Abstract
Background
Advances in human development sciences point to tremendous possibilities to promote healthy child development and well-being across life by proactively supporting safe, stable and nurturing family relationships (SSNRs), teaching resilience, and intervening early to promote healing the trauma and stress associated with disruptions in SSNRs. Assessing potential disruptions in SSNRs, such as adverse childhood experiences (ACEs), can contribute to assessing risk for trauma and chronic and toxic stress. Asking about ACEs can help with efforts to prevent and attenuate negative impacts on child development and both child and family well-being. Many methods to assess ACEs exist but have not been compared. The National Survey of Children’s Health (NSCH) now measures ACEs for children, but requires further assessment and validation.
Methods
We identified and compared methods to assess ACEs among children and families, evaluated the acceptability and validity of the new NSCH-ACEs measure, and identified implications for assessing ACEs in research and practice.
Results
Of 14 ACEs assessment methods identified, 5 have been used in clinical settings (vs public health assessment or research) and all but 1 require self or parent report (3 allow child report). Across methods, 6 to 20 constructs are assessed, 4 of which are common to all: parental incarceration, domestic violence, household mental illness/suicide, household alcohol or substance abuse. Common additional content includes assessing exposure to neighborhood violence, bullying, discrimination, or parental death. All methods use a numeric, cumulative risk scoring methodology. The NSCH-ACEs measure was acceptable to respondents as evidenced by few missing values and no reduction in response rate attributable to asking about children’s ACEs. The 9 ACEs assessed in the NSCH co-occur, with most children with 1 ACE having additional ACEs. This measure showed efficiency and confirmatory factor analysis as well as latent class analysis supported a cumulative risk scoring method. Formative as well as reflective measurement models further support cumulative risk scoring and provide evidence of predictive validity of the NSCH-ACEs. Common effects of ACEs across household income groups confirm information distinct from economic status is provided and suggest use of population-wide versus high-risk approaches to assessing ACEs.
Conclusions
Although important variations exist, available ACEs measurement methods are similar and show consistent associations with poorer health outcomes in absence of protective factors and resilience. All methods reviewed appear to coincide with broader goals to facilitate health education, promote health and, where needed, to mitigate the trauma, chronic stress, and behavioral and emotional sequelae that can arise with exposure to ACEs. Assessing ACEs appears acceptable to individuals and families when conducted in population-based and clinical research contexts. Although research to date and neurobiological findings compel early identification and health education about ACEs in clinical settings, further research to guide use in pediatric practice is required, especially as it relates to distinguishing ACEs assessment from identifying current family psychosocial risks and child abuse. The reflective as well as formative psychometric analyses conducted in this study confirm use of cumulative risk scoring for the NSCH-ACEs measure. Even if children have not been exposed to ACEs, assessing ACEs has value as an educational tool for engaging and educating families and children about the importance of SSNRs and how to recognize and manage stress and learn resilience.
Keywords: adverse childhood experiences, child health, resilience, measurement
Led by a new paradigm, scientists adopt new instruments…and see new and different things when looking with familiar instruments.
—Thomas Kuhn, The Structure of Scientific Revolutions, 1962
Our ever deepening understanding of the science of human development opens the door to possibilities for much needed improvements in child health and well-being in the United States and globally. These advances especially highlight the central role of social determinants of health and the importance of fostering safe, stable, nurturing relationships in infancy, childhood, and throughout life.1–4 It is now well known that the stress and trauma associated with disruptions in safe, stable, nurturing relationships affect children’s development, health, and well-being into adulthood.5–10 These advances inspire and require us to evolve models of care and use new measurement instruments to guide the design, delivery, and evaluation of health and human services, such as well-child care, early learning, social services, and other medical, public health, and social services.11–15
In particular, paradigm shifting neurobiological and epidemiologic findings show cumulative, cascading and multidimensional effects of trauma and stress associated with adverse childhood experiences (ACEs).10,16–20 ACEs include physical or emotional abuse or neglect, loss of a parent, family discord and divorce, and exposure to alcohol or drug abuse and mental illness in the home, or violence in the home or neighborhood.10,19 The high prevalence of ACEs in the child and adult population combined with evidence on their effect on health, life satisfaction, and social and medical care costs10,19,21–23 have now positioned ACEs as a matter of public health in the United States as well as globally.16–19,24,25 In this article we focus on the measurement of ACEs of children and families in research, public health, and clinical practice.
The most recent national, population-based data show that nearly one-half of US children have ACEs exposure and studies document the dose-response effect on child health status that has long been observed in studies on the adult population. Despite these findings, a recent national survey suggests that the majority of pediatric providers are not knowledgeable about the science related to ACEs and many barriers exist to integrate knowledge about ACEs into practice, including lack of information on methods to assess and respond to information about ACEs for children and families.12,15,26,27 Although studies confirm systematically higher rates of health status and school engagement problems among US children exposed to ACEs, they also document wide variations in outcomes among otherwise similar children who have equal exposure to ACEs. This raises questions about individual differences in sensitivity to ACEs and discerning appropriate approaches to discussing ACEs and interventions with families. Research on variations in the effect of ACEs point to the importance of protective factors, like nurturing relationships, teaching children how to be resilient, and supportive school and community environments, which can be viewed as falling outside of the purview of children’s health services.9,28–36 This can be true although national Bright Futures health promotion guidelines recommend pediatric providers address family psychosocial issues, like ACEs, and proactively promote healthy family relationships, resilience, and supportive community and school environments.37
Adding up the number of ACEs a person reports having been exposed to (or a parent reports a child has been exposed to) is termed “cumulative scoring.” This type of scoring challenges traditional notions about what is a more versus less severe traumatic experience or event. However, the ACEs dose-response effect consistently emerges in research irrespective of the specific ACEs involved. Although some analyses recommend scoring specific types of ACEs into subscales or groups,38,39 the analyses in these studies use reflective-based measurement models, which we suggest might not be appropriate for ACEs measurement. Reflective measurement models assume that an underlying latent variable causes responses on items. In this perspective, a child would have an underlying adversity level and that would cause the experiences of adversity. The use of alternative formative-based measurement approaches might be more appropriate because formative models assume that experiences of adversity (eg, witnessing violence) cause adversity.40 This will be addressed in this article.
To date, evidence on assessing ACEs in adults suggests that patients do not object to41 and find dialogue about ACEs empowering41,42 and some even see failure to inquire about ACEs as a denial of their occurrence and effect.43 Other studies suggest harm can be done when patients are not asked about adversities like ACEs, including missed or incorrect diagnosis, failure to adhere to treatment,44 revictimization,45 perpetuation of poor self-image, and failure to legitimize the effect of traumatic experiences, and increased mental illness symptoms and/ or substance abuse relapse.46 Barriers to assessing ACEs in practice have been reported to include provider discomfort with the topic, including their own history of adversity, and lack of training or clarity on resources and appropriate response to assessment of results.41,47 Worries that asking about ACEs will trigger severe traumatic reactions are of concern; although this has not been confirmed to occur or, if it does, to pose a clinical problem in research to date.47
Research documenting the role, value, and methods for assessing and addressing ACEs in child and family clinical contexts is beginning to emerge.13,15,48,49 However, many questions and controversies exist, including whether and how to directly inquire about ACEs with children and youth in addition to ACEs of parents, ensuring assessment promotes trust and empowers families and children, other information to collect simultaneously, data protection and confidentiality, and feasibility and practice redesign implications.12,27,50 Because assessing ACEs in clinical or community public health contexts is not yet well studied, we approached this study with neutrality as to the value, efficacy, and feasibility of ACEs assessment in practice. Rather, in this article we seek to contribute to efforts to examine methods for assessing ACEs should doing so be found to contribute to mitigating the effects of ACEs, preventing ACEs, and promoting resilience and social and emotional well-being among children and families. However, for purposes of this study, we did characterize the nature and purpose of ACEs assessment in 3 ways:
-
1
ACEs assessment relates to exposures to adverse experiences that can disrupt the safety, stability, and nourishing qualities of a child’s primary relationships and environment and that, in turn, pose risk for trauma and chronic stress linked to healthy development and well-being. Assessment of ACEs generates a measure of adversity-related risk.
-
2
ACEs assessment is intended to operate in a relationship-centered context to cultivate family engagement and education, to cultivate healing conversations, and to build awareness, strengths, resources, and support to address any trauma and chronic stress that may exist. ACEs assessment is not intended to diagnose trauma or provide adequate information on its own to guide specific clinical interventions. We view ACEs assessment as a relationship-centered method to spark dialogue with families and children about:
how ACEs might contribute to or influence healthy development and/or parenting;
how the trauma and chronic stress that ACEs can lead to might affect the diagnosis or treatment of current symptoms or health conditions;
identifying strengths, resources, and formal and informal supports.
In this way, ACEs assessment does not take the place of formal screening for current trauma or symptoms associated with past trauma, such as might be assessed using the National Child Traumatic Stress Network proposed “developmental trauma disorder” (DTD) diagnostic model and many other available instruments.51–54 ACEs assessment might point to the need to conduct such formal screening and treatment for complex trauma. Likewise, we have not viewed assessment of trauma symptoms to replace ACEs assessment because it has unique value to facilitate education and awareness about the effect of ACEs and possibilities for healing.
-
3
Even without current ACEs exposure, asking about ACEs in the context of a trusting relationship can facilitate a personalized dialogue with parents and children about how social and emotional experiences affect healthy development and well-being, the importance of safe and nurturing relationships, healthy stress regulation, and ways to prevent or minimize the effect of ACEs should they occur.
Specific objectives for this study were to: 1) characterize and compare, using a standardized framework, existing and emerging measures of ACEs in adult and child populations (part 1); and 2) evaluate psychometric properties and internal and external validity of the new childhood ACEs measure included in the National Survey of Children’s Health (NSCH)-ACEs,55 which provides data on ACEs nationally, for all US states and, potentially, counties and cities (part 2). Findings address practical questions about the feasibility, acceptability, validity, and approach to assessing ACEs in populations and in clinical and other practice contexts. We provide a Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) with: 1) more detailed information comparing ACEs measures reviewed in this report; 2) NSCH-ACEs population prevalence norms for US children according to age, household income, race and ethnicity, chronic disease, and health insurance status; 3) a reference list and links to the literature supporting selection of topics included in the initial specification of the NSCH-ACEs measure, the presentation of which is beyond the scope of this report; and 4) more in-depth analytic results, tables, and graphs as noted in the text. This study adds to existing early reports from the NSCH and other more narrowly focused US studies on childhood trauma19,23,56–58 by evaluating the measurement properties and validity of the NSCH-ACEs as it relates to its possible use in research, policy, and practice contexts.
