Abstract
Background
Long-term individual prognosis and risk factors for quality of life and disability following anterior cruciate ligament (ACL) reconstruction remain unknown.
Hypothesis/Purpose
Our objective was to identify patient-reported outcomes and patient-specific risk factors from a large prospective cohort at a minimum 10-year follow-up after ACL reconstruction. We hypothesized that meniscus and articular cartilage injuries, revision ACL reconstruction, subsequent knee surgery, and certain demographic characteristics would be significant risk factors for inferior outcomes at 10 years.
Study Design
Prospective longitudinal cohort study
Methods
Unilateral ACL reconstructions were identified and prospectively enrolled between 2002 and 2004 from 7 sites in the Multicenter Orthopaedics Outcome Network (MOON). Patients pre-operatively completed a series of validated outcome instruments, including the IKDC, KOOS, and Marx activity rating scale. At the time of surgery, physicians documented all intraarticular pathology, treatment, and surgical techniques utilized. Patients were followed at 2, 6, and 10 years post-op, and asked to complete the same outcome instruments that they completed at baseline. Incidence and details of any subsequent knee surgeries were also obtained. Multivariable regression analysis was used to identify significant predictors of outcome.
Results
A total of 1592 patients were enrolled (57% male; median age 24 years). Ten-year follow-up was obtained on 83% (1320) of the cohort. Both IKDC and KOOS scores significantly improved at 2 years and were maintained at 6 and 10 years. Conversely, Marx activity level scores dropped markedly over time, from a median score of 12 points at baseline, 9 points at 2 years, 7 points at 6 years, to 6 points at 10 years.
The patient-specific risk factors for inferior 10-year outcomes were lower baseline outcome scores, higher BMI, smoker at baseline, having a medial or lateral meniscus procedure done prior to the index ACL reconstruction, having a revision ACL reconstruction, lateral meniscectomy, grades 3–4 articular cartilage pathology in the medial, lateral or patellofemoral compartments, and having any subsequent ipsilateral knee surgery following the index ACL reconstruction.
Conclusions
Patients are able to perform sports-related functions and maintain a relatively high knee-related quality of life 10 years after ACL reconstruction, although activity level significantly declines over time. Multivariable analysis identified several key modifiable risk factors that significantly influence outcome.
Key Terms: anterior cruciate ligament, ACL reconstruction, follow-up, outcomes, IKDC, KOOS, Marx, revision ACL reconstruction, meniscus, articular cartilage, subsequent surgery
INTRODUCTION
Numerous studies have reported on the short- and intermediate-term successful results of anterior cruciate ligament (ACL) reconstruction.3, 10, 32, 54, 56 However, while researchers have documented the long-term risks of osteoarthritis following ACL reconstruction1, 2, 4, 6, 11, 13, 19, 20, 25, 27–29, 31, 33, 40–42, 45, 52, 55, 57 and incidence of subsequent surgeries and ACL graft tears,7, 10 there has been less discussion of patient-specific risk factors and patient-reported outcome measures following ACL reconstruction.36 Patient-reported outcome measures offer a complementary set of diagnostic tools with which to quantify “outcome”. A subset of these patient-reported outcome measures have been validated, defined as undergone testing for the instrument’s reliability, responsiveness, and validity (i.e. content validity, face validity, construct validity and/or criterion validity). During the last decade, validated patient-reported outcome measures have become more popular, as these measures have provided invaluable information to researchers about the relative success of orthopaedic interventions.5, 30, 46, 49 These instruments document information about knee function, symptoms, and quality of life from the patient’s point of view, and have been reported to be strong proxies for onsite assessments.58 Because patient-reported outcomes have come to play an increasingly large role in the assessment of outcomes after treatment, they have become a recommended component of all clinical trials.9 Additionally, a unique advantage of questionnaire-based validated patient-reported outcomes is the ability to follow hundreds or thousands of patients at a fraction of the cost, and with improved follow-up compared to the logistic difficulties of having patients return for onsite evaluations (e.g., clinical exam, radiographs, etc).
Ten-year patient-reported outcomes (e.g., the International Knee Documentation Committee [IKDC]50 form, the Knee injury and Osteoarthritis Outcome Score [KOOS],49 and the Marx activity rating scale38) as well as the modifiable risk factors for an individual patient’s worse outcomes have not yet been determined in a large prospective cohort with high (>80%) follow-up. In a systematic review36 on 10-year patient-reported outcomes, only three studies reported use of the IKDC: Lebel27 (n=154; 67% follow-up), Bourke8 (n=755; 79% follow-up), and Shelbourne52 (n=1276; 72% follow-up), with both larger studies excluding long-term graft failure or contralateral ACL tears. The KOOS has been reported in two studies, by Barenius4 and Moller39, with a total sample size of 226 and with both greater than 80% follow-up. The Marx activity scale has not been reported at 10 years.36 In a 2014 systematic review on the long-term natural history of ACL injuries, Chalmers et al.10 identified 27 studies that reported outcomes following surgical reconstruction (incidence of subsequent surgeries and Tegner activity level). Unfortunately, the mean sample size of the 27 operative cohorts was n=59 (range, 22 to 181), with a cumulative sample size of 1585 patients. As such, the ability to control for confounding factors which may influence outcomes has been extremely limited.
The Multicenter Orthopaedics Outcome Network (MOON) population cohort was designed in 2002 to prospectively determine which variables at the time of an ACL injury (including previous surgical history of the knee, patient demographics, mechanism of the current injury, surgical technique/choices at the time of the index ACL surgery, concomitant meniscal and/or articular cartilage pathology and treatment, among other potential modifiable and non-modifiable variables), would influence and predict both short and long-term outcomes following ACL reconstruction. This consortium has a proven ability to maintain 80% follow-up at 2 and 6 years as well as capture important time-dependent risk factors like activity level and additional surgery.12, 15, 18, 53 Utilizing this infrastructure, the objective of the current study was to identify both patient-specific risk factors as well as the sports-specific patient-reported outcomes measures (IKDC, KOOS, and Marx activity scale) 10 years after ACL reconstruction in a prospective longitudinal cohort. We hypothesized that meniscus and articular cartilage injuries (noted at the time of the index ACL reconstruction), revision ACL reconstruction, any subsequent knee surgeries occurring after the index ACL reconstruction, and certain demographic characteristics would be significant risk factors for inferior 10-year patient-reported outcomes.
METHODS
Setting and Study Population
After obtaining approval from each site’s respective institutional review boards, the multicenter consortium began enrolling patients in 2002. This consortium consisted of 7 sites (Vanderbilt University, Nashville, TN; Cleveland Clinic Foundation, Cleveland, OH; The Ohio State University, Columbus, OH: University of Iowa, Iowa City, IA; Washington University in St. Louis, MO; Hospital for Special Surgery, New York, NY; and University of Colorado, Boulder, CO) with 12 surgeons over a 3 year enrollment period (2002–2004). One university functioned as the data processing center for the study and was responsible for entering baseline data and collecting follow-up data on all patients. The trial is registered at ClinicalTrials.gov: NCT00463099. The details of enrollment, patient-reported outcome capture, surgical documentation at ACL reconstruction and method of follow-up has been described previously.12
All patients who underwent unilateral primary or revision ACL reconstruction surgery between January 1, 2002 and December 31, 2004, were eligible for enrollment. During this time frame, sites identified 1678 subjects who were slated to have an ACL reconstruction. A total of 1592 subjects met the study’s inclusion criteria and were enrolled into the study (Figure 1).
Figure 1.
