Abstract
Background
Universal healthcare coverage provides healthcare and financial protection to all citizens and might help to facilitate gender equity in care. We assessed the utilisation of hospital care services among women and men in a large underprivileged population with access to free hospital care in India.
Methods
The Rajiv Aarogyasri Community Health Insurance Scheme, a state-sponsored scheme, provided access to free hospital care for poor households across undivided Andhra Pradesh. Claims data for hospitalisations between 2008 and 2012 were analysed to determine the number of individuals, hospitalisations, bed-days and hospital expenditure for sex-specific and sex-neutral conditions, by sex, disease category and age group.
Results
A total of 961 442 individuals (43% women), 1 223 723 hospitalisations (48% women), 7.7 million bed-days (47% women) and hospital expenditure of US$579.3 million (42% women) were recorded. Sex-specific conditions accounted for 27% of hospitalisations, 12% of bed-days and 15% of costs for women, compared with 5%, 4% and 4% in men. Women had a lower share of hospitalisations (42%), bed-days (45%) and costs (39%) for sex-neutral conditions than men. These findings were observed across 14 of 18 disease categories and across all age groups, but especially for older and younger women.
Interpretation
In this large underprivileged population in India with access to free hospital care, utilisation of hospital care differed for women and men. For sex-neutral conditions, women accessed a smaller proportion of care than men, suggesting that coverage of hospital care alone is not sufficient to guarantee gender equity in access to healthcare.
Keywords: health policy, public health, epidemiology
Key questions.
What is already known?
Universal healthcare coverage (UHC) aims to ensure access to quality essential healthcare services for all who need it, without experiencing financial hardship.
Women are the majority of the world’s poor and might be major beneficiaries from UHC.
What are the new findings?
Among poor households with access to free hospital care in India, the proportion of women receiving hospital care for sex-neutral conditions was lower than for men across most disease categories and all age groups, but especially among the oldest and youngest women.
What do the new findings imply?
This study suggests that equal health coverage alone does not necessarily ensure equal access to essential health services.
Unless explicit attention is given to women and their barriers to accessing healthcare, movement towards UHC alone may be insufficient to achieve gender equity in healthcare
Background
Globally, there has been an increasing call for the implementation of universal healthcare coverage (UHC), as a means to ensure access to quality essential healthcare services for all who need it, without experiencing financial hardship.1 2
UHC is included in the United Nations Sustainable Development Goals,3 to be achieved by 2030, and is expected to provide full coverage of essential health services to everyone, and to lay the foundation for making progress towards several other Sustainable Development Goals, including ending poverty and improving gender equality.2 4
To date, at least half of the world’s population does not have full coverage of essential health services and about 100 million people are being pushed into extreme poverty because they have to pay for healthcare.1 Women are the majority of the world’s poor and therefore less able to afford healthcare than men.5 Hence, women are likely to be the major beneficiaries from UHC.6 7
The healthcare system in India is primarily administered by the states and private healthcare facilities are the primary source of healthcare for many households, resulting in substantial out-of-pocket, potentially catastrophic, health spending for poor households.8 9 The Rajiv Aarogyasri Community Health Insurance Scheme (RACHIS) is a state-sponsored scheme that provides access to free hospital care for economically marginalised households across undivided Andhra Pradesh in India.10–13 Introduced in 2007, the scheme provides household-level insurance for a wide range of surgical and medical treatments for a defined list of conditions. The RACHIS scheme has increased the use of hospital care of poor households, although disparities may exist.14–18 In particular, it is uncertain whether women and men have benefitted equally, which may not be the case considering that India has some of the world’s highest levels of gender inequality.19 The objective of this study was to use hospital claims data from the RACHIS to first examine the sex-specific utilisation of hospital care services, and to then determine whether differences exist in utilisation of care between women and men for sex-neutral conditions.
