Abstract
Background:
A secure airway and effective ventilation are key components of advanced life support, and misplacement of endotracheal tube (ETT) can lead to morbidity in multiple trauma patients. The purpose of this study was to investigate the accuracy of ultrasound in diagnosis of direction for tracheal intubation.
Materials and Methods:
This descriptive-analytical study was conducted on 100 traumatic patients requiring intubation in 2016 in the Emergency Department of Al-Zahra and Kashani Medical Education Centers in Isfahan. Surface probe was placed transversally in the front of the neck at the top of the suprasternal notch, and the position of trachea was specified by front of comet-tail artifact which is the contour between hyperechoic air–mucosa (A–M) and a posterior reverberation artifact. Intubation accuracy by capnography was investigated, and the results were recorded in each patient's profile. Tracheal sonography was done during placement, or as soon as, the ETT has been embedded. The scanning time was minimized and it was carried out in total time of 10 s.
Results:
The diagnosis of intubation accuracy indicated that it was successful in 94 individuals (94%) and unsuccessful in 6 ones (6%). Intubation accuracy in 93 people (93%) was confirmed, and inaccuracy of intubation in 7 people (7%) was diagnosed. Ultrasound sensitivity in diagnosis of intubation accuracy was 97.9% (92.94) with 83.3% (5.6%) specificity. The positive and negative predictive values were 98.9% (92.93) and 71.4% (5.7%) respectively.
Conclusion:
Ultrasound method has high sensitivity and specificity to determine the correct placement of the tracheal tube, and it can be implemented as a reliable method given the acceptable positive and negative predictive values.
Keywords: Accuracy, capnography, intubation, multiple trauma, ultrasonography
Introduction
Tracheal intubation in respiratory management of critically ill patients who suffer from airway impairment or ventilation for any reason plays an important role in the treatment process.[1] Unfortunately, in some cases, doing such activity is difficult even if it is done by skilled and experienced individuals. The most dangerous and serious complication of endotracheal intubation is esophageal intubation in an unknown way which results in hypoxia in the brain.[2]
Abundant primary methods for proper endotracheal tube (ETT) intubation can be used, including observation of vocal cords, observation of the chest symmetrical movement, monitoring of the abdominal distention of respiratory sounds, and epigastric auscultation each of which has its own limitations.[3,4,5] However, a variety of secondary methods such as capnometry, capnography, esophageal detector device, and chest radiography are used for ETT intubation routinely. Capnometry and capnography are known as the most effective secondary methods, but they can be associated with false-positive or false-negative responses.[6]
None of the secondary methods are reliable, and pulmonary ventilation is needed.[7] The risk of pulmonary aspiration in these patients increases due to stomach ventilation to confirm the insertion of the tracheal tube if the tube is placed randomly in the esophagus. Therefore, passing tracheal tube into the esophagus is catastrophic. This case usually happens in an emergency. The occurrence of these events in an emergency has been reported in 6%–16% of cases.[6] Therefore, efforts which are performed to intubate in the emergency department should focus on preventing tube from going into the esophagus. Unfortunately, capnography is not always available, especially in small centers. Therefore, an auxiliary method is required to confirm the intubation of tracheal tube. The ideal method should be fast, simple, and noninvasive and normally available.
Ultrasonography has this characteristic as it easily recognizes neurovascular structures and not affected by very little pulmonary flow. Unlike the capnography, esophageal intubation by ultrasound can be used in earlier detection and prevent from stomach ventilation and other complications.[8]
However, if the accuracy and reliability of ultrasound in performing the tracheal intubation is proven, it can be used in emergency section or special care units that difficult intubation is observed so much. A study conducted in California, USA, for proving tracheal intubation in which sonography images were taken from the location of cricothyroid cartilage. The purpose of research was to investigate the sensitivity and specificity of the method. The research was a prospective and coincidental study, and it was shown that dynamic methods were better than static methods to evaluate the location of the tube of intubation, but this study was done on the corpses.[9]
There are different ways to find ETT location by ultrasound. These methods are divided into two types: direct and indirect. Direct method is referred to direct observation of trachea which was used in this study. The true method that was previously mentioned is different from trans-cricothyroid membrane ultrasound because it uses a convex transducer on suprasternal notch. As it is obvious from the name, convex probes of ultrasound have lower frequency that they cause the tissues to be visible on the hard skin. Calcifications within the thyroid gland lead to false-negative reports for the tracheal tube.[9,10]
An ultrasound evaluation can also be done in dynamic and also static modes. Static method was used in the present study for sonography of the upper airways. Although dynamic techniques may be more accurate, they disrupt the process of intubation.[11] Proving ultrasonic intubation is shown and taken into account by indirect methods in two other windows well.