Methods
Part 1: Comparison of ACEs Measurement Methods
To identify ACEs measurement tools for adults and children, we conducted a structured search of published research literature and reviewed online resources from federal, state, local, academic, and community-based health programs recognized as being engaged in activities related to ACEs. Key informant interviews with measure developers and early adopters of ACEs assessment in research, public health, and/or clinical practice confirmed our characterization of the tools reviewed in this report. These interviews also helped to identify these entities and assisted in identifying emerging ACEs measures not yet characterized in the published literature. Inherent in assessing exposure to ACEs among children is the fact that these adversities might still be taking place; thus, available measurement instruments to assess current exposures were also of interest. Although this is critical, a review of the many available measures58,59 to formally document the current occurrence of specific adversities are beyond the scope of this report, as are reviews of biomarkers and specific measures of chronic (or “toxic”) stress or, as noted previously, “DTD.” Likewise, although identified, broadly characterized, and referenced, companion guidelines for research, clinical, or program implementation and response to ACEs data collected from children and/or parents/families are not systematically compared or characterized in this report.
Currently, there is no consensus on a framework for evaluating ACEs measures, in part because ACEs measurement is only recently being used in clinical practice, where standardization of methods is more critical. As such, we specified a set of parameters for comparing ACEs measurement methods identified, including: 1) primary purpose and target population, 2) data source and collection methods, 3) types and numbers of adversities addressed, 4) scoring and reporting of results, 5) development and validation status, 6) concurrent information collected, and 7) availability of tools, user guidelines, and publications. Technical assistance logs from the Child and Adolescent Health Measurement Initiative’s Data Resource Center for Child and Adolescent Health further informed content to address when comparing methods. The 10 child-focused ACEs measurement methods identified for comparison in this report include: 1) the 2011/12 NSCH-ACEs,19,60 2) the National Survey of Child and Adolescent Well-being (NSCAW),61,62 3) the Yale-Vermont Adversity in Childhood Scale adult, youth, youth self-reported, and clinician-reported versions,63 4) Center for Youth Wellness Adverse Childhood Experiences Questionnaire child, youth, and youth self-reported versions,63,64 5) the Marie-Mitchell and O’Connor Child ACEs algorithm,14 6) the Montefiore Group Attachment Based Intervention study Clinical ACEs measure,42,65,66 7) Philadelphia Childhood Adversity Questionnaire (CAQ),18,67 8) Washington State University (WSU) ACEs tool for schools,68 9) WSU ACEs tool for Head Start, and 10) the Crittenton Foundation/Aspen Institute ACEs assessment tool.69–71 We also characterize and compare the child measures against the 4 adult ACEs measures identified: 1) the original Centers for Disease Control and Prevention (CDC) and Kaiser Permanente study ACEs measure,72,73 2) the state-level Behavioral Risk Factor Surveillance Survey (BRFSS) ACEs module,74–76 3) the World Health Organization’s (WHO) ACEs International Questionnaire,24,77,78 and 4) the Philadelphia Urban ACEs tool.18
Part 2: Assessment of the NSCH-ACEs
Data
We used data from the 2011/12 NSCH to evaluate the acceptability, efficiency, reliability, and validity of the NSCH childhood ACEs measure.60 The 2011/12 NSCH was the first to include a childhood ACEs measure in a nationally representative sample of US children. This measure is included in the 2016 NSCH and is expected to continue to be included on a yearly basis through the NSCH. Dr Braveman (coauthor of this paper) and a Technical Expert Panel to the federal Maternal and Child Health Bureau led the conceptualization, literature review, drafting, and rationale for the initial design of this measure. References and summaries of articles reviewed for this effort are included in the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf). The 2011/12 NSCH included the list of ACEs used in the original CDC/Kaiser adult ACEs study, with modifications overseen by a technical expert panel and evaluated using standard cognitive interviewing-based survey item testing through the CDC’s National Center for Health Statistics (NCHS). The NSCH-ACEs items were worded to minimize under-reporting associated with social desirability bias. The 9 topics included were selected as valid for report by parents and guardians on the basis of the observable nature of the ACEs evaluated. English and Spanish language cognitive testing (conducted by the National Opinion Research Center) with approximately 100 parents of children on the NSCH-ACEs confirmed content validity and did not result in recommended modifications to the NSCH-ACEs items. The NSCH surveyed a representative sample of children ages 0 to 17 years (95,677 children, with approximately 1800 per state). Child-level household surveys were conducted with parents or guardians under the leadership of the Maternal and Child Health Bureau and implemented through NCHS. Data were weighted to represent the population of noninstitutionalized children ages 0 to 17 years nationally and in each state.
Evaluation of the NSCH-ACEs: Acceptability, Efficiency, and Validity of Cumulative Scoring
Acceptability and efficiency
The acceptability of the NSCH-ACEs to parent/guardian respondents was first evaluated by calculating the prevalence of NSCH-ACEs unknown and missing values for each item, categorized into “don’t know,” “refused,” and “system missing” responses. Efficiency (or extent of collinearity) of the NSCH-ACEs items was assessed by calculating the correlation across ACE items as well as item-total correlations and, for each ACEs item/topic, calculating the proportion of children with only this 1 ACE, up to 2 other ACEs, or 3 or more other ACEs among the 9 assessed.
Internal validity of NSCH-ACEs score
The extent to which the questions included in a measurement tool measure the underlying construct(s) (in this report, ACEs/adversity-related risk) as hypothesized is called internal validity.55,79 For example, creating a single composite ACEs score from the NSCH-ACEs items implicitly assumes that the NSCH-ACEs items measure a single ACEs/adversity-related risk construct. Importantly, a lack of internal validity can lead to spurious conclusions. Thus, it is critical to evaluate whether the data support the hypothesis that NSCH-ACEs measure a single construct. Latent (unobserved) variable measurement models use a set of equations to describe how people tend to answer questions. They provide a flexible method for evaluating internal validity. ACEs present a unique challenge with respect to evaluating internal validity. It is hard to argue that there is a latent ACEs construct that exists and causes individuals to experience adversity. Rather, children have adverse experiences and these form a latent variable that is a measure of these adverse experiences. The former type of model is called a reflective model and the later a formative model.40,80
Much of measurement theory and the statistical models that accompany it center on reflective models. In the reflective vein, confirmatory factor analysis (CFA) is frequently used to evaluate internal validity. With CFA, one could test the hypothesis that a single factor (unidimensional) CFA model fits the data well and sufficiently explains the covariance among item responses.81,82 This would support the creation of a single summary score from NSCH-ACEs item responses. CFA has been used to evaluate the CDC/Kaiser and BRFSS adult ACEs measures. For consistency, we also use CFA in this study to assess the child-focused NSCH-ACEs. Because conceptually, ACEs are more aligned with a formative measurement approach, we also used 3 different structural equation modeling (SEM) methods to specify the latent variable and evaluate the relationship between the underlying construct measured by the NSCH-ACEs items and 5 predictors: having an ongoing chronic condition requiring more complex services; having emotional, behavioral, or developmental problems; usually or always being engaged in school; having repeated a grade in school and exhibiting 1 critical and observable aspect of resilience—usually or always being able to stay calm and in control when faced with a challenge.
The first of the 3 approaches is a formative approach suggested by Bollen83 that constrains the residual variable of the latent adversity variable and items to 0 and is statistically identified through the regression of the latent variable on the predictor variables in the model. The second SEM approach is also a formative approach suggested by Treiblmaier et al84 that uses the parameters from canonical correlation to create indicators for the latent adversity variable and overcome the 0 residual variance limitation. The latent variable is then regressed on the predictors. The third SEM approach treats adversity as a reflective variable (as in traditional CFA) and regresses the latent variable on the predictors. We included a reflective approach because of our interest in the covariance among ACEs items and concerns about the state of the art in formative variable assessment methods raised in the literature.40,80,81 Using these different approaches all set within SEM allowed us to compare the results across models (fit as well as parameters), with convergence providing support for the internal validity of a latent ACEs construct from a variety of perspectives. It also allowed us to examine predictive validity (whether ACEs predict the key child health and school outcomes assessed). However, it is important to note that, although we used reflective as well as formative analytical approaches, the concept of ACEs as used throughout this report, is inherently formative.
Last, rather than seeking to create a single continuous score, one might wish to categorize children into nominally different groups on the basis of the types and patterns of ACEs children have experienced. We used latent class analysis (LCA) to further investigate the suitability of using item response patterns to create typologies. Consistent with recommendations,85,86 we first fit a model with 2 latent classes and attempted to increase the number of classes until the adjusted Bayesian information criterion began to increase in value indicating the potential numbers of scoring typologies to consider for the NSCH-ACEs.86 In addition, we examined whether the Lo-Mendell-Rubin likelihood test suggested the addition of an extra class. For CFA, we used the weighted least squares mean and variance adjusted estimator. For SEM, we used the robust maximum likelihood estimator with a logit link. Finally, to further examine use of cumulative versus categorical or topic-specific scoring, we assessed whether specific NSCH-ACEs items have a unique explanatory effect on key outcomes. To do so, we ran separate multivariate regression models on whether a child had an emotional, mental, or behavioral health (EMB) condition for each NSCH-ACEs item and compared findings with cumulative scoring methods. Unless otherwise noted, all adjusted odds ratios that we report in this article are significant on the basis of their 95% confidence intervals.
