Abstract
Background
Non-invasive assessment of myocardial ischaemia is a cornerstone of the diagnosis of coronary artery disease. Measurement of myocardial blood flow (MBF) using positron emission tomography (PET) is the current reference standard for non-invasive quantification of myocardial ischaemia. Dynamic myocardial perfusion cardiovascular magnetic resonance (CMR) offers an alternative to PET and a recently developed method with automated inline perfusion mapping has shown good correlation of MBF values between CMR and PET. This study assessed the repeatability of myocardial perfusion mapping by CMR in healthy subjects.
Methods
Forty-two healthy subjects were recruited and underwent adenosine stress and rest perfusion CMR on two visits. Scans were repeated with a minimum interval of 7 days. Intrastudy rest and stress MBF repeatability were assessed with a 15-min interval between acquisitions. Interstudy rest and stress MBF and myocardial perfusion reserve (MPR) were measured for global myocardium and regionally for coronary territories and slices.
Results
There was no significant difference in intrastudy repeated global rest MBF (0.65 ± 0.13 ml/g/min vs 0.62 ± 0.12 ml/g/min, p = 0.24, repeatability coefficient (RC) =24%) or stress (2.89 ± 0.56 ml/g/min vs 2.83 ± 0.64 ml/g/min, p = 0.41, RC = 29%) MBF. No significant difference was seen in interstudy repeatability for global rest MBF (0.64 ± 0.13 ml/g/min vs 0.64 ± 0.15 ml/g/min, p = 0.80, RC = 32%), stress MBF (2.71 ± 0.61 ml/g/min vs 2.55 ± 0.57 ml/g/min, p = 0.12, RC = 33%) or MPR (4.24 ± 0.69 vs 3.73 ± 0.76, p = 0.25, RC = 36%). Regional repeatability was good for stress (RC = 30–37%) and rest MBF (RC = 32–36%) but poorer for MPR (RC = 35–43%). Within subject coefficient of variation was 8% for rest and 11% for stress within the same study, and 11% for rest and 12% for stress between studies.
Conclusions
Fully automated, inline, myocardial perfusion mapping by CMR shows good repeatability that is similar to the published PET literature. Both rest and stress MBF show better repeatability than MPR, particularly in regional analysis.
Electronic supplementary material
The online version of this article (10.1186/s12968-018-0462-y) contains supplementary material, which is available to authorized users.
Keywords: Myocardial perfusion, Cardiac magnetic resonance, Myocardial perfusion reserve
Background
There is increasing evidence that revascularisation decisions in patients with coronary artery disease (CAD) should be based on objective measurements of ischaemia rather than visual assessment [1–3]. Positron emission tomography (PET) is the current reference standard for non-invasive quantification of myocardial blood flow (MBF) and detection of ischaemia. Quantitative perfusion cardiovascular magnetic resonance (CMR) offers an alternative to PET with the advantage of lack of ionising radiation, higher spatial resolution and the added value of providing comprehensive data on left ventricular size, function and scar within a single study. Quantification of MBF by CMR has been validated in several small scale studies against microspheres, PET and invasive fractional flow reserve (FFR) measurements [4–7]. However, the wider adoption of quantitative perfusion CMR has been limited by the need for time consuming, off line processing and poor repeatability [8]. Recently, a new motion corrected (MOCO) myocardial perfusion CMR method with Gadgetron-based automated in-line perfusion mapping has been proposed, allowing free breathing acquisition and pixel-wise quantification of MBF [9]. The method has been shown to have good correlation with PET in patients with stable CAD [10], but needs to proceed through a number of validation steps before it can be used clinically and as a research surrogate endpoint. In this study, the repeatability of myocardial perfusion mapping by CMR was assessed in healthy subjects.
Methods
Study population
Forty-two healthy subjects were recruited (23 female, median age 23 yrs., IQR 22–29 yrs). Exclusion criteria were known cardiovascular disease, hypertension, hyperlipidaemia, diabetes mellitus, smoking and any contraindication to CMR, adenosine or gadolinium based contrast agents.
Study protocol
The 42 healthy subjects underwent repeat CMR studies in two groups to allow assessment of intrastudy and interstudy repeatability of rest and stress MBF as well as MPR.
Group 1: 30 subjects underwent CMR studies on two separate visits. In visit 1, they had three rest perfusion scans and in visit 2, they had two stress and one rest perfusion scans. The acquisition of three rest scans in visit 1 allowed us to study the short-term repeatability of rest MBF with minimal physiological variation and to assess the effect of residual gadolinium (Gd) on repeated perfusion measurements. The fourth rest scan acquired in visit 2 was used to assess long-term variability of rest MBF. The two stress scans in visit 2 assessed short-term variability of stress MBF.
Group 2: 20 subjects (8 from the first cohort and 12 additional subjects) had stress followed by rest perfusion scans in two separate visits to assess long-term repeatability of stress MBF and MPR (Fig. 1).
Fig. 1.
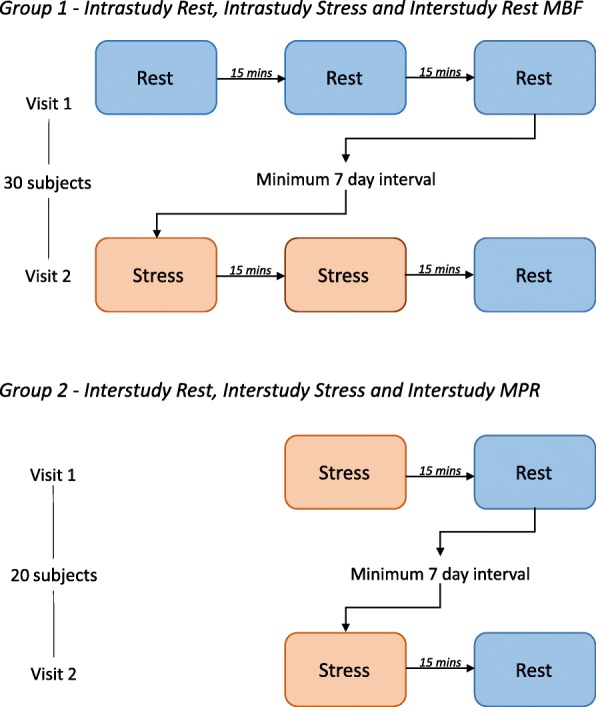
Study Protocol. Group one consisted of 30 volunteers, Group two included 8 volunteers from Group one, and an additional 12 healthy volunteers
All CMR studies were carried out on a 3 T scanner (Magnetom Prisma, Siemens Healthineers, Erlangen, Germany). A minimum of 7 days was allowed between each visit (mean 41, SD 40 days). Subjects were advised to avoid caffeine for 24 h before each scan. Survey images were acquired, followed by vertical and horizontal long axis images to plan the short axis view for perfusion in three slice positions (basal, mid and apex).
Pharmacological stress was achieved with adenosine infusion at 140mcg/kg/min for a minimum of 3 min. The dose was increased to 175mcg/kg/min after 2 min if there was no symptomatic or haemodynamic response to adenosine. Subjects were monitored for symptoms and heart rate throughout the infusion, blood pressure and heart rate were recorded every 2 min during adenosine infusion. An intravenous bolus of 0.05 mmol/kg gadobutrol (Gadovist, Leverkusen, Germany) was administered at 5 ml/s followed by a 20 ml saline flush for each perfusion scan. A minimum gap of 15 min was maintained between each perfusion scan to allow for equilibrium of gadolinium kinetics from the previous series, and to ensure that the effects of adenosine had resolved.
