Introduction
Chronic kidney disease–mineral and bone disorder (CKD-MBD) becomes clinically detectable by late stage 3 or early stage 4 when up to 60% of patients have elevated parathyroid hormone (PTH) levels.1 Secondary hyperparathyroidism (SHPT) is a known cause of secondary myelofibrosis and refractory anemia in patients with CKD. The age of onset of kidney disease, duration of illness, and severity of hyperparathyroidism appear to be risk factors for myelofibrosis in patients in CKD. Excessive PTH upregulates elaboration of cytokines and paracrine factors in the bone marrow (IL-1α, IL-6, tumor necrosis factor–α, transforming growth factor–β, and platelet-derived growth factor). This causes marrow fibrosis, worsens the anemia seen with CKD, and at times, causes pancytopenia by undermining the hematopoetic microenvironment. PTH itself has a potent stimulatory effect on fibroblast proliferation. Its levels correlate directly with serum alkaline phophatase, which is a marker of the severity of bone disease.1, 2, 3
Although the pathogenesis of renal anemia is multifactorial, a deficiency of erythropoietin (EPO) secretion is the most important cause.2 Several factors are known to attenuate the erythropoietic response to exogenous EPO, namely, iron and/or folic acid deficiency, infections, inflammatory diseases, myelofibrosis, aluminum-induced microcytosis, and severe hyperparathyroidism. Iron deficiency is the most common factor among these. In some ways, responsiveness to EPO therapy is analogous to insulin resistance; virtually all patients respond if the dose is large enough. An inverse relation exists between serum intact PTH (iPTH) and hemoglobin and hematocrit (Hct) values.2, 3 High iPTH levels inhibit sodium−potassium adenosine triphosphatase activity, interfere with energy metabolism, and significantly shorten the life span of red blood cells. PTH also reduces the renal or extrarenal production of EPO, because serum EPO concentrations increase after parathyroidectomy (PTx) in some patients. Deficiency of active vitamin D and peripheral tissue resistance to EPO are other relevant factors that compound renal anemia. Some studies have endorsed an increase in erythrocyte osmotic fragility due to raised PTH levels in CKD patients.4 Excess PTH may also directly inhibit erythropoiesis by suppressing the burst forming units,5 but this proposition has not been confirmed by other studies.6, 7
Clinically, it is difficult to assess the refractoriness of parathyroids. However, in the absence of a response to medical therapy, despite high doses of calcitriol, vitamin D analogs, and cinacalcet, PTx may be suggested.
According to Kidney Disease: Improving Global Outcomes guidelines, it has been suggested that patients with stages 3 to 5 CKD who have severe hyperparathyroidism and in whom medical therapy has failed should be considered for PTx in view of apparent resistance. The higher the PTH level, the less likely the glands shall involute to medical therapy. When the PTH level is >800 pg/ml, only 22% of patients respond to cinacalcet therapy, which leads to a PTH level of <300 pg/ml.8, 9, 10