Population-Based Versus High-Risk Assessment
To inform practice based decisions on whether to assess ACEs on a population-based level (for all children and families) or to target assessment to subgroups according to risk, especially poverty, we evaluated the differential effect of ACEs across child household income groups. In this evaluation, we separately evaluated key child outcomes for each of 4 household income subgroups (below federal poverty level [FPL], 100%–199% of the FPL, 200%–399% of the FPL, and ≥400% of the FPL) across 4 NSCH-ACEs score categories (0, 1, 2–3, ≥4). Outcomes assessed were: 1) whether a child has a special health care need that is more (vs less) complex (complex children with special health care needs [CSHCN]), 2) experienced an emotional, behavioral, or developmental health condition, 3) demonstrated aspects of resilience (defined in the survey as “staying calm and in control when faced with a challenge,” for children ages 6–17 years), or 4) was engaged in school (ages 6–17 years); chi-square tests of statistical difference and stratified multivariate logistic regression analyses were used to evaluate differences observed across NSCH-ACEs score levels for each child household income group. All regression models controlled for a child’s age, sex, race and ethnicity, and insurance status. For regression models for which resilience and school engagement were the outcomes of focus, we also adjusted for a children’s special health care needs status. Methods for constructing all variables are available in codebooks accessible at www.childhealthdata.org. For NSCH-ACEs-related analyses other than CFA, SEM, and LCA, we used SPSS Complex Samples, version 22 (IBM Corp, Armonk, NY). For all CFA, LCA, and SEM analyses we used Mplus, version 7 (Muthén & Muthén, Los Angeles, Calif), which allowed us to appropriately include the survey design information and weights.
Results
Part 1: Comparison of ACEs Measurement Methods
Purpose
All but 5 of the 14 ACEs assessment tools evaluated were initially designed and used for public health assessment, research, or for program and policy planning purposes. Although 5 were specified for use in clinical and/ or service delivery contexts, they nonetheless share many similarities with the other 9 tools in terms of topics included and administration methods used, including methods to assist respondents who might request resources on ACEs (Table 1).
Table 1.
Summary and Comparison of Methods to Assess ACEs
| ACEs Measurement Tool Name and Sponsor | TP, PP, and DS | Adversity Content* | Scoring and Reporting Convention† | DH, TVS, and IG | Concurrent Content Included | Comparison With NSCH-ACEs; AQ and UAT Versus NSCH |
|---|---|---|---|---|---|---|
| Original ACE Study (CDC and Kaiser Permanente, San Diego Health Appraisal Clinic)10,21,72,73,87 | TP: Adults about self PP: Research DS: Self-report |
No.: 28 questions; 10 topics Types: PA, PN‡, EA, EN‡, SA, HHSA, HHMI, DV, DIV‡, J Age: some§ FIE: some§ |
CS: 0–10 (0–7 in first wave) CA: 0, 1, 2–3, ≥4 typical |
DH: Used/adapted available questions (eg, Conflict Tactics Scale; Childhood Trauma Questionnaire; Wyatt (sexual abuse), etc) TVS: Testing and validation occurred in the context of the study, although no publications specific to this were found IG: Questionnaires available on CDC ACEs page |
Demographic characteristics, health history, current conditions and symptoms | AQ: PN, EN, PA, SA, EA UAT: PD, CNV, DIS, economic hardship |
| WHO ACE-International Questionnaire; sponsored by International ACE Research Network (led by WHO and CDC)16,24,77,78 | TP: Adults about self PP: Advocacy, program planning, and international comparisons DS: Self-report |
No.: 29 questions; 13 topics Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, DIV/PD, J, B, CNV, OE Age: no FIE: some |
CS: 0–13 CA: Not specified O: Binary and frequency (only some “yes” responses count) scoring |
DH: Used all from BRFSS and added questions to increase international cultural applicability TVS: Field testing done in 6 countries; currently undergoing reliability and validity testing IG: Interview guidelines, scoring metrics, and other supporting documents available |
Demographic characteristics, marriage, and family information | AQ: PA, PN, EA, EN, SA, B, OE UAT: DIS, economic hardship |
| BRFSS; sponsored by the CDC22,74–76,88,89 | TP: Adults about self PP: State policy and practice DS: Self-report |
No.: 11 questions; 8 topics Types: PA, EA, SA, HHSA, HHMI, DV, DIV, J Age: no FIE: some§ |
CS: 0–8 CA: 0, 1, 2, 3, 4, ≥5 |
DH: Modified from original CDC/Kaiser study TVS: Focus group testing; factor analysis IG: Interviewer script; information about state implementation, some analysis guidelines (all for overall survey) |
Many other health modules, no other questions in ACEs module | AQ: PA, EA, SA UAT: PD, CNV, DIS, economic hardship |
| NSCH-ACEs19,23,28,60 | TP: Adults about child PP: Research DS: Parent-report |
No.: 9 questions; 9 topics Types: HHSA, HHMI, DV, DIV, J, PD, CNV, DIS, OI Age: no FIE: no |
CS: 0–9 CA: 0, 1, ≥2 |
DH: Adapted from original CDC/Kaiser study for parent-reported survey TVS: Extensive cognitive and pilot testing IG: Information on survey implementation, scoring, reporting, and microdata available |
Physical and emotional health; health care access, insurance, medical homes, family interactions, parental health, school experiences, and safe neighborhoods | |
| Center for Youth Wellness ACE-Questionnaire Child, Teen, and Teen Self-Report64 | TP: Adults about child (Child and Teen versions) and child about self PP: Health care services DS: Parent- and self-report |
No.: 17 or 19 questions¶; 17 or 19 topics¶ Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, DIV, J, B, PD, CNV, DIS, OI, OE Age: no FIE: no |
CS: 0–17/0–19¶ CA: 0–3 (no symptoms), 0–3 (with symptoms), ≥4 |
DH: Original CDC/Kaiser questions, additional questions from experts and community stakeholders TVS: Under way IG: User guide (background, implementation, scoring) and questionnaires available for download to health care professionals |
None; intended as part of primary care visit | AQ: PA, EA, EN, SA, B, OI, OE UAT: economic hardship |
| Y-VACS; Sponsored by National Institute for Mental Health63 | TP: Adults about child, child about self, and adults about self PP: Health care services, research DS: Parent-, clinician-, and self-report |
No.: 20 questions; 20 topics each (4 different versions) Types: PA, PN, EA, SA, HHSA, HHMI, DV, DIV, J, B, CNV, OI, OE Age: no FIE: yes |
CS: 0–20 CA: Not specified# O: Each item scored 0–2 on frequency and 1–3 on severity |
DH: Adapted from original CDC/Kaiser questions, additional questions added on the basis of common “other” responses in initial draft# TVS: Inter-rater reliability analyses performed# IG: Questionnaires available on request from authors# |
None | AQ: PA, EA, SA, B, OI, OE UAT: PD, DIS, economic hardship |
| The Institute for Safe Families/ACE Task Force Philadelphia Urban ACE Study; Sponsored by Robert Wood Johnson Foundation67 | TP: Adults about self PP: Research/policy recommendations DS: Self-report |
No.: 22 questions; 14 topics Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, J, B, CNV, DIS, OI Age: no FIE: some§ |
CS: 0–14 CA: 0, 1–3, ≥4 |
DH: Used original CDC/Kaiser questions, added questions to make applicable to an urban population TVS: Logistic regression done to test associations between original CDC and additional ACEs scores and demographic characteristics IG: Questionnaire and overall methodology information available in report |
Past/current health conditions, sexual history, drug use | AQ: PA, PN**, EA, EN, SA, B, OI UAT: PD, DIV |
| NSCAW; Sponsored by the Office of Planning, Research, and Evaluation, Administration for Children and Families90,91 | TP: Adults about child PP: Research DS: Parent-, caregiver-, and caseworker-report (and CPS reports) |
No.: 21 questions; 10 topics Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, DIV/PD, J Age: no FIE: no |
CS: 0–10 CA: 0, 1, 2, 3, ≥4 |
DH: Mapped CDC/Kaiser ACEs constructs to questions that already existed in NSCAW TVS: None documented (questions mostly from already validated scales, such as the Childhood Trauma Scale)# IG: None available (data sets can be requested by researchers via National Data Archive on Child Abuse and Neglect at Cornell University)# |
Physical, mental, and emotional well-being and functioning, family characteristics, community environment, and service needs and use | AQ: PA, PN, EA, EN, SA UAT: PD, CNV||, DIS, economic hardship|| |
| Marie-Mitchell and O’Connor Child ACE tool; Sponsored by the Commonwealth Fund via the Academic Pediatric Association Young Investigator Award14 | TP: Adults about child PP: Primary care practice DS: Parent-report and medical records |
No.: 6 or 7 questions††; 6 or 7 topics†† Types: HHSA, HHMI, DV, J, OI (could include PA, PN, EA, EN, SA, DIV, PD), OE Age: no FIE: no |
CS: 0–6/0–7†† CA: 0–2, 3–6/3–7†† |
DH: Developed from risk factors described in the literature on ACEs TVS: Pilot testing only IG: None |
Developmental screening, child health status, and health care use | AQ: OI (could include PA, PN, EA, EN, SA) UAT: CNV, DIS, economic hardship |
| Montefiore—Clinical ACE questionnaire Adult/Child65,66 | TP: Adults about child and adults about self PP: Health care services DS: Parent- and self-report |
No.: 25 questions; 10 topics Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, DIV, J Age: no FIE: some§ |
CS: 0–10 CA: 0–3, ≥4; 0, 1, 2, 3, ≥4 |
DH: Modified slightly from original CDC/Kaiser questions TVS: Validated for Group Attachment-Based Intervention use by analyzing association between ACEs and unresolved/cannot classify outcomes on the Adult Attachment Interview IG: Implementation described in article by Murphy et al42 |
None in ACEs questionnaire, study also includes items on body mass index and stressors | AQ: PA, PN, EA, EN, SA UAT: PD, CNV, DIS, economic hardship |
| WSU ACEs tool for schools; Sponsored by the Spokane County Community Network with funds awarded by the Washington State Family Policy Council49,68 | TP: Adults about child PP: Research DS: Teacher-report |
No.: 11 topics Types: PA, PN, EA, SA, HHSA, HHMI, DV, DIV, J, PD, CNV, OI Age: no FIE: no‡‡ |
CS: 0–11 CA: 0, 1, 2, ≥3 O: Asked lifetime as well as past year prevalence |
DH: Modified from original CDC/Kaiser questions TVS: None shown IG: None available |
Demographic characteristics, academic problems, health concerns | AQ: CPS report (including PA, EA, SA), PN, OI UAT: DIS, economic hardship‡‡ |
| WSU ACEs tool for Head Start; Sponsored by Office of Juvenile Justice and Delinquency Prevention, Office of Justice Programs, US Department of Justice49,68 | TP: Adults about child and adults about self PP: Research DS: Parent- and self-report |
No.: 9 topics Types: PA, EA, EN, SA, HHSA, HHMI, DV, DIV, J, OI Age: no FIE: no |
CS: 0–9 CA: varies |
DH: Modified from original CDC/Kaiser questions TVS: None shown IG: None available |
Demographic characteristics, child development, child adjustment | AQ: EA, EN, CPS report (including PA, SA), OI UAT: PD, CNV, DIS, economic hardship |
| Children’s Hospital of Philadelphia CAQ (under development); Sponsored by the Stoneleigh Foundation | TP: Adults about child and older children about self# PP: Community organization# DS: Parent- and self-report# |
No.: 8 topics# Types: PA, PN, EA, EN, SA, DIV, DIS, OI#(under development) Age: unknown# FIE: unknown# |
CS/CA: Under development# | DH: Questions created from statements from interviews with children and youth impacted by ACEs# TVS: None yet# IG: None available# |
Demographic characteristics, protective factors (eg, positive relationship and coping skills)# | AQ: PA, PN, EA, EN, SA# UAT: DIV (uses single parent)# (under development) |
| The National Crittenton Foundation’s ACEs Survey; Aided by Dr. Roy Wade for development and implementation69–71 | TP: Adults about child and adults about self PP: Social services, program planning DS: Parent- and self-report |
No.: 10 topics Types: PA, PN, EA, EN, SA, HHSA, HHMI, DV, DIV, J Age: no FIE: no |
CS: 0–10 CA: 0, 1, 2, 3, ≥4; 0, 1–3, 4–7, 8–10 |
DH: Questions ACEs# TVS: None# IG: Extensive provider implementation guidelines and tips available in toolkit |
Demographic characteristics, well-being assessment (stress, coping, and connection to adults) | AQ: PA, PN, EA, EN, SA UAT: PD, CNV, DIS, economic hardship |
ACE indicates adverse childhood experience; AQ, additional questions; B, bullying; BRFSS, Behavioral Risk Factor Surveillance Survey; CA, categorical score; CAQ, Childhood Adversity Questionnaire; CDC, Centers for Disease Control and Prevention; CNV, community and neighborhood violence; CPS, Child Protective Services; CS, continuous score; DH, design highlights; DIS, discrimination; DIV, parents divorced; DS, data source; DV, domestic violence; EA, emotional abuse; EN, emotional neglect; HHMI, household mental health problem; HHSA, household alcohol or substance abuse; IG, implementation guidelines available; J, parent incarcerated/spent time in jail; NSCAW, National Survey of Child and Adolescent Well-being; NSCH, National Survey of Children’s Health; OE, other environmental/extrapersonal trauma; OI, other interpersonal trauma; PA, physical abuse; PD, parental death; PN, physical neglect; PP, primary purpose; SA, sexual abuse; TP, target population; TVS, testing and validation status; UAT, unaddressed topics; WHO, World Health Organization; WSU, Washington State University; and Y-VACS, Yale-Vermont Adversity in Childhood Scale.