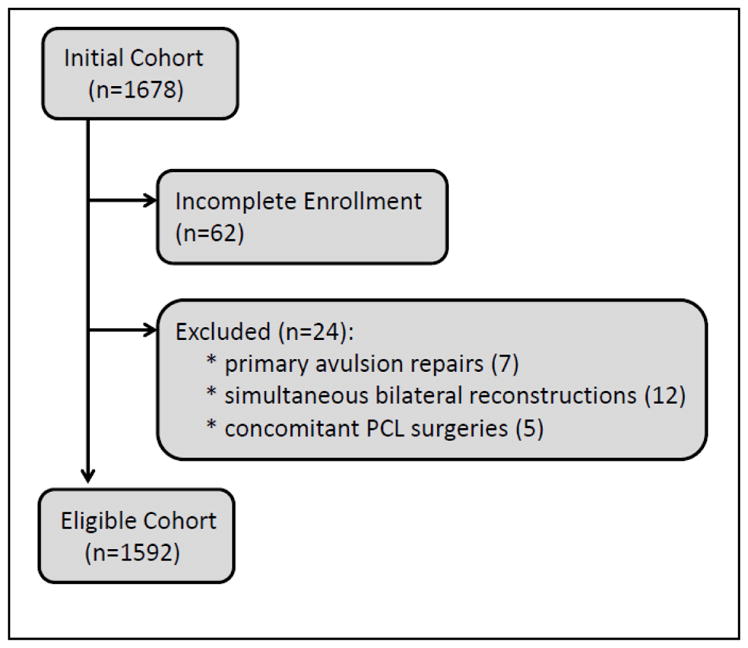
Enrollment Flow Diagram
Data Sources and Measurement
After informed consent was obtained, each participant was asked to complete a 13-page questionnaire encompassing baseline demographics, injury descriptors, sports participation level, comorbidities, knee surgical history, and patient-reported outcome measures that included the IKDC,22, 23 the five KOOS subscales (symptoms, pain, activities of daily living [ADL], sports and recreation, knee-related quality of life [QOL])49 and the Marx activity rating scale.38 The questions related to the IKDC and KOOS pertain to the time frame of the patient’s pain and function level within the past week, while the Marx activity rating scale queries the patient’s activity level from the past year. As such, the baseline IKDC and KOOS scores represent the ACL-deficient post-injury/pre-surgery state, while the baseline Marx activity score likely reflects the patient’s pre-injury state. The validity, reliability, responsiveness to clinical change, and minimal clinically meaningful differences of these instruments have been previously documented (IKDC22–24; KOOS44, 48, 49; Marx38). Each surgeon completed a detailed form that documented the results of the examination under anesthesia, surgical technique, and arthroscopic findings and treatment of concomitant meniscus and cartilage injury. Surgeon documentation of articular cartilage injury was recorded, based on the modified Outerbridge classification.14, 37, 43 Presence of linear cracks/fracture lines in the articular cartilage surfaces were also noted (if applicable). Meniscus injuries were classified by size, location, and partial versus complete tears, while treatment was recorded as not treated, repair, or extent of resection.16 After surgery, the patients were given a uniform set of standardized, evidence-based rehabilitation guidelines.59–61 Completed data forms were mailed from each participating site to the data coordinating center. Data from both the patient and surgeon questionnaires were scanned with Teleform software (Cardiff Software Inc., Vista, California, USA) using optical character recognition, and the scanned data were verified and exported to a master database. A series of logical error and quality control checks were subsequently performed. Cases which failed these checks were tagged and verified against the source documents in order to resolve prior to data analysis.
Follow-up
Two, six, and ten-year follow-up were completed by mail with re-administration of the same questionnaire that the patients completed at baseline (defined as the time of index ACL surgery). In addition, patients were also contacted to determine whether any underwent additional surgical knee procedures since baseline (e.g., revision ACL reconstruction on the ipsilateral knee, primary ACL reconstruction on the contralateral knee, and/or any arthroscopic procedures on either knee). Every effort was made to obtain the operative note on these additional surgical procedures. Follow-up was managed at a central coordinating site, but also required surgeon investigators and/or their respective sites to aid in contacting patents, in order to achieve a high level of follow-up.
Statistical Analyses
To determine the association between independent (risk factor) variables and 10-year patient-reported outcome measures, multivariable regression models were utilized. Multivariable analysis was used to determine which baseline variables measured at the time of index ACL surgery were significant predictors (risk factors) of the IKDC, KOOS, and Marx scores at 2, 6, and 10 years after surgery. Longitudinal analysis was performed using proportional odds ordinal logistic regression in lieu of linear regression models because the assumption of normal linear residuals was violated.51
The dependent variables (IKDC, KOOS, and Marx) were treated as continuous and consisted of the 10-year IKDC (scored 0 [worst] to 100 [best]), the five KOOS subscales (scored 0 [worst] to 100 [best]), and the Marx (scored 0 [low activity] to 16 [highest activity]). Independent patient covariates (risk factors) in the model included age at the time of surgery, gender, ethnicity, education level, body mass index (BMI), smoking status, sport played at the time of injury, competition level, baseline activity level as assessed using the Marx activity rating scale, and the baseline outcome measure (IKDC, KOOS, or Marx).
Independent surgical risk factors included surgeon, history of previous meniscal surgery (medial and/or lateral) at the time of index ACL reconstruction (yes/no), history of previous ACL reconstruction on the contralateral knee (yes/no), primary vs. revision surgery, graft type (autograft patellar bone-tendon-bone (BTB), autograft soft tissue, allograft BTB, allograft soft tissue), and concomitant MCL or LCL pathology. Meniscal injuries noted at the time of the index ACL reconstruction were classified by location (medial, lateral), size, and treatment (categorized as not treated, repaired, or percent excised). Excision options were categorized as none, 33%, 67%, or 100% excision for each segment (anterior and/or posterior). For this study, we used the largest excision in either segment. Articular cartilage variables noted at the time of the index ACL reconstruction were grouped by location to include the medial compartment (medial femoral condyle, medial tibial plateau), lateral compartment (lateral femoral condyle, lateral tibial plateau), and patellofemoral (patella, trochlea). Severity of articular cartilage degeneration in each location was categorized according to the modified Outerbridge classification14 and included normal, grade 1 (softening), grade 2 (fraying or fissures), grade 3 (partial thickness loss with fibrillation), or grade 4 (full thickness loss with exposed subchondral bone). If pathology was present in both locations within a compartment (e.g., lateral femoral condyle and lateral tibial plateau for the lateral compartment), the highest grade from either location was selected and extracted for analyses. Presence of linear cracks (fracture lines) in the articular cartilage surfaces were also noted (yes/no), and grouped in the same way as the articular cartilage degeneration pathology: medial compartment, lateral compartment, and patellofemoral compartment. Articular cartilage fracture pathology was defined as a ‘yes’ if any surface within a compartment presented with these linear cracks/fracture lines at the time of the index ACL reconstruction.
