), and establishing reliability of coding by having a second coder (KBH) for a subset of interviews (n = 3) and resolving discrepancies through consensus (Morse, 2015).
Results
Twenty-six nurses participated in the study, including 20 visiting nurses, two Medicare case managers, and four nurse managers (see Table 3). Medicare case managers were specific to Agency 2 and responsible for reviewing nurses’ documentation and evaluating whether it justified the need for services requested. The participant sample was largely White (46.2%), female (92.3%), with a mean age of 47 years (± 8.7 years, range 30-65 years), and most had a Bachelor’s degree in Nursing (76.9%). On average, participants had practiced as registered nurses for 17 (± 10.2) years, with most of their professional experience (12 years ± 9) in HH.
Table 3.
Demographic and Professional Characteristics
| Variable | All Participating Nurses (n = 26) Mean ± SD or n (%) |
Visiting Nurses Only (n = 20) Mean ± SD or n (%) |
|---|---|---|
| Age (years) | 47.2 ± 8.7 | 45.5 ± 8.6 |
| Gender | ||
| Male | 2 (7.7%) | |
| Female | 24 (92.3%) | |
| Race | ||
| Asian | 3 (11.5%) | |
| Black or African American | 9 (34.6%) | |
| White | 12 (46.2%) | |
| Other | 2 (7.7%) | |
| Ethnicity | ||
| Hispanic or Latino | 2 (7.7%) | |
| Not Hispanic or Latino | 20 (76.9%) | |
| Missing response | 4 (15.4%) | |
| Educational background (highest level completed) | ||
| Diploma in Nursing | 2 (7.7%) | |
| Associate’s degree in Nursing | 3 (11.5%) | |
| Bachelor's degree in Nursing | 20 (76.9%) | |
| Master’s degree | 1 (3.8%) | |
| Experience as a Registered Nurse (years) | 17.4 ± 10.2 | 14.8 ± 8.5 |
| Experience as a Registered Nurse in home health care (years) | 12.2 ± 9.0 | 9.0 ± 5.5 |
| Experience at current home health agency (years) | 8.5 ± 5.4 | 7.8 ± 4.6 |
| Home visits per day (patients) | ||
| Total (n = 20) | 6.7 ± 1.0 | |
| Agency 1 (n = 7) | 5.9 ± 0.4 | |
| Agency 2 (n = 6) | 6.5 ± 0.8 | |
| Agency 3 (n = 7) | 7.6 ± 0.8 | |
| New admissions per week (patients) | ||
| Total (n = 20) | 5.5 ± 1.8 | |
| Agency 1 (n = 7) | 5.3 ± 1.8 | |
| Agency 2 (n = 6) | 4.5 ± 1.0 | |
| Agency 3 (n = 7) | 6.4 ± 2.0 |
Nurse decision-making regarding visit intensity planning is an overarching process that happened in a cyclical pattern throughout the episode of care. When nurses identified a new situation, they engaged in a new decision-making process to revise the initial plan. The study participants described the multilevel factors influencing their visit plan decisions. From a socio-ecological perspective, these contextual factors ranged from micro-level (patient and nurse) factors, to agency-level factors, and policy/payer-level factors.
Visit Plan Development
Nurses reviewed the referral information to paint a preliminary picture of the patient and prepare for the first visit, but made final decisions after assessing the patient in person. The referral information was often incomplete and inaccurate, missing a description of the patient’s health behaviors, treatment adherence, health literacy, and socioeconomic concerns. Nurses also encountered discordant findings where the referral information did not match their assessment findings; the patient’s condition was either better or worse than the description on the referral. One nurse said regarding the patient’s assessment: “It may look very simple on paper, and when you get there, they're disheveled, they have no idea what they're doing. So they need a couple extra visits.” Nurses then engaged in a multidimensional analysis that depended on multiple factors. Considering specific patient characteristics and needs, relying on previous experience, and referring to agency protocols and HH policies, nurses wrote visit orders for nine weeks while trending down their frequency because, as one said, “it’s supposed to look like there’s a plan. Eventually the patient gets better, and you pull out.”
Patient-Level Factors
During the initial visit, nurses completed a thorough patient assessment, verified the referral information, gathered additional patient information, and built rapport with patients and caregivers. Nurses sometimes faced challenges when evaluating patient honesty at the start of care in order to develop their visit plan and set common goals for the episode of care. Patients did not always express genuine readiness to engage with the nurse, as one of the nurses observed:
If I ask direct questions, that’ll help me understand how far we need to go, how long it’s going to take. But sometimes patients aren’t honest, so they’ll say, “Yeah, yeah.” Then you find out in three visits that they were just talking, and didn’t do anything. You don’t always get all the information you want up front.