One of the windows is intercostal and another one is subxiphoid window for observing diaphragm movements[12] which acts based on movements of the diaphragm and pleura.[13] However, these methods operate based on positive ventilation pressure, and in cases of pathology such as pneumothorax and pneumonia, they can disrupt it. In addition, several studies have shown that ultrasonography can specify tracheal and esophagus intubation in models of corpse autopsies.[3,4,5,11,12,13] Two recent studies have shown that the use of ultrasonography in support of ETT placement on the tracheal tube has sensitivity and specificity close to 100% in human living samples under controlled conditions.[14,16]
As far as we know, few studies have been done in assessing the accuracy of ultrasound in emergency situations on real patients instead of controlled conditions or its results on dead person. Therefore, their outcomes can be generalized to intubation in emergency situations to fewer extents. Although ultrasound is dependent to the experience of the person performing this activity, studies have shown that it can be done after the correct training of inexperienced physicians.[9]
Due to increasing number of traumatic patients who require intubation in emergency section and the need of a quick cheap, affordable, and reliable method to verify intubation, the present study was done with the aim of determining the value of intubation diagnosis in traumatic patients referred to the Emergency Department of Al-Zahra and Kashani Hospitals of Isfahan who needed intubation.
Materials and Methods
The research is a descriptive-analytic study to evaluate diagnostic tests which was conducted in 2014 in the Emergency Department of Al-Zahra and Kashani Medical Education Centers in Isfahan. The surveyed community included traumatic patients requiring intubation who were referred to mentioned center.
The required sample size for this study was determined 101 patients using the estimating sample size formula for outbreak studies considering the confidence level of 95% (Z1-α/2 = 1.96) and test power of 80%.
The sensitivity of ultrasound to correct intubation was considered as 0.5% due to lack of similar study (P = 0.5) and accepting error rate of 0.1 (d = 0.16). Finally, for more certainty, 100 patients were studied. Sampling method in this study was in an easy and accessible way, and patients who had criteria for entering the study were selected in order of admission to the hospital during 2014.
Inclusion criteria were the patients with multiple traumas requiring endotracheal intubation in emergency department as well as lack of damage to trachea area and the surrounding region.
In case of failed airway, laryngeal fracture, anterior neck injury which prevents endotracheal intubation, lack of possibility of checking the intubation with ultrasound for various reasons (abnormal anatomy, tumor, goiter, and tracheotomy), thyromental distance <6 cm, spinal cord disease and coagulation disorders of patients, and patients with cardiac arrest were excluded from the study. All patients with multiple traumas who require intubation for maintenance from patient ventilation were examined in emergency section. Thyromental distance has been considered as neck circumference. Anesthetic measures were completely standardized. Patient monitoring included heart monitoring, pulse oximetry, capnography, and noninvasive method of blood pressure measurement. The head and neck of the patient were in the supine state. Intubation was carried out with the slightest extension of the neck in sniffing mode with the Macintosh laryngoscope to see the epiglottis with appropriate size for each patient. Standard size of tracheal tube was selected for each patient and it was conducted by related attending.
Gold standard method for confirmation of endotracheal intubation is a combination of physical examination and capnography in auscultation and exhaling co2 (after at least 5 breaths  ) along with typical wavy co2 of mainstream capnography. Esophageal intubation is detected when there are no respiratory sounds and capnography is an abnormal waveform. Tracheal sonography is done during placement or as soon as the ETT has been embedded. The scanning time was minimized and it was carried out in total time of 10 s.
) along with typical wavy co2 of mainstream capnography. Esophageal intubation is detected when there are no respiratory sounds and capnography is an abnormal waveform. Tracheal sonography is done during placement or as soon as the ETT has been embedded. The scanning time was minimized and it was carried out in total time of 10 s.
Surface probe was placed transversally in the front of the neck at the top of the suprasternal notch, and the position of trachea was specified by the front of comet-tail artifact which is the contour between Hyper Ecoline of air-mucosa (A-M) and a posterior reverberation artifact. Position of ETT, when it is placed in trachea, is defined as observable contour between A-M and comet-tail artifact. If the second contour is appeared, it will be similar to the second airway which is called double-tract sign.
If position of the esophagus is suspected of being exactly behind the trachea, operator of ultrasound can specify the location of the esophagus by moving the probe to the left and right sides during scan.