Methods
Study population
Data were used from the RACHIS for hospitalisations between 2008 and 2012. RACHIS, the largest state-funded health insurance scheme in India, provides access to hospital care for households with an annual income below INR60 000 (approximately US$1000 in 2014) in rural and below INR75 000 (US$1250) in urban areas across all 23 districts of undivided Andhra Pradesh (split into Andhra Pradesh and Telangana in June 2014).10–13 Beneficiary households can use free hospital services in a large network of public and private hospitals for up to INR150 000 per year (US$2500) per household, plus an extension of INR50 000 (US$833) under special circumstances. The coverage was shared between all members of the family. Health insurance is provided by a private insurer, with the premium paid by the state government at no cost to the beneficiaries. By 2012, RACHIS covered 18.8 of 22.1 million households, covering 81% of the population of undivided Andhra Pradesh. The scheme covers 912 hospitalisation billing codes which can be mapped to 674 unique procedures (online supplementary webtable 1) and to International Classification of Diseases, Tenth Edition, disease categories.20 The scheme excludes costs for cataracts and caesarean sections, which were covered by other schemes, and specific expensive and specialised treatments such as hip and knee replacements and bone marrow, heart and liver transplantations. Since demographic data for the entire beneficiary population were not available, we used data from the 2011 census for Andhra Pradesh to determine the age-sex distribution of the entire beneficiary population. These data showed that the proportions of women and men in the population were comparable (online supplementary webtable 2). Hence, sex differences in the use of hospital services are unlikely to be explained by differences in the sex distribution.
bmjgh-2018-000859supp001.pdf (712.2KB, pdf)
Hospital claims data
Data on the number of beneficiaries and the utilisation of hospital services were ascertained from hospital claims records published by the RACHIS administration.20 The number of bed-days was calculated as the difference between the date of primary procedure for a hospitalisation event and the date of discharge. The total amount claimed for all procedures (billing codes) associated with a hospitalisation event was used to calculate the hospital costs. Hospital costs were attributed to the primary condition for hospitalisation. Data on out-of-pocket expenses made by patients and/or households were not available.
Outcome measures
The primary outcome measures, by sex and disease group, are (1) number of unique individuals seeking care; (2) number of hospitalisation events; (3) number of bed-days used; and (4) expenditure in US$. Hospitalisations were classified as female-specific, male-specific and sex-neutral conditions. Female-specific conditions comprised childbirth-associated complications; diseases of the genitourinary system specific to female reproductive organs (ie, vagina, cervix, uterus, fallopian tubes and ovaries); and diseases of the breast. Male-specific conditions comprised diseases of the genitourinary system affecting male reproductive organs (ie, penis, testis, scrotum and prostate). All other conditions, including conditions of genitourinary system not affecting the reproductive organs, were classified as sex neutral. The billing code of the primary indication for hospitalisation was used to determine the sex specificity of a hospitalisation event and the type, duration and cost of care received.
Statistical analyses
Claims data for hospitalisations between 2008 and 2012 were used to calculate the number of individuals, hospitalisations, bed-days and hospital expenditure for sex-specific and sex-neutral conditions, by sex and disease category. We also calculated the women-to-men ratio of individuals, hospitalisations, expenditure and bed-day utilisation across disease categories and by age group.
Results
Between 2008 and 2012, a total of 961 442 individuals (43% women) accessed hospital care under the RACHIS, accounting for 1 223 723 hospitalisations (48% by women), 7.7 million bed-days (47% by women) and a hospital expenditure of US$579.3 million (42% by women) (table 1).
Table 1.
Utilisation of hospital care and resources by sex specificity of the condition
| Total, n (%) | Percentage of total women | Women, n (%) | Men, n (%) | |
| Number of individuals * | 961 442 | 43.1 | 414 042 | 550 219 |
| Sex-neutral conditions | 881 528 | 40.5 | 356 701 | 524 219 |
| Sex-specific conditions | 101 953 | 73.1 | 74 505 | 27 448 |
| Number of hospitalisations | 1 223 723 (100) | 48.2 | 590 053 (100) | 633 670 (100) |
| Sex-neutral conditions | 1 036 259 (84.7) | 41.7 | 432 295 (73.3) | 603 964 (95.3) |
| Sex-specific conditions | 187 464 (15.3) | 84.2 | 157 758 (26.7) | 29 706 (4.7) |
| Number of bed-days | 7 778 953 (100) | 46.6 | 3 627 901 (100) | 4 151 052 (100) |
| Sex-neutral conditions | 7 164 673 (92.1) | 44.5 | 3 189 275 (87.9) | 3 975 398 (95.8) |
| Sex-specific conditions | 614 280 (7.9) | 71.4 | 438 626 (12.1) | 175 654 (4.2) |
| Hospital expenditure in million USD | 593.9 (100) | 42.0 | 249.5 (100) | 344.4 (100) |
| Sex-neutral conditions | 543.2 (91.5) | 39.3 | 213.6 (85.6) | 329.6 (95.7) |
| Sex-specific conditions | 50.7 (8.5) | 70.8 | 35.9 (14.4) | 14.8 (4.3) |
*Row totals do not add up due to patients seeking care might have accessed care in both sex-neutral and sex-specific conditions. Values in bold are for all conditions.