Nurses considered specific characteristics based on the assessment of the patient’s clinical status, level of care participation, and social status. All nurses completed a comprehensive clinical assessment to evaluate patients’ symptoms, wounds, and functional ability. If the patient was stable and did not receive specific treatments, nurses started with a baseline of two visits per week, as one nurse explained: “As long as you don’t see anything on that initial assessment and they’re stable, they should not be getting more than two visits in a week.” Patients who had complicated wounds or an unstable clinical status, such as increased pain or labored breathing, often received more intensive visits for frequent monitoring and interventions. Nurses differentiated between chronic (wounds, heart failure) and acute (orthopedic, surgical) conditions, requiring different visit intensity. For instance, one of the nurses said that patients recovering from an orthopedic surgery “need a couple visits to teach pain management and signs and symptoms of infection, [and] make sure they're taking their medications. Then therapy usually takes over.” Whereas for patients who had a recent heart failure exacerbation, most nurses would “frontload” by providing at least two to three visits during the first two weeks to avoid hospital readmissions. Moreover, if patients were prescribed injections or specific treatments such as wound care or a PleurX catheter drain, visit patterns were often derived from the physician’s order. For instance, nurses visited patients on wound vacuum therapy three times per week unless otherwise indicated by the referring physician. In some cases, nurses altered the physician’s order based on their assessment of the wound for drainage and signs of infection. If the patient needed daily visits, wound care nurses were often consulted to recommend an alternative treatment to decrease visit frequency. Besides completing a thorough physical assessment, nurses identified patients who were prescribed new or “high alert” medications such as anticoagulants, insulin, and narcotics to provide them with increased visit intensity for adequate monitoring and teaching reinforcement.
Nurses assessed the patient’s level of knowledge, adherence, and engagement. Nurses faced difficulty developing visit plans when patients were not engaged to set and achieve certain goals, as one nurse explained:
Having a patient who participates and is able to comprehend your teaching, you reach your goal quicker and decrease your visits quicker. But if a patient is not listening to you or can’t understand, it does make it more difficult, so they may require more visits—a lot a reinforcement.
A few nurses described how they evaluated their patient’s cognitive ability and alertness because it influenced the extent of patient engagement in the plan of care and the level of support they needed, such as reminders to take their medications.
Lastly, nurses considered social factors that influence the frequency of their visits, such as patient health literacy and caregiver support. If a caregiver was available, capable, and willing to participate, the nurse visited the patient frequently for the first couple of weeks to teach the caregiver and provide professional support.
Nurse-Level Factors
Nurse-level factors included the skills developed through clinical experience in HH and elsewhere. Over time, nurses encountered diverse scenarios and learned to practice as autonomous decision makers. They refined their critical thinking and organizational skills, which enabled them to better identify those who required more attention through increased visit intensity. One nurse said:
You know from experience patients that tend to be unsteady. You get a feel for that the first visit and say, ‘I’ve got to go back and check on her, I’m not sure she’s going take those meds like I taught her. I might need to reinforce that again tomorrow.’
In contrast, nurses who are new to HH faced difficulty when predicting how many visits a patient will need, as one nurse commented:
When you start in home health, you’re much more nervous and tend to schedule a lot more because you’re like, I need to see them three, four times a week because God knows what’ll happen when I’m not there, not realizing that 23 hours out of the 24, you aren’t there.
Agency-Level Factors
Agencies had varying levels of oversight in terms of meeting with managers, following agency-specific protocols, and reviewing nurses’ documentation. Managers were in continuous contact with nurses to support them in their decisions through individual and team meetings. Team meetings served as a learning experience where nurses received feedback about the plan of care from their colleagues who had previously cared for the same or a similar patient. Moreover, agency-specific protocols offered standardization to visit planning and guided nurses’ decisions. In two of the participating agencies, committees developed visit intensity protocols based on a score derived from the documentation at the initial visit. Nurses shared the importance of complementing protocol recommendations with their clinical judgment to finalize visit orders. One nurse described:
[The Outcome and Assessment Information Set (OASIS) assessment] doesn’t see the depth of what we see. Unfortunately, it’s very clean cut, either black or white. And we see all the grey areas. So we have to supplement what we see with what the OASIS gives.