The availability of recombinant EPO has proved to be a boon for CKD patients since the introduction of dialysis and renal transplantation because it has obviated the need for blood transfusions, which adds to the burden of CKD treatment.11 However, there is a significant variability in the sensitivity to EPO because up to 5% to 10% of patients show a marked resistance to EPO therapy. An inadequate response to EPO therapy is defined as failure to reach or maintain a target hemoglobin concentration within 4 to 6 weeks of treatment, in the presence of adequate iron stores, when a dose of 300 U/kg per week is administered subcutaneously. Dependence on regular blood transfusions and resistance to EPO in the face of optimal micronutrient supplementation portend a poor prognosis and might be a cue to development of a state of refractory or tertiary hyperparathyroidism.12, 13
Case Presentations
Case 1
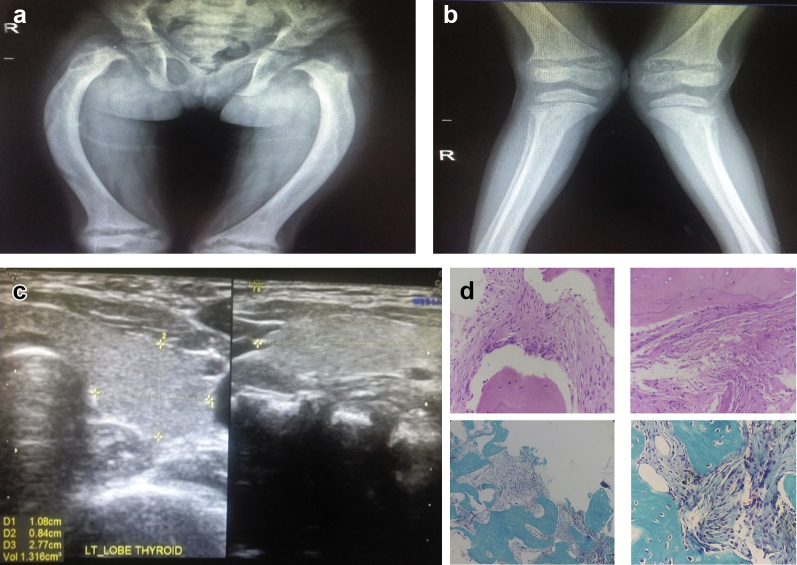
A 10-year-old female child of consanguineous parents was evaluated for severe unremitting anemia. She was diagnosed with CKD stage 5 at the age of 4 years due to autosomal recessive polycystic kidney disease, for which she underwent a successful living-related elective renal transplantation 2 years later. In the second post-transplantation year she developed with new-onset diabetes mellitus after transplantation, and thereafter, she developed evidence of graft dysfunction (creatinine levels rose to 2.7 mg/dl from a baseline of 0.5 mg/dl) as found with biopsy proven chronic interstitial fibrosis and tubular injury. The clinical scenario further deteriorated due to the MBD resulting from SHPT (PTH levels 3200 pg/ml). She was started on cinacalcet and calcitriol therapy. However, in addition to short stature, she developed gradual worsening of the rachitic stigmas (coxa vara, genu valgum, and widened wrists) (Fig. 1a and b). She had severe anemia despite treatment with high-dose EPO (dosage 400 U/kg per week, twice weekly) and required blood transfusions every month for the last 1.5 years, and was finally referred at our institution for further management.
Figure 1.
Diffuse osteopenia and rickets in long bones (a). Radiological and histologic findings in case 1 (b). A well-defined heterogeneously hyperechoic round lesions in the parathyroid suggestive of parathyroid hyperplasia or adenoma (c). A bone marrow biopsy showing hypocellularity and prominent resorption bays (Howship lacunae). Increased reticulin deposition and myelofibrosis (World Health Organization myelofibrosis grade 2) with paratrabecular accentuation evident on Masson trichome staining (d).
At our institution, peripheral smear showed a severe microcytic hypochromic anemia with anisopoikilocytosis and tear-drop cells. Iron studies suggested iron overload due to repeated blood transfusions. Serum calcium and phosphate levels were on the low-normal and high-normal side, respectively, but she had extremely high levels of PTH (Table 1). Ultrasound neck showed well-defined heterogenously hyperechoic round lesions suggestive of parathyroid hyperplasia or adenoma (Fig. 1c). Subsequent sestamibi nuclear scan revealed enhanced uptake throughout the glands.
Table 1.
Laboratory investigations: patient 1
| Laboratory parameters | Values (reference ranges) |
|---|---|
| Urea nitrogen (mg/dl) | 47 (7−20) |
| Creatinine (mg/dl) | 2.7 (0.6−1.2) |
| Calcium (mg/dl) | 9 (9−11) |
| Phosphorus (mg/dl) | 4.8 (3−4.5) |
| iPTH (pg/ml) | 3100 (230−630) |
| 25-OH vitamin D (ng/ml) | 18.4 (30−40) |
| Hemoglobin (g/dl) | 6.5 (12−15.5) |
| Hematocrit (%) | 21 (35−40) |
| Iron (μg/dl) | 156 (50−150) |
| TIBC (μg/dl) | 256 (360−400) |
| Tf saturation (%) | 61 (30−40) |
| Ferritin (μg/l) | 2000 (50−200) |
| Reticulocyte count (%) | 1.4 (0.5−1.5) |
| TLC (×103/mm3) | 13.8 (4−11) |
| Platelet count (×105/mm3) | 1.7 (1.5−4) |
iPTH, intact parathyroid hormone; Tf, transferrin; TIBC, total iron binding capacity; TLC, total leucocyte count.