The five leading causes of hospital care utilisation for women were genitourinary diseases (ie, diseases of the reproductive organs and the urinary system) (18%), neoplasms (ie, benign (not cancer) or malignant (cancer) tumours) (16%), injuries (14%), digestive diseases (12%) and circulatory diseases (10%) (online supplementary webtable 3). However, neoplasms accounted for the largest number of hospitalisations (38%) and bed-days used (38%), with the highest hospital expenditures for both neoplasms (20%) and circulatory diseases (20%). By comparison, the five leading causes of hospital care utilisation by men were injuries (22%), circulatory diseases (16%), genitourinary diseases (16%), digestive diseases (12%) and musculoskeletal conditions (12%) (online supplementary webtable 4). Injuries were also the leading cause of hospitalisations (20%) and bed-days (25%), but the highest hospital costs were associated with circulatory diseases (29%).
Sex-specific conditions
Sex-specific conditions accounted for 27% of hospitalisations, 12% of bed-days and 15% of hospital expenditure in women (table 1). Chemotherapy for breast cancer (9%), cervical cancer (6%), ovarian cancer (2%) and hysterectomy (5%) were the most frequent sex-specific indications for hospitalisation in women. In men, sex-specific indications accounted for 5% of hospitalisations, 4% of bed-days and 4% of hospital costs and included transurethral resection of the prostate (3%), surgical correction of hypospadias (1%), surgical management of undescended testis (0.3%) and chemotherapy for testicular cancer (0.2%).
Sex-neutral conditions
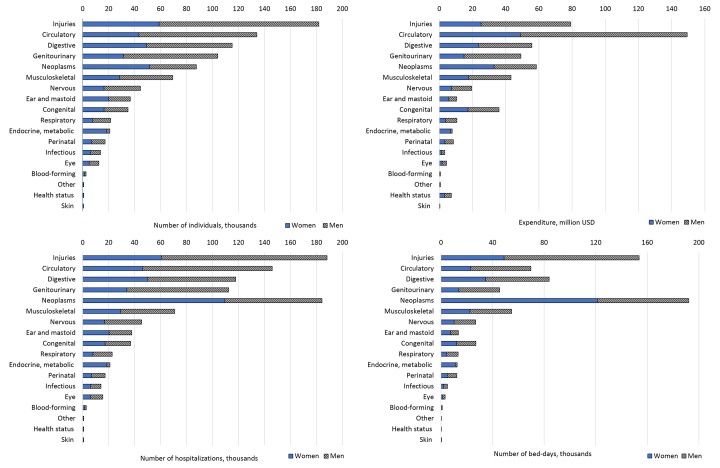
The five leading causes of hospital care utilisation for women for sex-neutral conditions were injuries (16%), neoplasms (14%), digestive diseases (14%), circulatory diseases (12%) and diseases of the genitourinary system (9%) (figure 1 and online supplementary webtables 5–8). However, neoplasms accounted for the largest number of hospitalisations (25%) and bed-days used (38%), with circulatory diseases (20%) accounting for the highest hospital costs (23%). By comparison, the five leading causes of hospital care utilisation by men for sex-neutral conditions were injuries (23%), circulatory diseases (17%), genitourinary diseases (13%), digestive diseases (12%) and musculoskeletal conditions (7%). Injuries were also the leading cause of hospitalisations (21%) and bed-days (26%), but the highest hospital costs were associated with circulatory diseases (31%).