Examples of factors that protocols overlooked were mental health assessment, ability and willingness of the patient to be engaged in the plan of care, and psychosocial factors such as emotional distress, socioeconomic status, literacy level, family dynamics, and willingness of available caregivers to participate in the care plan. Additionally, protocols never indicated daily visits for wound care and did not account for changes that happened during the episode. In cases of discrepancies between visit patterns and nurses’ documentation of patient need, some nurse managers reached out to visiting nurses and made suggestions to add or remove visits.
Policy/Payer-Level Factors
Nurses faced challenges related to HH policy constraints. They were required to justify patient needs, as exemplified in one nurse’s remarks: “If there’s no true justification, if it’s just a gut feeling, Medicare doesn’t pay for gut feelings. There’s got to be a skilled reason.” The changes in the CMS rules and regulations led nurses to condense the care that they provided and reduce the number of visits, as one nurse explained, “It’s a lot more discipline. Every visit has to stand alone and have a skilled intervention focused towards the primary condition.” Some older and more experienced nurses embraced these changes to make every visit count, whereas others were still struggling. Some had recognized that the current HH environment was no longer a “doing environment,” but rather, a “teaching environment,” where nurses assist patients and caregivers to reach their maximum potential. One nurse shared: “As a visiting nurse, my job is to get you to fire me. I’m a short-term nurse. I’m here if you need me, but my job is to instill in you the tools to take care of yourself.” However, others had developed habits of visiting patients more frequently just to “check on them” and found difficulty realizing that insurance companies were regulating the number of visits most of the time. The latter often struggled to justify the need for their visits. Many nurses spoke of the flexibility of developing visit plans for patients on Medicare, because they do not require prior authorization. When caring for patients on managed care, some nurses described working harder to reach their goals with fewer visits. In cases where the private insurer approved only a specific number of visits for the whole episode, nurses spread their visits out to ensure that patients were still monitored until they were ready for discharge.
Visit Plan Reevaluation
Nurses described the start of care visit as a snapshot of the episode and often faced uncertainty anticipating changes following that initial visit. They perceived visit planning as an ongoing process in which they adjusted their initial plan based on unanticipated changes. These changes were related to the patient’s clinical status, level of engagement, or caregivers’ availability. Nurses relied on their experience to communicate with the responsible physician any changes in patients’ conditions and documented their justification for changing visit patterns. They encountered challenges when physicians were unavailable and did not respond in a timely manner to their requests.
Patient-Level Factors
Nurses altered their visit intensity according to the patient’s changing clinical needs, such as having a better or worse condition, as illustrated in this nurse’s explanation: “if they have an increase in edema, increased weight gain, increased shortness of breath—they need adjustments in their Lasix dose, and I might add a visit to that week to check on them.” Nurses also added visits when new problems emerged during the episode of care, such as sustaining a fall, getting a wound infection, or a new pressure ulcer. Some nurses needed to increase the intensity of visits depending on the patient’s level of knowledge, adherence, and engagement in order to reach certain goals before discharge. One nurse explained, “She was [seen] twice [every week], and we moved her up to three times because she wasn’t taking her Lasix the way she was supposed to. So she started swelling up.” On the other hand, nurses gradually decreased their visit frequency when patients were collaborating with the nurse, responsive to the teaching, and meeting their goals. In some cases, nurses discussed how they decreased their visit frequency when a patient refused to be seen according to the nurse’s plan. Lastly, nurses added visits if caregivers were no longer available or realized that they could not provide adequate care for their loved one, especially in cases of wound care.
Nurse- and Agency-Level Factors
Nurses described visit planning as a continuous process that evolved with any changes in the patient’s status. Therefore, agency-specific protocols served as a starting point and nurses made changes to the visit plan during the episode of care based on their clinical judgment. Depending on the agency’s practice, some discussed those changes with their managers or other clinicians. Other agency practices such as telemonitoring and telephone call visits influenced changes in visit intensity. Nurses employed by two of the participating agencies mentioned telemonitoring as a strategy to engage patients with heart failure or uncontrolled hypertension in their care. During the episode, nurses felt comfortable decreasing their visit frequency when stable patients receiving telemonitoring demonstrated appropriate use of the equipment on a daily basis. One nurse explained:
If we’re seeing them three times a week, we would decrease it by one. So the telehealth will take one visit per week. If it’s twice a week, we’ll now see them once a week. But we never leave telehealth and not see them… Telehealth doesn’t replace the nurse. I still want to make sure that they understand the education component.
