Abstract
Objective
Former youth in foster care (YFC) are at greater risk of chronic health conditions than their peers. Although research in general population samples has demonstrated a dose-response relationship between adverse childhood experiences (ACEs) and adult health outcomes, few studies have conducted similar analyses in highly stress-exposed populations such as YFC. This paper uses person-centered latent class analysis (LCA) methods to examine the relationship between different profiles of ACE exposures and divergent health trajectories amongst this high-risk population.
Methods
Data are from longitudinal research that followed transition-age YFC from age 17–26 (N =732). Using three subgroups previously identified by their ACEs histories, Complex, Environmental, and Lower Adversity groups, we applied group mean statistics to test for differences between the groups for physical and sexual health outcomes in young adulthood.
Results
In contrast to prior research demonstrating that the Environmental group was at the highest risk of criminal behavior outcomes, for most of the physical and sexual health risk outcomes evaluated in this paper, the Complex Adversity group had the highest risk.
Conclusions
This study demonstrates that there are subgroups of YFC which each have a distinct profile of risk in young adulthood, with the Complex group being at highest risk of the physical and sexual health risk outcomes evaluated. Findings strongly suggest the need for targeted strategies to promote screening for ACEs and chronic health conditions, linkage to adult healthcare, and continuity of care for adolescents and young adults in foster care to offset these trajectories.
Keywords: adverse childhood experiences, foster care, aging out, latent class analysis
Introduction
Youth who have been in foster care (YFC) are at high risk of many health problems in young adulthood including hypertension, diabetes, being a smoker, heart disease, stroke, attention deficit hyperactivity disorder, and asthma compared with peers who have not resided in foster care.1,2 The disproportionately high rates of these negative health outcomes may be explained, at least in part, by the high levels of adverse childhood experiences (ACEs) to which these youth are exposed during their early years. In general population samples, a large body of literature has consistently demonstrated a dose-response relationship between the number of childhood stressors and the likelihood of mental health, substance-related, and physical health problems.8 Recent research has broadened our understanding of the impact of ACEs by measuring effects of these stressors in highly stressed groups (rather than in general population samples) such as those with lower household incomes and those who identify as racial/ethnic minorities. These studies have also expanded the ACEs framework to incorporate additional stressors that may be experienced by these groups (e.g. racism).6–7
However, little research has been conducted to understand the impacts of ACEs exposures among YFC. These youth are exposed to high rates of poverty, abuse, neglect, domestic violence, and parental substance use.3–5 In addition to these family-based ACEs, YFC are also more likely be exposed to other forms of stress, such as being involved in or witnessing traumatic events and undergoing placement changes or adoption plan failures while in foster care.3 Finally, by definition they are universally exposed to one adversity – being removed from the home(s) of their parent(s).
The body of literature defining the impact of ACEs is an important and emerging area for the pediatric community.8 Though this significant population health relationship between cumulative stress and negative health outcomes has been broadly established, a gap in the literature is whether and how different patterns of ACEs exposure are associated with differential health outcomes later in life. Said another way, in addition to understanding that more stress equals higher risks, a clearer and more nuanced understanding of how adversity impacts the transition into adulthood for specific groups of youth can inform policy and practice.
As a population, YFC have likely both higher and different patterns adversity experiences compared to the general public, thus, a nuanced understanding of the composition of adversities and their relationships to specific outcomes may provide distinguishing opportunities for interventions. Variable-oriented methods such as regression analyses provide estimates of sample wide relationships between variables.19 In contrast person-centered tools, such as latent class analysis (LCA), test for structure within a sample’s heterogeneity.20 LCA and related techniques thereby build on sample aggregate analyses, offering potential for discerning subgroups of a population that are likely to benefit from tailored intervention efforts.
Previous studies have employed LCA to assess subgroups within youth emancipating from foster care.21–23 The current study builds upon a prior analysis that included conventional ACEs variables alongside the above-described variables to which YFC have the potential to be uniquely exposed.24 This analysis yielded 3 subgroups of youth which we labeled Complex, Environmental, and Lower Adversity classes. The Complex Adversity class had the highest proportions of youth reporting conventional ACEs (maltreatment and adverse household factors). The Environmental Adversity class reported highest levels of exposure to harm in their environments (physical fighting, natural disasters), and the Lower Adversity class experienced adversity at lowest rates (see Methods section for more detail). That analysis established that these three patterns of adversity exposures were differentially associated with economic, psychosocial, and criminal behavior outcomes. 24 Specifically, Complex Adversity youth reported greater homelessness and depressive symptoms, Environmental exposure youth reported more crime-related indicators (e.g., being arrested), and youth with both the Complex and Environmental adversities reported higher proportions of the psychosocial problems and criminal behaviors than Lower Adversity youth.
