Elective ICU admissions represent an important part of all ICU admissions worldwide (1,2). Considering the significant mortality and morbidity associated with major surgery and its complications, it is conceivable that admission to an environment with intensive monitoring and with a staff capable of immediate recognition and treatment of abnormalities could reduce mortality (1). This concept, albeit based on a solid rationale, has been recently challenged in large cohort studies (3).
Morbidity and mortality after elective surgery: what is the size of the problem?
It has been suggested that mortality after high-risk surgery may be close to 0.5% (1). This comes from a large 7-day cohort study that included 44,814 patients in 27 countries (1). Due to the high number of high-risk surgeries performed annually, the apparently low mortality is still associated with a huge mortality burden for the society. Complications occurred in up to 16.8% of all patients, representing a large source of morbidity and costs (1). About 10% of all patients were admitted to the ICU after surgery. Unsurprisingly, these patients had more complications (50%) and had higher mortality (2.5%), that could be related to a selection bias (that is, sicker patients or those submitted to higher risk procedures were more frequently admitted to the ICU). One important point is that this reported mortality is much lower than previous reports (2). In the EuSOS study, published in 2012, mortality after elective surgery peaked 3%, with important variations between European countries.
What can explain the differences in mortality between EuSOS and ISOS studies? EuSOS included only European hospitals, while ISOS included hospitals from middle income countries and one hospital from a low income country. Additionally, EuSOS excluded cardiac surgery. EuSOS patients also had slightly higher ASA scores. EuSOS may also have had representative issues, since some countries included few patients for analysis, which could induce selection bias. Nevertheless, both studies provide relevant data on the prevalence of complications and mortality after surgery.
Causes of morbidity and mortality after surgery
On the ISOS database, complications occured in 26% of all patients (11,690), of which 2.8% died. Much emphasis has been given to cardiovascular complications after major surgery. In fact, using data from the ISOS database (1), cardiovascular complications occured in 4.5% of all patients in the ISOS study, with a 7.9% mortality. It should be highlighted that most of the “cardiovascular deaths” reported were due to cardiac arrest that were attributed to be of cardiovascular origin (91 of all 144 cardiovascular deaths: 64%). Mortality for feared cardiovascular complications such as pulmonary embolism was rather slow (only five patients in the whole cohort of 44,814 patients developed fatal pulmonary embolism). Myocardial infarction occured in 0.3% of all patients; from those who developed myocardial infarction, 18.7% died in hospital.
Infectious complications occurred in 8.9% (4,032 patients), but only 2.6% of those who developed infection perished due to its occurrence (1). Other complications associated with high mortality included acute kidney injury and acute respiratory distress syndrome (1).
Therefore, a myriad of possible complications may be related to hospital mortality and morbidity after surgery. When faced with this complex array of conditions, it becomes clear that reducing mortality will be an extremely difficult task. For example, let´s imagine an intervention that is anticipated to reduce cardiovascular complications in the postoperative period by 10% that would be applied to a population similar to that of ISOS. Considering ISOS data, over 84 thousand patients would be required to obtain 90% power with 0.05 alpha, which is unpractical.
Does elective ICU admission help?
The rationale of ICU admission after elective surgery supposes that ICU admission can be preventive, which is not necessarily true. However, many complications discussed above have their roots on the pre-operative and operative period and, therefore cannot be prevented by ICU admission. For example, postoperative acute respiratory distress syndrome and occurrence of other respiratory complications is directly related to use of high tidal volumes during operative period (3).
In a landmark secondary analysis of the ISOS database, Kahan and workers evaluated whether routine ICU admission after surgery would be associated with improved outcomes (4). At the patient level, the authors found that after correcting for important confounders (such age, gender, current smoker, American Society of Anesthesiologists physical status (ASA) score, severity of surgery and presence of co-morbid diseases) hospital mortality remained higher for those admitted to the ICU (3.01; 95% confidence intervals, 2.10–5.21; P<0.001). Three other analyses were performed by the authors, one hospital-level analysis for planned ICU admission after surgery, one hospital-level analysis for ICU admission to treat a postoperative complications and, finally, a hospital-level analysis for the association between mortality and critical care capacity. In neither hospital-level analysis ICU admission was shown to change mortality. In a subgroup analysis of the most severely ill patients (ASA III or IV and undergoing major surgery), results were unaltered. The authors concluded that elective ICU admission was not associated with improved outcomes.