In two agencies, nurses added telephone call visits, which consisted of a systematic and documented conversation to reinforce teaching, follow up with stable patients, and reassure patients and families. Nurses provided an additional home visit if they identified a change in the patient’s status over the phone.
Policy/Payer-Level Factors
Nurses emphasized the importance of documenting their justification for any change in visit patterns, as exemplified in this nurse’s remark: “You’re not going to get anything if you don’t back it up with your documentation.” Nurses continuously evaluated their patient’s homebound status and skilled needs to confirm their HH eligibility. One nurse said, “If they’re not homebound, you’re supposed to discharge them or [the agency] won’t get paid.” In these cases, nurses informed patients that their skilled needs should be addressed elsewhere. Moreover, if a patient no longer had a skilled nursing need, the physical therapist coordinated the case and reactivated skilled nursing services if the patient’s condition deteriorated.
Discussion
In this qualitative descriptive study guided by an adapted decision-making model, we explored how HH nurses develop and revise visit plans for newly admitted patients. Nurse decision-making is a recurring and multifactorial process based on patient, nurse, agency, and policy/payer factors. At the start of care, nurses considered specific patient characteristics, referred to their agency protocols, and complemented them with their experience and clinical judgment. During the episode, nurses revised the initial plan based on changes in the patient’s condition, level of engagement, and caregiver availability. Nurses communicated with the responsible physician, and in some cases, with their managers, before responding to these changes. Nurses also highlighted the importance of sharing accurate patient information and coordinating services across care settings. Based on the findings, we validated the concepts of the initial model and refined it by reorganizing the relationship between “nurse decision-making” and other concepts of the model (Figure 2). In the final model, nurse decision-making was illustrated as an overarching concept that encompasses processes of visit plan development, implementation, and reevaluation.
Figure 2. Model of Nurse Decision-Making Regarding Visit Intensity Planning in Home Health Care.
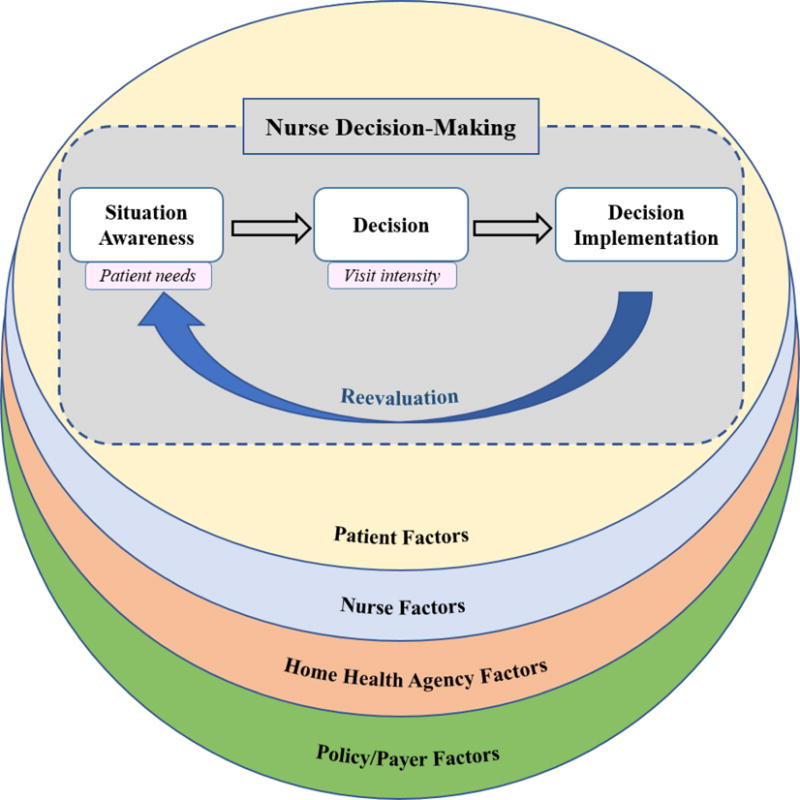
Revised based on the study findings.