In the present study, we sought to evaluate whether these patterns of adversity exposures are associated with differences in physical and sexual health risk outcomes over time among youth aging out of the foster care system. We included markers of overall health as well as several specific physical and sexual health risk indicators which: 1) have been previously found to be disproportionately represented among youth aging out of foster care,1–2 and/or 2) have potential to become chronic health conditions that affect lifelong quality of life. Thus, we selected outcomes which are likely to have particular relevance for early and preventive health care intervention among YFC.
Methods
Study Design and Data Collection Procedures
We used data from the Midwest Evaluation of the Adult Functioning of Former YFC (Midwest Study), the largest longitudinal study of youth aging out of foster care.1 The Midwest Study followed youth who were in foster care in Illinois, Iowa, and Wisconsin from the time they were 17 years old (wave 1 assessment) through waves 2 through 5 at ages 19, 21, 23–24, and 25–26. Youth were eligible for the study if they had been in out-of-home care for at least one year, were between 17 and 17½ years old at the time of recruitment (2002), and consented to participate. Youth were excluded if they had severe developmental disability or mental illness, were placed in a correctional/psychiatric facility, or were on runaway status. All eligible youth from Iowa and Wisconsin and a random sample of two-thirds of the eligible youth from Illinois who fit the study criteria were recruited for the study. Overall, the response rate was 95.4% for a total of 732 youth who participated in the study. Institutional Review Board (IRB) approval and informed consent were obtained prior to all interviews.
Variables
Measures Used to Identify LCA Subgroups
At Wave 1 in accordance with the IRB, youth were asked about adversity that they had experienced during their childhood. We applied a modified cumulative scale that assessed 1) conventional ACEs domains,8–9 2) experiences in the youth’s social environment relevant to YFC included in other prior expanded ACEs frameworks,12, 25–26 and 3) childhood stressors associated with the foster care system (for other illustrations of modified ACEs see 6–7). Responses were coded dichotomously--including four maltreatment variables (sexual assault, physical abuse by a caregiver, neglect by a caregiver, and abandonment), six household factors: four characteristics of caregivers in the households from which youth were removed at the time they were placed in foster care (caregiver substance abuse, mental illness, domestic violence, and/or criminal record) as well as two adversities while in care (placement in five or more foster homes, adoption plan failure), and five environmentally-based factors (witnessed others being seriously hurt or killed, were involved in physical fighting, experienced a natural disaster or fire, experienced a life-threatening accident, and/or a very serious injury).
As previously noted, LCA methods assessed the sample for subgroup structure based on these items. Unlike similar methods, such as cluster analysis, LCA uses statistical methods to test for goodness-of-fit, providing a more objective assessment of the identified groups.25 A three-class model was found to be the best fit among adverse childhood experiences based on conventional model-test statistics.
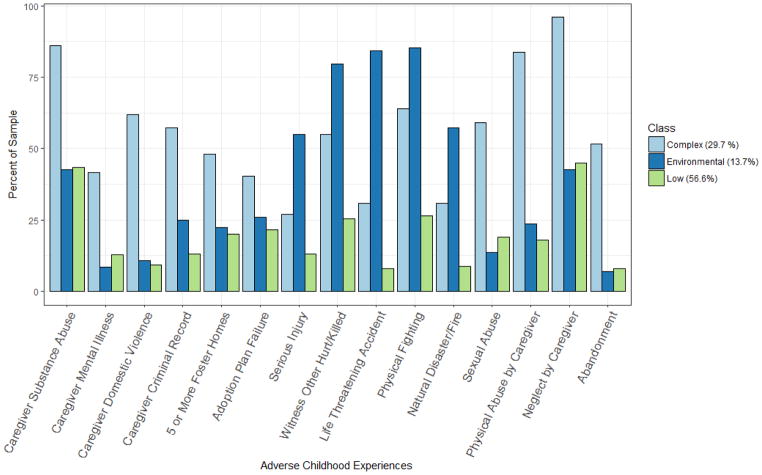
The patterns resulted within these three profiles: Complex Adversity (29.7%), Environmental Adversity (13.7%), and Lower Adversity (56.6%).22 As described earlier, the Environmental Adversity class was distinct in experiencing the environmental context adversities at higher rates than the other two classes. The Complex Adversity youth reported a mean of 7.92 types of adversities, the Environmental Adversity youth a mean of 5.71, and the Lower Adversity youth a mean of 2.85. The distributions of adversity experiences of the sample are presented in Figure 1. For more information about the latent class analysis results, see [Anonymous (2017)].