Figure 1.
Number of unique individuals, hospitalisations, hospital expenditure and bed-days utilised, by sex and disease category.
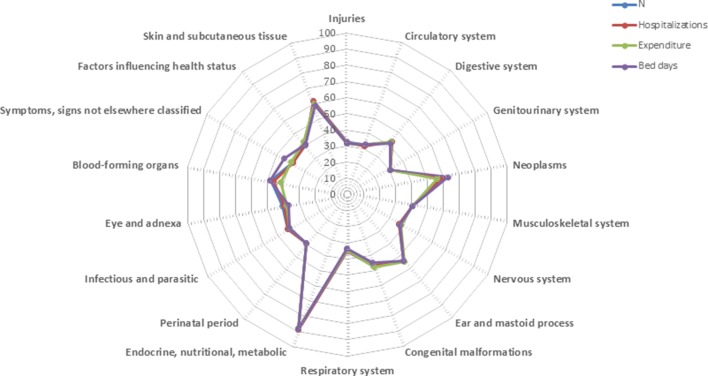
Sex differences in the utilisation of hospital care
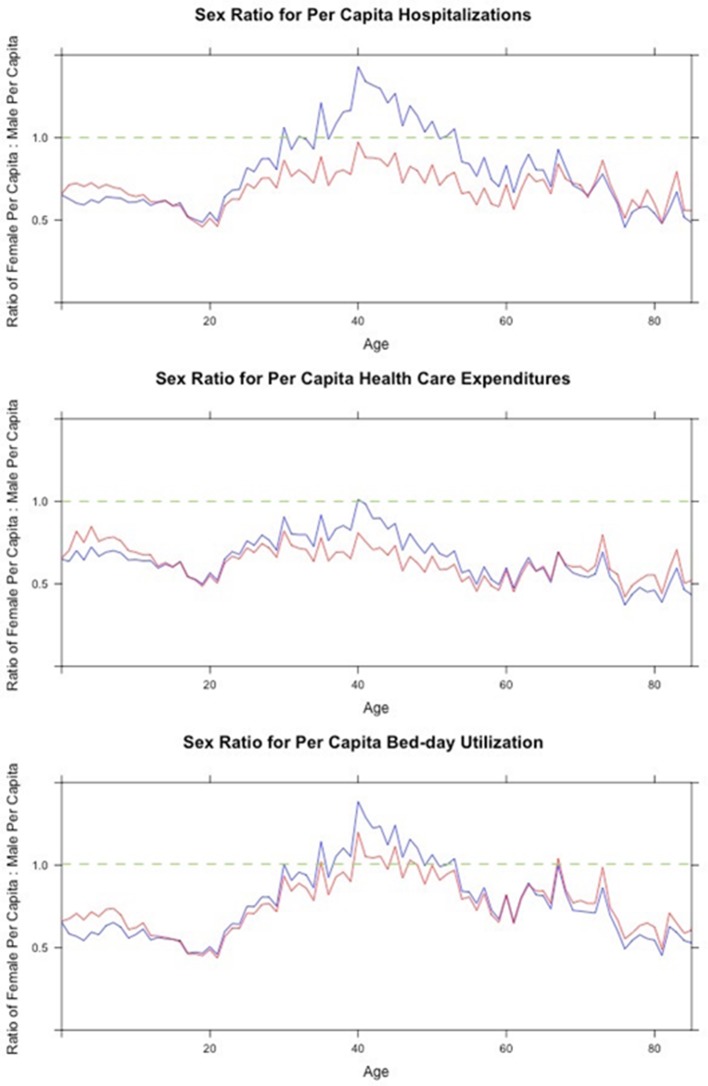
Women had a lower share of hospitalisation events (42%), bed-days (44%) and hospital costs (39%) than men (table 1). This finding was observed in 14 of the 18 disease categories (figure 2). In particular, less than a third of hospitalisations, bed-days and hospital costs for injuries, circulatory diseases and genitourinary diseases were for care provided to women. In contrast, about 55%–60% of care for neoplasms was for women and over 80% of the care for endocrine-related disorders was for women, largely driven by care related to thyroid disorders. The women-to-men ratio of sex-neutral hospitalisations, bed-days and hospital costs was below unity across all age groups, except for bed-day utilisation in those aged 40–50 years, which may be explained by hospitalisations for neoplasms in women (figure 3). The ratios were lowest in those in the oldest and youngest age groups.