To respect blindness, three persons including the ones who doing intubation, ultrasound, and capnography worked independently. Assessments were carried out, and the verbal communication was prevented by headphones. Moreover, ultrasound and capnography operators did not intervene in care measures of patients.
All three individuals (intubation, ultrasound, and capnography operators) were not aware about the results of each other's actions during the intubation. Ultimately, intubation accuracy by capnography was investigated, and the results were recorded in each patient's profile. Other patient information includes age, sex, body mass index (BMI), neck circumference, thyromental distance, blood pressure, number of pulses, type and severity of trauma, used drugs, intubation method, tube size, size of the laryngoscope blade, and its type and the number of attempts to intubate was recorded in the questionnaire. Finally, the collected information was analyzed by SPSS software (ver. 20) (SPSS Inc. in Chicago). using Mann–Whitney and Rock analysis tests. The significance level was considered <0.05.
To calculate sensitivity, specificity, positive predictive value, and negative predictive value of ultrasound for confirmation, the following formulas were used based on the agreed table 2 × 2:
Sensitivity = TP/(TP + FN)
Specificity = TN/(FP + TN)
Positive predictive value = TP/(TP + FP)
Negative predictive value = TN/(FN + TN).
Results
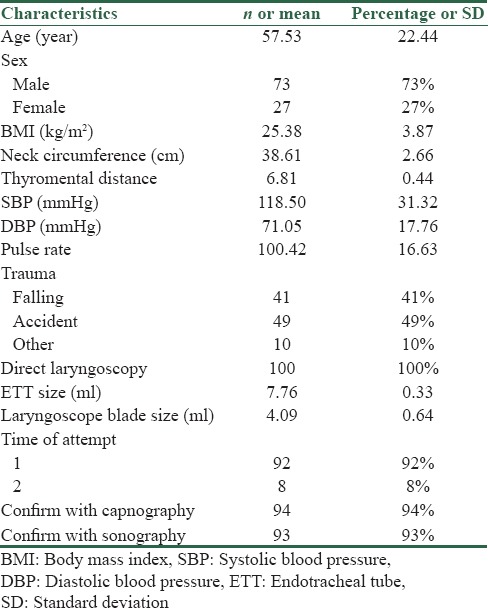
In this study, 100 patients with multiple trauma including 73 males and 27 females were identified for endotracheal intubation with the mean age of 57.53 ± 22.44 years. Type of trauma in 41% was falling, in 49% was motorcycle or car accident, and in 10% was dedicated to other items. The drug used in all of them was RSI, and all patients had direct laryngoscopy in which the type of laryngoscopy was Macintosh [Table 1].
Table 1.
Main and clinical characteristics of the studied patients
The diagnosis of intubation accuracy indicated that it was successful in 94 individuals (94%) while it was unsuccessful in 6 ones (6%) based on the results of capnography (true diagnosis of intubation). Moreover, based on ultrasound, intubation accuracy in 93 people (93%) was confirmed while inaccuracy of intubation in 7 people (7%) was diagnosed. in diagnosis of intubation accuracy the sensitivity and specificity of ultrasound were 97.9% (92.94) and 83.3% (5.6%) respectively.
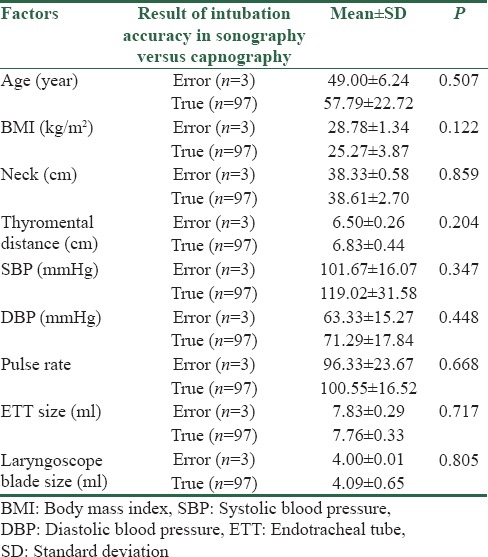
The positive predictive value was 98.9% (92.93) and its negative predictive value was 71.4% (5.7%) (area under the receiver operating characteristic curve = 0.906, P = 0.001) [Table 2 and Figure 1]. As it was mentioned, there were only three errors in the ultrasound method compared to the capnographic method for intubation accuracy (Mismatch of the intubation accuracy results between the two methods) in two men and one woman with the mean age of 49.00 ± 6.24 years. Means of BMI and thyromental distance in cases of fault diagnosis of intubation accuracy using ultrasound method were 28.78 ± 1.34 kg/m2 and 6.50 ± 0.26 cm, respectively, and were 25.27 ± 3.87 kg/m2 and 6.83 ± 0.44 cm, respectively, in cases of correct diagnosis of the intubation accuracy (P = 0.122, 0.204). Therefore, patients, who detection of intubation accuracy for them using ultrasound was diagnosed with error, had higher amount of BMI and less thyromental distance, but these disparities were not recognized as significant differences due to the low error rate [Table 3].