Perfusion imaging used a dual sequence approach which employed separately optimized sequences for the myocardium and blood pool signals in order to avoid blood pool signal saturation. Full details of the myocardial perfusion sequence have been previously described [9]. Both sequences were electrocardiogram (ECG) triggered saturation recovery prepared. The sequence used for imaging the left ventricular (LV) blood pool to estimate the arterial input function (AIF) used a low flip angle FLASH low resolution protocol with 2 echos such that the echo times were short to minimize T2* losses at high concentration, and so that remaining T2* losses could be estimated and corrected. Parameters for this protocol were: flip angle 5 degrees, matrix 48 × 34, parallel imaging factor 2, TEs 0.76 and 1.76 ms, TR 2.45 ms, slice thickness 10 mm, saturation preparation used 6-pulse sequence, saturation delay TS 24 ms to k-space center, imaging duration 42 ms, total sequence duration 57 ms acquired immediately following the R-wave trigger. The myocardial imaging protocol in this study used a FLASH readout with typical imaging parameters: flip angle 14 degrees, spatial resolution 1.9 × 2.4 mm2, slice thickness 8.0 mm, TE/TR 1.0/2.1 ms, matrix size 192 × 111, field of view 360 × 270 mm2, parallel imaging acceleration factor 3, saturation recovery time (TS) 110 ms to center of k-space, trigger delay 72 ms, imaging duration 59 ms, saturation preparation used 5-pulse sequence, total duration including saturation 143 ms per slice, enabling acquisition of 3-slices plus AIF sequence in less than 500 ms permitting hear rates up to 120 bpm. Both AIF and myocardial imaging sequences included 3 measurements of proton density (PD) weighted images with flip angle of 5 degrees used for surface coil intensity correction. Slice spacing was varied on per patient basis to cover the LV.
In-line automatic reconstruction and post-processing were implemented within the Gadgetron software framework [9]. Images were motion corrected and then corrected for surface coil intensity variation based on the proton density weighted images. Signal intensity data were converted to Gd concentration (mmol/L) based on automatically generated look-up tables for the magnetization Bloch simulation. AIF data were extracted from the low-resolution Gd concentration images using automated segmentation of the LV cavity. MBF was calculated on a pixel-wise basis in the high-resolution images by blood tissue exchange (BTEX) model constrained deconvolution incorporating estimation of the delay time between bolus arrival in the LV cavity and the tissue of interest. Details of the reconstruction and processing including conversion to [Gd] concentration units, blood pool signal segmentation, and BTEX modeling are previously reported [9].
Quantitative analysis
The in-line processing on the scanner console included the image reconstruction, respiratory motion correction, LV blood pool segmentation, conversion of signals to [Gd] concentration units, and quantitative tissue mapping. These steps were fully automatic. For a protocol with AIF plus 3-slices acquired for 60 measurements, the processing time was < 3 min.
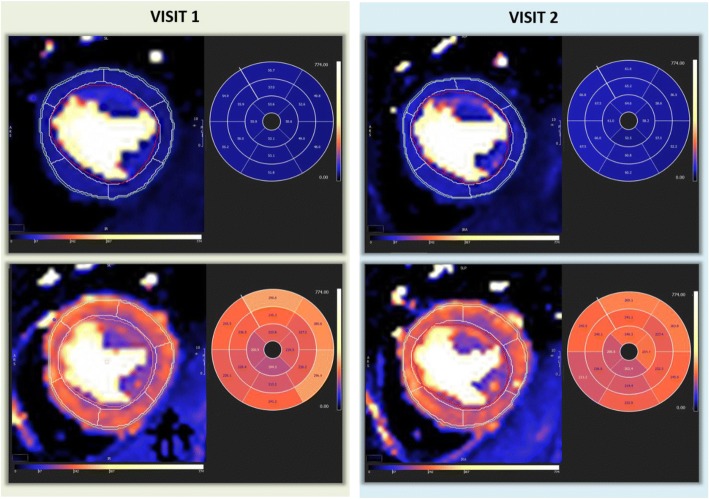
The analysis of the quantitative maps was performed off-line on a separate workstation using CVi 42 software (Circle Cardiovascular Imaging, Calgary, Canada). This process was performed manually by tracing endo- and epi-cardial contours for each slice and marking RV insertion points; a 16-segment American Heart Association (AHA) model was then applied [11]. In order to minimise partial volume effect, a 10% offset was applied to endocardial and epicardial borders (Fig. 2). MBF was recorded for each of the 16 segments. Where the LV outflow tract was included in the basal slice, or partial volume effect meant segments were too thin to contour, these segments were excluded from further analysis. Analysis time was less than 5 min per set of perfusion maps.
Fig. 2.
Rest and Stress MBF maps from visit 1 and visit 2 for the same subject. Values are displayed as ml/100 g/min
Segmental values were averaged to give values for slice, coronary territory and global MBF. Coronary territories consisted of: left anterior descending coronary artery (LAD) - segments 1, 2, 7, 8, 13 and 14, circumflex coronary artery (Cx) - segments 5, 6, 11, 12 and 16, and right coronary artery (RCA) – segments 3, 4, 9, 10 and 15.
Correlation of MBF with HR and RPP were analysed, and where significant correlation was present, MBF values were corrected. Values for resting MBF were corrected for heart rate (HR) by dividing by scan heart rate and multiplying by the mean resting HR (62 bpm) among all subjects. Interstudy repeatability was analysed on a regional basis for slices (basal, mid and apical) and coronary territories (LAD, Cx and RCA). MPR was calculated as a ratio of stress MBF:rest MBF.
Reproducibility of analysis
Intra- and inter-observer variability were assessed by repeating the analysis of 10 subject data sets for stress and rest after 1 month, by the same observer (LB) and by a second observer (SO). The second observer was blinded to the previous results.
Statistical analysis
Analysis was performed using SPSS 23 (International Business Machines, Armonk, New York, USA). Normality of data distribution was assessed using Shapiro-Wilk test. Data are presented as mean ± standard deviation (SD). Repeatability was assessed using a wide range of methods to facilitate comparison with the inconsistent methods in the published literature. The three intrastudy rest scans were compared using repeated measures analysis of variance (ANOVA) with Bonferroni adjustment for post-hoc analysis. All other repeated mean MBF and inter- and intra- observer variability were compared using paired t tests. Coefficient of variation (CV) was calculated using the root mean square method [12]. Reproducibility coefficient (RC) was calculated as 1.96*SD of difference and given as a percentage of the total mean and used to demonstrate bias and accuracy with Bland Altman plots. Reliability was assessed using intraclass correlation coefficient (ICC). All statistical tests were two-tailed and a p value < 0.05 was considered significant.
Results
All subjects tolerated repeated CMR scans and adenosine stress well. One subject did not attend the second visit for assessment of intrastudy rest repeatability, another was not included in intrastudy stress analysis due to triggering problems causing artefact on the MBF maps on one stress scan. One result was excluded from analysis of repeat stress MBF or MPR due to lack of stress response on one visit, confirmed by lack of symptoms despite increased adenosine dose, haemodynamic response and splenic switch off. One result was excluded from comparison of MPR due to severe artefact on rest perfusion maps.
Intrastudy repeatability
Twenty-nine studies were analysed for intrastudy repeatability of resting and hyperaemic MBF from the two separate visits of Group 1.
Mean global MBF at rest was 0.69 ± 0.13 ml/g/min, 0.65 ± 0.13 ml/g/min and 0.62 ± 0.12 ml/g/min for scans 1, 2 and 3 respectively (Table 1). There was a significant difference in mean MBF on the first rest scan compared to both the second (p = 0.01) and third (p = 0.001). There was no significant difference between the second and third scans (Fig. 3). Coefficient of variation was 11–12% between the first scan and repeats, and 8% between second and third scans with good reliability (ICC = 0.8, RC 24%). Assessment of repeatability with Bland-Altman plots (Fig. 4) showed a bias of − 0.03 ml/g/min (3.9% of the mean).
