Abstract
Langerhans cell histiocytosis (LCH) is characterized by idiopathic monoclonal infiltration of Langerhans cells in different organs such as the skeleton, skin, pituitary gland, liver, spleen, lungs, and the hematopoietic system. Skin lesions are common in LCH and affect about 40% of cases. It is reported that skin lesions are usually the first manifestation of LCH in 80% of patients. Usually, cutaneous presentations of LCH in adults are generalized or seborrhea-like lesions and it is often the first manifestation of disease. Here, we describe a 45-year old female who was known case of hypothyroidism, systemic lupus erythematosus, and diabetes insipidus. In our patient, cutaneous involvement was unusual. It was single and presented in unusual site (ankle) and before developing such lesion, she had diabetes insipidus for several years due to the involvement of pituitary gland.
Keywords: Diabetes insipidus, Langerhans cell histiocytosis, skin
Introduction
Langerhans cell histiocytosis (LCH) is a common name for a group of rare diseases, characterized by idiopathic monoclonal infiltration of Langerhans cells in different organs.[1,2,3,4,5] Whether LCH is a neoplasm or an inflammatory condition still remains controversial.[1,2,4] These cells may infiltrate at any organ such as the skin, bones, lungs, and brain.[1,2,5,6,7,8]
The most common organs to involve are skeleton (80%), skin (33%), and the pituitary gland (25%). The less frequently involved organs are the liver, spleen, lungs, the hematopoietic system, lymph nodes, and central nervous system (except from the pituitary gland).[1,2,5,6,7,8]
LCH is mainly seen in children between 1 and 4 years but it can occur at any age.[1,3,5] LCH is very rare in adults and the estimated incidence of LCH is about 1–2 cases per million in adults which is lower than children.[1,2,3,5,9]
Diagnosis of LCH is difficult due to its rare occurrence and wide range of clinical manifestations.[1] The diagnosis of LCH is based on the histologic and immunophenotypic examination of tissue lesions. Morphologic identification of LCH cells and positive staining of lesional cells with CD1 and S100 are necessary for definitive diagnosis of LCH.[1,2,10]
Prognosis of LCH depends on the age of onset, the number of involved organs, organ dysfunction, and severity of disease.[1,2,5,11]
Skin lesions are common in LCH and affect about 40% of cases.[1,2,3] It is reported that skin lesions are usually the first manifestation of LCH in 80% of patients.[1,3]
Cutaneous lesions in LCH are commonly brown to red papules with scaly, erythematous, seborrhea-like eruptions which mostly involve the face, scalp, and trunk. Nodules may develop in mucous membranes and sometimes become crusted and ulcerated.[1,2,3]
Here, we describe an adult-onset LCH with rare, atypic, and very unusual cutaneous involvement.
Case Report
A 45-year-old female presented to dermatological consultation with a large ulcerative plaque in posterior side of left ankle for 2 months. She was a known case of hypothyroidism from 10 years ago, a known case of systemic lupus erythematosus (SLE) from 5 years ago and a known case of diabetes insipidus from 3 years ago. The patient was on levothyroxine (0.1 mg daily), prednisolone (5 mg daily), hydroxychloroquine (200 mg daily), and DDAVP (desmopressin acetate) Nasal Spray 1 puff q12 h.
Dermatologic examination revealed a single, well-defined ulcerative erythematous plaque in the posterior side of left ankle. On palpation, it was indurated without tenderness and discharge [Figure 1]. No lymphadenopathy or organomegaly was detected around the lesion. The patient did not complain of any pain or pruritus as well.
Figure 1.

Clinical appearance of lesion
As the patient was on prednisolone for the treatment of SLE for several years, she was initially diagnosed as having an infectious lesion and treated with antibiotics for 2 weeks without any improvement. At this stage, the patient was referred to our dermatology clinic for further evaluation. Smear and culture from ulcerative part of the lesion were done but the results were negative. After that, skin biopsy of the infiltrated margin of the lesion was performed.
Sections showed focally, invasion of the epidermis by small aggregation of large ovoid cells with abundant eosinophilic cytoplasm. The nucleus was reniform and some was coffee-bean shape. Hence, the diagnosis of LCH was made based on morphologic findings in microscopic examination [Figures 2-4] and confirmed by immunohistochemical staining which revealed the aggregation of S100 and CD1apositive tumoral cells [Figures 5 and 6].