See the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) for more details on each instrument.
For adversity content, No. indicates number of adversity topics and number of survey items; Types indicates type of adversity; Age indicates the age at which the adverse childhood experience occurred; and FIE indicates frequency, intensity, or effect.
O indicates scoring and reporting convention other than continuous or categorical.
Included in second wave of study only.
Not included in scoring mechanisms.
Included in the larger NSCAW, but not in the questions used for the ACEs scale.
Multiple questionnaire versions for different people (eg, parents, children, clinicians, adults about themselves).
Personal communication: for NSCAW, M.B. Webb, September 29, 2015; for Y-VACS, J. Hudziak, October 7, 2015; for CAQ, R. Wade, November 2, 2015; for Crittenton, S. Lopez, March 17, 2016.
Covers the same information as in the NSCH question on economic hardship, but is considered to be a question on physical neglect.
One questionnaire with multiple options for scoring (can use with or without question on maternal education).
This information derived from reports on the study; the tool itself was not available to examine.
Data Source and Collection Methods
Person-reported methods (adult, parent, child, or youth) are used for 13 of the 14 methods evaluated, with 1 exception—the WSU School ACEs tool, which is teacher-reported only. In addition, teacher, clinician, caseworker, and/or medical record data sources are used in 4 of the 14. Age 8 years is the youngest age at which children are recommended to be asked about ACEs (CAQ—under development; Table 1).
Number of Constructs and Survey Items
The number of constructs included ranges from 6 to 20 across the 13 methods for which this information is known (not including the CAQ, which is under development). All but 2 tools have 14 or fewer constructs. Some tools have multiple versions with slightly varying construct and item counts. The 11 tools for which detailed item-specific information is available (not including the CAQ or WSU tool) contain between 6 and 29 ACEs-specific survey items, with 6 of 11 using multiple items to measure 1 or more of their constructs. The greatest number of items were included in the WHO’s ACEs assessment survey. Of the 13 non-NSCH-ACEs tools, all include additional questions to the NSCH-ACEs, primarily in areas deemed invalid to ask parents about in a national survey context (eg, emotional or sexual abuse).
ACEs Topics Addressed
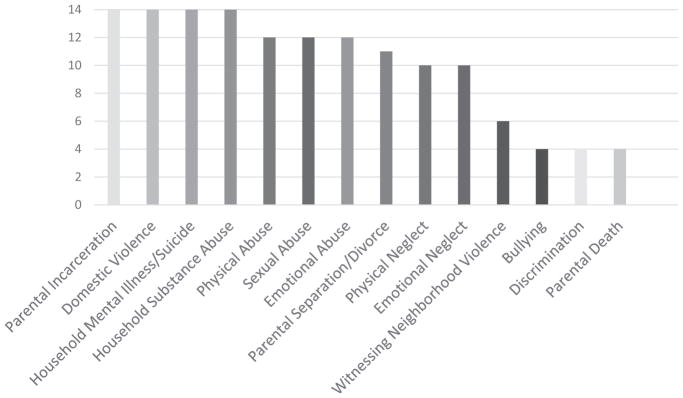
As summarized in Figure 1, each of the 14 ACEs assessment tools included items on parental incarceration, domestic violence, household mental illness/suicide, and household substance abuse. Physical abuse, sexual abuse, and emotional abuse were included in 12, parental separation/divorce in 11, physical neglect in 10, and emotional neglect in 9. Four tools (BRFSS, NSCAW, Montefiore Clinical ACE questionnaire, and Crittenton/Aspen ACEs Survey) only use constructs from the original CDC/Kaiser study; the other tools added between 1 and 9 constructs each. The most common of these additional constructs include witnessing neighborhood violence (6 tools), bullying (4 tools), discrimination (4 tools), and parental death (4 tools). More information about the specific wording of the items across the original CDC/Kaiser and common additional constructs can be found in the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) to this article and references noted in Table 1.
Figure 1.
Prevalence of assessment of particular ACEs among 14 tools evaluated in this article.
Scoring and Reporting Results
Each of the 13 tools for which this information is available (not including CAQ) report findings using a continuous scoring mechanism in which each construct is weighted equally and given 1 “point.” However, some tools include graded response options (such as never, once or twice, sometimes, often), which are all dichotomized in some way to provide an overall ACEs score. Most tools also represent scores in numeric categories, such as 0, 1, 2 to 3, and ≥4 ACEs. None of the tools alter scoring on the basis of the age an individual was when exposed to ACEs. Two tools, the WHO ACEs International Questionnaire and the Yale-Vermont Adversity in Childhood Scale, have a mechanism for incorporating the frequency with which an individual experienced an ACE into the scoring. See the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) and references noted in Table 1 for information on these mechanisms.
Testing and Validation
Survey items included in each tool are adopted or adapted from those included in the original CDC/Kaiser ACEs study instrument, which was itself primarily developed using constructs from existing theoretical and empirical research and survey items from previously developed and tested tools (eg, the Childhood Trauma Questionnaire). Information about testing and validation varied widely across ACEs measurement methods. Some reported no documented testing/validation whereas others reported extensive cognitive testing, focus group discussions, pilot testing, and use of statistical modeling and factor analysis to assess scoring and internal validity. No reviews of unknown/missing reports, nor more extensive psychometric testing using SEM or LCA methods used in our study were found. When cognitive testing, pilot testing, or statistical analyses were conducted, in no cases were specific problems regarding the reliability, validity, acceptability, or feasibility of implementing the ACEs survey items noted. More information on the particular testing and validation for individual tools is included in Table 1, in the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf), and references included in Table 1.
Additional Content Assessed
Nearly all ACEs tools identified (12 of 14) are recommended for use in conjunction with other questionnaires or as part of a larger survey. Aside from basic demographic questions, the most commonly asked additional questions covered topics such as current and past health history, health care access, and overall well-being, resilience, and other types of protective factors, like supportive relationships in the home, school, or community.
Recommendations for Administration
Documentation for 11 of the 14 tools include some type of guidance for introducing and framing ACEs questions with respondents and/or for what to do in response to ACEs disclosed by respondents. Three main types of guidance are provided: 1) prefacing (8 tools: eg, explaining that questions ask about sensitive topics and participants can choose not to answer), 2) follow-up (7 tools: in the form of either a referral to services or information from a clinician), and 3) training guidelines (6 tools: guidelines for health care or other service providers or survey administrators). See the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) and references included in Table 1 for more information.
Part 2: Assessment of the NSCH-ACEs
Acceptability and Efficiency
Regarding NSCH-ACEs acceptability and efficiency, when children whose parents were not administered the NSCH-ACEs items because they dropped off before these items were not included, the NSCH-ACEs survey items had rates of missing or unknown values <1%. Increases in survey drop-off rates were not observed either during or after the administration of the NSCH-ACEs items. Unknown/missing value rates are commensurate with nearly all other NSCH survey items where unknown values (“don’t know,” “refused”) and skipped/missing values make up <1.5% of the responses to any single question; with notable exceptions for household income (9.7% nationwide), body mass index for age (4.8% nationwide), and race/ethnicity (2.7% nationwide). The “difficult to get by on income” NSCH-ACEs item had the highest proportion of “refused” responses (0.5%) and witnessing domestic (0.6%) or neighborhood (0.5%) violence and experiencing discrimination (0.5%) had the highest levels of “don’t know” responses (Table 2). For all but 1 of the NSCH-ACEs items (difficult to get by on income), 70% to 91.4% of children with an affirmative response to 1 item was accompanied by an affirmative response to at least 1 other NSCH-ACEs item. For 5 of the 9 items, >40% of those with an affirmative response also had an affirmative response on 2 or more additional NSCH-ACEs items (Table 2). Despite this overlap, neither item-to-item correlations nor item-total correlations were so high as to suggest redundancy of information across the NSCH-ACEs items, which we would expect when stable and discrete item combination patterns are not anticipated. The highest correlations were observed between NSCH-ACEs items and either the “witnessed domestic violence” or “alcohol/drug abuse” ACEs topics. Least correlated with other NSCH-ACEs items were: 1) “difficult to get by on income,” which is distinct from poverty (fewer than 50% of children living in household with incomes at 0–99% of the FPL responded affirmatively to this item), 2) “treated unfairly due to race/ethnicity,” and 3) “parental death,” the latter two of which were also the items with the lowest prevalence, the lowest unidimensional factor loadings, and the lowest item-total correlations. Parental death was most correlated with “alcohol/drug use” and “treated unfairly due to race/ethnicity” was most correlated with “neighborhood violence.” The “difficult to get by on income” item was most prevalent as well as most likely to occur as the only ACE identified (48.5% with this ACE had no other ACEs). This item was most correlated with “parental divorce” at a low 0.152. See the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) for the full item-to-item correlation matrix.