Figure 1.
Adverse Childhood Experiences by Class
Outcome Measures
General health status, assessed as poor, fair, good, very good, excellent across all 5 waves was used to construct a dichotomous variable -- assigned 1 if reported poor or fair health at any wave. Existence of a disability or health condition that limited activities of daily living was similarly coded dichotomously as 1 if a participant answered affirmatively at any assessed wave (Waves 3–5).
Cardiovascular indicators were assessed at Wave 5, when respondents were 25 or 26 years old. This included cardiovascular/metabolic outcomes of dyslipidemia, hypertension, diabetes, whether they were a chronic smoker (defined as having ever smoked “regularly” and for the past 30 days), and whether they reported a body mass index (BMI) of greater than 30 at any wave 1–5. A summary variable of any cardiovascular risk condition (dyslipidemia, hypertension, diabetes, obesity, and smoker) was created.
Other chronic health conditions (Wave 5) included asthma, seizure disorder, ADHD, eating disorder, and (Waves 1 and 2) sleep disturbance (“trouble with falling or staying asleep on a weekly or more frequent basis”). Female respondents were also asked about polycystic ovary syndrome (PCOS) which was not included in the summary indexes. A summary variable was generated for other chronic physical health conditions: asthma, seizure disorder, ADHD, sleep problems, or eating disorder.
Sexual health risk outcomes (Waves 2–5), included: 1) ever had sex with a partner who was infected with a sexually transmitted infection, and 2) number of sexual partners in the past year-- dichotomously coded as 1 for an affirmative response at any waves, as well as a dichotomous variable (Wave 5) whether a participant had ever had a prior diagnosis of a sexually transmitted infection.
Analyses
We used chi-square analyses to test for significant differences in proportions by LCA groups by health indicator. We then used one-way analysis of variance (ANOVA) and post-hoc Tukey’s test to test for between group differences in terms of the percentage for each outcome. Additionally, we conducted sensitivity analyses to determine whether results were as expected using a more classic variable-oriented approach. Specifically, we conducted logistic regression analyses to determine whether a summary variable that counted the number of ACEs endorsed by respondents was significantly associated with each health outcome.
Results
Demographically, the sample comprised 48.50% males and 51.50% females. Over half (55.88%) identified as Non-Hispanic Black, 29.05% as Non-Hispanic White, 8.02% as Any Race Hispanic, and 5.12% as Mixed Race. More than 80% of the original sample participated in each subsequent wave of data collection. No statistically significant demographic differences were found between the full Wave 1 sample and the Wave 5 sample, indicating stability of gender and racial representation in the sample over time. Demographics by class are presented in Table 1.
Table 1.
Demographics by Class in Percentages
| Complex (29.32%) | Environmental (12.19%) | Low (58.49%) | X2 | |
|---|---|---|---|---|
| Race and Ethnicity | 35.60*** | |||
| Non-Hispanic White | 42.92 | 20.69 | 23.82 | |
| Non-Hispanic Black | 41.04 | 60.92 | 62.26 | |
| Hispanic | 8.49 | 6.9 | 8.02 | |
| Mixed Race | 5.66 | 8.05 | 4.25 | |
| Other Race | 1.89 | 3.45 | 1.65 | |
| Gender | 12.94** | |||
| Male | 47.66 | 66.29 | 45.43 | |
| Female | 52.34 | 33.71 | 54.57 |
p < .05
p < .01
p < .001
Among the non-cardiovascular outcomes, 5.55% of the overall sample reported being diagnosed with asthma, 1.51% a seizure disorder, and 6.21% with ADHD. Of the cardiovascular outcomes, 4.19% to having hypertension, 0.84% with diabetes, and 40.17% of the sample reported being a smoker. The sexual health risk outcomes were more frequently endorsed with 32.63% reporting being diagnosed with a sexually transmitted infection, and about one in five (21.20%) indicating that they had five or more sexual partners in the past year at some point during the study. More than two-thirds of the sample were obese at any of the waves (69.81%), almost a quarter reported a disability (24.53%), and 64.62% rated their health as poor or fair. Table 2 contains a full description of the sample proportions reporting each outcome.