Table 1.
Intrastudy repeatability of global MBF measurements
| Test 1 ml/g/min |
Test 2 ml/g/min | Difference in mean ml/g/min | p | RC | RC (%) | CV (%) | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rest | < 0.01 | ||||||||||
| Rest 1 - Rest 2 | 0.69 | ±0.13 | 0.65 | ±0.13 | −0.04 | ±0.09 | 0.04 | 0.19 | 28.5 | 10.9 | 0.73 |
| Rest 1 - Rest 3 | 0.69 | ±0.13 | 0.62 | ±0.12 | −0.07 | ±0.10 | 0.02 | 0.23 | 35.2 | 11.9 | 0.58 |
| Rest 2 - Rest 3 | 0.65 | ±0.13 | 0.62 | ±0.12 | −0.03 | ±0.07 | 0.24 | 0.15 | 23.8 | 7.93 | 0.80 |
| Stress | |||||||||||
| Stress 1- Stress 2 | 2.89 | ±0.56 | 2.83 | ±0.64 | −0.06 | ±0.42 | 0.41 | 0.82 | 28.5 | 10.6 | 0.76 |
p – from repeated measures ANOVA and level of significance using Bonferroni post-hoc analysis for rest data, Student’s T-test for stress values
RC repeatability coefficient, RC (%)repeatability coefficient as percentage of the mean, CV within subject coefficient of variation, ICC intraclass correlation coefficient
Fig. 3.
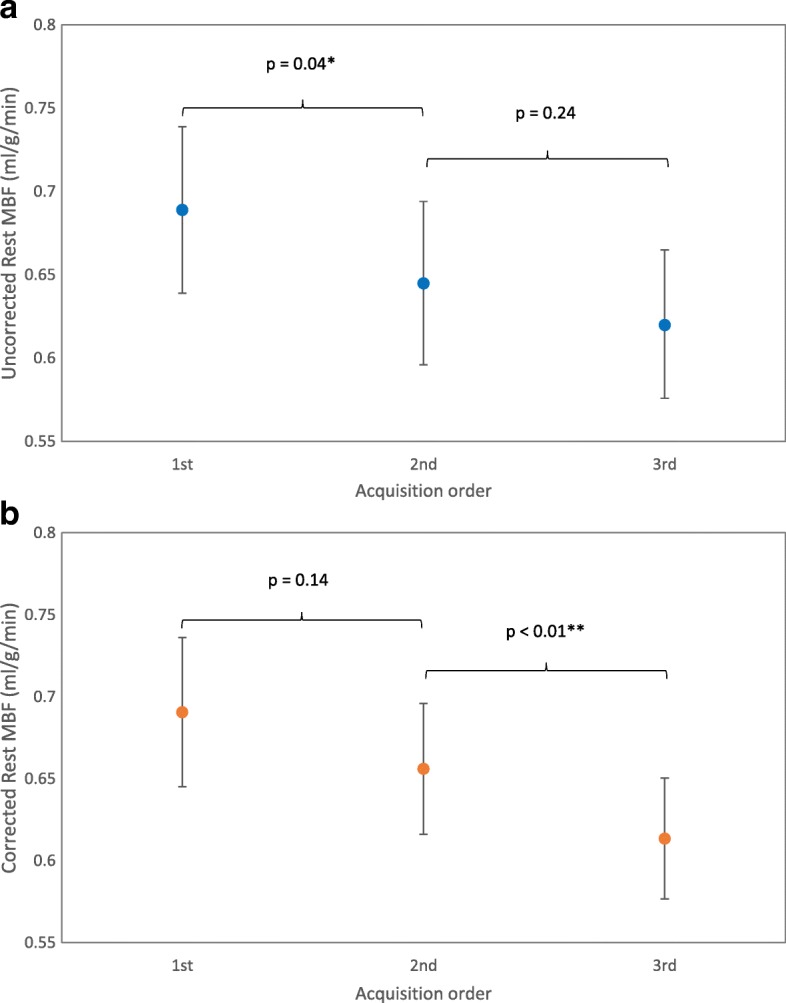
Global resting myocardial blood flow (MBF) on repeat throughout the same visit. A – uncorrected values, B – corrected values (mean and 95% confidence interval of the mean)
Fig. 4.
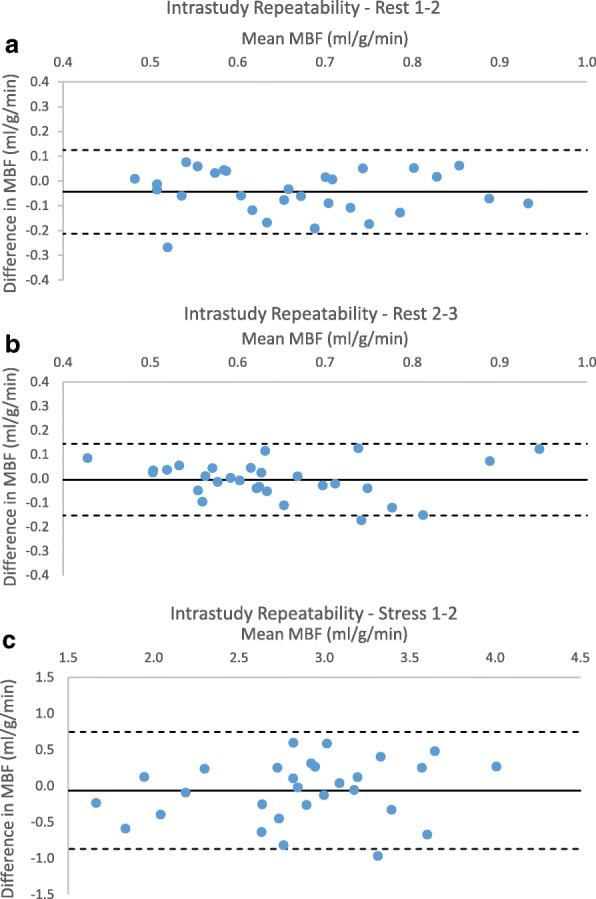
Intrastudy myocardial blood flow (MBF) repeatability (a) Rest 1–2 (b) Rest 2–3 (c) Stress 1–2
Resting MBF correlated with HR (r = 0.49, p < 0.01), therefore MBF corrected for HR was also analysed (Table 2). A significant difference was still present between the groups (p < 0.01) and the decrease with sequential scans remained (0.69 ml/g/min, 0.66 ml/g/min and 0.61 ml/g/min for scans 1, 2 and 3). A significant difference was seen between scan 3 and the other two results (p < 0.01). Whilst the level of significance differed when corrected for heart rate, both sets of values showed a trend to decrease with repeated measurement (Fig. 3).
Table 2.
Global rest myocardial blood flow (MBF) corrected for heart rate (HR)
| Test 1 ml/g/min | Test 2 ml/g/min | Difference in mean ml/g/min | p | RC | RC (%) | CV (%) | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rest | < 0.01 | ||||||||||
| Rest 1 - Rest 2 | 0.69 | ±0.12 | 0.66 | ±0.10 | −0.03 | ±0.09 | 0.14 | 0.18 | 27.3 | 9.9 | 0.66 |
| Rest 1 - Rest 3 | 0.69 | ±0.12 | 0.61 | ±0.10 | −0.07 | ±0.07 | < 0.01 | 0.20 | 30.3 | 10.5 | 0.62 |
| Rest 2 - Rest 3 | 0.66 | ±0.10 | 0.61 | ±0.10 | −0.04 | ±0.06 | < 0.01 | 0.15 | 23.7 | 8.3 | 0.72 |
p – from repeated measures ANOVA and Bonferroni post-hoc analysis
RC repeatability coefficient, RC (%)repeatability coefficient as percentage of the mean, CV within subject coefficient of variation, ICC intraclass correlation coefficient
Stress MBF showed no significant difference between the two repeat acquisitions in visit 2 (mean difference − 0.06 ± 0.42, p = 0.41). Within subject coefficient of variation was 11% with good correlation and repeatability (ICC 0.76, RC 29%). One value was outside the limits of agreement on assessment with Bland-Altman plots, with a bias of 2.2% of the mean (Fig. 4). Stress RPP was comparable between both studies (11,202 ± 2188 vs 10,858 ± 1877, p = 0.09) as was the percentage increase in HR (47.3 ± 18.8% vs 44.4 ± 18.4%, p = 0.24) and RPP (51.1 ± 21.7% vs 46.9 ± 22.1%, p = 0.14).