Table 2.
NSCH-ACEs Item by Item Findings on Acceptability, Efficiency, Consistency, and “Single Score” Construct Validity
| Type of Adverse Childhood Experience | National Prevalence (US State) Range | Missing Values
|
Additional ACEs
|
Correlation With Other Items, Range | Item-Total Correlation | Unidimensional Confirmatory Factor Loading | |||
|---|---|---|---|---|---|---|---|---|---|
| Don’t Know | Refused | None | 1–2 Other | ≥3 Other | |||||
| Difficult to get by on current income | 25.7% 20.1% (Md)–34.3% (Ariz) |
0.2% | 0.5% | 48.5% | 34.5% | 17.0% | 0.054–0.152 | 0.232 | 0.39 |
| Divorce/parental separation | 20.1% 15.2% (DC)–29.5% (Okla) |
0.3% | 0.2% | 30.4% | 44.4% | 25.2% | 0.062–0.342 | 0.393 | 0.67 |
| Lived with someone with alcohol or drug problem | 10.7% 6.4% (NY)–18.5% (Mont) |
0.2% | 0.2% | 10.3% | 44.2% | 45.5% | 0.073–0.398 | 0.496 | 0.85 |
| Victim or witnessed neighborhood violence | 8.6% 5.2% (NJ)–16.6% (DC) |
0.5% | 0.1% | 15.1% | 41.5% | 43.4% | 0.079–0.360 | 0.380 | 0.70 |
| Lived with someone mentally ill or suicidal | 8.6% 5.4% (Calif)–14.1% (Mont) |
0.4% | 0.2% | 17.2% | 42.1% | 40.7% | 0.078–0.350 | 0.381 | 0.67 |
| Domestic violence witness | 7.3% 5.0% (NJ, Conn)–11.1% (Okla) |
0.6% | 0.3% | 6.4% | 36.4% | 57.2% | 0.085–0.398 | 0.482 | 0.84 |
| Parent served time in jail | 6.9% 3.2% (NJ)–13.2% (Ky) |
0.2% | 0.2% | 8.6% | 41.4% | 50.0% | 0.057–0.397 | 0.409 | 0.76 |
| Treated or judged unfairly due to race/ethnicity | 4.1% 1.8% (Vt)–6.5% (Ariz) |
0.5% | 0.1% | 29.7% | 44.2% | 26.1% | 0.032–0.144 | 0.131 | 0.33 |
| Death of parent | 3.1% 1.4% (Conn)–7.1% (DC) |
0.1% | 0.1% | 25.7% | 42.9% | 31.3% | 0.032–0.118 | 0.138 | 0.38 |
ACE indicates adverse childhood experience; NSCH, National Survey of Children’s Health.
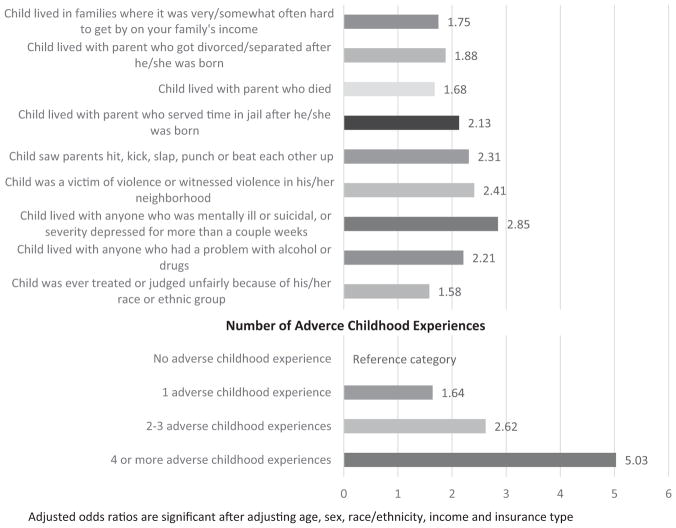
When the “difficult to get by on income,” “parental death,” or “treated unfairly due to race/ethnicity” topics were removed from the NSCH-ACEs, prevalence of ACEs among US children decreased from 48.7% to 35.6%, 47.1%, and 46.7%, respectively. When all 3 were removed, prevalence of ACEs was 32.9%. This lower rate is similarly predictive of whether a child has an EMB problem, defined using similar methods as reported in recent studies.28 We found that among children with 4 or more ACEs, 37% are identified as having EMB for the reduced NSCH-ACEs compared with 39% with EMB for the full NSCH-ACEs (adjusted odds ratios are 4.65 and 5.02 respectively). As shown in Figure 2, multivariate regression analyses reveal that although the 3 topics in question are less predictive, individual NSCH-ACEs items do not vary dramatically in their power to predict whether a child has an EMB problem and that cumulative NSCH-ACEs scores are more powerful predictors compared with any single item.
Figure 2.
Adjusted odds ratios for emotional, mental, or behavioral problems (age 2–17 years) by adverse childhood experiences. Data from the 2011/12 National Survey of Children’s Health.
Internal and External Validity of a Cumulative Risk Scoring Approach: Evaluating Cumulative Risk, Dimensional, and Categorical Approaches to Scoring
Confirmatory factor analysis
A single-factor model fit the data well (root mean square error of approximation = 0.01; comparative fit index = 0.99; Tucker-Lewis Index = 0.98; chi-square = 312.84; n = 94,520; P < .01). This is consistent with the hypothesis that, taken together, the NSCH-ACEs items measure a single construct. Table 2 shows the unidimensional factor loading for each NSCH-ACEs item and the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) shows the single factor model in a logistic item response theory metric. Although the covariance matrix of the NSCH-ACEs items is consistent with a single construct’s covariance matrix, some of the items do not relate as strongly to the overall adversity construct as others. The “difficult to get by on income” and “treated unfairly due to race/ethnicity” items have relatively low (although not necessarily problematically low)79 loadings. The remaining ACEs items are more strongly related to the overall construct of adversity assessed using the NSCH-ACEs.
LCA
Consistent with recommendations,86 we first fit a model with 2 latent classes and sought to increase the number of classes until the adjusted Bayesian information criterion began to increase in value. Models with ≥8 classes failed to converge (indicative of a poor model) despite the fact that the information-based criteria had yet to increase. In addition, these models were increasingly difficult to interpret. However, the Lo-Mendell-Rubin likelihood ratio test was no longer significant with ≥4 classes, which indicated the appropriateness of a 3-class solution. In addition, the 3-class solution was interpretable. Class 1 appears to correspond to a group of children who have not experienced ACEs. For all of the NSCH-ACEs items, the odds are nearly 100% that these children have not experienced that hardship. Latent class 2 appears to correspond to children who, relative to class 1, are more likely to have experienced difficulty getting by on income (odds of no income difficulty 0.21 vs 0.52 for class 1) and whose odds of having a divorced parent were nearly 50%. Additionally positive odds relative to class 1 were found for all other adversities, although these odds were less than for class 3. Thus, class 2 children were characterized by notably greater odds of some income difficulty and parental divorce (relative to class 1) and somewhat increased odds of experiencing any of the other ACEs, but with no distinct pattern with respect to the remaining items. Last, class 3 seems to correspond to children who have likely experienced several specific ACEs and are likely as not to have experienced several others. They are likely to have experienced: income difficulty (at least some income difficulty odds = 0.82), having a divorced parent (0.77), having seen physical abuse (0.72), and having lived with someone who has a drug or alcohol problem (0.83). They were likely as not to have had a parent who served time in jail, have been the victim of neighborhood violence, or lived with someone with mental illness. Table 3 shows the 3-class solution results in a probability metric.
Table 3.
Latent Class Analysis Results for the NSCH-ACEs
| ACE | Latent Class
|
||
|---|---|---|---|
| 1 | 2 | 3 | |
|
| |||
| Probability of Item Response | |||
| Difficult to get by on current income? | |||
| Never | 0.52 | 0.21 | 0.18 |
| Not very often | 0.30 | 0.37 | 0.27 |
| Somewhat often | 0.14 | 0.29 | 0.33 |
| Very often | 0.04 | 0.12 | 0.22 |
| Parental divorce? | |||
| No | 0.92 | 0.57 | 0.23 |
| Yes | 0.08 | 0.43 | 0.77 |
| Parental death? | |||
| No | 0.99 | 0.94 | 0.87 |
| Yes | 0.01 | 0.06 | 0.13 |
| Parent served time in jail? | |||
| No | 1.00 | 0.85 | 0.43 |
| Yes | 0.00 | 0.15 | 0.57 |
| See violence in the home? | |||
| No | 1.00 | 0.86 | 0.28 |
| Yes | 0.00 | 0.14 | 0.72 |
| Victim/witness of neighborhood violence? | |||
| No | 0.99 | 0.81 | 0.44 |
| Yes | 0.01 | 0.19 | 0.56 |
| Live with anyone mentally ill/suicidal? | |||
| No | 0.98 | 0.81 | 0.50 |
| Yes | 0.02 | 0.19 | 0.50 |
| Live with anyone with alcohol/drug problem? | |||
| No | 0.99 | 0.76 | 0.17 |
| Yes | 0.01 | 0.24 | 0.83 |
| Treated unfairly because of race/ethnicity? | |||
| No | 0.98 | 0.91 | 0.89 |
| Yes | 0.02 | 0.09 | 0.11 |
ACE indicates adverse childhood experience; NSCH, National Survey of Children’s Health.