An additional independent surgical risk factor included in the model was preoperative laxity of the knee (defined as “high grade” laxity = yes or no). “High grade” laxity was determined by having either a Lachman or anterior drawer examination greater than a 10mm difference from the contralateral side or a 3+ pivot-shift during their examination under anesthesia. Previous literature has shown this definition to be predictive of increased odds of having a subsequent revision ACL surgery.34, 35
Description of the cohort was performed using counts and percentages for describing categorical data and medians and inner quartile range (IQR) for describing continuous data. Each of the seven outcomes was recorded at 10 years and risk factors were recorded at the time of surgery. The risk factors, baseline outcomes scores, BMI, smoking status and occurrence of subsequent surgery to the ipsilateral knee and contralateral knee were recorded at 2 years post-surgery and 6 years post-surgery. Therefore, a model at baseline, 2 years after surgery and 6 years after surgery was created to predict 10-year outcome scores with updated risk factors. Since the amount of missing information was small, only complete cases were used in the modeling and no imputation was used. All models were constructed using a proportional odds regression model, because this method has been reported to produce better predictive models.51 The baseline model was created using all risk factors available at baseline and reduced using a step-down reduction process, where the removal of each variable was evaluated by determining which had the smallest effect on the R2 and was stopped when the adjusted R2 was maximized and the Bayesian Information Criterion (BIC) was minimized. The models at 2 years and 6 years were created using the same variables in the baseline model, while updating BMI, smoking status and baseline outcome scores if they were included within the baseline model, and added subsequent surgeries. The performance of each model was measured using bootstrap optimize correction to the adjusted R2. Each model was then programmed into an online calculator for an easier assessment of a patient’s risk at time of surgery, 2 years or 6 years after surgery.
Regarding clinically meaningful change in score, we utilized 11 points for the IKDC,21 8 points for the KOOS,47 and 2 points for the Marx activity scale. All statistical analysis was performed using R open-source statistical software (2016, Vienna, Austria. URL https://www.R-project.org/).
RESULTS
Study Population
A total of 1592 patients fit the inclusion criteria and were enrolled. Ten-year follow-up was obtained on 83% (1320) [86% (1379) at 2 years, 86% (1375) at 6 years], while subsequent surgery information (performed after the index ACL surgery, if applicable) was obtained on over 90% of the cohort.
Baseline demographic and clinical characteristics of the analyzed cohort are provided in Table 1. The study population was 57% male with a median age of 24 years (IQR: 17, 35) at the time of their ACL reconstruction. Ninety percent (90%) underwent a primary ACL reconstruction, while the remaining 10% underwent a revision ACL reconstruction. Graft choice at the time of surgery was 42% autograft BTB, 31% autograft soft tissue, and 27% allograft. Thirty-seven percent (37%) had documented medial meniscal pathology at the time of their surgery, while 45% had documented lateral meniscal pathology. Articular cartilage pathology (grades 2–4) at the time of ACL surgery was less prevalent in this cohort: 24% in the medial compartment, 22% in the lateral compartment, and 22% in the patellofemoral compartment. Interestingly, 37% of patients in this cohort were classified as having “high grade” knee laxity preoperatively.
Table 1.
Baseline and Intermediate Patient and Surgical Characteristics of the Study Cohort
| Patient Demographic Factors
| |
|---|---|
| Age | 24 (17, 35) |
|
| |
| Gender | |
| • Male | 902 (57%) |
| • Female | 690 (43%) |
|
| |
| Ethnicity/Race | |
| • White | 1,333 (84%) |
| • Black | 135 (8%) |
| • Other | 114 (7%) |
| • Missing | 10 (1%) |
|
| |
| Baseline BMI | 25 (22.4, 28.1) |
| • Missing | 35 (2%) |
|
| |
| Baseline Smoking Status | |
| • Never | 1,248 (78%) |
| • Quit | 158 (10%) |
| • Current | 170 (11%) |
| • Missing | 16 (1%) |
|
| |
| Education level (years) | 14 (11, 16) |
| • Missing | 11 (1%) |
|
| |
| Main Sport | |
| • None | 123 (8%) |
| • Baseball / Softball | 141 (9%) |
| • Basketball | 358 (23%) |
| • Football | 174 (11%) |
| • Soccer | 212 (13%) |
| • Other | 577 (36%) |
| • Missing | 7 (0%) |
|
| |
| Competition Level | |
| • None | 205 (13%) |
| • Recreational | 527 (33%) |
| • Amateur | 222 (14%) |
| • High School | 440 (28%) |
| • College | 159 (10%) |
| • Semi-Pro / Professional | 30 (2%) |
| • Missing | 9 (0%) |
| Surgical Characteristics
| |
|---|---|
| Surgeon Volume | |
| • #1 | 75 (5%) |
| • #2 | 14 (1%) |
| • #3 | 459 (29%) |
| • #4 | 86 (5%) |
| • #5 | 27 (2%) |
| • #6 | 95 (6%) |
| • #7 | 301 (19%) |
| • #8 | 7 (0%) |
| • #9 | 72 (5%) |
| • #10 | 304 (19%) |
| • #11 | 147 (9%) |
| • #12 | 5 (0%) |
|
| |
| Reconstruction type | |
| • Primary | 1,439 (90%) |
| • Revision | 153 (10%) |
|
| |
| Graft type | |
| • Autograft (BTB) | 674 (42%) |
| • Autograft (Soft Tissue) | 496 (31%) |
| • Allograft (BTB) | 122 (8%) |
| • Allograft (Soft Tissue) | 300 (19%) |
|
| |
| Previous ACL reconstruction on contralateral knee | |
| • Yes | 138 (9%) |
| • No | 1,454 (91%) |
|
| |
| Previous medial meniscal surgery | |
| • Yes | 151 (9%) |
| • No | 1,441 (91%) |
|
| |
| Previous lateral meniscus surgery | |
| • Yes | 67 (4%) |
| • No | 1,525 (96%) |
|
| |
| MCL Pathology | |
| • Normal/Grade 1 | 1,497 (94%) |
| • Grades 2/3 | 95 (6%) |
|
| |
| LCL Pathology | |
| • Normal/Grade 1 | 1,554 (98%) |
| • Grades 2/3 | 38 (2%) |
|
| |
| Medial Meniscal pathology | |
| • No Tear | 999 (63%) |
| • No Treatment for Tear | 87 (5%) |
| • Repair | 199 (12%) |
| • Excision - 1/3 | 72 (5%) |
| • Excision - 2/3 | 193 (12%) |
| • Excision – all | 32 (2%) |
| • Other | 10 (1%) |
|
| |
| Lateral Meniscal pathology | |
| • No Tear | 880 (55%) |
| • No Treatment for Tear | 167 (10%) |
| • Repair | 99 (6%) |
| • Excision - 1/3 | 260 (16%) |
| • Excision - 2/3 | 155 (10%) |
| • Excision – all | 24 (2%) |
| • Other | 7 (0%) |
|
| |
| AC pathology (medial compartment) | |
| • Normal/Grade 1 | 1,207 (76%) |
| • Grade 2 | 229 (14%) |
| • Grades 3–4 | 156 (10%) |
|
| |
| AC pathology (lateral compartment) | |
| • Normal/Grade 1 | 1,252 (79%) |
| • Grade 2 | 231 (15%) |
| • Grades 3–4 | 109 (7%) |
|
| |
| AC pathology (patellofemoral) | |
| • Normal/Grade 1 | 1,241 (78%) |
| • Grade 2 | 202 (13%) |
| • Grades 3–4 | 149 (9%) |
|
| |
| AC pathology – linear cracks/fracture lines (medial compartment) | |
| • Yes | 119 (7%) |
| • No | 1,473 (93%) |
|
| |
| AC pathology – linear cracks/fracture lines (lateral compartment) | |
| • Yes | 176 (11%) |
| • No | 1,416 (89%) |
|
| |
| AC pathology – linear cracks/fracture lines (patellofemoral compartment) | |
| • Yes | 31 (2%) |
| • No | 1,561 (98%) |
|
| |
| Surgical exposure | |
| • 1 incision | 1,103 (69%) |
| • 2 incision | 488 (31%) |
| • Missing | 1 (0%) |
|
| |
| Notchplasty | |
| • Yes | 1,545 (97%) |
| • No | 47 (3%) |
|
| |
| High-grade Laxity | |
| • Yes | 587 (37%) |
| • No | 1,005 (63%) |
| Intermediate Variables
| |
|---|---|
| 2-year BMI | 25.1 (22.6, 28.1) |
| • Missing | 237 (15%) |
|
| |
| 6-year BMI | 25.8 (23.0, 28.7) |
| • Missing | 224 (14%) |
|
| |
| 2-year Smoking Status | |
| • Current | 127 (8%) |
| • Quit | 201 (13%) |
| • Never | 1,013 (64%) |
| • Missing | 251 (16%) |
|
| |
| 6-year Smoking Status | |
| • Current | 156 (10%) |
| • Quit | 238 (15%) |
| • Never | 965 (61%) |
| • Missing | 233 (15%) |
|
| |
| Subsequent surgery (ipsilateral knee) | |
| • None | 1,223 (77%) |
| • Scope | 221 (14%) |
| • Revision ACL reconstruction | 132 (8%) |
| • Total knee arthroplasty | 16 (1%) |
|
| |
| Subsequent surgery (contralateral knee) | |
| • None | 1,310 (82%) |
| • Scope | 78 (5%) |
| • ACL reconstruction | 140 (9%) |
| • Total knee arthroplasty | 3 (0%) |
| • Missing | 61 (4%) |
Key: Continuous variables are listed as median (25%, 75% quartiles). Categorical variables are listed as frequency counts, n, (percentage). BMI = body mass index; BTB = bone-patellar tendon-bone; AC = articular cartilage.