A bone marrow biopsy (Fig. 1d) showed hypocellularity and prominent resorption bays (Howship lacunae). Increased reticulin deposition and myelofibrosis (World Health Organization myelofibrosis grade 2) with paratrabecular accentuation were evident on reticulin and Masson’s trichome staining. CD-71 immunostaining revealed the presence of erythroid clusters in the few cellular areas seen in the specimen.
Due to relentless progression of SHPT despite previous aggressive medical treatment with calcitriol and cinacalcet (given for up to 6 months), she underwent a subtotal PTx with autoimplantation of parathyroid tissue in the forearm. Subsequent histopathology of the parathyroid tissue showed hyperplasia of the glands. Since then, at a follow-up of 2 years, electrolyte and iPTH levels have normalized, and her refractory anemia has also shown satisfactory improvement, with blood transfusion requirements reduced to once every 3 to 4 months.
Case 2
A 2-year-old male child of consanguineous parents presented with severe recalcitrant anemia. He was diagnosed with CKD during infancy due to chronic interstitial nephritis. On admission, his eGFR was estimated to be 20 ml/min per 1.73 m2 (CKD stage 4). His physical examination was remarkable for severe anemia, massive hepatosplenomegaly, bony deformities, and bilateral hearing loss.
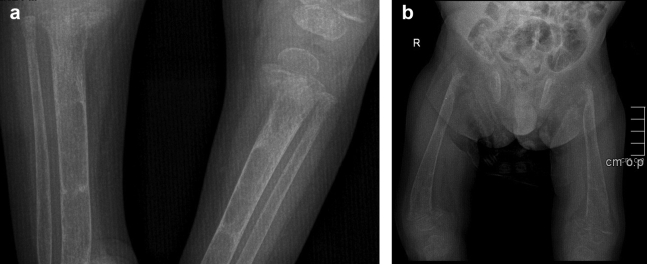
Table 2 shows the laboratory investigations of patient 2. Workup revealed pancytopenia. A peripheral smear showed normocytic normochromic red blood cells, anisocytosis, and tear drop cells. Occasional nucleated red blood cells and myelocytes were also seen in addition to thrombocytopenia. A bone marrow biopsy showed marked hypocellularity and extensive myelofibrosis (grade MF-3). Increased reticulin deposition with foci of hemosiderin laden macrophages was evident. Brainstem-evoked response audiometry confirmed bilateral profound sensorineural hearing loss. Urinalysis showed minimal proteinuria. Ultrasound scan confirmed massive hepatosplenomegaly and normal-sized kidneys with medullary cysts and cortical hyperechogenicity. Skeletal survey was remarkable for severe rickets, diffuse osteopenia, and pseudofractures in the tibia and fibula (Fig. 2a and b). A comprehensive neuro-ophthalmologic examination was unremarkable. An echocardiogram demonstrated a mildly dilated left ventricle with a normal ejection fraction.
Table 2.
Laboratory investigations: patient 2
| Laboratory parameters | Values (reference ranges) |
|---|---|
| Urea (mg/dl) | 91 (7−20) |
| Creatinine (mg/dl) | 0.9 (0.6−1.2) |
| Calcium (mg/dl) | 10 (9−11) |
| Phosphorus (mg/dl) | 7.3 (3−4.5) |
| iPTH (pg/ml) | 2500 (230−630) |
| 25-OH vitamin D (ng/ml) | 22.2 (30−40) |
| Hemoglobin (g/dl) | 5.8 (12−15.5) |
| Hematocrit (%) | 17.5 (36−40) |
| Iron (μg/dl) | 135 (50−150) |
| TIBC (μg/dl) | 301 (360−400) |
| Transferrin saturation (%) | 45 (30−40) |
| Ferritin (μg/l) | 2440 (50−200) |
| Reticulocyte count (%) | 0.2 (0.5−1.5) |
| TLC (×103/mm3) | 3.3 (4−11) |
| Platelet count (×105/mm3) | 0.8 (1.5−4) |
iPTH, intact parathyroid hormone; Tf, transferrin; TIBC, total iron binding capacity; TLC, total leucocyte count.