Finally, Table 4 shows the findings from the SEM, showing the b coefficients and odds ratios for the latent adversity variable across outcomes and modeling approaches described previously. These models provide evidence of internal validity as well as external, predictive validity. All 3 approaches (reflective or formative) show a statistically significant and positive relationship between the latent adversity variable and outcome; as NSCH-ACEs scores increase the odds of the outcome also increase. Not surprisingly, because the Bollen83 approach constrains the residual variances to 0 (unrealistic but necessary for statistical identification), the size of the b coefficients that result from the Bollen83 approach are smaller than the coefficients from the other 2 approaches. Nevertheless, the substantive conclusions are similar across approaches and the “true” value is likely somewhere between the smallest and largest values.
Table 4.
NSCH-ACEs Structural Equation Model Assessing Validity With 5 Key Child Health and School Outcomes
| Predictor | Reflective
|
Formative
|
||||
|---|---|---|---|---|---|---|
| Bollen83
|
Treiblmaier et al84
|
|||||
| Odds Ratio* | b* | Odds Ratio* | b* | Odds Ratio* | b* | |
| CSHCN status | 1.63 (0.05)† | 0.51 (0.03)† | 1.23 (0.03)† | 0.20 (0.03)† | 1.54 (0.05)† | 0.45 (0.03)† |
| Emotional, behavioral, or developmental problem‡ | 1.89 (0.06)† | 0.64 (0.03)† | 1.27 (0.04)† | 0.24 (0.03)† | 1.73 (0.06)† | 0.55 (0.03)† |
| School engagement | 1.72 (0.06)† | 0.54 (0.03)† | 1.23 (0.04)† | 0.21 (0.029)† | 1.59 (0.06)† | 0.47 (0.04)† |
| Repeated a grade | 1.45 (0.07)† | 0.37 (0.05)† | 1.10 (0.05)† | 0.09 (0.04)† | 1.44 (0.07) | 0.36 (0.05)† |
| Resilience | 1.41 (0.04)† | 0.34 (0.03)† | 1.19 (0.03)† | 0.18 (0.03)† | 1.42 (0.05)† | 0.35 (0.03)† |
ACE indicates adverse childhood experience; CSHCN, children with special health care needs; and NSCH, National Survey of Children’s Health.
Adjusted for age, race/ethnicity, insurance status, and income.
Statistically significant at P < .05.
Children who qualify on the CSHCN Screener criteria for having emotional, developmental, or behavioral conditions that have lasted or are expected to last for ≥12 months and require treatment or counseling and/or who have had a doctor indicate current presence of ≥1 of 10 emotional, mental, or behavioral conditions asked in the NSCH.
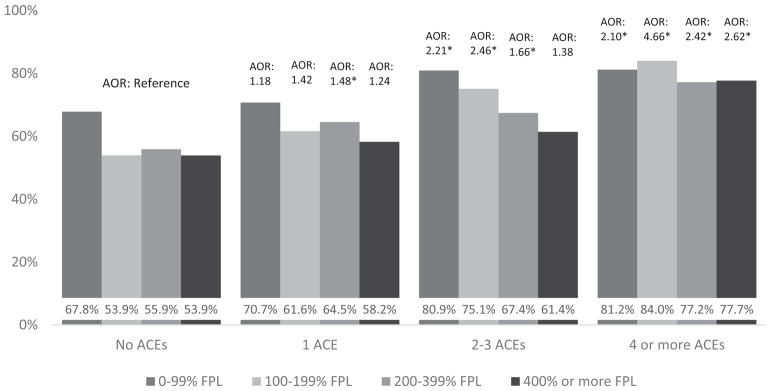
Findings Related to Recommendations for Population Based or High-Risk Assessment
As reported in a recent study, although prevalence using the NSCH-ACEs is higher for lower-income children, consistently high relative odds ratios for having health and related problems are observed among children with ACEs across income groups.28 Findings from this earlier study were replicated for each of the outcomes of focus in this analysis (CSHCN-More Complex, EMB, School Engagement, Resilience). Figure 3 shows findings for the “More complex CSHCN” outcome variable. Appendix E in the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) shows prevalence of each outcome across income groups and according to NSCH-ACEs status (no ACEs, 1, 2–3, or ≥4 ACEs). Nearly all adjusted odds ratios for comparisons of children with no ACEs with those with 1, 2 to 3, or ≥4 are significant for each outcome across each of the 4 income stratum (0–99% of the FPL, 100%–199% of the FPL, 200%–399% of the FPL, and ≥400% of the FPL) and are generally similar in magnitude across income groups. See the Technical Appendix (http://www.cahmi.org/wp-content/uploads/2015/01/ACEs-Measurement-paper-Technical-Appendix.pdf) for figures as well as tables showing the details of these findings.
Figure 3.
Prevalence of children with special health care needs with complex needs, by income and adverse childhood experiences (ACEs) status. AOR indicates adjusted odds ratio; FPL, federal poverty level. Data from the 2011/12 National Survey of Children’s Health.
Discussion
This study identified 14 distinct ACEs assessment tools for use in research, population surveillance, and clinical contexts. Although distinct, these tools were similar in the core content included, scoring methods used, and nearly uniformly recommended to assess ACEs in a relationship-centered context92 aimed at engaging and educating families and children in learning about their health and well-being and to promote prevention and healing from the effect of ACEs. Although most ACEs assessment methods appear to be easily replicated across a variety of settings, those that rely on administrative data are inherently unique to the setting in which the methods are used (eg, NSCAW, Marie-Mitchell and O’Conner Child ACE tool), are not readily replicable and their properties are less clear, especially with respect to whether they assess past exposures versus only currently occurring ACEs. We found evidence that parents are comfortable answering questions about their child’s ACEs in the context of a population-based survey. However, although guidelines for ACEs assessment in clinical settings are set forth for many methods reviewed and findings in our study suggest value and acceptability for assessing ACEs in practice, no studies were found that specifically document methods and outcomes for clinical (vs research) purposes for assessing ACEs among children, youth, or families.
We found strong internal validity for using a cumulative risk NSCH-ACEs score. In our study we did not identify any consistent patterns to provide evidence for creating categorical subgroups on the basis of types of adverse experiences. Compared with any single NSCH-ACEs topic, cumulative risk scores were more discriminating and predictive of outcomes assessed, such as having an emotional, behavioral, or mental health condition. Results across CFA and formative as well as reflective analyses provided evidence that a continuous score on the basis of parent’s NSCH-ACEs item responses appears to be a valid approach to creating an NSCH-ACEs score. This is consistent with human development science studies that link the stress and trauma associated with ACEs to the common factor of a lack of safety, security, and nurturance in a child’s primary relationships and environment; and evidence that each child’s unique adaptive or maladaptive reaction predict effects on child development and health, rather than the specific type of ACE.
For purposes of assessing adversity associated with risk for trauma and chronic stress, we recommend the continued use of a cumulative ACEs score and analysis along a dose-response continuum. Use of the NSCH-ACEs to separately evaluate types of ACEs, versus using a cumulative risk score, should be sure to take into account the high degree of overlap across types of ACEs and to clarify the theoretical and conceptual reasons for addressing specific experiences (such reasons might be well founded). In addition, at least with respect to the ACEs included on the NSCH, our LCA results suggest that, beyond separating children into those who have and have not experienced ACEs, there are not distinct patterns of ACEs experiences that readily separate children into substantively meaningful and easily identifiable types; with the possible exception of the “income difficulty” NSCH-ACEs topic.
We do not assess the temporal stability of the NSCH-ACEs, nor recommend classic test-retest analyses for this type of measure, which is distinct in ways that diminish the interpretability of any test-retest findings. For instance, if different responses were to be observed across administration intervals of the NSCH-ACEs, it could be explained by changes in awareness brought about by the self-reflection that can occur when first asked about ACEs, or subsequent learning. Changes in ACEs scores for children are also expected because they might encounter additional adversities. Finally, ACEs assessment is not intended to objectively document the occurrence of events, but to assess recollection of experiences of such events. This view calls upon neuroscience and related findings that perceived experiences drive many of the effects of concern.
Despite evidence supporting a cumulative scoring method for the NSCH-ACEs, we recognize that such a measure might not have the greatest possible predictive power for specific versus the more general types of outcomes evaluated in this study. It is important to note that there is evidence that specific types of adversities might be associated with specific types of mental health symptoms90 (eg, hallucinations, paranoia). However, ACEs assessment has not been recommended to be diagnostic, nor to differentiate among specific symptoms, but to open dialogue and flag needs for further evaluation.
Some NSCH-ACEs items are inherently more exact than others (eg, parental divorce, incarceration, or death vs parental mental illness, substance abuse), which might lead to more variability and weaker inferences for these less exact types of ACEs. Although we do not recommend deleting the “difficult to get by on income” or “ethnic or racial discrimination” NSCH-ACEs items, we do note their weaker association with the overall NSCH-ACEs score. These are also items unique to the NSCH-ACEs compared with many other ACEs measurement methods assessed in this study. Further evaluation of these constructs and how they are asked about might be advisable. The 2016 NSCH will allow consideration of other ACEs, like being bullied and assessments against school readiness, family resilience, and other new topics assessed in the 2016 NSCH.
For children and youth, ACEs assessments might occur in the context of well child care visits or other health care encounters, like hospitalizations. For children, such encounters might also involve an assessment of current (vs historic/past) exposures. This raises important questions as to the process for doing so in ways that ensure trust is maintained with parents and families. As recommended in guidelines associated with several ACEs tools, assessment of ACEs might be most effective when addressed in the larger context of history-taking and health promotion conversations to proactively promote positive health and resilience for children and families. Such contexts might also involve concurrent assessment of: 1) biologic indicators of stress or trauma, 2) resilience, 3) protective factors, like family connection, 4) mental and physical functioning and symptoms, and 5) positive functioning and well-being. This additional information provides the contextual information needed to understand needs and recommend supports. In a research context, this information is essential to learning about the wide variations in outcomes for those exposed to ACEs (so-called positive and negative deviance). Despite consistent findings of systematically higher risk of poor outcomes with ACEs, many children do not experience such outcomes. This points to the need for research to advance thriving even with adversity.