Table 2.
Frequency of Young Adult Health Outcomes for Sample
| N | % | |
|---|---|---|
| Cardiovascular Risk Conditions | ||
| Dyslipidemia | 596 | 0.67 |
| Hypertension | 596 | 4.19 |
| Diabetes | 595 | 0.84 |
| Chronic Smoker | 595 | 40.17 |
| Ever Obese | 730 | 69.81 |
| Any Cardiovascular Risk Condition a | 596 | 43.12 |
| Other Chronic Health Conditions | ||
| Asthma | 596 | 5.55 |
| Seizures | 596 | 1.51 |
| ADHD | 596 | 6.22 |
| Eating Disorder | 596 | 2.01 |
| Sleep Problem | 635 | 41.10 |
| PCOS c | 377 | 3.45 |
| Any Other Chronic Physical Health Condition b | 596 | 9.23 |
| Sexual Health Risk Outcomes | ||
| Sex with an Infected Partner | 647 | 22.26 |
| Five or more Sexual Partners in a Year | 684 | 21.20 |
| Sexually Transmitted Infection | 472 | 32.63 |
| Other Health Outcomes | ||
| Health Rating Poor or Fair | 730 | 64.62 |
| Any Disability | 685 | 24.53 |
Includes dyslipidemia, hypertension, diabetes, and smoking
includes asthma, seizures/epilepsy, diabetes, ADHD, eating disorder, and sleep problem
analysis only includes females
In our main analyses, we found differences in health outcomes amongst the three different patterns of early life adversity. The Complex Adversity class reported statistically significantly higher proportions than the Lower Adversity class of smoking (51.50% vs. 34.89%), asthma (10.18% vs. 3.56%), ADHD (11.38% vs. 3.56%), ever being obese (75.23% vs. 65.57%), rating their health as fair or poor (71.03% vs. 60.19%), any disability (34.01% vs. 20.10%), and any cardiovascular condition (86.23% vs. 75.62%). The Complex (52.80%) and Environmental Adversity classes (40.45%) had statistically significantly higher reports than the Lower Adversity class (26.23%) of sleep problems. Additionally, the Lower Adversity class had statistically significantly lower reports of non-cardiovascular chronic physical health conditions (33.46%) than did both other classes (Complex Adversity: 61.39%; Environmental Adversity: 54.55%). A third of the Environmental Adversity class reported five or more sexual partners in the past year, which is a significantly higher rate than the Lower Adversity class (18.52%). Complete results of the analyses of differences in health outcomes between the classes are presented in Table 3.
Table 3.
Percent of Young Adult Health Outcomes by Adversity Class
| N | Complex (29.32%) | Environmental (12.19%) | Lower (58.49%) | X2 | Between Classes | ||
|---|---|---|---|---|---|---|---|
| Cardiovascular (CVD) Risk Conditions | |||||||
| Dyslipidemia | 595 | 2.40 | 0.00 | 0.55 | 4.64 | ||
| Hypertension | 595 | 7.19 | 4.76 | 3.29 | 4.03 | ||
| Diabetes | 594 | 1.20 | 3.17 | 0.27 | 5.76 | ||
| Chronic Smoker | 594 | 51.50 | 39.68 | 34.89 | 13.15 | ** | y |
| Ever Obese | 730 | 75.23 | 76.40 | 65.57 | 8.44 | * | y |
| Any Cardiovascular Risk Condition a | 595 | 86.23 | 82.54 | 75.62 | 15.93 | * | y |
| Non-CVD Chronic Health Conditions | |||||||
| Asthma | 595 | 10.78 | 6.35 | 4.11 | 8.74 | * | y |
| Seizures | 595 | 1.80 | 1.59 | 1.64 | 0.02 | ||
| ADHD | 595 | 12.57 | 7.94 | 4.38 | 11.80 | ** | y |
| Eating Disorder | 595 | 2.99 | 1.59 | 1.64 | 1.12 | ||
| Sleep Problem | 635 | 58.55 | 48.65 | 30.43 | 43.31 | *** | y, z |
| PCOS c | 375 | 4.46 | 10.00 | 2.15 | 5.37 | ||
| Any Non-CVD Chronic Physical Health Condition b | 532 | 61.39 | 54.55 | 34.48 | 33.46 | *** | y, z |
| Sexual Health Risk Outcomes | |||||||
| Sex with Infected Partner | 647 | 26.34 | 17.11 | 21.30 | 3.17 | ||
| 5+ Sexual Partners in a Year | 684 | 21.72 | 33.33 | 18.52 | 8.91 | * | z |
| Sexually Transmitted Infection | 471 | 38.41 | 27.78 | 30.82 | 3.08 | ||
| Other Health Statuses | |||||||
| Health Rating Ever Poor or Fair | 730 | 71.03 | 69.66 | 60.19 | 8.49 | * | y |
| Any Disability | 684 | 34.01 | 24.05 | 20.10 | 13.89 | ** | y |
p < .05
p < .01
p < .001
Includes dyslipidemia, hypertension, diabetes, and smoking
includes asthma, seizures/epilepsy, ADHD, eating disorder, and sleep problem
analysis only includes females
y = statistically significant difference between Complex & Lower classes
z = statistically significant difference between Environmental & Lower classes