Table 2.
Sonography compared with capnography for diagnosis confirmatory for endotracheal tube
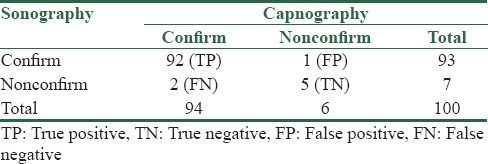
Figure 1.
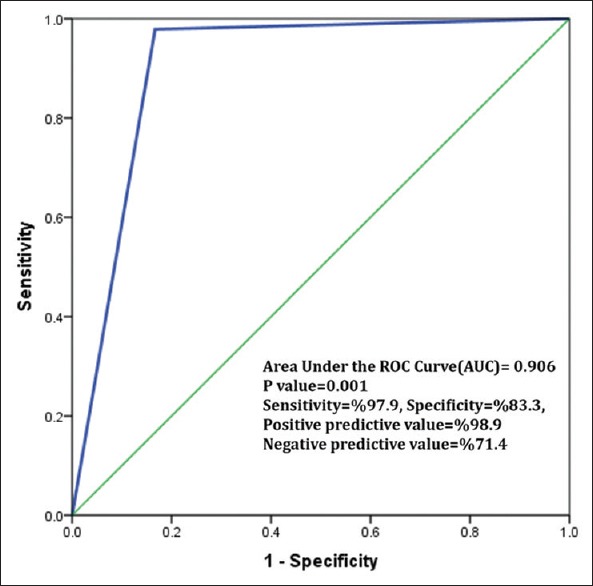
Receiver operating characteristic for comparison of sonography versus capnography for diagnosis confirmatory for endotracheal tube
Table 3.
Comparison of main and clinical characteristics of patients in terms of the correct and false diagnosis of intubation using ultrasound method
Discussion
The purpose of this study was to investigate the accuracy of ultrasound in the diagnosis of direction for tracheal intubation. According to the results of this study, ultrasound method in determining the correct location of the tracheal tube has high sensitivity and specificity. Moreover, it is comparable to capnography in our study. In setting of emergency materials, correct determination of the ETT is one of the most important measures which is essential and important to prevent brain hypoxic injury.[14] If misplacement of tracheal tube whose prevalence is about 6%–16% was not diagnosed, it causes brain damage and death.[16] Therefore, it is necessary for any physician that works in an emergency section to confirm correct placement of the tracheal tube.[17] There are several ways to confirm the proper placement of the tracheal tube. Each of which has limitations and problems.[15] Based on America's heart guideline (American Heart Association), it was stated in 2010 that confirmation of the correct intubation must be done by clinical evaluation as well as a machine method.[18] According to studies, only physical examinations such as listening to the lungs and patient's epigastric pain, observing chest movements, and steam out of the tracheal tube are not secure methods to evaluate the correct placement of the tracheal tube. In addition, pulse oximetry and chest X-ray (CXR) are not reliable methods, and CXR also needs time, which cannot be performed during the recovery period.[18] It was stated by advanced cardiac life support in 2015 that continuous clinical evaluation along with the evaluation of capnography is one of the most reliable assessments to check the correct placement and monitoring.[19] Therefore, capnography is a gold standard method for proper evaluation of the tracheal tube.[20] However, this method has its own limitations. Capnography measures the amount of carbon dioxide. Thus, this method is reliable in patients who have a lung airflow, but it cannot be evaluated in patients with cardiac arrest and pulmonary massive embolism as well as the cases in which the patient has complete apnea.[11] On the other hand, capnography is not available in all emergency departments.[21] Using ultrasound is a reliable and useful method in evaluating the correct placement of the tracheal tube.