Conclusion
Feasible and valid measurement methods are required to guide and evaluate primary care, public health, acute care, and other community-based models that endeavor to prevent and address the consequences of ACEs and promote healthy development and well-being among children, youth, and families. Future research is required to specify approaches, requirements, and the value of engaging families, children, and youth in assessing, addressing, and preventing ACEs in clinical and related settings, because previous research has focused more on adult populations and population-based assessment and research versus practice. Although studies on protective factors that buffer the effect of ACEs exist, further research is needed to understand the variable effect of ACEs across children and move toward evidence to guide recommended prevention and treatment approaches in primary care as well as in the wide range of community-based contexts in which ACEs assessment, education, and interventions might take place. Because a great deal of variability exists within risk groups, further assessment of positive and negative deviance in outcomes and effects for otherwise similar groups of children might prove especially valuable, and would ideally occur in the context of longitudinal studies. Existing longitudinal studies should consider including ACEs and related variables for this purpose.
Whether ACEs are unique compared with other types of stressors, such as exposure to war and other types of violence in the environment (vs the home), bullying at school, and other adversities is unclear. Health services research is also needed to examine the possible value and effect of specifying new diagnostic codes like “developmental trauma disorder (DTD)” and how specification of DTD might affect diagnoses and treatment for other conditions linked to ACEs exposure (eg, asthma, attention-deficit/hyperactivity disorder, depression, etc) many of which share some of the same symptoms as DTD. Effects of assessing and addressing ACEs on health care costs should also be assessed.
Within any given context or purpose for measurement, identifying a standardized method to assess ACEs is important to accurately evaluate the effect of ACEs on children’s outcomes as well as to understand how ACEs assessment might inform or improve larger efforts to promote child well-being. In this regard, conceptual clarity as to purpose for measurement, definition of ACEs, and measurement specification is fundamental. Also essential is establishing the feasibility, validity, and specific implementation approach for ACEs assessment methods, including evaluating the validity and value of methods to score and interpret information resulting from the use of a measure of ACEs with children or adults/parents. In this article we have endeavored to address many of these questions to inform public health and practice-based applications and advance ACEs assessment in the context of larger goals to promote early and lifelong health and well-being for children, youth, and families.
Acknowledgments
Financial disclosure: This study was supported by the Child and Adolescent Health Measurement Initiative Leadership Fund with additional support from the Health Resources and Services Administration through its Maternal and Child Health Measurement Research Network grant (UA6MC30375) to the Child and Adolescent Health Measurement Initiative at the Johns Hopkins Bloomberg School of Public Health.
Publication of this article was supported by the Promoting Early and Lifelong Health: From the Challenge of Adverse Childhood Experiences (ACEs) to the Promise of Resilience and Achieving Child Wellbeing project, a partnership between the Child and Adolescent Health Measurement Initiative (CAHMI) and Academy-Health, with support from the Robert Wood Johnson Foundation (#72512).
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities. JAMA. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 2.Sameroff AJ, Seifer R, Baldwin A, et al. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Dev. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- 3.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center on the Developing Child. Harvard University. [Accessed February 17, 2016];Supportive Relationships and Active Skill-Building Strengthen the Foundations of Resilience: Working Paper 13. 2015 Available at: http://developingchild.harvard.edu/resources/supportive-relationships-and-active-skill-building-strengthen-the-foundations-of-resilience/
- 5.Shonkoff JP, Garner AS Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 6.Jones DE, Greenberg M, Crowley M. Early social-emotional functioning and public health: the relationship between kindergarten social competence and future wellness. Am J Public Health. 2015;105:2283–2290. doi: 10.2105/AJPH.2015.302630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park S, Kim BN, Kim JW, et al. Interactions between early trauma and catechol-O-methyltransferase genes on inhibitory deficits in children with ADHD. J Atten Disord. 2017;21:183–189. doi: 10.1177/1087054714543650. [DOI] [PubMed] [Google Scholar]
- 8.Romens SE, Mcdonald J, Svaren J, et al. Associations between early life stress and gene methylation in children. Child Dev. 2014;86:303–309. doi: 10.1111/cdev.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zannas A, West A. Epigenetics and the regulation of stress vulnerability and resilience. Neuroscience. 2014;264:157–170. doi: 10.1016/j.neuroscience.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anda RF, Dong M, Brown DW, et al. The relationship of adverse childhood experiences to a history of premature death of family members. BMC Public Health. 2009;9:106. doi: 10.1186/1471-2458-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schor EL. Whole child care. J Dev Behav Pediatr. 2015;36:467–468. doi: 10.1097/DBP.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 12.Wissow LS, Brown J, Fothergill KE, et al. Universal mental health screening in pediatric primary care: a systematic review. J Am Acad Child Adolesc Psychiatry. 2013;52:1134–1147. doi: 10.1016/j.jaac.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vu C, Rothman E, Kistin CJ. Adapting the patient centered medical home to address psychosocial adversity: Results of a qualitative study. Acad Pediatr. 2017;17:S115–S122. doi: 10.1016/j.acap.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Marie-Mitchell A, O’Connor TG. Adverse childhood experiences: translating knowledge into identification of children at risk for poor outcomes. Acad Pediatr. 2013;13:14–19. doi: 10.1016/j.acap.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Marie-Mitchell A, Studer KR, O’Connor TB. How knowledge of adverse childhood experiences can help pediatricians prevent mental health problems. Fam Syst Health. 2016;34:128–135. doi: 10.1037/fsh0000179. [DOI] [PubMed] [Google Scholar]
- 16.Butchart A. Addressing adverse childhood experiences to improve public health: Expert consultation, 4–5 May 2009: Meeting report. WHO; [Accessed February 17, 2016]. Available at: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/global_research_network_may_2009.pdf?ua=1. [Google Scholar]
- 17.Academy on Violence & Abuse. Corwin D, Alexander R, Bair-Merrit M, et al. Adverse childhood experiences: informing best practices. [Accessed September 14, 2015];Online collaborative living document – version 1.0. Available at: http://www.avahealth.org/aces_best_practices/aces-best-practices.html.
- 18.Cronholm PF, Forke CM, Wade R, et al. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. 2015;49:354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Bethell CD, Newacheck P, Hawes E, et al. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff (Millwood) 2014;33:2106–2115. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- 20.Dube SR, Felitti VJ, Dong M, et al. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37:268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- 21.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Adverse childhood experiences reported by adults – five states. MMWR Morb Mortal Wkly Rep. 2010;59:1609–1613. [PubMed] [Google Scholar]
- 23.Data Resource Center for Child and Adolescent Health. [Accessed June 1, 2015];Overview of adverse child and family experiences among US children. Available at: http://www.childhealthdata.org/docs/drc/aces-data-brief_version-1-0.pdf.
- 24.World Health Organization. Adverse childhood experiences international questionnaire: pilot study review and finalization meeting, 4–5 May 2011, WHO headquarters, Geneva: Meeting report; [Accessed February 17, 2016]. Available at: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/global_research_network_may_2011.pdf?ua=1. [Google Scholar]
- 25.Bloom S. Advancing a national cradle-to-grave to-cradle public health agenda. J Trauma Dissociation. 2016;17:383–396. doi: 10.1080/15299732.2016.1164025. [DOI] [PubMed] [Google Scholar]
- 26.Garg A, Dworkin PH. Surveillance and screening for social determinants of health: the medical home and beyond. JAMA Pediatr. 2016;170:189–190. doi: 10.1001/jamapediatrics.2015.3269. [DOI] [PubMed] [Google Scholar]
- 27.Brown JD, King MA, Wissow LS. The central role of relationships to trauma-informed integrated care for children and youth. Acad Pediatr. 2017;17:S94–S101. doi: 10.1016/j.acap.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 28.Bethell C, Gombojav N, Solloway M, et al. Adverse childhood experiences, resilience and mindfulness-based approaches. Child Adolesc Psychiatr Clin N Am. 2016;25:139–156. doi: 10.1016/j.chc.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Embry DD, Biglan A. Evidence-based kernels: fundamental units of behavioral influence. Clin Child Fam Psychol Rev. 2008;11:75–113. doi: 10.1007/s10567-008-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Day A. The power of social support: mentoring and resilience. Reclaiming Children and Youth. 2006;14:196–198. [Google Scholar]
- 31.Durlak JA, Weissberg RP, Dymnicki AB, et al. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev. 2011;82:405–432. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- 32.Garner AS, Forkey H, Szilagyi M. Translating developmental science to address childhood adversity. Acad Pediatr. 2015;15:493–502. doi: 10.1016/j.acap.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 33.Klika JB, Herrenkohl TI. A review of developmental research on resilience in maltreated children. Trauma Violence Abuse. 2013;14:222–234. doi: 10.1177/1524838013487808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Masten AS. Ordinary Magic: Resilience in Development. New York, NY: Guilford Press; 2014. [Google Scholar]
- 35.Ungar M, Ghazinour M, Richter J. Annual research review: what is resilience within the social ecology of human development? J Child Psychol Psychiatry. 2012;54:348–366. doi: 10.1111/jcpp.12025. [DOI] [PubMed] [Google Scholar]
- 36.Usable Knowledge. Walsh B. The science of resilience. [Accessed June 1, 2015];Why some children can thrive despite adversity. Available at: http://www.gse.harvard.edu/news/uk/15/03/science-resilience.
- 37.Hagan JF, Shaw JS, Duncan PM, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4. Elk Grove Village, Ill: American Academy of Pediatrics; 2017. [Google Scholar]
- 38.Ford DC, Merrick MT, Parks SE, et al. Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychol Violence. 2014;4:432–444. doi: 10.1037/a0037723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finkelhor D, Shattuck A, Turner H, et al. Improving the adverse childhood experiences scale. JAMA Pediatr. 2013;167:70–75. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- 40.Edwards JR. The fallacy of formative measurement. Organ Res Methods. 2010;14:370–388. [Google Scholar]
- 41.Gallop R, Mckeever P, Toner B, et al. Inquiring about childhood sexual abuse as part of the nursing history: opinions of abused and non-abused nurses. Arch Psychiatr Nurs. 1995;9:146–151. doi: 10.1016/s0883-9417(95)80037-9. [DOI] [PubMed] [Google Scholar]
- 42.Murphy A, Steele H, Bate J, et al. Group attachment-based intervention. Fam Community Health. 2015;38:268–279. doi: 10.1097/FCH.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 43.Doob D. Female sexual abuse survivors as patients: avoiding retraumatization. Arch Psychiatr Nurs. 1992;6:245–251. doi: 10.1016/0883-9417(92)90068-t. [DOI] [PubMed] [Google Scholar]
- 44.Tucker WM. How to include the trauma history in the diagnosis and treatment of psychiatric inpatients. Psychiatr Q. 2002;72:135–144. doi: 10.1023/a:1015007828262. [DOI] [PubMed] [Google Scholar]
- 45.Pennebaker JW, Susman JR. Disclosure of traumas and psychosomatic processes. Soc Sci Med. 1988;26:327–332. doi: 10.1016/0277-9536(88)90397-8. [DOI] [PubMed] [Google Scholar]
- 46.Stewart SH. Alcohol abuse in individuals exposed to trauma: a critical review. Psychol Bull. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- 47.Becker-Blease KA, Freyd JJ. Research participants telling the truth about their lives: the ethics of asking and not asking about abuse. Am Psychol. 2006;61:218–226. doi: 10.1037/0003-066X.61.3.218. [DOI] [PubMed] [Google Scholar]
- 48.OPIP. Oregon Pediatric Improvement Partnership. Gillespie RJ. [Accessed October 14, 2015];ACE screening in practice: the medical home response. Available at: http://www.oregon-pip.org/resources/November%20webinar%20ACE%20in%20practice_2013.pdf.