Figure 2.
Radiological features of long bones of patient 2. (a) Severe rickets, diffuse osteopenia of long bones, and (b) diffuse osteopenia in pseudofractures in the tibia and fibula.
The SHPT triggered by the kidney disease did not relent even after beginning cinacalcet and sevelamer. The severe EPO resistant renal anemia required frequent blood transfusions. He was put on deferiprone due to development of iron overload. The child was lost to follow-up. A few months later, the patient passed away at home due to unknown causes.
Discussion
Various reports confirmed the relationship between severity of hematological manifestations and grade of myelofibrosis secondary to hyperparathyroidism. A landmark study by Rao et al. concluded that the severity of SHPT and the extent of bone marrow fibrosis increased the EPO dose required to maintain adequate Hct.11 In the poor response group, the mean EPO dose required to maintain the target Hct of 35% was dramatically higher compared with the good response group (176 U/kg 3 times a week vs. 56 U/kg 3 times a week).The mean serum PTH levels (880 ± 648 pg/ml vs. 266 ± 322 pg/ml) and the degree of bone marrow fibrosis (15.6 ± 16.4% vs. 1.1 ± 1.1%) were significantly greater in the poor response group. Another study on the positive effects of PTx in ameliorating the anemic status of uremic patients by Zingraff et al.12 and Barbour13 established a correlation between the amount of marrow fibrosis and rise in Hct after PTx. Those who showed a higher rise of Hct had a higher degree of bone marrow fibrosis at the time of surgery. Because responders and nonresponders had similar PTH plasma levels, both above authors concluded that the negative role of PTH in conditioning anemia was mediated by marrow fibrosis, similar to what was reported by Rao et al.11
Improvement in the cytopenias and restoration of Hct has been documented post-PTx, even in cases with severe renal osteodystrophy. This holds true in regard to our first case, who now requires a lesser dose of EPO and less frequent blood transfusions. Although the frequency of blood transfusions has decreased significantly, the need still persists. Transfusion-dependent anemia due to secondary or tertiary hyperparathyroidism traditionally has been an indication for PTx in end-stage renal disease patients.14, 15 A combined therapeutic approach using an i.v. vitamin D analog and cinacalcet serves as an equally efficacious alternative to PTx because it has consistently been shown to reduce the EPO requirement by abrogating myelofibrosis. Several uncontrolled studies have confirmed an increase in Hct levels with vitamin D therapy. Also, the use of cinacalcet in recent years has burgeoned because it suppresses PTH secretion and normalizes serum calcium in almost all patients within a few weeks.16, 17, 18, 19, 20 It has proven to be antiproliferative, and the apoptotic effects on parathyroid cells undoubtedly remain unmatched to date. Apart from that, the Action in Diabetes and Vascular Disease Preterax and Diamicron MR Controlled Evaluation (ADVANCE) and Evaluation of Cinacalcet HCl Therapy to Lower Cardiovascular Events (EVOLVE) trials have shown a statistically significant (P = 0.009) improvement in cardiovascular outcomes (measured by a reduction in coronary artery calcium scores) with cinacalcet therapy.21, 22 On the downside, a few studies demonstrated a 50% prevalence of adynamic bone disease in hypercalcemic, hyperparathyroid renal transplantation recipients on long-term calcimimetic therapy.23
Successful kidney transplantation can reverse many metabolic abnormalities, but abnormal bone turnover can persist in a significant proportion of renal transplantation recipients despite normal PTH levels. Chronic allograft nephropathy and preexisting SHPT were probably responsible for the nonresponsiveness of our first patient (case 1) to even a 6-month course of cinacalcet therapy, which made her an absolute candidate for surgery. PTx successfully reduced iPTH levels and ameliorated renal anemia, which was evident by the end of 6 months postoperatively. Hyperparathyroidism-related myelofibrosis usually lacks a general morphological sign of myelofibrosis (e.g., hepatosplenomegaly or leukoerythroblastosis), but interestingly, this was seen in our second case. This could also be an extrarenal manifestation of infantile nephronophthisis, but the NPHP-1 deletion analysis was negative. This finding corroborated with the high grade of myelofibrosis (grade MF-3) evident on bone biopsy, which rendered our patient pancytopenic. Unfortunately, he succumbed to his illness before PTx could be performed.