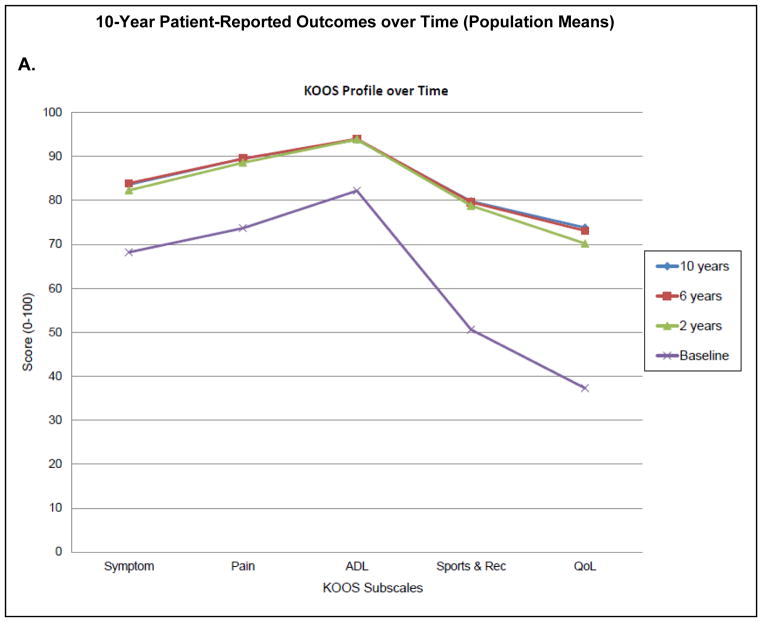
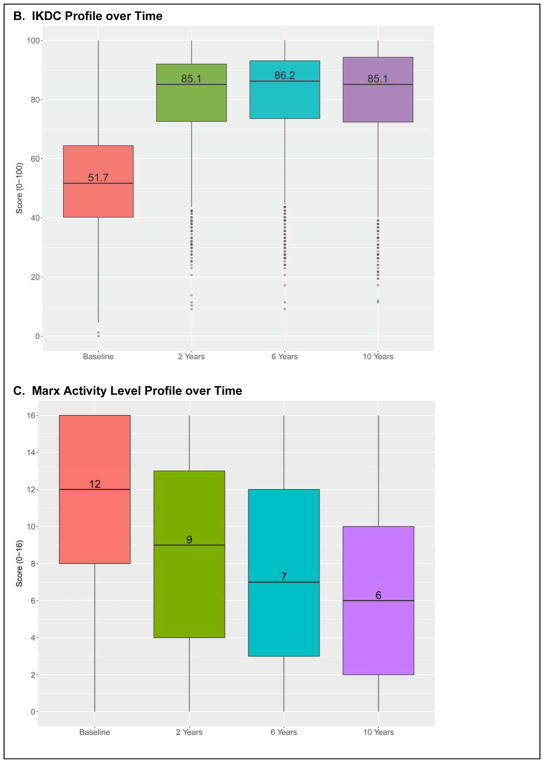
10-Year Population Outcomes
Both IKDC and KOOS scores for the entire cohort population significantly improved after 2 years and were maintained at 6 and 10 years (Table 2; Figure 2a,b). Interestingly, Marx activity level for the cohort population scores dropped markedly over time (Figure 2c), from a median score of 12 points at baseline, 9 points at 2 years, 7 points at 6 years, to 6 points at 10 years (Table 2).
Table 2.
Median (IQR) of KOOS, IKDC, and Marx Outcomes over Time
| Score Range | Baseline | 2 Years | 6 Years | 10 Years | |
|---|---|---|---|---|---|
| KOOS symptoms | 0–100 | 71 (57, 82) | 86 (75, 93) | 89 (75, 96) | 89 (75, 96) |
| KOOS pain | 0–100 | 75 (61, 89) | 92 (83, 97) | 94 (86, 100) | 94 (86, 100) |
| KOOS ADL | 0–100 | 88 (72, 96) | 99 (93, 100) | 99 (93, 100) | 99 (93, 100) |
| KOOS sports & recreation | 0–100 | 50 (25, 75) | 85 (70, 95) | 85 (70, 100) | 90 (70, 100) |
| KOOS QOL | 0–100 | 38 (25, 50) | 75 (56, 88) | 75 (63, 94) | 75 (63, 94) |
| IKDC | 0–100 | 52 (40, 64) | 85 (72, 92) | 86 (74, 93) | 85 (72, 94) |
| Marx Activity Level | 0–16 | 12 (8, 16) | 9 (4, 13) | 7 (3, 12) | 6, (2, 10) |
Key: ADL = activities of daily living; QOL = quality of life
Figure 2.
10-Year Patient-Reported Outcomes over Time (Population Means). Figure 2a: KOOS profile over time; Figure 2b: IKDC profile over time; Figure 2c: Marx activity level profile over time.
Patient-Specific Risk Factors
The patient-specific risk factors for inferior 10-year outcomes are reported in Table 3 and summarized in Table 4. The consistent risk factors for inferior 10-year outcomes across all outcome scales were lower baseline outcome scores, higher BMI, and having a medial meniscus procedure done prior to the index ACL reconstruction (Tables 3, 4). Other significant risk factors shown in the majority of our outcome scales (but not all), were female gender, higher age, smoker at baseline, lower baseline activity level, lower educational level, having a revision ACL reconstruction, having grades 3–4 articular cartilage pathology in the medial, lateral or patellofemoral compartments at the time of index ACL surgery, and having any subsequent ipsilateral surgery after the index ACL surgery (Tables 3, 4). Having either a lateral meniscus procedure done prior to the index ACL reconstruction or having a lateral meniscectomy at the time of the index ACL reconstruction were significant risk factors for poorer 10-year KOOS QOL outcomes, while having high-grade preoperative knee laxity was a significant independent risk factor for worse 10-year Marx activity levels.
Table 3.