Our sensitivity analysis revealed an expected dose-response pattern within the sample overall – e.g. that higher scores on the ACEs summary variable was associated with higher risk of physical and sexual health outcomes, with most outcomes demonstrating a statistically significant relationship. This illuminates the complementarity of the variable-oriented and person-oriented analytic approach wherein subgroup heterogeneity (e.g., the respondent classes or groups) may reside alongside aggregate full sample trends (e.g., cumulative adversity dose-response).
Discussion
Use of latent class analysis provides value-added extension in documenting patterned differences as a function of distinct profiles among adversity exposures, with results that hold implications for life course health within this high-risk population and others exposed to similarly high rates of early adversity. This examination establishes that, as foster care youth are transitioning into early adulthood, relatively elevated histories of childhood adversity increase the risk of poor health outcomes in young adulthood, and also increase risk of health behaviors that are likely to contribute to health problems later in adulthood.
The current work extends previous ACEs studies that have found a dose-response relationship between the number of ACEs experienced and risk of poor health outcomes in general population samples. This is the first study, to our knowledge, that has examined the relationship of ACEs and young adult health outcomes among youth who have aged out of foster care. The results here support the broader findings of increased ACEs exposure leading to increased health problems that constitute targets for early intervention to interrupt the longer-term physiology of stress-related health erosion.16, 26 Further, our work supports the use of expanded ACEs assessments with higher risk populations where adversity exposures beyond conventional assessment, including sources outside the home are likely to be relevant. Further research is necessary to identify whether similar patterns are found among other higher risk populations, such as homeless youth and youth involved in the juvenile justice system.
A comparison of these health outcomes with the economic, psychosocial, and criminal behavior outcomes by class in our previous research are consistent with health erosion through multiple pathways. Those earlier results illuminated substantially higher health risk profiles (e.g., drug and alcohol use, criminogenic behaviors, homelessness and trading sex for money) as well as poorer mental health that place those youth in circumstances and conditions likely to carry a range of additional life stressors.22 This continuing trend of stress and adversity exposure will likely add to the physiological dysregulation and allostatic load that incrementally leads to chronic health conditions in later adulthood.
The current findings indicate that with respect to health outcomes and risk behaviors that are precursors to later poor health outcomes, the Complex Adversity class demonstrated the highest rates. Asthma, an inflammatory system marker more likely to evidence dysregulation, demonstrated a similar trend. This may be due to a simple dose response relationship, as this class had the highest number of total ACEs of all of the groups. Alternatively, it may be explained by the specific constellation of ACEs for which this group was at highest risk (e.g. maternal substance abuse and neglect), or a combination of both dose and composition of ACEs. Regardless of causative explanation, this relatively consistent trend across a variety of health outcomes during young adulthood illustrates the value of beginning preventive and health buffering activities within primary health well before chronic health conditions are fully established.27–28
Our findings indicate that, even within a high-risk population that is exposed to a panoply of stressful life circumstances, those who have experienced both greater numbers of adversities as well as certain types are at increased risk of entering young adulthood with poorer current health and possible subclinical trajectories toward poor health that becomes evident later in adulthood.