The previously underestimated role of bone marrow activity in deciding optimal graft survival has been highlighted recently with the emerging use of hematopoietic stem cells in the repair of ischemia and/or reperfusion damage to avoid delayed graft function. Myelofibrosis has been shown to drastically undermine the potential of hematopoietic stem cells for damage repair after kidney transplantation.24
Conclusion
It is important for clinicians to be vigilant for a deteriorating hematological and skeletal status in patients with refractory renal anemia and/or pancytopenia and severe MBD in CKD patients. It should be kept in mind that progressive hyperparathyroidism results in a progressive resistance of a bone marrow response to EPO treatment. It is therefore obvious that early control of PTH secretion is crucial for preventing MBD and worsening of cytopenias. An effective management of the calcium−phosphate balance with a combination of adequate dialysis, dietary restrictions, vitamin D analogs, cinacalcet, and phosphate binders should be a major objective in the early phase of treatment of uremic patients.
Disclosure
All the authors declared no competing interests.
References
- 1.Oliveira R.B., Cancela A.L., Graciolli F.G. Early control of PTH and FGF23 in normophosphatemic CKD patients: a new target in CKD-MBD therapy? Clin J Am Soc Nephrol. 2010;5:286–291. doi: 10.2215/CJN.05420709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sliem H., Tawfik G., Moustafa F., Zaki H. Relationship of associated secondary hyperparathyroidism to serum fibroblast growth factor-23 in end stage renal disease: a case-control study. Indian J Endocrinol Metab. 2011;15:105–109. doi: 10.4103/2230-8210.81939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trovato G.M., Iannetti E., Carpinteri G. Systolic function impairment in higher erythropoietin requirement patients in hemodialysis. Recenti Prog Med. 1997;88:217–222. [PubMed] [Google Scholar]
- 4.Wu S.G., Jeng F.R., Wei S.Y. Red blood cell osmotic fragility in chronically hemodialyzed patients. Nephron. 1998;78:28–32. doi: 10.1159/000044878. [DOI] [PubMed] [Google Scholar]
- 5.Meytes D., Bogin E., Ma A. Effect of parathyroid hormone on erythropoiesis. J Clin Invest. 1981;67:1263–1269. doi: 10.1172/JCI110154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delwiche F., Garrity M.J., Powell J.S. High levels of the circulating form of parathyroid hormone do not inhibit in vitro erythropoiesis. J Lab Clin Med. 1983;102:613–620. [PubMed] [Google Scholar]
- 7.McGonigle R.J.S., Wallin J.D., Husserl F. Potential role of parathyroid hormone as an inhibitor of erythropoiesis in the anemia of renal failure. J Lab Clin Med. 1984;104:1016–1026. [PubMed] [Google Scholar]
- 8.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD) Kidney Int Suppl. 2009;113:S1–S130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 9.Isakova T., Nickolas T.L., Denburg M. KDOQI US commentary on the 2017 KDIGO clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD) Am J Kidney Dis. 2017;70:737–751. doi: 10.1053/j.ajkd.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 10.Azevedo P.D.G.G., Cardoso P.S.R., Farah K.P. Complete reversal of bone marrow fibrosis after parathyroidectomy for secondary hyperparathyroidism. Br J Haematol. 2017;178:500. doi: 10.1111/bjh.14774. [DOI] [PubMed] [Google Scholar]