Interstudy repeatability
Global perfusion analysis
A total of 41 studies were analysed for interstudy repeatability of resting MBF with an average gap of 27 days between scans in visits 1 and 2. No significant difference was seen in MBF between scans (mean difference 0.004 ± 0.1 ml/g/min, p = 0.8) (Table 3). Within subject coefficient of variation was 11%, RC 32% and bias was < 1% of the mean (Fig. 5).
Table 3.
Interstudy repeatability of MBF measurements – by slice and coronary artery territory
| Test 1 ml/g/min |
Test 2 ml/g/min |
Difference in mean ml/g/min | p | RC | RC (%) | CV (%) | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rest | |||||||||||
| Global | 0.64 | ±0.13 | 0.64 | ±0.15 | 0.004 | ±0.10 | 0.8 | 0.20 | 31.5 | 11.3 | 0.74 |
| Basal | 0.66 | ±0.14 | 0.67 | ±0.16 | 0.015 | ±0.13 | 0.46 | 0.25 | 37.7 | 13.6 | 0.65 |
| Mid | 0.64 | ±0.14 | 0.64 | ±0.15 | −0.003 | ±0.10 | 0.87 | 0.20 | 31.0 | 11.2 | 0.76 |
| Apex | 0.60 | ±0.13 | 0.60 | ±0.15 | −0.003 | ±0.10 | 0.86 | 0.20 | 33.4 | 11.5 | 0.73 |
| P | 0.13 | 0.089 | |||||||||
| LAD | 0.69 | ±0.16 | 0.68 | ±0.16 | −0.003 | ±0.11 | 0.86 | 0.22 | 32.2 | 11.7 | 0.75 |
| Cx | 0.60 | ±0.13 | 0.60 | ±0.14 | 0.005 | ±0.11 | 0.74 | 0.20 | 34.0 | 11.8 | 0.70 |
| RCA | 0.61 | ±0.12 | 0.62 | ±0.15 | 0.01 | ±0.11 | 0.59 | 0.22 | 35.6 | 12.6 | 0.66 |
| P | 0.01* | 0.04* | |||||||||
| Stress | |||||||||||
| Global | 2.71 | ±0.61 | 2.55 | ±0.57 | −0.161 | ±0.43 | 0.12 | 0.87 | 33.1 | 12.2 | 0.72 |
| Basal | 3.01 | ±0.80 | 2.80 | ±0.74 | −0.209 | ±0.51 | 0.09 | 1.05 | 36.1 | 13.2 | 0.76 |
| Mid | 2.48 | ±0.55 | 2.39 | ±0.51 | −0.092 | ±0.44 | 0.38 | 0.86 | 35.4 | 13.4 | 0.66 |
| Apex | 2.62 | ±0.65 | 2.42 | ±0.56 | −0.201 | ±0.62 | 0.17 | 1.24 | 49.2 | 16.3 | 0.48 |
| P | 0.05 | 0.07 | |||||||||
| LAD | 2.79 | ±0.61 | 2.62 | ±0.55 | −0.167 | ±0.39 | 0.08 | 0.82 | 30.3 | 10.8 | 0.75 |
| Cx | 2.69 | ±0.61 | 2.51 | ±0.66 | −0.180 | ±0.47 | 0.12 | 0.97 | 37.3 | 15.4 | 0.71 |
| RCA | 2.53 | ±0.61 | 2.44 | ±0.56 | −0.096 | ±0.47 | 0.39 | 0.92 | 37.0 | 13.6 | 0.68 |
| P | 0.442 | 0.629 | |||||||||
| MPR | |||||||||||
| Global | 4.24 | ±0.69 | 3.73 | ±0.76 | −0.214 | ±0.76 | 0.25 | 1.46 | 36.4 | 13.3 | 0.46 |
| Basal | 4.53 | ±0.90 | 4.27 | ±1.00 | −0.262 | ±0.89 | 0.23 | 1.78 | 40.4 | 15.3 | 0.55 |
| Mid | 3.84 | ±0.70 | 3.73 | ±0.66 | −0.113 | ±0.83 | 0.57 | 1.60 | 42.4 | 15.5 | 0.26 |
| Apex | 4.42 | ±0.90 | 4.12 | ±0.76 | −0.293 | ±1.04 | 0.25 | 2.06 | 48.1 | 16.0 | 0.30 |
| p | 0.047* | 0.130 | |||||||||
| LAD | 3.96 | ±0.58 | 3.83 | ±0.81 | −0.128 | ±0.71 | 0.45 | 1.35 | 35.3 | 13.1 | 0.50 |
| Cx | 4.47 | ±0.93 | 4.14 | ±0.93 | −0.325 | ±0.86 | 0.13 | 1.76 | 40.8 | 15.7 | 0.54 |
| RCA | 4.06 | ±0.76 | 3.91 | ±0.66 | −0.150 | ±0.89 | 0.49 | 1.72 | 43.3 | 15.7 | 0.23 |
| p | 0.118 | 0.480 | |||||||||
RC repeatability coefficient, RC (%)repeatability coefficient as percentage of the mean, CV within subject coefficient of variation, ICC intraclass correlation coefficient
p – level of significance using Student’s T-test
*=significant at p < 0.05
Fig. 5.
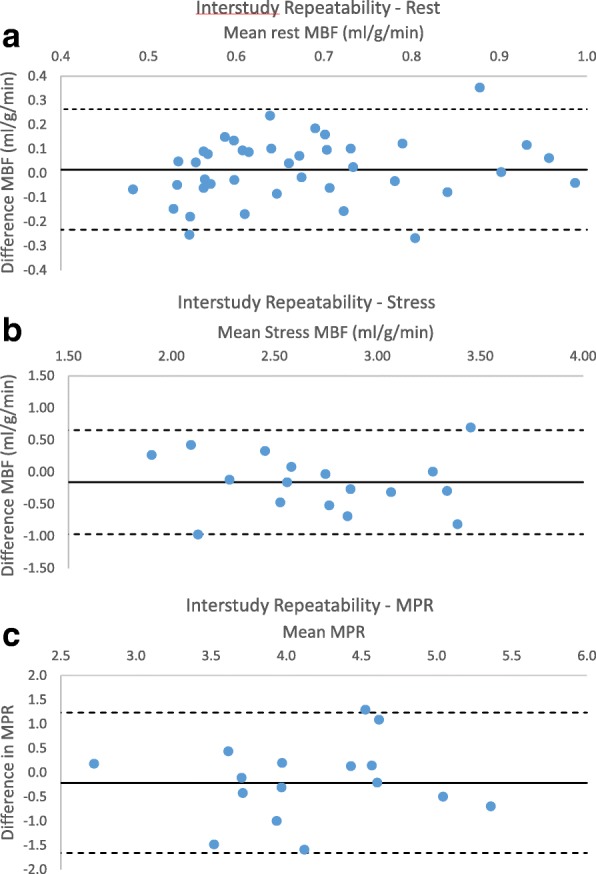
Interstudy repeatability (a) Rest MBF (b) Stress (c) myocardial perfusion reserve (MPR)
Nineteen pairs of scans were analysed for interstudy stress MBF and 18 for interstudy MPR in Group 2. The percentage increase in HR (52.1 ± 26.6% vs 50.4 ± 23.4%, p = 0.7) and RPP (56.6 ± 32.7% vs 52.1 ± 26.6%, p = 0.11) between rest and stress scans showed no significant difference between visits. Adenosine stress MBF had good repeatability with ICC 0.72 and RC 33%. CV was 12% and bias was − 6% of the mean. Repeat MPR had a CV of 13.3 with no significant difference between the two measurements. Weaker correlation was seen compared to stress and rest, although this remained significant (ICC 0.46, p < 0.01).