Figure 2.
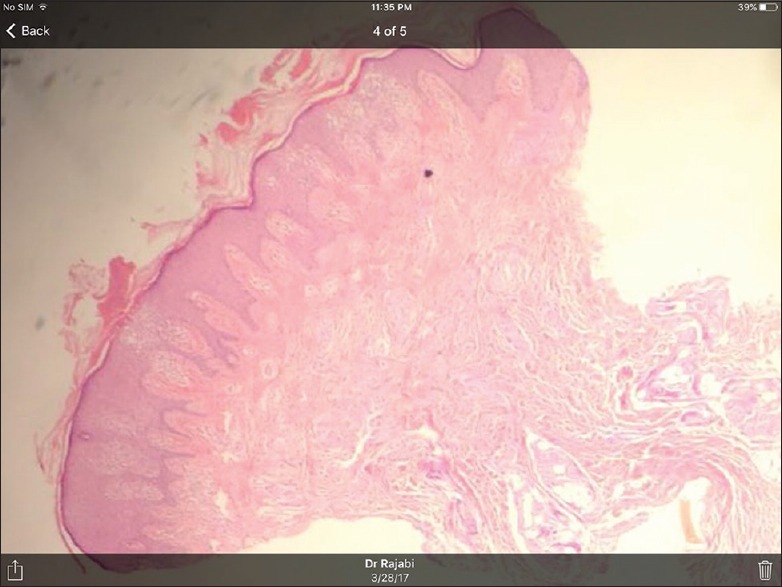
H and E, ×4
Figure 4.
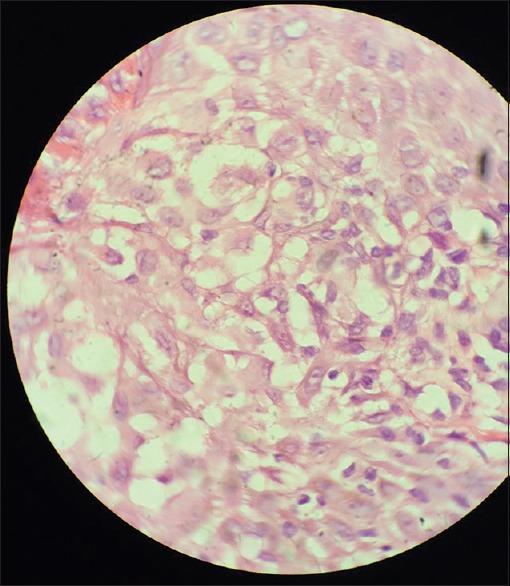
H and E, invasion of the epidermis by small aggregation of large ovoid cells with abundant eosinophilic cytoplasm and reniform nucleus
Figure 5.
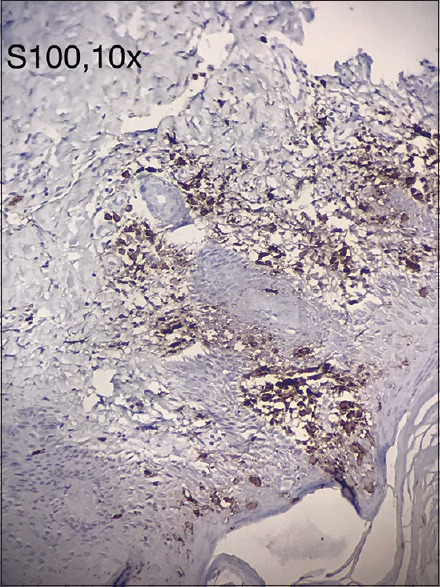
Immunohistochemical staining with S100 marker
Figure 6.
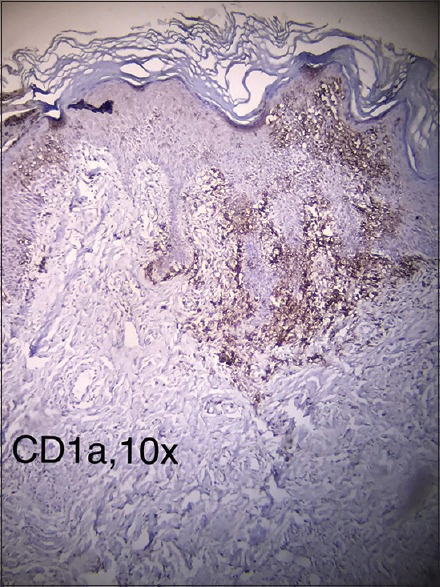
Immunohistochemical staining with CD1a marker
Figure 3.