Figure 2.
Women’s share in hospitalisations, hospital expenditure and bed-day utilisation across disease categories. Values represent the percentage of women among the total number of individuals, hospitalisations, expenditure and bed-days.
Figure 3.
Sex ratio of per capita rates of hospitalisation, hospital expenditure and bed-day utilisation. The blue line represents per capita values for all conditions and the red line represents per capita values for all sex-neutral conditions. A value of 1.0 represents equivalence between the sexes (green dotted line).
Discussion
This study evaluated the sex-specific utilisation of hospital care services in a marginalised population in South India with access to free hospital care through a state-funded insurance programme. Despite access to free hospital care, the proportion of women receiving inpatient care for sex-neutral conditions was lower than for men for all age groups, but especially for the youngest and oldest women, and across 14 of 18 disease categories.
Previous research on the impact of the RACHIS scheme on access to hospital care and out-of-pocket expenses has shown that the scheme has increased the use of hospital care of poor households.14–18 However, out-of-pocket expenses have increased over recent years, with evidence to suggest that the most vulnerable groups, such as female-headed households and those with the lowest education, remain disadvantaged and do not receive equitable healthcare.16 18 These data suggest that financial difficulties alone do not explain disparities in healthcare, and that other barriers, including gender inequity, might exist.15
Many leading health agencies, including the WHO and the World Bank, are promoting UHC as the best strategy to both ensure healthy lives for all and achieve gender equity.1 4 21 India is among the countries with the highest levels of gender inequality in the world,19 which is underpinned by poverty, social hierarchy and a strong patriarchal structure that disempowers and deprioritises the health of women.6 7 Lower empowerment in women may result in poor health, disparities in allocation of household resources, medical care and education.22 As the benefits of RACHIS are shared at household level, women’s lower empowerment could imply that the healthcare needs of men may be prioritised over those of women, especially among those beyond reproductive age. This, in turn, could explain why adolescent girls, young women and older women had considerably lower per capita rates for hospitalisations, bed occupancy and hospital expenditure as compared with men of the same age. Despite several initiatives to increase coverage of healthcare services to low-income groups,23 24 healthcare continues to be predominantly paid by out-of-pocket expenditure in India. Recent evidence from the India Human Development survey demonstrated that healthcare expenditure was systematically lower in women, regardless of demographic and socioeconomic characteristics.25 Hence, while RACHIS only provided access to free hospital care for poor households, educated women from middle to upper income households might equally encounter financial barriers in accessing quality healthcare.
It is critically important to use a gender lens in the design and implementation of UHC systems.4 7 26 Sex-based and gender-based differences between women and men result in differences in health risks, disease patterns and health service needs, each of which have a major impact on health-seeking behaviour, health status and access to health services. For example, there are major differences between men and women in the presentation of cardiovascular disease across the life course, with earlier onset of coronary heart disease in men and a greater propensity to stroke in women, which usually occurs at older age.27 28 Gender-based differences exist in many countries in terms of access to and control of household resources, power and decision-making, and roles and responsibilities within the family, labour market and society.4 Moreover, an increasing number of women provide informal care to their children and elderly parents, which is yet another reason for governments and health organisations to consider sex and gender in the development of UHC, thereby optimising their effectiveness and reducing gender inequality.4
Historically, a greater use of healthcare by women for sex-specific conditions has been attributed to gynaecological conditions and childbirth-related care in women of childbearing age.29 However, notwithstanding that this scheme does not provide coverage for a range of childbirth-related conditions, this study demonstrated that a quarter of all care used by women was for sex-specific indications beyond childbirth, including conditions of the genitourinary system and neoplasms of the breast, cervix and ovaries. Hence, sex-specific conditions continue to be a major driver of need for hospital care and resource utilisation by women after childbearing age. In the absence of UHC, there could be a huge unmet health need among women as these conditions are not covered under the reproductive health programmes.