Regional perfusion analysis
At rest there was no significant difference between slices (p = 0.13 and 0.09 for first and second scans) (Table 3). No significant difference was seen in individual slices between scans and all showed good repeatability and correlation (p < 0.01 in all slices) (Additional file 1: Figure S1). Coefficient of variation was 13.6, 11.2 and 11.5% for basal, mid and apical slices respectively.
Mean MBF at stress was 3.01 ± 0.8 ml/g/min, 2.48 ± 0.55 ml/g/min and 2.62 ± 0.65 ml/g/min on the first visit and 2.8 ± 0.74 ml/g/min, 2.39 ± 0.51 ml/g/min and 2.42 ± 0.56 ml/g/min in basal, mid and apical slices respectively. No significant difference was seen between scans for any slice. The apical slice exhibited the lowest repeatability, ICC 0.46, RC 49% and within subject coefficient of variation 16%. Good correlation was seen in all slices (Additional file 1: Figure S1).
No significant difference was seen in mean MPR between visits for any slice, RCs were 40, 42 and 48% and CVs 15, 15 and 16% for basal mid and apical slices.
Coronary territory flows were significantly different between vessel territories at rest on both visits. MBF in the LAD was higher than the Cx territory on both visits (mean difference 0.09 ml/g/min, p = 0.01 on the first scan, and 0.08 ml/g/min, p = 0.04 on the second). There was good correlation within all coronary territories between scans (Additional file 2: Figure S2). All territories showed similar ICC (0.66–0.75) and repeatability coefficients (32–36%). CVs were very similar between territories (11.7, 11.8 and 12.6%).
No significant difference was seen between coronary territories in stress MBF, or in calculated MPR at either scan. All coronary territories showed good repeatability and correlation between scans. Coefficients of variation ranged between 10.8 and 15.4%, being highest in the circumflex territory.
No significant difference was seen in MPR in any coronary territory between visits. The LAD and Cx territories showed acceptable correlation and repeatability coefficients (LAD: ICC 0.5, RC 35%, Cx: ICC 0.54, RC 41%). The RCA territory did not show significant correlation between visits, ICC = 0.23.
Interobserver and Intraobserver repeatability
Ten sets of perfusion maps were assessed for intraobserver variability at a minimum gap of 4 weeks between analysis, and for interobserver variability. There was excellent agreement for all measurements (Table 4). The highest coefficients of variation were seen in the apical slice.
Table 4.
Intra and inter-observer MBF reproducibility
| Intra-observer | Inter-observer | |||
|---|---|---|---|---|
| CV (%) | ICC | CV (%) | ICC | |
| Rest | ||||
| Global | 0.7 | 0.999 | 0.8 | 0.999 |
| Basal | 1.1 | 0.998 | 1.2 | 0.998 |
| Mid | 1.0 | 0.999 | 0.6 | 0.999 |
| Apical | 3.0 | 0.990 | 3.7 | 0.980 |
| LAD | 1.1 | 0.997 | 1.3 | 0.996 |
| Cx | 1.4 | 0.997 | 1.3 | 0.995 |
| RCA | 1.8 | 0.996 | 1.8 | 0.991 |
| Stress | ||||
| Global | 2.0 | 0.995 | 2.4 | 0.995 |
| Basal | 2.0 | 0.996 | 3.0 | 0.993 |
| Mid | 2.6 | 0.999 | 3.3 | 0.994 |
| Apical | 6.3 | 0.963 | 8.0 | 0.959 |
| LAD | 2.8 | 0.99 | 2.6 | 0.99 |
| Cx | 2.5 | 0.992 | 4.3 | 0.986 |
| RCA | 1.9 | 0.992 | 1.9 | 0.993 |
CV coefficient of variation, ICC intraclass correlation coefficient
Discussion
The main findings of this study are 1) Gadgetron in-line myocardial perfusion mapping by CMR has good short and long-term repeatability, 2) regional assessment of coronary artery territory MBF has good repeatability, 3) MPR is a less reproducible method of assessment than MBF, particularly for regional assessment.
Global perfusion analysis
We have shown good repeatability of global stress and rest MBF for automated perfusion mapping with CMR, both within one scan and with an interval between scans. Our results are consistent with previous studies, using both invasive and non-invasive estimates of MBF and MPR.
Invasive assessment of coronary flow reserve has a coefficient of variation of 19% on repeat within minutes [13]. Table 5 contains a summary of the published literature on repeatability of non-invasive MBF measurement. PET repeatability in the published literature has ranged from RCs of 18–35% for resting MBF and 18–41% for stress MBF [14–17]. The largest study of test-retest repeatability in PET to date involved 120 volunteers who underwent serial stress or rest scans. Rest MBF CVs were 10.7% within test and 21.1% between tests, and stress MBF CVs were 9.6–10.6 and 19–21% [18]. As in most of the published literature, short-term repeatability had lower coefficients of variation and repeatability than delayed repeatability. In a recent study to assess the optimal kinetic model for repeatability in PET the best results gave a combined repeatability coefficient of 15.8% for stress and rest [19].
Table 5.
Summary of literature on MBF repeatability
| Rest | Stress | MPR | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Year | n | T test | r/ICC | RC (%) |
CV (%) |
T test | r/ICC | RC (%) |
CV (%) |
T test | r/ICC | RC (%) |
CV (%) |
|
| Immediate (intrastudy) | |||||||||||||||
| PET | Nitzsche [30] | 1996 | 15 | 0.33 | 0.99 | 33 | 0.16 | 0.97 | 13 | ||||||
| Kaufmann [14] | 1999 | 21 | ns | 18 | ns | 25 | ns | 33 | |||||||
| Wyss [23] | 2003 | 11 | ns | 0.77 | 21 | 0.77 | 27 | ns | 0.74 | 35 | |||||
| Schindler [31] | 2007 | 20 | 0.72 | 29 | 0.76 | 20 | |||||||||
| Manabe [15] | 2009 | 15 | 0.31 | 22 | 0.81 | 27 | 0.53 | 37 | |||||||
| Kitkungvan [18] | 2017 | 120 | 0.93 | 11 | 0.74 | 10 | |||||||||
| Ocneanu [19] | 2017 | 12 | 21 | 15 | |||||||||||
| CMR | Keitha [32] | 2017 | 10 | 53 | 13 | ||||||||||
| This study | 0.08 | 0.8 | 24 | 8 | 0.41 | 0.76 | 29 | 11 | |||||||
| Delayed (interstudy) | |||||||||||||||
| PET | Nagamachi [16] | 1996 | 30 | ns | 0.63 | 31 | ns | 0.69 | 18 | 20 | |||||
| Schindler [31] | 2007 | 20 | 0.75 | 30 | 0.71 | 23 | |||||||||
| Sdringola [17] | 2011 | 48 | p < 0.05 | 0.68 | 35 | ns | 0.53 | 34 | ns | 0.47 | 38 | ||||
| Johnson [24] | 2015 | 50 | 0.46 | 41 | 0.13 | 34 | 0.29 | 34 | |||||||
| Kitkungvan [33] | 2017 | 19 | 0.13 | 0.94 | 17 | 0.26 | 20 | ||||||||
| Kitkungvan [18] | 2017 | 120 | 0.13 | 21 | 0.81 | 19 | |||||||||
| CMR | Jerosch-Herold [20] | 2008 | 30 | 0.001 | 30 | 0.11 | 41 | ||||||||
| Larghata [8] | 2013 | 11 | 0.2 | 45 | 20 | 0.61 | 73 | 40 | 0.11 | 69 | 35 | ||||
| Likhite [21] | 2016 | 10 | 0.77 | 0.88 | |||||||||||
| Keitha [32] | 2017 | 10 | 61 | 16 | |||||||||||
| This study | 0.8 | 0.74 | 32 | 11 | 0.12 | 0.72 | 33 | 12 | 0.25 | 0.44 | 36 | 13 | |||
ns not significant (p value not reported), r Pearson correlation coefficient, RC reproducibility coefficient (% of mean), CV coefficient of variation
aRepeatability data is given for single mid-ventricular slice, all other studies, data is for global myocardium, averaged from multiple slices. Where RC was not published, but sufficient data was provided, this has been calculated using 1.96*SD of difference. Similarly, all RC are given as % for ease of comparison
There are few CMR studies of repeatability. The largest, a subset of the Multi-Ethnic Study of Atherosclerosis (MESA) study, included 30 patients with an interval of almost a year between scans [20], and reported repeatability coefficients of 30 and 41% for rest and stress MBF respectively, similar to values in PET studies. Another small sample of 10 patients showed good correlation for interstudy repeatability at rest (r = 0.77) and stress (r = 0.9) and CVs of 23% at rest and 20% for stress, in keeping with previous PET literature [21]. Other CMR studies have shown poorer repeatability than PET; a more recent, smaller study of 11 subjects [8] showed repeatability coefficients of 45 and 73%, with coefficients of variation of 20 and 40% for rest and stress respectively.