A caveat regarding the labeling of the Lower Adversity group is that their lower risk is relative to their YFC peers but not to the general population. The Ahrens et al. study1 examined health outcomes for former YFC with economically secure (ES) and economically insecure (EI) youth from the nationally representative National Longitudinal Study of Adolescent Health study (Add Health). Some of the same health conditions were examined as in the present study allowing for comparison between the Lower Adversity group and the general population. Comparing the two Add Health groups and the Lower Adversity (LA) group shows that the Lower Adversity group had higher proportions of poor health outcomes than both Add Health groups for hypertension, chronic smoking, asthma, seizures, ADHD, and any cardiovascular risk condition. The only health problems examined by both studies for which the LA group did not have higher prevalence rates than the Add Health groups were dyslipidemia and diabetes. Thus, while the Lower Adversity group is at lower risk compared to other youth aging out of foster care it still has poorer health outcomes than the general population.
Results specifically indicate that ACEs screenings are warranted for high-risk populations, such as YFC. Recent research indicates that most pediatricians do not screen for and are unfamiliar with ACEs.29 Although routine screening among children may not be universally judicious, we argue that it is valuable for high risk populations providing greater opportunity for trauma-informed patient education and care. More toxic levels of childhood adversity signal risk of neurobiological dysregulations that can lead to a cascade of later health problems, the development of which may go undetected until chronic conditions emerge.30 These adverse patterns are also associated with exposure to subsequent social contexts and environments that carry health jeopardizing risks,31 particularly among low income youth such as those exiting foster care.26 Medical providers have opportunities to assess ACEs profiles and to support youth and caregivers in fostering resilience building social, emotional, and health resources and habits, and to refer youth and caregivers for trauma-informed care.32
Findings also highlight the importance for all youth aging out of foster care to continue to have health insurance into young adulthood and access to trauma-informed medical care. Given the high prevalence of chronic health conditions in this population, and that gaps and delays in care are linked to increased morbidity and mortality during the transition to adult health care for a variety of chronic health conditions, programs that promote linkage to adult care and continuity of providers are likely to be of significant benefit for these youth, perhaps even more so than for youth in the general population.33–34 In particular, this highlights the importance of the ACA provision for youth aging out of care being eligible for Medicaid until 26 in all 50 states.
There are a few limitations to this study. First, responses were obtained via self-report without clinical or administrative data available. However, evidence from other studies has indicated that self-report tends to be satisfactory for assessment of trends in relationships among variables.35 Self-reporting of ACEs in particular has indicated adequate variance, stability of linear trends between retrospectively assessed adversity and subsequent outcomes, and weak to no evidence of current mood state effects on reporting.36–37 It is, however, possible and even likely that rates of chronic health conditions were underreported; thus our point estimates are likely to be underestimates of the true prevalence for each condition. Second, the ACEs were assessed dichotomously, not capturing the duration or frequency of these traumatic experiences. Although this kind of epidemiological assessment has proven satisfactory in ACEs research to date, future research should explore more detailed clinical information about the experiences of this population to ascertain factors like timing and duration of exposures and of health problem onset. Third, we used methods that allowed us to utilize all of the available data points even if a youth did not participate in one or more follow-up waves. While the response rates at each follow-up wave were quite high (between 81 and 83%).38 it is possible that missing data could have influenced our results. Further, the parent study excluded some youth that would have been difficult to assess longitudinally, which may have reduced the prevalence of the health outcomes of interest. Finally, low rates of some of health disorders at this relatively early point in adulthood may have limited our ability to detect statistically significant relationships between classes and health outcomes, some of which will be more clinically evident in later adulthood.
Conclusion
In combination with prior work,24 this study both demonstrates health erosion among child welfare system-involved youth even for those with the lowest levels of exposure relative to general population youth and highlights specific subgroups of youth in care who are at risk for criminal and economic outcomes (Environmental Class) and physical and sexual health outcomes (Complex Class). These findings argue for investigating adversity exposure and trajectories among higher risk youth, applying tools for screening that capture adversity relevant to youths’ developmental contexts, and using assessment profiles to anticipate and tailor service responsiveness to youth who are more susceptible to deleterious health outcomes as a function of their childhood adversity histories.
What’s New.
We present findings indicating there are subgroups within the high-risk population of youth aging out of foster care based on adverse childhood experiences. These subgroups have differential health trajectories as measured in young adulthood.
Acknowledgments
Funding Source: The authors would like to acknowledge financial support for this research through grant TL1 TR000422 and K23MH090898. Partial support for this research came from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, R24 HD042828, to the Center for Studies in Demography & Ecology at the University of Washington. The authors acknowledge the support of the state public child welfare agencies in Illinois, Iowa, and Wisconsin for their participation in the parent study, which received financial support from the Bill and Melinda Gates Foundation, Annie E. Casey Foundation, Casey Family Programs, the Jim Casey Youth Opportunities Initiative, the Stuart Foundation, the Walter S. Johnson Foundation, and the W.T. Grant Foundation.