Significant Odds Ratios (95% CI) for Variables in Model
| Comparison | Worse Outcome | IKDC | KOOS | Marx | |||||
|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Pain | ADL | Sports/Rec | QOL | |||||
|
| |||||||||
| Baseline Outcome Score | lower baseline score | 1.03 (1.03, 1.04) p<0.0001 |
1.02 (1.02, 1.03) p<0.0001 |
1.03 (1.02, 1.03) p<0.0001 |
1.03 (1.02, 1.04) p<0.0001 |
1.01 (1.01, 1.02) p<0.0001 |
1.02 (1.01, 1.03) p<0.0001 |
1.08 (1.06, 1.11) p<0.0001 |
|
|
| |||||||||
| Patient Demographics | |||||||||
|
| |||||||||
| Age | older age | 1.02 (1.01, 1.04) p=0.0007 |
1.02 (1.01, 1.04) p=0.0003 |
1.02 (1.01, 1.03) p=0.003 |
1.02 (1.01, 1.04) p=0.0007 |
0.97 (0.96, 0.98) p<0.0001 |
|||
|
| |||||||||
| Gender | male vs. female | females | 1.30 (1.04, 1.62) p=0.021 |
1.37 (1.09, 1.71) p=0.006 |
1.70 (1.38, 2.10) p<0.0001 |
||||
|
| |||||||||
| BMI | higher BMI | 0.96 (0.93, 0.98) p=0.0005 |
0.94 (0.92, 0.96) p<0.0001 |
0.96 (0.93, 0.98) p=0.0006 |
0.97 (0.94, 0.99) p=0.016 |
0.96 (0.94, 0.99) p=0.002 |
0.97 (0.95, 1.00) p=0.025 |
0.96 (0.94, 0.98) p=0.001 |
|
|
| |||||||||
| Smoking status | never vs. quit | quit smoking | 0.59 (0.42, 0.83) p=0.002 |
0.64 (0.46, 0.89) p=0.008 |
0.68 (0.49, 0.95) p=0.025 |
0.68 (0.48, 0.97) p=0.031 |
|||
|
| |||||||||
| never vs. current | current smoker | 0.62 (0.43, 0.90) p=0.011 |
0.66 (0.45, 0.95) p=0.026 |
0.60 (0.41, 0.88) p=0.009 |
0.62 (0.42, 0.90) p=0.013 |
||||
|
| |||||||||
| Education level | lower education | 1.06 (1.03, 1.10) p=0.0006 |
1.06 (1.02, 1.10) p=0.006 |
1.07 (1.02, 1.12) p=0.004 |
1.10 (1.06, 1.15) p<0.0001 |
||||
|
| |||||||||
| Baseline Marx Activity level | lower activity level | 1.03 (1.01, 1.06) p=0.013 |
1.03 (1.00, 1.06) p=0.031 |
1.03 (1.00, 1.05) p=0.024 |
1.08 (1.06, 1.11) p<0.0001 |
||||
|
| |||||||||
| Main sport | none vs. football | football | 0.47 (0.23, 0.96) p=0.038 |
||||||
|
| |||||||||
| none vs. other | none | 1.64 (1.06, 2.53) p=0.027 |
|||||||
|
| |||||||||
| Competition level | None vs. high school | none | 1.75 (1.01, 3.03) p=0.048 |
||||||
|
| |||||||||
| None vs. recreational | none | 1.70 (1.05, 2.76) p=0.03 |
|||||||
|
| |||||||||
| “High-grade” laxity | no vs. yes | yes | 1.08 (1.06, 1.11) p<0.0001 |
||||||
|
| |||||||||
| Surgical Factors | |||||||||
|
| |||||||||
| Reconstruction type | primary vs. revision | revision | 0.37 (0.26, 0.54) p<0.0001 |
0.51 (0.35, 0.75) p=0.0006 |
0.57 (0.39, 0.82) p=0.003 |
0.46 (0.32, 0.66) p<0.0001 |
0.44 (0.30, 0.65) p<0.0001 |
||
|
| |||||||||
| Medial meniscus procedure prior to index ACL reconstruction | no vs. yes | yes | 0.52 (0.36, 0.76) p=0.0006 |
0.64 (0.44, 0.93) p=0.019 |
0.60 (0.42, 0.88) p=0.008 |
0.43 (0.31, 0.62) p<0.0001 |
0.53 (0.36, 0.78) p=0.001 |
0.49 (0.33, 0.71) p=0.0002 |
0.48 (0.33, 0.69) p<0.0001 |
|
| |||||||||
| Lateral meniscus procedure prior to index ACL reconstruction | no vs. yes | yes | 0.54 (0.32, 0.90) p=0.019 |
||||||
|
| |||||||||
| Lateral meniscus pathology | no tear vs. excision | excision | 0.80 (0.64, 1.00) p=0.05 |
||||||
|
| |||||||||
| AC Medial pathology | normal vs. Grades 3–4 | Grades 3–4 | 0.70 (0.49, 0.99) p=0.047 |
0.65 (0.45, 0.94) p=0.022 |
0.68 (0.48, 0.98) p=0.036 |
||||
|
| |||||||||
| AC Lateral pathology | normal vs. Grades 3–4 | Grades 3–4 | 0.58 (0.39, 0.86) p=0.008 |
0.57 (0.38, 0.86) p=0.006 |
0.66 (0.44, 0.99) p=0.043 |
0.60 (0.40, 0.90) p=0.013 |
|||
|
| |||||||||
| AC Lateral pathology | normal vs. fracture lines | linear crack/fracture lines | 0.61 (0.43, 0.86) p=0.005 |
||||||
|
| |||||||||
| AC Patellofemoral pathology | normal vs. Grades 3–4 | Grades 3–4 | 0.58 (0.41, 0.83) p=0.003 |
0.46 (0.32, 0.66) p<0.0001 |
0.53 (0.37, 0.77) p=0.0009 |
0.58 (0.39, 0.84) p=0.005 |
0.51 (0.35, 0.74) p=0.0004 |
||
|
| |||||||||
| Intermediate Variables | |||||||||
|
| |||||||||
| 2-year Outcome score | lower 2 year score | 1.06 (1.06, 1.07) p<0.0001 |
1.06 (1.06, 1.07) p<0.0001 |
1.03 (1.02, 1.03) p<0.0001 |
1.08 (1.07, 1.10) p<0.0001 |
1.01 (1.01, 1.02) p<0.0001 |
1.05 (1.04, 1.05) p<0.0001 |
1.15 (1.12, 1.18) p<0.0001 |
|
|
| |||||||||
| 2-year Marx activity level | lower activity level | 1.03 (1.01, 1.05) p=0.015 |
1.03 (1.01, 1.06) p=0.011 |
1.03 (1.01, 1.05) p=0.015 |
1.15 (1.12, 1.18) p<0.0001 |
||||
|
| |||||||||
| 2-year BMI | higher BMI | 0.97 (0.95, 1.00) p=0.0005 |
0.94 (0.92, 0.96) p<0.0001 |
0.96 (0.94, 0.99) p=0.004 |
0.97 (0.94, 1.00) p=0.037 |
