Abstract
Biomedical approaches for diagnosing and managing disabling low back pain (LBP) have failed to arrest the exponential increase in health care costs, with a concurrent increase in disability and chronicity. Health messages regarding the vulnerability of the spine and a failure to target the interplay among multiple factors that contribute to pain and disability may partly explain this situation. Although many approaches and subgrouping systems for disabling LBP have been proposed in an attempt to deal with this complexity, they have been criticized for being unidimensional and reductionist and for not improving outcomes. Cognitive functional therapy was developed as a flexible integrated behavioral approach for individualizing the management of disabling LBP. This approach has evolved from an integration of foundational behavioral psychology and neuroscience within physical therapist practice. It is underpinned by a multidimensional clinical reasoning framework in order to identify the modifiable and nonmodifiable factors associated with an individual's disabling LBP. This article illustrates the application of cognitive functional therapy to provide care that can be adapted to an individual with disabling LBP.
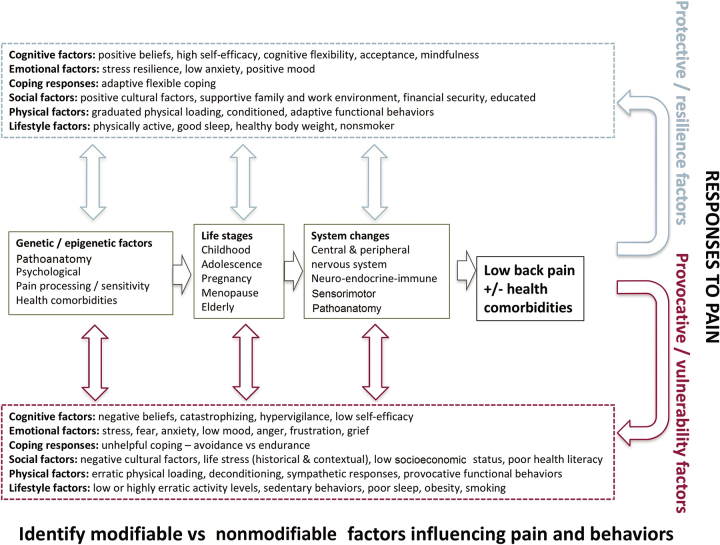
Low back pain (LBP) is ranked globally as the leading cause of disability1 that emerges during adolescence, escalating into adulthood.2 Although for some LBP is self-limiting and not disabling, for many others LBP becomes disabling and distressing and negatively affects many aspects of daily life.3 Disabling low back pain (LBP)in the absence of serious pathology is best seen as neurobiological and behavioral responses to individuals’ actual and/or perceived threat to their body, lifestyle, or social circumstances and/or disruption to their homeostasis. This response is modulated by an array of changes across the neuroendocrine-immune-motor systems. These changes interact with, and are influenced by, different combinations of genetic, pathoanatomical, physical, psychological, social, lifestyle and other health factors that are largely unique for each individual, cannot be decoupled from each other, and vary at different life stages (Fig. 1). These interacting factors fluctuate temporally, influencing inflammatory processes, levels of pain perception, levels of distress, and behavioral responses.4 In this light, rather than being an “injury” related to tissue damage, an acute presentation of disabling LBP frequently presents as a pain “flare,” driven by a combination of multidimensional factors that yield pain as the output. With research displaying that the multiple factors at play in disabling LBP coexist, and are not separate entities, “boxing” patients into rigid subgroups on the basis of the clustering of common clinical features within a single domain could miss the crucial interrelationships between factors. Attempts to deal with complexity such as through classification and subgrouping systems has been criticized for being unidimensional, reductionist and failing to reflect the biopsychosocial nature of disabling LBP.5 Similar to nontargeted interventions, they neither target multiple aspects of an individual's pain experience nor individualize the targeting of such factors for each patient. Understanding these interacting processes demands a flexible multidimensional clinical reasoning framework, which allows the clinician to identify the various factors that can contribute to disabling LBP and act as targets for change in each individual.6 The framework considers both modifiable and nonmodifiable factors associated with an individual's disabling LBP experience. Rather than being a rigid subgrouping system, the framework provides clinicians with the opportunity to explore the multidimensional nature of disabling LBP through the context of the individual. The aims of this approach are to help individuals make sense of their pain within their own context and to develop an individualized management plan aligned with their personally relevant goals.
Figure 1.
Multidimensional factors associated with resilience and vulnerability to disabling low back pain.
Multidimensional Factors Associated With Disabling LBP
Pain Characteristics
It is now widely acknowledged that the experience of pain is not simply an incoming message regarding tissue “damage” from the periphery. Instead, the pain experience reflects the person's assessment of how dangerous a particular input (eg, nociceptive input from an intervertebral disk) is, on the basis of not just the intensity of the input but also the person's prior experiences, beliefs, and contextual factors. Therefore, it is unsurprising that pain characteristics for individuals with disabling LBP are highly variable and fluctuate over time, reflecting the influence of different multidimensional influences on pain mechanisms.7,8 A history of LBP is one of the strongest predictors for future disabling LBP, suggesting that these processes are ongoing for many people.9
Although subgrouping people into purely “central” or “peripheral” pain mechanisms does not reflect the individual and complex nature of disabling LBP,10 understanding that there is a spectrum of pain characteristics facilitates an understanding of the multidimensional interactions associated with an individual's presentation and helps guide management.11 For some, pain is localized with a clear “mechanical stimulus–pain response” (ie, pain is momentarily provoked and relieved by specific spinal postures, movements and activities).12 These features may reflect primarily peripherally mediated nociceptive processes linked to increased loading and reduced movement variability associated with provocative motor responses to pain13,14 and/or learned associations between feared (threatening) activities or movements and nociceptive processing at a cortical level (Tab. 1: case 2).15 For others, pain may present as widespread or ill-defined, with a disproportionate mechanical stimulus–pain response (ie, amplified, inconsistent, and/or sustained pain responses to minor mechanical stimuli) (Tab. 1: case 3). The pain may be associated with sensitivity to pressure, cold, movement, and loading, reflecting primarily central nervous system amplification of nociceptive inputs.12,16 For some with disabling LBP, there is an absence of clear reproducible clinical findings, when central pain mechanisms are likely to dominate16; whereas many present with a mixed pain picture (Tab. 1: case 1).