Consistent with previous research (Stajduhar et al., 2011), nurses’ decisions were based on a multifactorial assessment of patient and caregiver needs. A patient’s physical status influenced visit intensity. Other researchers established that patients with open wounds receive more nurse visits per week compared to those with other needs (Yeboah-Korang, Kleppinger, & Fortinsky, 2011). Few participants mentioned assessing the patient’s cognitive ability to evaluate the need for additional visits and reinforcement. Productivity requirements and the lack of adequate training and confidence are potential explanations of this gap in cognitive assessments of patients (Burns & Neville, 2016; Cliff & McGraw, 2016). Nurses may have overlooked cognitive assessment because they were working within the constraints of HH policy and may have been unprepared to address the patient’s cognitive limitations within an episode focused on other health priorities. Mental health assessment is also beneficial to identify those with depressive symptoms who are not ready or able to be engaged in the plan of care. There is evidence of lower risk of hospitalizations when integrating depression care management into routine HH nursing care for patients screening positive for depression (Bruce, Lohman, Greenberg, Bao, & Raue, 2016).
Patient engagement was another factor that influenced nurses’ decisions. It has emerged as a critical concept in recent research designed to promote patient participation in healthcare activities (Gruman et al., 2010). Nurses participating in this study provided less frequent visits to patients actively involved in the plan of care, which supports the existing literature on lower rates of healthcare utilization in highly activated patients (Hibbard & Greene, 2013). HH nurses are perfectly situated to promote patient engagement and foster collaborative goal setting given the trusting relationship they build with patients (Leslie & Lonneman, 2016). However, it is unknown how nurses can do so, and what strategies can be extrapolated from other community-based interventions.
Besides assisting patients to participate in their plan of care and reach their maximum potential, the nurse participants in this study developed visit plans to contribute to lower rehospitalization rates. They described providing early frequent visits to patients with frequent health status fluctuation, such as those with heart failure or any new diagnosis. Nurses from two agencies used the word “frontloading” to refer to this practice, which is consistent with the existing literature (O’Connor et al., 2014). Some of the study participants described it as providing early, frequent visits, while others specified the number of visits, such as at least three times per week, or every other day, or even back-to-back visits. In a recent definition of frontloading, a panel of experts in HH and heart failure suggested a specific number and timing of nursing visits within the first posthospital week (Murtaugh et al., 2017). Their definition is broadly aligned with our findings and provides direction to visiting nurses as they develop visit plans.
Early and intensive skilled nursing visits contribute to decreased hospital readmission when combined with a physician follow-up visit in the first week after hospital discharge (Murtaugh et al., 2017). Nurses need to identify who would benefit from this treatment combination to prevent or at least delay hospital readmissions. When describing visit patterns, very few of the study participants mentioned the importance of having patients visit their primary care provider within the first two weeks of the episode. Some patients are less likely to follow up with their provider within seven days after hospital discharge (Kociol et al., 2011). Therefore, it is essential to start planning for post-acute care services while patients are still in the hospital. This planning includes close communication and coordination between in-patient providers and HH clinicians, as well as patients and their caregivers, to arrange for timely intensive skilled nursing visits and early physician follow-up.
The study participants described how poor communication with providers and incomplete referral information were barriers to developing personalized visit plans. These results are consistent with previous studies that highlight the challenges to interacting with providers to make changes to the plan of care (Bowles, Holland, & Horowitz, 2009) and the suboptimal transfer of patient information across care settings, specifically from hospitals to HH agencies (Bowles, Pham, O'Connor, & Horowitz, 2010; Egan et al., 2009). HH nurses rely on optimal communication across settings to provide “seamless, connected, and coordinated care” and ensure successful patient transitions (Landers et al., 2016). HH agencies need to develop new strategies to enhance information sharing and coordination with providers across care settings.
Limitations
This study was conducted with experienced nurses from three large urban HH agencies serving a diverse patient population in three Mid-Atlantic states. Therefore, the findings may have been different if interviews were conducted with less-experienced nurses from smaller agencies or agencies from other geographical regions. Moreover, it is possible that nurses who expressed interest and participated in the study had a different approach to visit planning compared to nonparticipants. Data were collected through in-person or web-based video interviews, reflecting varying levels of interpersonal connections with the interviewer and potentially leading to different results. Finally, nurses were asked about their decision-making process regarding visit intensity planning and one cannot draw conclusions about which process has a better influence on care provision. While there is some literature to support that visit intensity may be associated with patient outcomes, future research is needed to further explore the association with improved patient care and outcomes.