Should we be surprised by these results? Not at all. In the EuSOS study, for example, 73% of all patients that died were not admitted to critical care during their hospital stay (1). The authors hypothesized that the higher mortality found in the individual patient analysis could be explained by residual confounding that could not be accounted for in their robust mixed model logistic regression. Indeed, the decision to admit a patient electively after major surgery is subjective most of the time. Therefore, the higher mortality observed could just suggest that physicians did a good job when doing triage of patients for ICU admission. However, would it be possible that ICU admission could indeed harm a patient in this scenario?
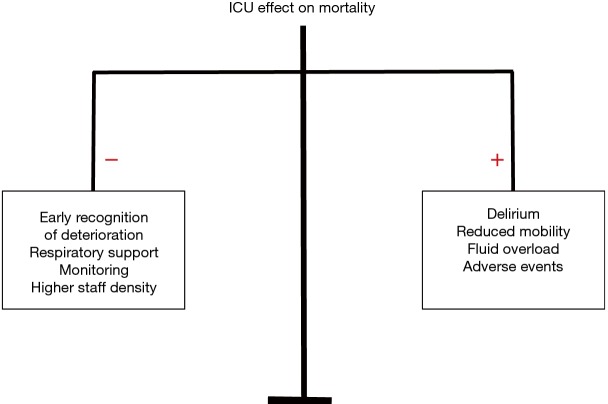
The answer is yes. The postoperative period is characterized by many physiological changes that may or may not require intervention. For example, reduction in urinary output may occur to mechanisms that are not related to insufficient fluid use, such as anti-diuretic hormone secretion or simply an increase in adrenergic tone (5). Additionally, even if acute kidney injury occurs, aggressive fluid resuscitation may be more harmful than beneficial for the patient (6). Minor changes in blood pressure, which may also be transient and of unknown clinical relevance may be further treated with fluid bolus and vasopressors, thereby increasing costs and ICU length-of-stay. By placing older frail patients in a confined environment, delirium may occur which may in turn increase mortality (7). Finally, adverse events are frequent in the ICU (8). Therefore, ICU eventual benefits of ICU admission may be overcome by overtreatment of possibly benign conditions and by the harms of ICU admission by itself (Figure 1).
Figure 1.
ICU effects on mortality may be mediated by its protective effects (left) and harms (right). The net benefit depends on which side prevails.
The findings by Kahan have limits that are inherent to observational studies. Far from being an evidence against ICU admission after major surgery, it makes us rethink whether sometimes too much treatment can be harmful of futile.
Acknowledgements
None.
Provenance: This is an invited Editorial commissioned by the Section Editor Dr. Xue-Zhong Xing [National Cancer Center (NCC)/Cancer Hospital, Chinese Academy of Medical Sciences (CAMS) and Peking Union Medical College (PUMC), Beijing, China].
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- 1.The International Surgical Outcomes Study group Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth 2016;117:601-9. 10.1093/bja/aew316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearse RM, Moreno RP, Bauer P, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet 2012;380:1059-65. 10.1016/S0140-6736(12)61148-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428-37. 10.1056/NEJMoa1301082 [DOI] [PubMed] [Google Scholar]
- 4.Kahan BC, Koulenti D, Arvaniti K, et al. Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med 2017;43:971-9. 10.1007/s00134-016-4633-8 [DOI] [PubMed] [Google Scholar]
- 5.Sear JW. Kidney dysfunction in the postoperative period. Br J Anaesth 2005;95:20-32. 10.1093/bja/aei018 [DOI] [PubMed] [Google Scholar]
- 6.Prowle JR, Kirwan CJ, Bellomo R. Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol 2014;10:37-47. 10.1038/nrneph.2013.232 [DOI] [PubMed] [Google Scholar]
- 7.Tosun Tasar P, Sahın S, Akcam NO, et al. Delirium is associated with increased mortality in the geriatric population. Int J Psychiatry Clin Pract 2017. [Epub ahead of print]. 10.1080/13651501.2017.1406955 [DOI] [PubMed] [Google Scholar]
- 8.Corwin GS, Mills PD, Shanawani H, et al. Root Cause Analysis of ICU Adverse Events in the Veterans Health Administration. Jt Comm J Qual Patient Saf 2017;43:580-90. 10.1016/j.jcjq.2017.04.009 [DOI] [PubMed] [Google Scholar]