0.97 (0.94, 0.99) p=0.011 |
0.96 (0.93, 0.99) p=0.002 |
||
|
| |||||||||
| 2-year Smoking status | never vs. quit | quit smoking | 0.70 (0.52, 0.94) p=0.017 |
0.71 (0.53, 0.94) p=0.019 |
|||||
|
| |||||||||
| never vs. current | current smoker | 0.59 (0.39, 0.89) p=0.011 |
0.62 (0.41, 0.92) p=0.018 |
||||||
|
| |||||||||
| 2-year Subequent Surgery (ipsilateral knee) | none vs. scope | scope | 0.52 (0.38, 0.71) p<0.0001 |
0.50 (0.36, 0.69) p<0.0001 |
0.41 (0.30, 0.55) p<0.0001 |
0.54 (0.40, 0.74) p=0.0001 |
0.42 (0.31, 0.57) p<0.0001 |
2.24 (1.47, 3.41) p=0.0002 |
|
|
| |||||||||
| none vs. revision ACL reconstruction | Revision ACL reconstruction | 0.48 (0.33, 0.71) p=0.0002 |
0.48 (0.32, 0.70) p=0.0002 |
0.39 (0.27, 0.58) p<0.0001 |
0.51 (0.34, 0.77) p=0.0013 |
0.34 (0.23, 0.50) p<0.0001 |
|||
|
| |||||||||
| 2-year Subequent Surgery (contralateral knee) | none vs. scope | scope | 1.48 (1.04, 2.12) p=0.031 |
||||||
|
| |||||||||
| none vs. ACL reconstruction | ACL reconstruction | ||||||||
|
| |||||||||
| 6-year Outcome score | lower 6 year score | 1.10 (1.09, 1.11) p<0.0001 |
1.10 (1.09, 1.10) p<0.0001 |
1.03 (1.02, 1.03) p<0.0001 |
1.12 (1.11, 1.14) p<0.0001 |
1.01 (1.01, 1.02) p<0.0001 |
1.07 (1.07, 1.08) p<0.0001 |
1.24 (1.21, 1.27) p<0.0001 |
|
|
| |||||||||
| 6-year Marx activity level | lower activity level | 1.04 (1.02, 1.06) p=0.0004 |
1.04 (1.02, 1.07) p=0.002 |
1.24 (1.21, 1.27) p<0.0001 |
|||||
|
| |||||||||
| 6-year BMI | higher BMI | 0.95 (0.93, 0.97) p<0.0001 |
0.96 (0.94, 0.99) p=0.002 |
0.96 (0.94, 0.99) p=0.003 |
0.98 (0.95, 1.00) p=0.036 |
0.95 (0.93, 0.98) p<0.0001 |
|||
|
| |||||||||
| 6-year Smoking status | never vs. quit | quit smoking | 0.74 (0.57, 0.98) p=0.034 |
||||||
|
| |||||||||
| never vs. current | current smoker | 0.65 (0.45, 0.93) p=0.017 |
0.61 (0.42, 0.87) p=0.006 |
||||||
|
| |||||||||
| 6-year Subsequent Surgery (ipsilateral knee) | none vs. scope | scope | 0.57 (0.42, 0.76) p=0.0001 |
0.55 (0.41, 0.74) p<0.0001 |
0.41 (0.31, 0.55) p<0.0001 |
0.58 (0.42, 0.78) p=0.0004 |
0.42 (0.31, 0.56) p<0.0001 |
1.71 (1.15, 2.55) p=0.008 |
|
|
| |||||||||
| none vs. revision ACL reconstruction | Revision ACL reconstruction | 0.58 (0.40, 0.86) p=0.006 |
0.55 (0.38, 0.81) p=0.002 |
0.38 (0.26, 0.55) p<0.0001 |
0.61 (0.41, 0.92) p=0.018 |
0.32 (0.22, 0.47) p<0.0001 |
|||
|
| |||||||||
| 6-year Subsequent Surgery (contralateral knee) | none vs. scope | scope | |||||||
|
| |||||||||
| none vs. ACL reconstruction | ACL reconstruction | ||||||||
Key: ADL = activities of daily living; sports/rec = sports and recreation; QOL = quality of life; BMI = body mass index; AC = articular cartilage; ACL = anterior cruciate ligament
Table 4.
Significant Predictors for Worse Outcome 10 Years after ACL Reconstruction
| IKDC | KOOS sports & recreation | KOOS QOL | Marx Activity Level |
|---|---|---|---|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
||
|
|
|
|
|
|
|
|
|
|||
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
Sport or level of competition, graft type (autograft BTB, autograft soft tissue, allograft), MCL or LCL pathology, medial meniscus pathology at the time of ACL reconstruction, and surgeon were not found to be significant risk factors.
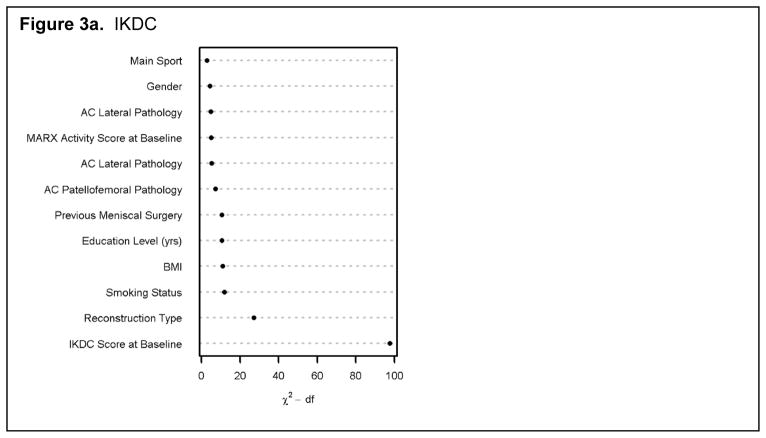
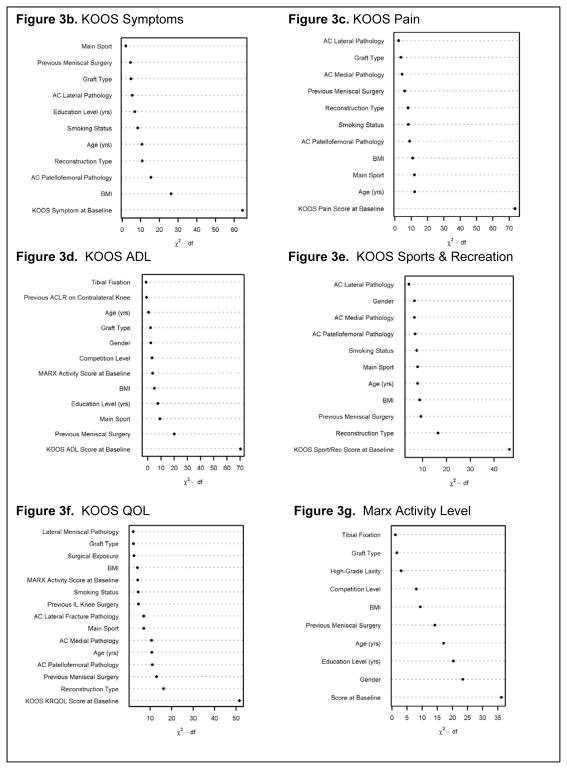
Relative Strength of Association between Predictor Variables and Outcomes
The relative strength of associations between predictor variables and IKDC, KOOS, and Marx activity levels at 10 years are shown in Figures 3a–g. These figures show the independent variables on the vertical axis, and the relative portion of the variation in the outcome accounted for by the given variable on the horizontal axis. This importance is measured by Wald chi-square statistics minus the degrees of freedom. The overarching result, regardless of outcome instrument, is that the score recorded at baseline has a dominating influence on the outcome score at 10 years post-surgery.
Figure 3.
The relative strength of association between predictor variables and IKDC (3a), KOOS (symptoms subscale – 3b; pain subscale – 3c; activities of daily living (ADL) – 3d; sports and recreation subscale – 3e; quality of life (QOL) – 3f), and Marx activity levels (3g) at 10 years.
Key: reconstruction type = primary versus revision ACL reconstruction; AC = articular cartilage; BMI = body mass index; IL = ipsilateral.