Recommendations for Future Research
The study participants described the importance of communicating with providers and accessing accurate referral information to coordinate care and develop personalized visit plans. Health information technology provides hope to facilitate the timely and efficient collection and transmission of patient information across care settings to support care decisions. The value of health information technology on care planning and care provision in HH was recently established (Alhuwail & Koru, 2016; Sockolow, Bass, Eberle, & Bowles, 2016; Sockolow, Bowles, Adelsberger, Chittams, & Liao, 2014). One potential strategy is to promote the use of a standardized document such as the Continuity of Care Document within electronic medical documentation. Researchers would first revise the document by including HH clinicians in the process to meet their information needs. Following the implementation of this initiative, researchers would evaluate its impact on information access and its interoperability to optimize information transfer across clinical settings.
The study participants also described how protocols guided their decisions by serving as a starting point and offering a standardization to the visit planning process. However, the protocols used by participating agencies were developed by agency staff and were not evidence-driven. Therefore, nurses would benefit from evidence-based clinical decision support tools to guide their decisions. The use of clinical decision support systems in nursing is an emerging field with potential to influence decision quality (Anderson & Willson, 2008). The patient factors described by the study participants inform the preliminary content of a tool that researchers can further develop and test in future studies. Additional research is necessary to identify visit patterns associated with specific patient characteristics, then examine the impact of these visit patterns on patient outcomes and make suggestions about visit intensity protocols. While the adoption of clinical decision support systems is a promising start, the federal government needs to provide financial support to implement health information technology initiatives in HH, because HH agencies are not eligible for “meaningful use” incentive payments.
Patients referred to HH have increasingly complex needs and are discharged sooner from acute care settings. The current HH setting is perceived as a short-term teaching environment where clinicians partner with patients to help them reach their maximum self-care potential with a limited number of visits. Future research needs to identify characteristics of activated HH patients and develop interventions to better engage patients and their caregivers in care provision as they transition from acute care settings to home.
Acknowledgments
The authors would like to thank the nurses who participated in the study.
This study was supported by a grant from the Frank Morgan Jones Fund at the University of Pennsylvania. Dr. Irani’s post-doctoral training is supported by the National Institute of Nursing Research of the National Institutes of Health (T32NR015433 Multiple Chronic Conditions, Interdisciplinary Nurse Scientist Training; Principal Investigator, Dr. Shirley M. Moore).
Footnotes
Author’s Note:
The findings were presented as part of a symposium at the International Association of Gerontology and Geriatrics (IAGG) 21st World Congress in San Francisco, California (July 23-27, 2017).
Contributor Information
Elliane Irani, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH, USA.
Karen B. Hirschman, School of Nursing, University of Pennsylvania, Philadelphia, PA, USA.
Pamela Z. Cacchione, School of Nursing, University of Pennsylvania, Philadelphia, PA, USA.
Kathryn H. Bowles, School of Nursing, University of Pennsylvania, Philadelphia, PA, USA; Center for Home Care Policy and Research, Visiting Nurse Service of New York, NY, USA.
References
- Abboud S, Kim SK, Jacoby S, Mooney-Doyle K, Waite T, Froh E, Kagan S. Co-creation of a pedagogical space to support qualitative inquiry: An advanced qualitative collective. Nurse Education Today. 2017;50:8–11. doi: 10.1016/j.nedt.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhuwail D, Koru G. Identifying home care clinicians' information needs for managing fall risks. Applied Clinical Informatics. 2016;7(2):211–226. doi: 10.4338/ACI-2015-11-RA-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JA, Willson P. Clinical decision support systems in nursing: Synthesis of the science for evidence-based practice. Computers, Informatics, Nursing: CIN. 2008;26(3):151–158. doi: 10.1097/01.NCN.0000304783.72811.8e. [DOI] [PubMed] [Google Scholar]
- Banning M. A review of clinical decision making: Models and current research. Journal of Clinical Nursing. 2008;17(2):187–195. doi: 10.1111/j.1365-2702.2006.01791.x. [DOI] [PubMed] [Google Scholar]
- Bowles KH, Holland DE, Horowitz DA. A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management. Journal of Telemedicine and Telecare. 2009;15:344–350. doi: 10.1258/jtt.2009.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowles KH, Pham J, O’Connor M, Horowitz DA. Information deficits in home care: A barrier to evidence-based disease management. Home Health Care Management & Practice. 2010;22(4):278–285. [Google Scholar]
- Bruce ML, Lohman MC, Greenberg RL, Bao Y, Raue PJ. Integrating depression care management into Medicare home health reduces risk of 30‐and 60‐Day hospitalization: The depression care for patients at home Cluster‐Randomized trial. Journal of the American Geriatrics Society. 2016;64(11):2196–2203. doi: 10.1111/jgs.14440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns SC, Neville M. Cognitive assessment trends in home health care for adults with mild stroke. American Journal of Occupational Therapy. 2016;70(2):1–8. doi: 10.5014/ajot.2016.016543. 7002290020. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. State operations manual. Chapter 2: The certification process. 2015 Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107c02.pdf.