Our data for automated in line perfusion CMR mapping fit well within this published data and are comparable to the best results achieved with PET. Compared with most CMR studies, the repeatability in the current study was better for global MBF at both rest and stress, and for both short and long-term repeatability.
Regional assessment
All coronary territories showed good repeatability for rest and stress MBF. Higher repeatability coefficients and coefficients of variation were seen than for global values, consistent with the limited published literature in CMR and some of the PET literature. These findings likely reflect the smaller volume of myocardium assessed in regional assessment. Early CMR studies of repeatability have included only the mid slice but have shown regional repeatability to be higher than global (RC 28% vs 21%) [22]. The PET literature is inconsistent regarding regional vs global repeatability. One PET study examined coronary territory MBF repeatability in 30 patients and reported similar repeatability coefficients to global flow at stress (RC 18% for global perfusion, 18–24% for regional perfusion) and at rest (RC 31% for global and 26–46% for regional perfusion). A further study of 48 subjects showed comparable values for global perfusion vs regional perfusion (quadrants), with regional rest values of RC 33–41% and stress 33–38% vs global values 35 and 34% [17]. Other PET studies have shown worse repeatability in regional assessment compared to global values. A study of 21 subjects assessing repeatability of 15O PET had regional repeatability coefficients of 22–46% at rest and 41–59% at stress vs 18 and 25% globally [14]. A smaller study of 11 showed regional repeatability coefficients of 38–55% at rest and 55–70% at stress vs 21 and 27% globally [23]. Numerically the regional variability in our study was similar to or lower than in most PET studies. All coronary territories showed good correlation and repeatability with RCs of 32–36% at rest and 30–37% at stress.
In addition to coronary territories, we also compared variability between the three acquired slices. At stress the apical slice had the lowest ICC, showing moderate reliability (ICC = 0.48, p = 0.02). It also showed the highest inter- and intra-observer variability, with higher coefficients of variation than other regions. This underlines the difficulty in assessment and quantification of the most apical slice, due to the small area of myocardium available for analysis and the larger partial volume effect due to the conical shape of the apex, exacerbated at stress by increased cardiac motion.
MPR assessment
We found that the repeatability of CMR MPR was lower than that of MBF, in particular for the analysis of coronary territories. Previous studies have shown similar values for repeatability of global MPR to resting and stress MBF, with PET values of multiple studies within the range of 33–38%, in keeping with our results [14, 15, 17, 23, 24]. A study of 30 subjects showed a repeatability coefficient of 20% for MPR; however, these results included some studies repeated within the same day, which may account for the lower values. Data on inter-test reproducibility for MPR in CMR is limited, with a single study of 11 subjects showing a RC of 69%, higher than PET data and those from this study [8].
Where regional MPR has been compared to global values for repeatability, some studies have shown markedly worse repeatability. One study showed regional RC of 68–82% vs 33% for global values [14] another showed an increase from 35% for to 67–96% [23]. Others have shown a small rise or comparable RC in a similar pattern to our data. The largest study, with 48 paired studies showed a RC of 38% globally with a maximum of 43% in the lateral wall [17].
The lack of significant correlation in repeated results both for apical and mid slices and the RCA territories supports the use of stress MBF rather than MPR for clinical assessment where regional differences are diagnostically important. It is known that stress MBF correlates with the severity of stenosis in CAD [25], therefore the better reliability we have demonstrated for stress MBF compared with MPR would support its use for this important diagnostic decision.
Variation in resting MBF
We have shown variation in resting MBF on short-term repeat, within the same scan. A trend for rest MBF to decrease with serial measurement was not removed by correction for heart rate. Whilst the level of significance in this difference altered when MBF was corrected for HR, there remained a trend for decrease with sequential repeat (Fig. 3).
Published literature has not shown this decrease in MBF during the same scan. Two studies have shown a decrease in resting MBF on repeat assessment with a longer interval between imaging. In a study of healthy subjects with no risk factors, a significant decrease of 0.05 ± 0.13 ml/g/min (p < 0.05) was seen with a median interval of 22 days between scans [17]. This effect was not present in those with cardiovascular risk factors or in stress perfusion. The MESA study produced a similar finding with a decrease in resting MBF of 0.1 ml/g/min, p = 0.001 over a longer time interval (mean 334 days) [20]. This change was also accompanied by a significant change in heart rate, which was proposed to account for the drop.
Although some of these results differ from those in our study and the intervals between scans were different from in our study, they do provide more evidence of the susceptibility of rest MBF to change and physiological variation. Our study is the first to report more than 2 repeated measurements within one scanning session. The decrease seen within our study may be caused by an element of anxiety present at the beginning of the CMR scan in the subjects examined. In addition to a rise in heart rate and blood pressure, stress is associated with vasodilation of the coronary microvasculature in healthy volunteers [26]. Following correction for heart rate, the decrease in MBF remained, suggesting that vasodilation rather than cardiac work is the cause of the higher values on the first scans. This assumption is supported by the lack of difference between sequential stress perfusion, where maximal vasodilatation is induced so that differences in anxiety have no additional impact. The absence of significant difference in sequential stress scans also supports that this change is likely to be physiological rather than an effect of residual Gd from the previous series. The lack of significant difference between the second perfusion acquisition and subsequent assessment is reassuring clinically, as this would imply that stress followed by rest perfusion assessment, the most commonly used protocol, would produce repeatable values for both rest and stress.
In-line perfusion mapping
The development of Gadgetron automated inline perfusion mapping overcomes one of the main previous limitations of quantitative perfusion CMR by removing the previously time-consuming analysis and the need for specialist knowledge. We have shown that this technique provides measurements of MBF with a repeatability that is comparable to the reference method PET and that is at least as good as previous, manual, CMR analysis methods. A recent study has shown that CMR perfusion mapping yields similar MBF values at rest and vasodilator stress as ammonia PET in patients with stable CAD [10]. Assessment using perfusion maps allows objective assessment of MBF, providing simpler and faster analysis and may have clinical advantages of detecting disease with global decrease in MBF such as microvascular and multivessel disease.