DISCUSSION
The major findings of this study are that both short- and long-term IKDC and KOOS outcomes significantly improve after an ACL reconstruction, and that these outcome levels are maintained through 10 years. However, Marx activity levels steadily decline over time. There are also patient-specific risk factors that significantly influence 10-year patient-reported outcomes. The risk factors which were found to negatively impact 10-year IKDC, KOOS, and Marx activity level outcomes included lower baseline outcome scores, higher BMI, being a smoker at baseline, history of a medial or lateral meniscus procedure done prior to the index ACL reconstruction, having a revision ACL reconstruction, lateral meniscectomy performed at the time of the index ACL reconstruction, grades 3–4 articular cartilage pathology in the medial, lateral or patellofemoral compartments at the time of the index ACL reconstruction, and having any subsequent ipsilateral surgery after the time of the index ACL reconstruction. Unfortunately, we still had insufficient sample size to model the interaction of meniscus injury and treatment with articular cartilage damage in the same compartment.
An unanticipated positive result was that the 10-year population IKDC and KOOS scores were similar to the 2- and 6-year levels (Figure 2a, b). However, patient activity level steadily declined over time. This finding, along with previous work from others,17, 26, 38 highlights the complexity of activity level. As we age, we may tend to be less active. However, unacceptable symptoms may accelerate this relative inactivity, and some treatments may improve symptoms so much that they allow for a higher activity.
The 10-year IKDC and KOOS QOL subscale identified nearly the same risk factors for worse outcome except for three variables: the IKDC uniquely identified lower education and the KOOS QOL uniquely identified higher age and previous lateral meniscectomy as risk factors for worse outcome. In our previous work at 2 and 6 years, the KOOS QOL scores tracked most closely with the IKDC.12 Thus, risk factors consistent across two “independent” scales are more likely to be more clinically meaningful. These risk factors should be explored to improve ACL reconstruction outcomes. Potential modifications to risk factors are to lower BMI, encourage smoking cessation, prevent/minimize subsequent ACL failure (revision ACL reconstructions), and identify optimal interventions for grades 3–4 articular cartilage pathology. A consistent observation was that a grade 3 or 4 articular cartilage lesion in the medial, lateral, or patellofemoral compartments at the time of the index ACL reconstruction predicted worse 10-year IKDC and KOOS outcome scores. The majority of these lesions were treated with chondroplasty/debridement, which negated our ability to model treatment options, including no treatment, debridement, and all various cartilage restorative procedures. Regardless, these patients should be counseled about a worse long-term prognosis. In the future, additional sample size may allow us to model a more diverse set of articular cartilage treatment options.
Surprisingly, meniscus pathology and treatment done at the time of the index ACL procedure were not risk factors for 10-year outcomes as they were at 6 years.12 The exception to this were patients who had a lateral meniscectomy at the time of the index ACL procedure were found to have significantly lower KOOS quality of life scores at 10 years. Meniscal repairs done at the time of the index ACL procedure did not affect 10 year outcomes. However, having a medial meniscus procedure prior to the index ACL reconstruction was an independent predictor of having significantly poorer IKDC, KOOS, and Marx activity level scores at 10 years.
The risk factors identified for poor 10-year activity levels included lower baseline activity level, higher age, female gender, higher BMI, lower education level, having a medial meniscus procedure done prior to the index ACL reconstruction, and having high-grade pre-operative knee laxity. These factors are similar to previously reported risk factors at 6-year follow-up.12
To assess an individual’s expected outcome, the entire spectrum of potential risk factors must be simultaneously evaluated either in a nomogram or risk calculator. An online risk calculator is available at Cleveland Clinic Quantitative Health Services (http://rcalc.ccf.org) for physicians and patients to evaluate their expected 10-year outcomes with baseline, 2-year, and 6-year data. The R2 value provides a measure of the variability in the 10-year IKDC, KOOS and Marx models, and was found to consistently improve from baseline to 2 years to 6 years. Thus, updating the baseline factors with current IKDC, KOOS and Marx scores, along with a patient’s current BMI, smoking status, and subsequent surgery information on either knee would provide more accurate estimates.
The main limitations of this study are that we did not obtain onsite measures (such as clinical exams, imaging, or other instrumented-based measures), and our sample size was too small to model the interaction between meniscus and articular cartilage pathology within the same compartment. The effect of treatment on grade 3 or 4 articular cartilage lesions could also not be assessed, given that the majority of these lesions were treated via chondroplasty. The lack of structural imaging (radiological or magnetic resonance imaging evaluation) to confirm the status of the articular cartilage and meniscus at 10+ years post-surgery is an area of future interest. An additional study limitation is the acknowledgement that baseline Marx activity scores likely reflect a patient’s pre-injury state, whereas the baseline KOOS and IKDC scores represent the ACL-deficient post-injury/pre-surgery state. Regarding activity levels over time, it remains unclear whether patients modified their activity level to one that allowed for acceptable symptoms or not.
CONCLUSIONS
Patients are able to perform sports-related functions and maintain a relatively high knee-related quality of life 10 years after ACL reconstruction, although activity level markedly declines over time. Multivariable analysis identified several key modifiable risk factors that significantly influence outcome. This information can be helpful to physicians counseling patients’ expectations of outcome after ACL reconstruction. Finally, intervention strategies for the potentially modifiable risk factors reported in this study should be developed and studied to assess their potential to improve outcomes following ACL reconstruction.
What is known about the subject
Several demographic risk factors and their treatment along with subsequent surgery have been identified in cohorts at intermediate follow-up (5–6 years) after ACL reconstruction.
What this study adds to existing knowledge
No comprehensive multivariable analysis of an ACL reconstruction prospective longitudinal cohort 10 years after surgery has been performed.
Acknowledgments
We would like to acknowledge the memory of Alexandra (Sandy) Kirkley, MD, who was a founding member of MOON 15 years ago and tragically died the next year with her husband in a plane crash. We have not forgotten her outstanding contributions to the field and she will always be remembered by the MOON group.
Research reported in this publication was partially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01AR053684 (K.P.S.), as well as by CTSA award No. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Institutes of Health. The project was also supported by the Vanderbilt Sports Medicine Research Fund, which received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics.
We wish to thank the research coordinators, analysts and support staff from the Multicenter Orthopaedic Outcomes Network (MOON) sites, whose efforts related to regulatory, data collection, subject follow-up, data quality control, analyses, and manuscript preparation have made this consortium successful.
We also thank all the subjects who generously enrolled and participated in this study.