- Cliff C, McGraw C. The conduct and process of mental capacity assessments in home healthcare settings. British Journal of Community Nursing. 2016;21(11):570–577. doi: 10.12968/bjcn.2016.21.11.570. [DOI] [PubMed] [Google Scholar]
- Egan M, Wells J, Byrne K, Jaglal S, Stolee P, Chesworth BM, Hillier LM. The process of decision‐making in home‐care case management: Implications for the introduction of universal assessment and information technology. Health & Social Care in the Community. 2009;17(4):371–378. doi: 10.1111/j.1365-2524.2008.00835.x. [DOI] [PubMed] [Google Scholar]
- Ellenbecker CH, Boylan LN, Samia L. What home healthcare nurses are saying about their jobs. Home Healthcare Nurse. 2006;24(5):315–324. doi: 10.1097/00004045-200605000-00010. [DOI] [PubMed] [Google Scholar]
- Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: A focus on trustworthiness. SAGE Open. 2014:1–14. doi: 10.1177/2158244014522633. [DOI] [Google Scholar]
- Flynn L. Extending work environment research into home health settings. Western Journal of Nursing Research. 2007;29(2):200–212. doi: 10.1177/0193945906292554. doi:29/2/200 [pii] [DOI] [PubMed] [Google Scholar]
- Gillespie M, Paterson BL. Helping novice nurses make effective clinical decisions: The situated clinical decision-making framework. Nursing Education Perspectives. 2009;30(3):164–170. [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Gruman J, Rovner MH, French ME, Jeffress D, Sofaer S, Shaller D, Prager DJ. From patient education to patient engagement: Implications for the field of patient education. Patient Education and Counseling. 2010;78(3):350–356. doi: 10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J. What the evidence shows about patient activation: Better health outcomes and care experiences; fewer data on costs. Health Affairs. 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. doi:15/9/1277 [pii] [DOI] [PubMed] [Google Scholar]
- Johansen ML, O’Brien JL. Decision making in nursing practice: A concept analysis. Nursing Forum. 2016;51(1):40–48. doi: 10.1111/nuf.12119. [doi] [DOI] [PubMed] [Google Scholar]
- Koch T. Establishing rigour in qualitative research: The decision trail. Journal of Advanced Nursing. 2006;53(1):91–100. doi: 10.1111/j.1365-2648.2006.03681.x. [DOI] [PubMed] [Google Scholar]
- Kociol RD, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Hernandez AF. Associations of patient demographic characteristics and regional physician density with early physician follow-up among Medicare beneficiaries hospitalized with heart failure. The American Journal of Cardiology. 2011;108(7):985–991. doi: 10.1016/j.amjcard.2011.05.032. [DOI] [PubMed] [Google Scholar]
- Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. New England Journal of Medicine. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landers S, Madigan E, Leff B, Rosati RJ, McCann BA, Hornbake R, Breese E. The future of home health care: A strategic framework for optimizing value. Home Health Care Management & Practice. 2016;28(4):262–278. doi: 10.1177/1084822316666368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie JL, Lonneman W. Promoting trust in the registered nurse-patient relationship. Home Healthcare Now. 2016;34(1):38–42. doi: 10.1097/NHH.0000000000000322. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education & Behavior. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. A data book: Health care spending and the Medicare program. 2016 Retrieved from http://www.medpac.gov/docs/default-source/data-book/june-2016-data-book-health-care-spending-and-the-medicare-program.pdf.
- Medicare Payment Advisory Commission. Report to the congress: Medicare payment policy. 2017 Retrieved from http://www.medpac.gov/docs/default-source/reports/mar17_entirereport.pdf.