Study limitations
Our data are influenced by physiological variation as well as variation within the model and analysis. While we aimed to minimise physiological variation as much as possible, some effects may not have been controlled for. Caffeine has been demonstrated to affect coronary vasomotor tone at rest [27] and adenosine stress perfusion CMR [28]. Although we advised our volunteers to avoid caffeine for 24 h prior to the scan, previous studies have demonstrated that up to 20% may still have detectable caffeine levels [29]. In addition, dosing of adenosine was determined clinically according to symptoms and response rather than a direct repeat from the previous scan. This would mimic clinical practice, and any difference in doses required may result in physiological variants in response. We can be confident that adequate stress was achieved; having seen appropriate increases in HR and RPP together with symptomatic response, however, the degree of hyperaemia may vary from maximal and account for the increased variation seen in stress MBF. All studies were performed using a FLASH perfusion sequence at 3 T, results for MBF may vary using other sequences or field strengths.
Conclusion
Quantitative perfusion CMR using automated perfusion mapping achieves estimates of MBF and MPR with repeatability similar to the reference standard method PET. In this study rest and stress MBF, rather than MPR were a more reproducible assessment, particularly in regional analysis. The degree of physiological variation emphasises the importance in establishing normal ranges to allow for accurate diagnostic use.
Additional files
Figure S1. Correlation by slice (A) rest (B) stress. Trend line represents line of perfect fit. (DOCX 119 kb)
Figure S2. Correlation by coronary territory (A) rest (B) stress. Trend line represents line of perfect fit. (DOCX 116 kb)
Acknowledgements
We thank David Shelley, Gavin Bainbridge, Petra Bijsterveld, Fiona Richards and Hannah Newman for their help in recruiting and scanning patients and the organisation of running this study.
Funding
This work was supported by British Heart Foundation grants CH/16/2/32089 and RG/16/1/32092 to Sven Plein.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHA
American Heart Association
- AIF
arterial input function
- ANOVA
analysis of variance
- BP
blood pressure
- BTEX
blood tissue exchange
- CAD
coronary artery disease
- CFR
coronary flow reserve
- CMR
cardiovascular magnetic resonance
- CV
coefficient of variation
- Cx
circumflex
- ECG
Electrocardiogram
- FFR
fractional flow reserve
- Gd
gadolinium
- HR
heart rate
- ICC
intraclass correlation coefficient
- IQR
interquartile range
- LAD
left anterior descending
- MBF
myocardial blood flow
- MOCO
motion corrected
- MPR
myocardial perfusion reserve
- PD
Proton density
- PET
Positron emission tomography
- RC
repeatability coefficient
- RCA
right coronary artery
- RPP
rate pressure product
- SD
standard deviation
- TE
Echo time
- TR
Repetition time
- TS
Saturation recovery time
Authors’ contributions
LB: Conception and design, recruitment, supervision of scans, analysis and interpretation of data, drafting of manuscript. SO: Supervision of scans, analysis and interpretation of data, critical & intellectual revision of manuscript. DB: analysis and interpretation of data, critical & intellectual revision of manuscript. KJ: Recruitment, supervision of scans, critical & intellectual revision of manuscript. GF: Critical & intellectual revision of manuscript. JF: Critical & intellectual revision of manuscript. PG: Critical & intellectual revision of manuscript. PC: Critical & intellectual revision of manuscript. KK: Critical & intellectual revision of manuscript. ED: Critical & intellectual revision of manuscript. PS: Critical & intellectual revision of manuscript. HX: Conception and design, processing and interpretation of CMR data, critical & intellectual revision of manuscript. JG: Critical & intellectual revision of manuscript. JM: Critical & intellectual revision of manuscript. PK: Conception and design, processing and interpretation of CMR data, critical & intellectual revision of manuscript. SP: Conception and design, interpretation of data and drafting of manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki (October 2000), with all volunteers providing informed written consent. Ethical approval was given by NRES Committee Yorkshire and the Humber – Leeds West, Ref 12/YH/0551.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12968-018-0462-y) contains supplementary material, which is available to authorized users.
Dr. Eike Nagel served as a Guest Editor for this manuscript.
Contributor Information
Louise A. E. Brown, Email: l.brown1@leeds.ac.uk
Sebastian C. Onciul, Email: s.c.onciul@leeds.ac.uk
David A. Broadbent, Email: d.broadbent@nhs.net
Kerryanne Johnson, Email: kerryannejohnson@nmdhb.govt.nz.
Graham J. Fent, Email: g.j.fent@leeds.ac.uk
James R. J. Foley, Email: j.foley@leeds.ac.uk
Pankaj Garg, Email: p.garg@leeds.ac.uk.
Pei G. Chew, Email: p.g.chew@leeds.ac.uk
Kristopher Knott, Email: kristopher.knott@nhs.net.
Erica Dall’Armellina, Email: e.dallarmellina@leeds.ac.uk.
Peter P. Swoboda, Email: p.swoboda@leeds.ac.uk
Hui Xue, Email: hui.xue@nih.gov.
John P. Greenwood, Email: j.greenwood@leeds.ac.uk
James C. Moon, Email: james.moon@bartshealth.nhs.uk
Peter Kellman, Email: kellmanp@nhlbi.nih.gov.
Sven Plein, Phone: +44 113 3437720, Email: s.plein@leeds.ac.uk.
References
- 1.Tonino PAL, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, et al. Angiographic versus functional severity of coronary artery Stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–2821. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- 2.Fischer JJ, Samady H, McPherson JA, Sarembock IJ, Powers ER, Gimple LW, et al. Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity. Am J Cardiol. 2002;90:210–215. doi: 10.1016/S0002-9149(02)02456-6. [DOI] [PubMed] [Google Scholar]
- 3.Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120:1505–1512. doi: 10.1161/CIRCULATIONAHA.109.850073. [DOI] [PubMed] [Google Scholar]
- 4.Lockie T, Ishida M, Perera D, Chiribiri A, De Silva K, Kozerke S, et al. High-resolution magnetic resonance myocardial perfusion imaging at 3.0-tesla to detect hemodynamically significant coronary stenoses as determined by fractional flow reserve. J Am Coll Cardiol. 2010;57:70–75. doi: 10.1016/j.jacc.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Christian TF, Rettmann DW, Aletras AH, Liao SL, Taylor JL, Balaban RS, et al. Absolute myocardial perfusion in canines measured by using dual-bolus first-pass MR imaging. Radiology. 2004;232:677–684. doi: 10.1148/radiol.2323030573. [DOI] [PubMed] [Google Scholar]
- 6.Wilke N, Jerosch-Herold M, Wang Y, Huang Y, Christensen BV, Stillman AE, et al. Myocardial perfusion reserve: assessment with multisection, quantitative, first-pass MR imaging. Radiology. 1997;204:373–384. doi: 10.1148/radiology.204.2.9240523. [DOI] [PubMed] [Google Scholar]
- 7.Jerosch-Herold M, Swingen C, Seethamraju RT. Myocardial blood flow quantification with MRI by model-independent deconvolution. Med Phys. 2002;29:886–897. doi: 10.1118/1.1473135. [DOI] [PubMed] [Google Scholar]
- 8.Larghat AM, Maredia N, Biglands J, Greenwood JP, Ball SG, Jerosch-Herold M, et al. Reproducibility of first-pass cardiovascular magnetic resonance myocardial perfusion. J Magn Reson Imaging. 2013;37:865–874. doi: 10.1002/jmri.23889. [DOI] [PubMed] [Google Scholar]
- 9.Kellman P, Hansen MS, Nielles-Vallespin S, Nickander J, Themudo R, Ugander M, et al. Myocardial perfusion cardiovascular magnetic resonance: optimized dual sequence and reconstruction for quantification. J Cardiovasc Magn Reson. 2017;19:43. doi: 10.1186/s12968-017-0355-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engblom H, Xue H, Akil S, Carlsson M, Hindorf C, Oddstig J, et al. Fully quantitative cardiovascular magnetic resonance myocardial perfusion ready for clinical use: a comparison between cardiovascular magnetic resonance imaging and positron emission tomography. J Cardiovasc Magn Reson. 2017;19:78. doi: 10.1186/s12968-017-0388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the cardiac imaging Committee of the Council on clinical cardiology of the American Heart Association. Circulation. 2002;105:539–542. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 12.Coefficient of variation from duplicate measurements. https://www.medcalc.org/manual/cvfromduplicates.php. Accessed 14 Mar 2018.