Abbreviations
- ACEs
Adverse Childhood Experiences
- ANOVA
analysis of variance
- ADHD
attention-deficit/hyperactivity disorder
- BMI
body mass index
- LCA
latent class analysis
- PCOS
polycystic ovary syndrome
Footnotes
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ahrens K, Garrison M, Courtney M. Health outcomes in young adults from foster care and economically diverse backgrounds. Pediatrics. 2014;134(6):1067–1074. doi: 10.1542/peds.2014-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zlotnick C, Tam TW, Soman LA. Life course outcomes on mental and physical health: the impact of foster care on adulthood. Am J Public Health. 2012;102(3):534–540. doi: 10.2105/AJPH.2011.300285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Courtney ME, Terao S, Bost N. [Accessed 2/27/2018];Midwest evaluation of the adult functioning of former YFC: Conditions of youth preparing to leave state care. 2004 Available at: http://www.chapinhall.org/research/report/midwest-evaluation-adult-functioning-former-foster-youth.
- 4.Barth RP, Wildfire J, Green RL. Placement into foster care and the interplay of urbanicity, child behavior problems, and poverty. Am J Orthopsychiatry. 2006;76(3):358–366. doi: 10.1037/0002-9432.76.3.358. [DOI] [PubMed] [Google Scholar]
- 5.McGuinness TM, Schneider K. Poverty, child maltreatment, and foster care. J Am Psychiatr Nurses Assoc. 2007;13(5):296–303. [Google Scholar]
- 6.Greeson JKP, Briggs EC, Kisiel CL, Layne CM, Ake GS, Ko SJ, … Fairbank JA. Complex trauma and mental health in children and adolescents placed in foster care: Findings from the national child traumatic stress network. Child Welfare. 2011;90(6):91–109. [PubMed] [Google Scholar]
- 7.Wade R, Shea JA, Rubin D, Wood J. Adverse childhood experiences of low-income urban youth. Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- 8.Bethell CD, Simpson LA, Solloway MR. Child Well-being and Adverse Childhood Experiences in the United States. Acad Pediatr. 2017 Sep 1;17(7):S1–3. doi: 10.1016/j.acap.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37(3):268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- 11.Lengua LJ, Honorado E, Bush NR. Contextual risk and parenting as predictors of effortful control and social competence in preschool children. J Appl Dev Psychol. 2007;28(1):40–55. doi: 10.1016/j.appdev.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turner RJ, Lloyd DA. Lifetime traumas and mental health: the significance of cumulative adversity. J Health Soc Behav. 1995;36(4):360–376. [PubMed] [Google Scholar]
- 13.Kim P, Evans GW, Angstadt M, et al. Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proc Natl Acad Sci U S A. 2013;110(46):18442–18447. doi: 10.1073/pnas.1308240110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuo AA, Etzel RA, Chilton LA, Watson C, Gorski PA. Primary care pediatrics and public health: meeting the needs of today’s children. Am J Public Health. 2012;102(12):e17–23. doi: 10.2105/AJPH.2012.301013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spencer N, Thanh TM, Louise S. Low income/socio-economic status in early childhood and physical health in later childhood/adolescence: a systematic review. Matern Child Health J. 2013;17(3):424–431. doi: 10.1007/s10995-012-1010-2. [DOI] [PubMed] [Google Scholar]
- 16.Nurius PS, Prince DM, Rocha A. Cumulative disadvantage and youth well-being: A multi-domain examination with life course implications. Child Adolesc Social Work J. 2015;32(6):567–576. doi: 10.1007/s10560-015-0396-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nurius PS, Green S, Logan-Greene P, Borja S. Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse Negl. 2015;45:143–153. doi: 10.1016/j.chiabu.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nurius PS, Green S, Logan-Greene P, Longhi D, Song C. Stress pathways to health disparities: Embedding ACEs within social and behavioral contexts. International Public Health Journal. 2016;8(2) [PMC free article] [PubMed] [Google Scholar]