The reasons that made this method as a reliable technique include the following points:
An ultrasound device is available in most emergency departments
Using an ultrasound machine requires less experience and training. Moreover, most doctors who work in an emergency department can use it for evaluation
Using ultrasound method is very convenient, noninvasive and it needs a little time. In addition, it does not interfere in the recovery process of patients
An ultrasound machine is a portable device and it is easy to use
Ultrasound images are not affected by pulmonary airflow and the heart condition of patient unlike the capnography that cannot be assessed in case of cardiac arrest or lack of pulmonary flow
Unlike the capnography, an ultrasound evaluation can be used before the bag-valve-mask tube intubation.[22] Therefore, diagnosis of esophageal intubation in the early stages can be done; before the time, the airflow enters into the stomach and causes subsequent complications such as aspiration, nausea, vomiting, and abdominal distention. In addition, sonography can be used in the outside of hospital setting as the outside of medical centers is where the most complications occur caused by abnormalities in placement of the tracheal tube and the outcome of brain hypoxemia. Considering a lot of advantages and benefits of ultrasound, it has become as a reliable and attractive method to check the tracheal tube.[23]
According to the results of the current study, an ultrasound method has high sensitivity and specificity to determine the correct placement of the tracheal tube and it can be implemented as a reliable method given the acceptable positive and negative predictive values. The latest and most reliable study that has been conducted recently in this area is referred to a systematic review and meta-analysis study in 2015 by Chou et al. which included 12 studies which have been done in this field. It consisted of 1656 attempts for intubation in which 550 of them (33.2%) were diagnosed as esophageal intubation. Finally, they came to the conclusion that using the ultrasonography method to detect esophageal intubation in case of wrong insertion of esophageal tubes is significant according to the results of this meta-analysis, especially because of its high specificity value.[23] Of course, in accordance with the results of this valuable research based on 12 studies, different settings, experiences of the person performing the ultrasound, as well as the type of ultrasound device and time of doing ultrasound cause very little but nonsignificant impact on ultrasound diagnostic accuracy.
These effects are not very specific and effective, and in fact, the mentioned research is the first meta-analysis study which has been done in this regard. The result of this meta-analysis is that ultrasonography with a favorable sensitivity and excellent specificity can detect esophageal intubation especially when capnography is not available. Another study was carried out by Ma et al. in 2007, and 7 residents of emergency medicine investigated 70 cases of ultrasound intubation in dynamic mode (when intubation was in progress) and 70 cases of ultrasound in static mode (after completion of intubation). Finally, they concluded that dynamic transcricothyroid ultrasound is a reliable method for evaluation which has sensitivity of 97% and specificity of 100%. Static method has sensitivity of 51% and specificity of 91% to diagnose esophageal intubation. They advised that dynamic method is the most reliable technique among others.[10] Among other benefits of using ultrasound, it can be said that there is no need to disconnect chest compression during the recovery operation to check the proper placement of the tracheal tube. In this regard, a study was carried out by Jen Tang in 2014 in which 96 patients with cardiac arrest who needed tracheal intubation were selected, and assessment of trachea was done by ultrasound. It was concluded that 7 individuals (7.3%) among 96 patients had esophageal intubation; they also represented that sensitivity and specificity as well as positive and negative predictive values of the ultrasound method are excellent and can be used as a useful method in evaluating these patients even without chest compression which is also one of the advantages of this method. An ultrasound method has its own limitations such as operator dependency which depends on the experience of the person performing it. In case that is done by attending, it has more sensitivity and specificity in comparison with residents. Moreover, it rests on the setting of the device, and the ways and location of doing it affect the accuracy of diagnosis. That is why sensitivity and specificity are expressed in different ways in various studies. One limitation of the current study is that ultrasonography has been compared with capnographic method in low volume and in a time range. However, method of capnography has its own limitations.
It is recommended that this study was done with higher rate of volume and more samples and in patients with a specific diagnosis. It is also suggested that this method be evaluated with other available methods such as clinical assessment so that it can be used in case of confirmation in the clinic.