- 49.Blodgett C. [Accessed February 17, 2016];Working paper 7/30/12: Adapting ACEs screening and assessment in child serving systems. Available at: http://ext100.wsu.edu/cafru/wp-content/uploads/sites/65/2015/03/Complex-Trauma-Research-ACE-Screening-and-Assessment-in-Child-Serving-Systems-7-12-final.pdf.
- 50.Borgers N, Leeuw ED, Hox J. Children as respondents in survey research: cognitive development and response quality 1. Bull Methodol Sociol. 2000;66:60–75. [Google Scholar]
- 51.DeAngelis T. A new diagnosis for childhood trauma? Some push for a new DSM category for children who undergo multiple, complex traumas. Monitor on Psychology: A Publication of the American Psychological Association. 2007;38:32. [Google Scholar]
- 52.Ford JD, Grasso D, Greene C, et al. Clinical significance of a proposed developmental trauma disorder diagnosis. J Clin Psychiatry. 2013;74:841–849. doi: 10.4088/JCP.12m08030. [DOI] [PubMed] [Google Scholar]
- 53.Rahim M. Developmental trauma disorder: an attachment-based perspective. Clin Child Psychol Psychiatry. 2014;19:548–560. doi: 10.1177/1359104514534947. [DOI] [PubMed] [Google Scholar]
- 54.Schmid M, Petermann F, Fegert JM. Developmental trauma disorder: pros and cons of including formal criteria in the psychiatric diagnostic systems. BMC Psychiatry. 2013;13:3. doi: 10.1186/1471-244X-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McDonald RP. Test Theory: A Unified Treatment. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- 56.Child Trends. Sacks V, Murphy D, Moore K. [Accessed February 3, 2016];Adverse childhood experience: national and state-level prevalence. Available at: https://www.childtrends.org/publications/adverse-childhood-experiences-national-and-state-level-prevalence/
- 57.Wildeman C, Emanuel N, Leventhal JM, et al. The prevalence of confirmed maltreatment among US children, 2004 to 2011. JAMA Pediatr. 2014;168:706. doi: 10.1001/jamapediatrics.2014.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vanaelst B, Vriendt TD, Huybrechts I, et al. Epidemiological approaches to measure childhood stress. Paediatr Perinat Epidemiol. 2012;26:280–297. doi: 10.1111/j.1365-3016.2012.01258.x. [DOI] [PubMed] [Google Scholar]
- 59.NCTSN. National Child Traumatic Stress Network. [Accessed August 10, 2015];Measures review database. Available at: http://www.nctsn.org/resources/online-research/measures-review.
- 60.Data Resource Center for Child & Adolescent Health. [Accessed February 17, 2016];Guide to topics & questions. Available at: http://www.childhealthdata.org/learn/nhis-child/topics_questions/3.3.9-2011-2012-nhis-family-guide-to-topics-and-questions.
- 61.Casanueva C, Smith K, Dolan M, et al. OPRE Report #2011–27c. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2011. NSCAW II Baseline Report: Maltreatment. [Google Scholar]
- 62.Stambaugh LF, Ringeisen H, Casanueva CC, et al. Adverse Childhood Experiences in NSCAW. OPRE Report 2013–26. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 63.Hudziak JJ, Kaufman J. Yale-Vermont Adversity in Childhood Scale (Y-VACS): Adult, Child, Parent, & Clinician Questionnaires. 2014. Available by request from james.hudziak@med.uvm.edu. [Google Scholar]
- 64.Bucci M, Gutierrez Wang L, Koita K, et al. Center for Youth Wellness ACE-Questionnaire User Guide. San Francisco, Calif: Center for Youth Wellness; 2015. [Google Scholar]
- 65.Murphy A, Steele M, Dube SR, et al. Adverse Childhood Experiences (ACEs) Questionnaire and Adult Attachment Interview (AAI): implications for parent child relationships. Child Abuse Neglect. 2014;38:224–233. doi: 10.1016/j.chiabu.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 66.Murphy, Dube, Steele, Steele . Clinical adverse childhood experiences questionnaire: Child and adult versions. 2007. Available by request at brooke.allman@einstein.yu.edu. [Google Scholar]
- 67.The Health Federation of Philadelphia. [Accessed February 17, 2016];The Philadelphia Urban ACE Study. Available at: http://www.instituteforsafefamilies.org/philadelphia-urban-ace-study.
- 68.Washington State University. CAHNRS. Child and Family Research Unit. Blodgett C. Research; [Accessed February 17, 2016]. Available at: http://ext100.wsu.edu/cafru/research. [Google Scholar]
- 69.The National Crittenton Foundation. [Accessed November 17, 2015];ACEs Toolkit for Providers. Available at: http://www.nationalcrittenton.org/aces-toolkit-for-providers.
- 70.The National Crittenton Foundation. [Accessed February 17, 2016];Beyond ACEs Webinar. Available at: http://nationalcrittenton.org/beyond-aces-webinar/
- 71.The National Crittenton Foundation. The National Crittenton Foundation 2014 ACE Questionaire. 2014. Available by request at samantha@nationalcrittenton.org. [Google Scholar]
- 72.U.S. Centers for Disease Control and Prevention. About the CDC-Kaiser ACE study. Study Questionnaires. [Accessed July 24, 2017];Family Health History Questionnaire, Male and Female versions. Available at: https://www.cdc.gov/violenceprevention/acestudy/about.html.
- 73.U.S. Centers for Disease Control and Prevention. About the CDC-Kaiser ACE study. Study Questionnaires. [Accessed July 24, 2017];Health Appraisal Questionnaire, Male and Female versions. Available at: https://www.cdc.gov/violenceprevention/acestudy/about.html.
- 74.Centers for Disease Control and Prevention. [Accessed February 17, 2016];Behavioral risk factor surveillance system. Available at: http://www.cdc.gov/brfss/questionnaires/index.htm.
- 75.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. [Accessed February 17, 2016];Survey data & documentation. Available at: http://www.cdc.gov/brfss/data_documentation/index.htm.
- 76.CDC. Centers for Disease Control and Prevention. Behavioral risk factor surveillance system. [Accessed February 17, 2016];State-by-state listing of how data are used. Available at: http://www.cdc.gov/brfss/state_info/brfss_use_examples.htm.
- 77.World Health Organization. Violence and Injury Prevention. Data management. [Accessed February 17, 2016];Guidance for analysing ACE-IQ. Available at: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/data/en.
- 78.World Health Organization. [Accessed February 17, 2016];Adverse Childhood Experiences International Questionnaire (ACE-IQ) Available at: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/en/. Published 2011.
- 79.Palmer RF, Graham JW, Taylor B, et al. Construct validity in health behavior research: interpreting latent variable models involving self-report and objective measures. J Behav Med. 2002;25:525–550. doi: 10.1023/a:1020689316518. [DOI] [PubMed] [Google Scholar]
- 80.Howell RD, Breivik E, Wilcox JB. Reconsidering formative measurement. Psychol Methods. 2007;12:205–218. doi: 10.1037/1082-989X.12.2.205. [DOI] [PubMed] [Google Scholar]
- 81.Diamantopoulos A, Riefler P, Roth KP. Advancing formative measurement models. J Bus Res. 2008;61:1203–1218. [Google Scholar]
- 82.Bollen KA, Lennox RD, Dahly DL. Practical application of the vanishing tetrad test for causal indicator measurement models: an example from health-related quality of life. Stat Med. 2009;28:1524–1536. doi: 10.1002/sim.3560. [DOI] [PubMed] [Google Scholar]
- 83.Bollen KA. Structural Equations With Latent Variables. New York, NY: Wiley; 1989. [Google Scholar]
- 84.Treiblmaier H, Bentler PM, Mair P. Formative constructs implemented via common factors. Struct Eq Modeling. 2011;18:1–17. [Google Scholar]
- 85.Hagenaars JA, McCutcheon AL. Applied Latent Class Analysis. Cambridge: Cambridge University Press; 2002. [Google Scholar]
- 86.McCutcheon AL. Latent Class Analysis. Lincoln, Neb: Sage; 1987. [Google Scholar]
- 87.CDC. Centers for Disease Control and Prevention. [Accessed February 17, 2016];Prevalence of individual adverse childhood experiences. Available at: https://www.cdc.gov/violenceprevention/acestudy/about.html.
- 88.CDC. Centers for Disease Control and Prevention. [Accessed February 17, 2016];The BRFSS data user guide. Available at: https://www.cdc.gov/brfss/data_documentation/pdf/userguidejune2013.pdf.
- 89.Centers for Disease Control and Prevention. [Accessed February 17, 2016];BRFSS Questionnaires. Available at: http://www.cdc.gov/brfss/questionnaires/index.htm.
- 90.Bentall RP, Wickham S, Shevlin M, et al. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 The Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38:734–740. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dolan M, Smith K, Casanueva C, et al. NSCAW II Baseline Report: Introduction to NSCAW II. OPRE Report 2011–27a. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 92.Kirkegaard M, Ring J. The Case for Relationship-Centered Care and How to Achieve It. Health Management Associates; 2017. [Accessed July 24, 2017]. Available at: https://www.healthmanagement.com/wp-content/uploads/The-Case-for-RCC-final-2-9-2017.pdf. [Google Scholar]