Footnotes
Investigation performed at Vanderbilt University Medical Center, Nashville, Tennessee, USA
References
- 1.Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC. Long-term results of anterior cruciate ligament reconstruction using bone-patellar tendon-bone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy. 2012;28(8):1114–1123. doi: 10.1016/j.arthro.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 2.Ait Si Selmi T, Fithian D, Neyret P. The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee. 2006;13(5):353–358. doi: 10.1016/j.knee.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Sonesson S, Forssblad M, Kvist J. Comparison of patient-reported outcomes among those who chose ACL reconstruction or non-surgical treatment. Scand J Med Sci Sports. 2016 Jun 23; doi: 10.1111/sms.12707. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 5.Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB. Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthritis Cartilage. 2009;17(11):1434–1439. doi: 10.1016/j.joca.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 6.Bjornsson H, Samuelsson K, Sundemo D, et al. A randomized controlled trial with mean 16-Year follow-up comparing hamstring and patellar tendon autografts in anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(9):2304–2313. doi: 10.1177/0363546516646378. [DOI] [PubMed] [Google Scholar]
- 7.Bottoni CR, Smith EL, Shaha J, et al. Autograft versus allograft anterior cruciate ligament reconstruction: a prospective, randomized clinical study with a minimum 10-year follow-up. Am J Sports Med. 2015;43(10):2501–2509. doi: 10.1177/0363546515596406. [DOI] [PubMed] [Google Scholar]
- 8.Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. doi: 10.1177/0363546512454414. [DOI] [PubMed] [Google Scholar]
- 9.Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA. 2013;309(8):814–822. doi: 10.1001/jama.2013.879. [DOI] [PubMed] [Google Scholar]
- 10.Chalmers PN, Mall NA, Moric M, et al. Does ACL reconstruction alter natural history?: A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292–300. doi: 10.2106/JBJS.L.01713. [DOI] [PubMed] [Google Scholar]
- 11.Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976. doi: 10.1007/s00167-012-2251-8. [DOI] [PubMed] [Google Scholar]
- 12.Cox CL, Huston LJ, Dunn WR, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42(5):1058–1067. doi: 10.1177/0363546514525910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Culvenor AG, Oiestad BE, Holm I, Gunderson RB, Crossley KM, Risberg MA. Anterior knee pain following anterior cruciate ligament reconstruction does not increase the risk of patellofemoral osteoarthritis at 15- and 20-year follow-ups. Osteoarthritis Cartilage. 2017;25(1):30–33. doi: 10.1016/j.joca.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997;13(4):456–460. doi: 10.1016/s0749-8063(97)90124-9. [DOI] [PubMed] [Google Scholar]
- 15.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn WR, Wolf BR, Amendola A, et al. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32(8):1937–1940. doi: 10.1177/0363546504264586. [DOI] [PubMed] [Google Scholar]
- 17.Frobell RB, Svensson E, Gothrick M, Roos EM. Self-reported activity level and knee function in amateur football players: the influence of age, gender, history of knee injury and level of competition. Knee Surg Sports Traumatol Arthrosc. 2008;16(7):713–719. doi: 10.1007/s00167-008-0509-y. [DOI] [PubMed] [Google Scholar]
- 18.Hettrich CM, Dunn WR, Reinke EK, Group M, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41(7):1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38(3):448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 20.Holm I, Oiestad BE, Risberg MA, Gunderson R, Aune AK. No differences in prevalence of osteoarthritis or function after open versus endoscopic technique for anterior cruciate ligament reconstruction: 12-year follow-up report of a randomized controlled trial. Am J Sports Med. 2012;40(11):2492–2498. doi: 10.1177/0363546512458766. [DOI] [PubMed] [Google Scholar]
- 21.Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res. 2002;(402):95–109. doi: 10.1097/00003086-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 23.Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 24.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 25.Janssen RP, du Mee AW, van Valkenburg J, Sala HA, Tseng CM. Anterior cruciate ligament reconstruction with 4-strand hamstring autograft and accelerated rehabilitation: a 10-year prospective study on clinical results, knee osteoarthritis and its predictors. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1977–1988. doi: 10.1007/s00167-012-2234-9. [DOI] [PubMed] [Google Scholar]
- 26.Krych AJ, Harnly HW, Rodeo SA, Williams RJ., 3rd Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am. 2012;94(11):971–978. doi: 10.2106/JBJS.K.00815. [DOI] [PubMed] [Google Scholar]
- 27.Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36(7):1275–1282. doi: 10.1177/0363546508314721. [DOI] [PubMed] [Google Scholar]
- 28.Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061–1069. doi: 10.1007/s00167-013-2466-3. [DOI] [PubMed] [Google Scholar]
- 29.Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(12):2595–2603. doi: 10.1177/0363546511424720. [DOI] [PubMed] [Google Scholar]
- 30.Lind M, Lund B, Fauno P, Said S, Miller LL, Christiansen SE. Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):166–172. doi: 10.1007/s00167-011-1629-3. [DOI] [PubMed] [Google Scholar]
- 31.Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806–819. doi: 10.4085/1062-6050-49.3.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19(3):462–472. doi: 10.1007/s00167-010-1277-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. doi: 10.1055/s-0030-1247773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magnussen RA, Reinke EK, Huston LJ, Group M, Hewett TE, Spindler KP. Effect of high-grade preoperative knee laxity on anterior cruciate ligament reconstruction outcomes. Am J Sports Med. 2016;44(12):3077–3082. doi: 10.1177/0363546516656835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magnussen RA, Reinke EK, Huston LJ, Group M, Hewett TE, Spindler KP. Factors associated with high-grade lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(6):1080–1085. doi: 10.1016/j.arthro.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Magnussen RA, Verlage M, Flanigan DC, Kaeding CC, Spindler KP. Patient-reported outcomes and their predictors at minimum 10 years after anterior cruciate ligament reconstruction: a systematic review of prospectively collected data. Orthop J Sports Med. 2015;3(3):2325967115573706. doi: 10.1177/2325967115573706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. doi: 10.1177/0363546505275129. [DOI] [PubMed] [Google Scholar]
- 38.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 39.Moller E, Weidenhielm L, Werner S. Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):786–794. doi: 10.1007/s00167-009-0788-y. [DOI] [PubMed] [Google Scholar]
- 40.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 41.Oiestad BE, Holm I, Engebretsen L, Aune AK, Gunderson R, Risberg MA. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):942–949. doi: 10.1007/s00167-012-2161-9. [DOI] [PubMed] [Google Scholar]
- 42.Oiestad BE, Holm I, Engebretsen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10–15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45(7):583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 43.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 44.Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM. Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS) BMC Musculoskelet Disord. 2006;7:38. doi: 10.1186/1471-2474-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Risberg MA, Oiestad BE, Gunderson R, et al. Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med. 2016;44(5):1215–1224. doi: 10.1177/0363546515626539. [DOI] [PubMed] [Google Scholar]
- 46.Roos EM. Effectiveness and practice variation of rehabilitation after joint replacement. Curr Opin Rheumatol. 2003;15(2):160–162. doi: 10.1097/00002281-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 47.Roos EM, Klassbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol. 1999;28(4):210–215. doi: 10.1080/03009749950155562. [DOI] [PubMed] [Google Scholar]
- 48.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 50.Rossi MJ, Lubowitz JH, Guttmann D. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2002;30(1):152. doi: 10.1177/03635465020300011301. [DOI] [PubMed] [Google Scholar]
- 51.Senn S, Julious S. Measurement in clinical trials: a neglected issue for statisticians? Stat Med. 2009;28(26):3189–3209. doi: 10.1002/sim.3603. [DOI] [PubMed] [Google Scholar]
- 52.Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37(3):471–480. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 53.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. doi: 10.1177/0363546510383481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Steadman JR, Matheny LM, Hurst JM, Briggs KK. Patient-centered outcomes and revision rate in patients undergoing ACL reconstruction using bone-patellar tendon-bone autograft compared with bone-patellar tendon-bone allograft: a matched case-control study. Arthroscopy. 2015;31(12):2320–2326. doi: 10.1016/j.arthro.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 55.Struewer J, Ziring E, Frangen TM, et al. Clinical outcome and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using hamstring graft: follow-up after two and ten years. Int Orthop. 2013;37(2):271–277. doi: 10.1007/s00264-012-1653-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ulstein S, Bredland K, Aroen A, Engebretsen L, Rotterud JH. No negative effect on patient-reported outcome of concomitant cartilage lesions 5–9 years after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016 May 19; doi: 10.1007/s00167-016-4163-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 57.van der Hart CP, van den Bekerom MP, Patt TW. The occurrence of osteoarthritis at a minimum of ten years after reconstruction of the anterior cruciate ligament. J Orthop Surg Res. 2008;3:24. doi: 10.1186/1749-799X-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20(2):60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 59.Wright RW, Haas AK, Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7(3):239–243. doi: 10.1177/1941738113517855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I: continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21(3):217–224. doi: 10.1055/s-0030-1247822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21(3):225–234. doi: 10.1055/s-0030-1247823. [DOI] [PMC free article] [PubMed] [Google Scholar]