Conclusion
The malposition of the tracheal tube in the early minutes of resuscitation can make irreparable complications to the patient. Therefore, diagnosis of correct placement of the tracheal tube is of vital importance. Secondary sonography method has many advantages and can be implemented in setting of inside and outside the hospital due to high specificity and sensitivity. Other studies are required in this regard to confirm these outcomes and it is suggested that in view of the high sensitivity and specificity of this method in other studies, the study of a combination of ultrasound and clinical evaluation (for example, hearing lung sounds at two points or aspiration procedure) compared to the gold standard to achieve specificity and sensitivity of 100% was done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Walls RM. Airway. In: Morx JA, editor. Rosen's Emergency Medicine: Concepts and Clinical Practice. 7th ed. London: Taylor & Francis; 2010. pp. 3–22. [Google Scholar]
- 2.Soleimanpour H, Sarahrudi K, Hadju S, Golzari SE. How to overcome difficult-bag-mask ventilation: Recents approaches. Emerg Med. 2012;2:e116. [Google Scholar]
- 3.Park SC, Ryu JH, Yeom SR, Jeong JW, Cho SJ. Confirmation of endotracheal intubation by combined ultrasonographic methods in the emergency department. Emerg Med Australas. 2009;21:293–7. doi: 10.1111/j.1742-6723.2009.01199.x. [DOI] [PubMed] [Google Scholar]
- 4.Leong MT, Ghebrial J, Sturmann K, Hsu CK. The effect of vinegar on colorimetric end-tidal carbon dioxide determination after esophageal intubation. J Emerg Med. 2005;28:5–11. doi: 10.1016/j.jemermed.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13:239–44. doi: 10.1197/j.aem.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–76. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 8.Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Kerrey BT, Geis GL, Quinn AM, Hornung RW, Ruddy RM. A prospective comparison of diaphragmatic ultrasound and chest radiography to determine endotracheal tube position in a pediatric emergency department. Pediatrics. 2009;123:e1039–44. doi: 10.1542/peds.2008-2828. [DOI] [PubMed] [Google Scholar]
- 10.Ma G, Davis DP, Schmitt J, Vilke GM, Chan TC, Hayden SR, et al. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32:405–7. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh KS, Lee CL, Lin CC, Huang TC, Weng KP, Lu WH, et al. Secondary confirmation of endotracheal tube position by ultrasound image. Crit Care Med. 2004;32:S374–7. doi: 10.1097/01.ccm.0000134354.20449.b2. [DOI] [PubMed] [Google Scholar]
- 12.Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49:75–80. doi: 10.1016/j.annemergmed.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Milling TJ, Jones M, Khan T, Tad-y D, Melniker LA, Bove J, et al. Transtracheal 2-D ultrasound for identification of esophageal intubation. J Emerg Med. 2007;32:409–14. doi: 10.1016/j.jemermed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 14.Thomas VK, Paul C, Rajeev PC, Palatty BU. Reliability of ultrasonography in confirming endotracheal tube placement in an emergency setting. Indian J Crit Care Med. 2017;21:257–61. doi: 10.4103/ijccm.IJCCM_417_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun J-T, Sim S-S, Chou H-C, Chong K-M, Ma MH-M, Lien W-C. Ultrasonography for proper endotracheal tube placement confirmation in out-of-hospital cardiac arrest patients: Two-center experience. Crit Ultrasound J. 2014;6(Suppl 1):A29. [Google Scholar]
- 16.Galicinao J, Bush AJ, Godambe SA. Use of bedside ultrasonography for endotracheal tube placement in pediatric patients: A feasibility study. Pediatrics. 2007;120:1297–303. doi: 10.1542/peds.2006-2959. [DOI] [PubMed] [Google Scholar]
- 17.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729–67. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 18.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S444–64. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 19.Rahul K, Cara K, Ahmad A. Using ultrasound to confirm endotracheal tube position in the Intensive Care Unit. J Anesth Intensive Care Med. 2016;1:555560. [Google Scholar]
- 20.Hernandez C, Shuler K, Hannan H, Sonyika C, Likourezos A, Marshall J, et al. C.A.U.S.E.: Cardiac arrest ultra.sound exam – A better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation. 2008;76:198–206. doi: 10.1016/j.resuscitation.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 21.Breitkreutz R, Walcher F, Seeger FH. Focused echocardiographic evaluation in resuscitation management: Concept of an advanced life support-conformed algorithm. Crit Care Med. 2007;35:S150–61. doi: 10.1097/01.CCM.0000260626.23848.FC. [DOI] [PubMed] [Google Scholar]
- 22.Breitkreutz R, Price S, Steiger HV, Seeger FH, Ilper H, Ackermann H, et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: A prospective trial. Resuscitation. 2010;81:1527–33. doi: 10.1016/j.resuscitation.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 23.Chou EH, Dickman E, Tsou PY, Tessaro M, Tsai YM, Ma MH, et al. Ultrasonography for confirmation of endotracheal tube placement: A systematic review and meta-analysis. Resuscitation. 2015;90:97–103. doi: 10.1016/j.resuscitation.2015.02.013. [DOI] [PubMed] [Google Scholar]