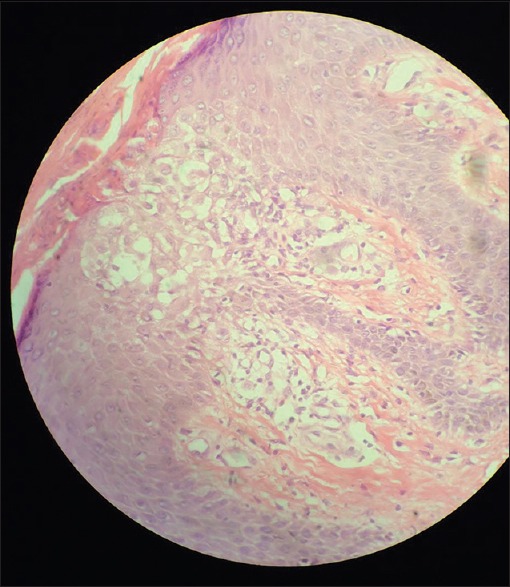
H and E, another picture
Hematologic examinations, liver, and renal function tests were within the normal range. Lipid profile showed mild hypercholestrolemia and mild hypertriglyceridemia.
Serologic examinations revealed positive antinuclear antibody test and positive anti-double stranded DNA test.
Right ankle radiography reported osteoporosis secondary to prolonged use of corticosteroids, fatty degeneration of bone marrow and slight osteochondral injury in tibiotalar joint, without any lytic bony lesions.
Since LCH is a multisystem disease, complete staging and more evaluations such as skull series, chest radiography, abdominal computed tomography, and magnetic resonance imaging of the brain are necessary to decide on the initiation of effective systemic treatments, so the patient was referred to the oncologist for further work up but she did not come back for follow-up to our clinic.
Discussion
LCH is a considerably rare disease, especially in adults.[1,2,3,5,12] The incidence of LCH is about 1–2 cases per million in this age group.[1,12]
Cutaneous lesions in LCH are commonly located on the scalp, face, trunk, flexural and intertriginous areas, glabrous skin, and external genitalia. In adults, the cutaneous manifestations of LCH include an erosive intertriginous eruption, xanthomatous eruption, or acneiform eruption. Skin lesions may manifest as papules, pustules, vesicle, petechiae, or purpura. In LCH, nodular lesions are commonly presented in the mucus membranes.[1,2,3,12]
Skin lesions in LCH may resemble seborrhic dermatitis, especially behind the ears, in the axillary and inguinal folds. Oral manifestations include gingival bleeding and necrotic and ulcerative lesions over the gums.[3]
Atypical cutaneous presentations of LCH have been reported as isolated tonsillar involvement, paronychia, and purely cutaneous forms of LCH in elderly patients.[12]
About 70% of adults with LCH have multisystem involvement.[5] Diabetes insipidus is the most common endocrine manifestation in LCH, and especially in adults, it is more frequent than children.[3,5] In women with genital ulcer and diabetes insipidus, LCH is among the differential diagnosis.[13]
As we mentioned in case presentation part, our patient had multisystem LCH with the pituitary gland and cutaneous involvement. Cutaneous lesion in our case presented as a large infiltrated ulcerative plaque on left ankle.
Presentation of cutaneous lesion on ankle in LCH is very rare and unusual. To the best of our knowledge, just one previous case study reported skin involvement in ankle area in an 81-year old man with generalized cutaneous LCH.[12]
This patient was much older than our patient and had generalized cutaneous LCH with multiple skin lesions in different areas besides ankles. Our case had only one plaque on left ankle which was large and ulcerated but in mentioned case study, the patient had multiple erythematous macules and plaques on his ankle.
No international guidelines for the treatment of LCH in adults is available.[1] The clinical stratification according to the extent of LCH is a very important factor in treatment.[3,14]
Local or systemic corticosteroids, thalidomide, azathioprine, methotrexate, PUVA, and narrow-band ultraviolet B are therapeutic options for mild cutaneous LCH, but severe forms need chemotherapy.[1,3,5]
Our patient, a known case of hypothyroidism, SLE, and diabetes insipidus, was on levothyroxine, prednisolone, hydroxychloroquine, and DDAVP (desmopressin acetate) before developing cutaneous lesion on the ankle with diagnosis of LCH. As LCH is a multisystem disease and required complete evaluations of other organs, we decided to refer the patient to the oncologist for further work up, but she did not come back for follow-up to our clinic.