- 13.Ng MKC, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006;113:2054–2061. doi: 10.1161/CIRCULATIONAHA.105.603522. [DOI] [PubMed] [Google Scholar]
- 14.Kaufmann PA, Gnecchi-Ruscone T, Yap JT, Rimoldi O, Camici PG. Assessment of the reproducibility of baseline and hyperemic myocardial blood flow measurements with 15O-labeled water and PET. J Nucl Med. 1999;40:1848–1856. [PubMed] [Google Scholar]
- 15.Manabe O, Yoshinaga K, Katoh C, Naya M, Dekemp RA, Tamaki N. Repeatability of rest and hyperemic myocardial blood flow measurements with 82 Rb dynamic PET. J Nucl Med. 2009;50:68–71. doi: 10.2967/jnumed.108.055673. [DOI] [PubMed] [Google Scholar]
- 16.Nagamachi S, Czernin J, Kim A, Sun K, Bottcher M, Phelps ME, et al. Reproducibility of measurements of regional resting and hyperemic myocardial blood flow assessed with PET. J Nucl Med. 1996;37:1626–1631. [PubMed] [Google Scholar]
- 17.Sdringola S, Johnson NP, Kirkeeide RL, Cid E, Gould KL. Impact of unexpected factors on quantitative myocardial perfusion and coronary flow reserve in young, asymptomatic volunteers. JACC Cardiovasc Imaging. 2011;4:402–412. doi: 10.1016/j.jcmg.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 18.Kitkungvan D, Johnson NP, Roby AE, Patel MB, Kirkeeide R, Gould KL. Routine clinical quantitative rest stress myocardial perfusion for managing coronary artery disease: Clinical Relevance of Test-Retest Variability. JACC Cardiovasc Imaging. 2017; [DOI] [PubMed]
- 19.Ocneanu AF, DeKemp RA, Renaud JM, Adler A, Beanlands RSB, Klein R. Optimally repeatable kinetic model variant for myocardial blood flow measurements with 82Rb PET. Comput Math Methods Med. 2017; [DOI] [PMC free article] [PubMed]
- 20.Jerosch-Herold M, Vazquez G, Wang L, Jacobs DRJ, Folsom AR. Variability of myocardial blood flow measurements by magnetic resonance imaging in the multi-ethnic study of atherosclerosis. Investig Radiol. 2008;43:155–161. doi: 10.1097/RLI.0b013e31815abebd. [DOI] [PubMed] [Google Scholar]
- 21.Likhite D, Suksaranjit P, Adluru G, Hu N, Weng C, Kholmovski E, et al. Interstudy repeatability of self-gated quantitative myocardial perfusion MRI. J Magn Reson Imaging. 2016;43:1369–1378. doi: 10.1002/jmri.25107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elkington AG, Gatehouse PD, Ablitt NA, Yang G-Z, Firmin DN, Pennell DJ. Interstudy reproducibility of quantitative perfusion cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2005;7:815–822. doi: 10.1080/10976640500287877. [DOI] [PubMed] [Google Scholar]
- 23.Wyss CA, Koepfli P, Mikolajczyk K, Burger C, Von Schulthess GK, Kaufmann PA. Bicycle exercise stress in PET for assessment of coronary flow reserve: repeatability and comparison with adenosine stress. J Nucl Med. 2003;44:146–154. [PubMed] [Google Scholar]
- 24.Johnson NP, Gould KL. Regadenoson versus dipyridamole hyperemia for cardiac PET imaging. JACC Cardiovasc Imaging. 2015;8:438–447. doi: 10.1016/j.jcmg.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 25.Uren NG, Melin JA, de Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary artery stenosis. N Engl J Med. 1994;330:1782–1788. doi: 10.1056/NEJM199406233302503. [DOI] [PubMed] [Google Scholar]
- 26.Dakak N, Quyyumi AA, Eisenhofer G, Goldstein DS, Iii RC. Sympathetically mediated effects of mental stress on the cardiac microcirculation of patients with Coranary artery disease. Am J Cardiol. 1995;76:125–130. doi: 10.1016/S0002-9149(99)80043-5. [DOI] [PubMed] [Google Scholar]
- 27.Bottcher M, Czernin J, Sun K, Phelps ME, Schelbert HR. Effect of caffeine on myocardial blood flow at rest and during pharmacological vasodilation. J Nucl Med. 1995;36:2016–2021. [PubMed] [Google Scholar]
- 28.Oudkerk M, Kuijpers D, Prakken NH, Vliegenthart R, van Dijkman M, Pvdijkman PR, van der Harst pvanderharst bronovonl P, et al. Caffeine intake inverts the effect of adenosine on myocardial perfusion during stress as measured by T1 mapping. Int J Cardiovasc Imaging. 2016;32:1545–1553. doi: 10.1007/s10554-016-0949-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banko LT, Haq SA, Rainaldi DA, Klem I, Siegler J, Fogel J, et al. Incidence of caffeine in serum of patients undergoing dipyridamole myocardial perfusion stress test by an intensive versus routine caffeine history screening. AJC. 2010;105:1474–1479. doi: 10.1016/j.amjcard.2009.12.072. [DOI] [PubMed] [Google Scholar]
- 30.Nitzsche EU, Choi Y, Czernin J, Hoh CK, Huang S, Schelbert HR. Noninvasive Quantification of Myocardial Blood Flow in Humans A Direct Comparison of the [ N]Ammonia and the [ O]Water Techniques. Circ Cardiovasc Imaging. 1996;93:2000–6. doi: 10.1161/01.cir.93.11.2000. [DOI] [PubMed] [Google Scholar]
- 31.Schindler TH, Zhang XL, Prior JO, Cadenas J, Dahlbom M, Sayre J, et al. Assessment of intra- and interobserver reproducibility of rest and cold pressor test-stimulated myocardial blood flow with 13N-ammonia and PET. Eur J Nucl Med Mol Imaging. 2007;34:1178–88. doi: 10.1007/s00259-007-0378-5. [DOI] [PubMed] [Google Scholar]
- 32.Keith GA, Rodgers CT, Chappell MA, Robson MD. A Look-Locker Acquisition Scheme for Quantitative Myocardial Perfusion Imaging with FAIR Arterial Spin Labeling in Humans at 3 Tesla. Magn Reson Med. 2017;78:541–9. doi: 10.1002/mrm.26388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kitkungvan D, Lai D, Zhu H, Roby AE, Patel MB, Kirkeeide R, et al. Optimal Adenosine Stress for Maximum Stress Perfusion, Coronary Flow Reserve, and Pixel Distribution of Coronary Flow Capacity by Kolmogorov-Smirnov Analysis. Circ Cardiovasc Imaging. 2017 doi: 10.1161/CIRCIMAGING.116.005650. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Correlation by slice (A) rest (B) stress. Trend line represents line of perfect fit. (DOCX 119 kb)
Figure S2. Correlation by coronary territory (A) rest (B) stress. Trend line represents line of perfect fit. (DOCX 116 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.