- Milne J, Oberle K. Enhancing rigor in qualitative description. Journal of Wound Ostomy & Continence Nursing. 2005;32(6):413–420. doi: 10.1097/00152192-200511000-00014. [DOI] [PubMed] [Google Scholar]
- Morse JM. Critical analysis of strategies for determining rigor in qualitative inquiry. Qualitative Health Research. 2015;25(9):1212–1222. doi: 10.1177/1049732315588501. [doi] [DOI] [PubMed] [Google Scholar]
- Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H. Complexity in geriatric home healthcare. Journal for Healthcare Quality. 2009;31(2):34–43. doi: 10.1111/j.1945-1474.2009.00017.x. [DOI] [PubMed] [Google Scholar]
- Murtaugh CM, Deb P, Zhu C, Peng TR, Barrón Y, Shah S, Siu AL. Reducing readmissions among heart failure patients discharged to home health care: Effectiveness of early and intensive nursing services and early physician follow‐up. Health Services Research. 2017;52(4):1445–1472. doi: 10.1111/1475-6773.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor M, Bowles KH, Feldman PH, St Pierre M, Jarrín O, Shah S, Murtaugh CM. Frontloading and intensity of skilled home health visits: A state of the science. Home Health Care Services Quarterly. 2014;33(3):159–175. doi: 10.1080/01621424.2014.931768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor M, Hanlon A, Naylor MD, Bowles KH. The impact of home health length of stay and number of skilled nursing visits on hospitalization among Medicare‐Reimbursed skilled home health beneficiaries. Research in Nursing & Health. 2015;38(4):257–267. doi: 10.1002/nur.21665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J, Perlic M, Madigan EA. The effect of frontloading visits on patient outcomes. Home Healthcare Nurse. 2007;25(2):103–109. doi: 10.1097/00004045-200702000-00011. [DOI] [PubMed] [Google Scholar]
- Rosati RJ, Huang L. Development and testing of an analytic model to identify home healthcare patients at risk for a hospitalization within the first 60 days of care. Home Health Care Services Quarterly. 2007;26(4):21–36. doi: 10.1300/J027v26n04_03. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Sample size in qualitative research. Research in Nursing & Health. 1995;18(2):179–183. doi: 10.1002/nur.4770180211. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Focus on research methods-whatever happened to qualitative description? Research in Nursing and Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Smith Higuchi KA, Christensen A, Terpstra J. Challenges in home care practice: A decision-making perspective. Journal of Community Health Nursing. 2002;19(4):225–236. doi: 10.1207/S15327655JCHN1904_03. [DOI] [PubMed] [Google Scholar]
- Sockolow P, Bass E, Eberle CL, Bowles KH. Homecare nurses’ decision-making during admission care planning. Nursing Informatics. 2016;225:28–32. doi: 10.3233/978-1-61499-658-3-28. [DOI] [PubMed] [Google Scholar]
- Sockolow PS, Bowles KH, Adelsberger MC, Chittams JL, Liao C. Impact of homecare electronic health record on timeliness of clinical documentation, reimbursement, and patient outcomes. Applied Clinical Informatics. 2014;5(2):445–462. doi: 10.4338/ACI-2013-12-RA-0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stajduhar KI, Funk L, Roberts D, McLeod B, Cloutier‐Fisher D, Wilkinson C, Purkis ME. Home care nurses’ decisions about the need for and amount of service at the end of life. Journal of Advanced Nursing. 2011;67(2):276–286. doi: 10.1111/j.1365-2648.2010.05491.x. [DOI] [PubMed] [Google Scholar]
- Tanner CA. Thinking like a nurse: A research-based model of clinical judgment in nursing. The Journal of Nursing Education. 2006;45(6):204–211. doi: 10.3928/01484834-20060601-04. [DOI] [PubMed] [Google Scholar]
- Tullai-McGuinness S, Riggs JS, Farag AA. Work environment characteristics of high-quality home health agencies. Western Journal of Nursing Research. 2011;33(6):767–785. doi: 10.1177/0193945910381490. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;185(4157):1124–1131. doi: 10.1126/science.185.4157.1124. doi:185/4157/1124 [pii] [DOI] [PubMed] [Google Scholar]
- Yeboah-Korang A, Kleppinger A, Fortinsky RH. Racial and ethnic group variations in service use in a national sample of Medicare home health care patients with type 2 diabetes mellitus. Journal of the American Geriatrics Society. 2011;59(6):1123–1129. doi: 10.1111/j.1532-5415.2011.03424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