- 19.Logan-Greene P, Nurius PS, Thompson EA. Distinct stress and resource profiles among at-risk adolescents: Implications for violence and other problem behaviors. Child and Adolescent Social Work Journal. 2012;29(5):373–390. doi: 10.1007/s10560-012-0269-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper BR, Lanza ST. Who benefits most from head start? Using latent class moderation to examine differential treatment effects. Child Development. 2014;85(6):2317–2338. doi: 10.1111/cdev.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keller TE, Cusick GR, Courtney ME. Approaching the transition to adulthood: distinctive profiles of adolescents aging out of the child welfare system. Social Service Review. 2007;81(3):453–84. doi: 10.1086/519536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Courtney ME, Hook JL, Lee JS. Distinct subgroups of former YFC during young adulthood: Implications for policy and practice. Child Care in Practice. 2012;18(4):409–418. [Google Scholar]
- 23.Havlicek J. Maltreatment histories of YFC exiting out-of-home care through emancipation: A latent class analysis. Child Maltreatment. 2014;19(3–4):199–208. doi: 10.1177/1077559514539754. [DOI] [PubMed] [Google Scholar]
- 24.Anonymous. Details omitted for double-blind reviewing 2017 [Google Scholar]
- 25.Bartholomew DJ, Steele F, Moustaki I, Galbraith JI, editors. Analysis of Multivariate Social Science Data. 2. Boca Raton: CRC Press; 2008. [Google Scholar]
- 26.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012 Apr 12;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 27.Pretty C, O’Leary DD, Cairney J, Wade TJ. Adverse childhood experiences and the cardiovascular health of children: a cross-sectional study. BMC Pediatrics. 2013;13:208. doi: 10.1186/1471-2431-13-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Su S, Jimenez MP, Roberts CTF, Loucks EB. The Role of Adverse Childhood Experiences in Cardiovascular Disease Risk: a Review with Emphasis on Plausible Mechanisms. Curr Cardiol Rep. 2015;17(10):88. doi: 10.1007/s11886-015-0645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerker BD, Storfer-Isser A, Szilagyi M, Stein RE, Garner AS, O’Connor KG, Hoagwood KE, Horwitz SM. Do pediatricians ask about adverse childhood experiences in pediatric primary care? Acad Pediatr. 2016 Mar 31;16(2):154–60. doi: 10.1016/j.acap.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, … Wood DL. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 31.Turner RJ, Thomas CS, Brown TH. Childhood adversity and adult health: Evaluating intervening mechanisms. Social Science & Medicine. 2016;156:114–124. doi: 10.1016/j.socscimed.2016.02.026. [DOI] [PubMed] [Google Scholar]
- 32.Soleimanpour S, Geierstanger S, Brindis CD. Adverse childhood experiences and resilience: Addressing the unique needs of adolescents. Acad Pediatr. 2017;17(7):S108–S114. doi: 10.1016/j.acap.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 33.McPheeters M, Davis AM, Taylor JL, Brown RF, Potter SA, Epstein RA. Transition Care for Children With Special Health Needs. Rockville (MD): 2014. [PubMed] [Google Scholar]
- 34.Betz CL, Ferris ME, Woodward JF, Okumura MJ, Jan S, Wood DL. The health care transition research consortium health care transition model: a framework for research and practice. J Pediatr Rehabil Med. 2014;7(1):3–15. doi: 10.3233/PRM-140277. [DOI] [PubMed] [Google Scholar]
- 35.Sullivan LM, Dukes KA, Harris L, Dittus RS, Greenfield S, Kaplan SH. A comparison of various methods of collecting self-reported health outcomes data among low-income and minority patients. Medical Care. 1995 Apr;33(4):AS183–194. [PubMed] [Google Scholar]
- 36.Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychol Rep. 2010 Oct;107(2):425–440. doi: 10.2466/02.04.09.10.16.21.PR0.107.5.425-440. [DOI] [PubMed] [Google Scholar]
- 37.Yancura LA, Aldwin CM. Stability and change in retrospective reports of childhood experiences over a 5-year period: findings from the Davis Longitudinal Study. Psychol Aging. 2009 Sep;24(3):715–721. doi: 10.1037/a0016203. [DOI] [PubMed] [Google Scholar]
- 38.Courtney ME, Dworsky A, Brown A, Cary C, Love K, Vorhies V. [Accessed 9/8/17];Midwest evaluation of the adult functioning of former YFC:Outcomes at age 26. 2011 Available at: http://www.chapinhall.org/sites/default/files/Midwest%20Evaluation_Report_4_10_12.pdf.