Moving towards UHC requires progress on three fronts: the range of services that are available, the proportion of the costs of those services that are covered and the proportion of the population that is covered.30 While the RACHIS scheme provided access to free hospital care for poor households for a wide range of conditions, it did not provide full coverage on all fronts. Nevertheless, this study suggests that equal health coverage of hospital services alone does not necessarily ensure equal access to essential quality health services. Thus, unless explicit attention is paid to women and their differential health needs across the lifespan, movement towards UHC may not achieve gender balance, and might even exacerbate gender inequity.
The strengths of this study are the very large sample size and availability of data on number of hospitalisations, bed-days and hospital expenditure for various major causes of death and disability in a contemporary Indian population covered by free health insurance for hospital care. The use of different outcomes allowed for detailed analyses of various related, yet different, aspects of healthcare utilisation. Our results suggest that health utilisation was lower in women than men regardless of the outcome measure used. Our study has some limitations. First, our analyses were restricted to conditions covered by the RACHIS and, as such, did not include hospital care used for maternal and child health and infectious diseases which represent a large proportion of hospital care used in India. Moreover, care provided outside hospital included in RACHIS was not captured. Furthermore, no data were available on the number of individuals who needed hospital care for the conditions evaluated. However, while it might be that the lower utilisation rates in women are, in part, explained by differences in healthcare needs for some conditions, such differences alone are unlikely to fully account for the lower rate of hospital utilisation in women as compared with men. Inequity in access to healthcare, to women’s disadvantage, is more likely to be the major explanation for the present findings. Finally, although several mechanisms might explain our findings, we were unable to assess in detail the biological, social, economic and behavioural processes involved.
Conclusion
In this large underprivileged population in India with access to free hospital care, utilisation of hospital care differed between the sexes. Women had a greater share of hospital care for sex-specific conditions than men. For sex-neutral conditions, women accessed a smaller proportion of care than men, suggesting that coverage of hospital care alone is not sufficient to guarantee gender equity in access to healthcare.
Footnotes
Handling editor: Seye Abimbola
Contributors: MW, RN and VJ conceived the research. MS performed the statistical analyses. MS and SAEP drafted the article. All authors contributed critical intellectual content and made important revisions to the manuscript.
Funding: SAEP is supported by a UK Medical Research Council Skills Development Fellowship (MR/P014550/1).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. World Health Organization. Universal health coverage (UHC). 2017. http://www.who.int/mediacentre/factsheets/fs395/en/ (accessed 15 Jan 2018).
- 2. World Health Organization. Universal health coverage: a political choice. 2017. http://www.who.int/dg/speeches/2017/universal-health-coverage/en/ (accessed 15 Jan 2018).
- 3. United Nations. Sustainable Development Goals. http://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed 15 Jan 2018).
- 4. Rodin J. Accelerating action towards universal health coverage by applying a gender lens. Bull World Health Organ 2013;91:710–1. 10.2471/BLT.13.127027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. United Nations. The World’s Women 2015: Trends and Statistics. New York, United Nationn: Department of Economic and Social Affairs, Statistics Division, 2015. [Google Scholar]
- 6. Raj A. Gender equity and universal health coverage in India. Lancet 2011;377:618–9. 10.1016/S0140-6736(10)62112-5 [DOI] [PubMed] [Google Scholar]
- 7. Witter S, Govender V, Ravindran TKS, et al. Minding the gaps: health financing, universal health coverage and gender. Health Policy Plan 2017;32(Suppl 5):v4–v12. 10.1093/heapol/czx063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berman P, Ahuja R, Bhandari L. The impoverishing effect of healthcare payments in India: new methodology and findings. Economic and Political Weekly 2010;45:65–71. [Google Scholar]
- 9. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005–06. Mumbai: IIPS, 2005-06. [Google Scholar]
- 10. Aarogyasri Health Care Trust. Aarogyasri scheme. http://www.aarogyasri.telangana.gov.in/web/guest/aarogyasri-scheme (accessed 15 Jan 2018).
- 11. Government of Andhra Pradesh. NTR Vaidya Seva Scheme. http://www.ntrvaidyaseva.ap.gov.in/web/guest/ntr-vaidya-seva-scheme (accessed 15 Jan 2018).