- 11.Rao D.S., Shih M.S., Mohini R. Effect of serum parathyroid hormone and bone marrow fibrosis on the response to erythropoietin in uremia. N Engl J Med. 1993;328:171–175. doi: 10.1056/NEJM199301213280304. [DOI] [PubMed] [Google Scholar]
- 12.Zingraff J., Drueke T., Marie P. Anemia and secondary hyperparathyroidism. Arch Intern Med. 1978;138:1650–1652. [PubMed] [Google Scholar]
- 13.Barbour G.L. Effect of PTx on anemia in chronic renal failure. Arch Intern Med. 1979;139:889–891. [PubMed] [Google Scholar]
- 14.D'Alessandro A.M., Melzer J.S., Pirsch J.D. Tertiary hyperparathyroidism after renal transplantation: operative indications. Surgery. 1989;106:1049–1055. [PubMed] [Google Scholar]
- 15.Gwinner W., Suppa S., Mengel M. Early calcification of renal allografts detected by protocol biopsies: causes and clinical implications. Am J Transplant. 2005;5:1934–1941. doi: 10.1111/j.1600-6143.2005.00938.x. [DOI] [PubMed] [Google Scholar]
- 16.Kruse A.E., Eisenberger U., Frey F.J., Mohaupt M.G. The calcimimetic cinacalcet normalizes serum calcium in renal transplant patients with persistent hyperparathyroidism. Nephrol Dial Transplant. 2005;20:1311–1314. doi: 10.1093/ndt/gfh924. [DOI] [PubMed] [Google Scholar]
- 17.Leca N., Laftavi M., Gundroo A. Early and severe hyperparathyroidism associated with hypercalcemia after renal transplant treated with cinacalcet. Am J Transplant. 2006;6:2391–2395. doi: 10.1111/j.1600-6143.2006.01475.x. [DOI] [PubMed] [Google Scholar]
- 18.Szwarc I., Argiles A., Garrigue V. Cinacalcet chloride is efficient and safe in renal transplant recipients with posttransplant hyperparathyroidism. Transplantation. 2006;82:675–680. doi: 10.1097/01.tp.0000232452.80018.ad. [DOI] [PubMed] [Google Scholar]
- 19.Srinivas T.R., Schold J.D., Womer K.L. Improvement in hypercalcemia with cinacalcet after kidney transplantation. Clin J Am Soc Nephrol. 2006;1:323–326. doi: 10.2215/CJN.00500705. [DOI] [PubMed] [Google Scholar]
- 20.Borchhardt K.A., Diarra D., Sulzbacher I. Cinacalcet decreases bone formation rate in hypercalcemic hyperparathyroidism after kidney transplantation. Am J Nephrol. 2010;31:482–489. doi: 10.1159/000304180. [DOI] [PubMed] [Google Scholar]
- 21.Raggi P., Chertow G.M., Torres P.U. The ADVANCE study: a randomized study to evaluate the effects of cinacalcet plus low-dose vitamin D on vascular calcification in patients on hemodialysis. Nephrol Dial Transplant. 2011;26:1327–1339. doi: 10.1093/ndt/gfq725. [DOI] [PubMed] [Google Scholar]
- 22.EVOLVE Trial Investigators. Chertow G.M., Block G.A. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367:2482–2494. doi: 10.1056/NEJMoa1205624. [DOI] [PubMed] [Google Scholar]
- 23.Wesseling-Perry K., Bacchetta J. CKD-MBD after kidney transplantation. Pediatr Nephrol. 2011;26:2143–2151. doi: 10.1007/s00467-011-1829-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bellavia M., Gioviale M.C., Damiano G. Is secondary hyperparathyroidism-related myelofibrosis a negative prognostic factor for kidney transplant outcome? Med Hypotheses. 2011;77:557–579. doi: 10.1016/j.mehy.2011.06.030. [DOI] [PubMed] [Google Scholar]