We reported this case because of very unusual cutaneous presentation of LCH. Usually, cutaneous presentations of LCH in adults are generalized or seborrhea-like lesions but in this patient, it was single and presented in a very unusual site (ankle) and before developing such lesion, she had diabetes insipidus for several years due to the involvement of pituitary gland.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blazewicz I, Biernat W, Kowalczyk A, Baranska-Rybak W, Nowicki R, Stawczyk-Macieja M, et al. Adult onset of multisystem Langerhans cell histiocytosis with skin and lymph node involvement. Postepy Dermatol Alergol. 2015;32:225–8. doi: 10.5114/pdia.2014.40970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jeunon T, Sousa MA, Santos-Rodrigues N, Lopes R. Langerhans cell histiocytosis - A case report. Dermatol Pract Concept. 2012;2:25–9. doi: 10.5826/dpc.0201a04.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy IS, Gowrishankar S, Somani VK, Murthy DB. Adult onset Langerhans cell histiocytosis: Report of two patients. Indian J Dermatol Venereol Leprol. 2014;80:560–2. doi: 10.4103/0378-6323.144206. [DOI] [PubMed] [Google Scholar]
- 4.Abla O, Egeler RM, Weitzman S. Langerhans cell histiocytosis: Current concepts and treatments. Cancer Treat Rev. 2010;36:354–9. doi: 10.1016/j.ctrv.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Lai JY, Tang MM, Priya G, Rajasuriar JS, Suganthi T. Langerhans Cell Histiocytosis in an Adult - a rare, life-threatening and not to be missed. Med J Malaysia. 2014;69:95–7. [PubMed] [Google Scholar]
- 6.Chai D, Tao Y, Bao Z, Yang L, Feng Z, Ma L, et al. The adverse prognostic hallmarks in identical twins with Langerhans cell histiocytosis: A clinical report and literature review. Tohoku J Exp Med. 2013;230:219–25. doi: 10.1620/tjem.230.219. [DOI] [PubMed] [Google Scholar]
- 7.Erdem H, Kadioglu N, Uzunlar AK, Yücel I, Oktay M, Besir FH. Langerhans cell histiocytosis mimicking osteomyelitis in an infant. APSP J Case Rep. 2013;4:27. [PMC free article] [PubMed] [Google Scholar]
- 8.Azreen AB, Kwan CY, Prepagaren N. Langerhans cell histiocytosis of maxillary sinus. Med J Malaysia. 2012;67:627–8. [PubMed] [Google Scholar]
- 9.Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol. 2006;76:363–8. doi: 10.1111/j.1600-0609.2006.00648.x. [DOI] [PubMed] [Google Scholar]
- 10.Histiocyte Society 2009. Langerhans Cell Histiocytosis Evaluation and Treatment Guidelines. Histocyte Society Online. 2009. [Last accessed on 2009 Apr]. Available from: http://www.histiocytesociety.org/site/c.mqISL2PIJrH/b.4442715/k.A339/Treatment_Plans.htm .
- 11.Gadner H, Grois N, Arico M, Broadbent V, Ceci A, Jakobson A, et al. A randomized trial of treatment for multisystem Langerhans' cell histiocytosis. J Pediatr. 2001;138:728–34. doi: 10.1067/mpd.2001.111331. [DOI] [PubMed] [Google Scholar]
- 12.Sun WG, Zhong LS, Chen H. A case of adult generalized cutaneous langerhans cell histiocytosis. Ann Dermatol. 2016;28:262–4. doi: 10.5021/ad.2016.28.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu YH, Fan XH, Fang K. Langerhans' cell histiocytosis with multisystem involvement in an adult. Clin Exp Dermatol. 2007;32:765–8. doi: 10.1111/j.1365-2230.2007.02467.x. [DOI] [PubMed] [Google Scholar]
- 14.Wong LS. An unusual case of neonatal langehrans cell histiocytosis presenting with diffuse hemorrhagic nodules and a cutaneous abdominal mass. Indian J Dermatol. 2015;60:424. doi: 10.4103/0019-5154.160545. [DOI] [PMC free article] [PubMed] [Google Scholar]