- 12. Reddy S, Mary I. Rajiv Aarogyasri Community Health Insurance Scheme in Andhra Pradesh, India: a comprehensive analytic view of private public partnership model. Indian J Public Health 2013;57:254–9. 10.4103/0019-557X.123264 [DOI] [PubMed] [Google Scholar]
- 13. J. Yellaiah JY. Health Insurance in India: Rajiv Aarogyasri Health Insurance Scheme in Andhra Pradesh. IOSR Journal of Humanities and Social Science 2013;8:7–14. 10.9790/0837-0810714 [DOI] [Google Scholar]
- 14. Fan VY, Karan A, Mahal A. State health insurance and out-of-pocket health expenditures in Andhra Pradesh, India. Int J Health Care Finance Econ 2012;12:189–215. 10.1007/s10754-012-9110-5 [DOI] [PubMed] [Google Scholar]
- 15. Narasimhan H, Boddu V, Singh PV, et al. The best laid plans: access to the Rajiv Aarogyasri community health insurance scheme of Andhra Pradesh. Health, Culture and Society 2014;6:85–97. 10.5195/HCS.2014.163 [DOI] [Google Scholar]
- 16. Rao M, Katyal A, Singh PV, et al. Changes in addressing inequalities in access to hospital care in Andhra Pradesh and Maharashtra states of India: a difference-in-differences study using repeated cross-sectional surveys. BMJ Open 2014;4:e004471 10.1136/bmjopen-2013-004471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rao M, Ramachandra SS, Bandyopadhyay S, et al. Addressing healthcare needs of people living below the poverty line: a rapid assessment of the Andhra Pradesh Health Insurance Scheme. Natl Med J India 2011;24:335–41. [PubMed] [Google Scholar]
- 18. Rao M, Singh PV, Katyal A, et al. Has the Rajiv Aarogyasri Community Health Insurance Scheme of Andhra Pradesh addressed the educational divide in accessing health care? PLoS One 2016;11:e0145707 10.1371/journal.pone.0145707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. United Nations Development Programme. Human Development Report, Gender Inequality Index. 2016. http://hdr.undp.org/en/composite/GII (accessed 15 Jan 2018).
- 20. Shaikh M, Woodward M, Rahimi K, et al. Use of major surgery in south India: a retrospective audit of hospital claim data from a large, community health insurance program. Surgery 2015;157:865–73. 10.1016/j.surg.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 21. World Health Organization and International Bank for Reconstruction and Development / The World Bank. Tracking universal health coverage: 2017 global monitoring report. 2017.
- 22. Velkoff VA, Adlahka A. Women of the world: women’s health in India. 1998. https://www.census.gov/content/dam/Census/library/publications/1998/demo/wid98-3.pdf (accessed 24 Apr 2018).
- 23. Patel V, Parikh R, Nandraj S, et al. Assuring health coverage for all in India. Lancet 2015;386:2422–35. 10.1016/S0140-6736(15)00955-1 [DOI] [PubMed] [Google Scholar]
- 24. Reddy KS. India’s aspirations for universal health coverage. N Engl J Med 2015;373:1–5. 10.1056/NEJMp1414214 [DOI] [PubMed] [Google Scholar]
- 25. Saikia N, Bora JK. Gender Difference in health-care expenditure: evidence from india human development survey. PLoS One 2016;11:e0158332 10.1371/journal.pone.0158332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ravindran TK. Universal access: making health systems work for women. BMC Public Health 2012;12(Suppl 1):S4 10.1186/1471-2458-12-S1-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Leening MJ, Ferket BS, Steyerberg EW, et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ 2014;349:g5992 10.1136/bmj.g5992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 2011;124:2145–54. 10.1161/CIRCULATIONAHA.110.968792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mustard CA, Kaufert P, Kozyrskyj A, et al. Sex differences in the use of health care services. N Engl J Med 1998;338:1678–83. 10.1056/NEJM199806043382307 [DOI] [PubMed] [Google Scholar]
- 30. World Health Organization. Health systems financing: the path to universal coverage. Geneva, Switzerland, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2018-000859supp001.pdf (712.2KB, pdf)