Table 1.
Multidimensional Factors and Cognitive Functional Therapy (CFT) Management for 3 Illustrative Cases of Disabling Low Back Pain (LBP).a
| Examination Findings | Case 1 | Case 2b | Case 3c |
|---|---|---|---|
| Interview | |||
| History | A 28-year-old man who was a manual worker (regularly lifting > 60 kg) developed LBP after a lifting/twisting incident 4 y earlier. He continued to work, but pain escalated. He underwent scanning and was told that he had torn disks and could not go back to manual work. He was given light duties. He received stabilization exercise training, massage, pain medication, and spine injections, without long-term benefits. He had no active management plan. |
A 64-year-old man had a 43-y history of back pain related to his work as a mechanic. His pain was episodic, with persistent background pain. He also reported generalized pain in his neck and legs. Previous pain medication, chiropractic, and physical therapy focusing on spine mobilization, spine stabilization, and postural training; these treatments provided only short-term pain relief, if any; he had given up treatments in the last 2 y. He had no active management plan. |
A 26-year-old woman was involved 2 y earlier in a traumatic bike accident in which she hit a brick wall. She experienced severe widespread pain in her thoracolumbar spine and had signs of a posttraumatic stress response (flashbacks). Her pain level eased over the subsequent 3 months and then deteriorated. In the last 2 y she received various interventions, such as acupuncture, stabilization training, Pilates, massage, and medical management. Her pain disorder had worsened in severity in the last 12 mo. She was receiving ongoing physical therapy. |
| Pathoanatomical factors | Modic changes associated with disk degeneration at L4-L5/L5-S1 on MRI | Normal age-related changes on radiographs | Normal MRI |
| Pain characteristics | LBP was present at rest and was provoked with flexion loading postures, movements, and activities | LBP and tension were present at rest (sitting and standing) and were provoked with lying, sitting, standing, and forward bending postures, movements, and activities Repeated forward bending escalated pain Pain was relieved with relaxing and walking |
Widespread thoracolumbar pain was greater on the left side Pain was present at rest and with sitting, standing, and lying Focusing on pain increased its intensity Thinking of the accident increased pain and muscle tension Pain flares were associated with stabilizing exercises Walking eased pain |
| Psychological factors: Cognitive | Beliefs: “My disk is stuffed, and I fear I will never be able to work again.” | Beliefs: pain is related to “bad posture”; need to “sit up straight” and “brace back with bending.” “I did damage years ago.” |
Belief: “I think I have developed bad habits.” “I have been told so many different things I am confused.” “My posture is wrong.” “Riding a bike is bad for my back.” “There is no relief from the pain; I have no control over it.” |
| Pain hypervigilance | Pain hypervigilance | Pain hypervigilance | |
| Low pain self-efficacy | Low pain self-efficacy | Low pain self-efficacy | |
| Avoidance coping related to bending, lifting, and work and social settings | Acceptance: “I just live with it”; “I have given up.” Avoidance coping related to physical activity: “I avoid bending, gardening, and lifting.” |
Avoidance of physical activity and housework Endurance coping related to work: “I just keep going in spite of pain escalation.” |
|
| Psychological factors: Emotional | Depressed mood, frustration and anger, stress sensitivity | Frustrated that nothing shows on scan and that he has no explanation for his pain | Posttraumatic stress response |
| Sense of loss of identity | “I am a stressed guy.” Fear avoidance related to forward bending and lifting: “The ‘thought’ of bending is frightening.” Pain-related anxiety and low mood |
“Thinking about the accident gives me pain.” “I have flashbacks about the accident.” “I feel panicky”; “I am a worrier”; “I get stressed easily.” “I worry I am not going to get better.” “I hate it; it's driving me mad; I am frustrated; it gets me down; I can’t do things; I used to be really active.” Pain-related anxiety Low mood and frustration |
|
| Social factors | Socially isolated Low levels of social support and engagement Relationship stress Light duties for 3 y (work absence because of pain) |
Supportive family environment Sad that he is unable to be physically active Retired from work |
Regarding working: “I enjoy it—although it is stressful.” “Pain is worse on stressful days.” Good social support |
| Lifestyle factors | Activity avoidance High level of sedentary behavior (rests 4 h/d), unhealthful sleep habits (stays up late at night) Normal work duties are physically demanding |
Walks daily: “It relaxes me.” Activity avoidance related to bending and lifting Sleep patterns: difficult to “switch off” and wakes if pain is exacerbated |
Walks daily Cycling causes pain (“my back tenses up”), so avoids it |
| Health-related factors | Generalized fatigue | Feels stressed, anxious, run down, and tense all the time | |
| Physical examination | |||
| Sensory profile | Localized hyperalgesia in lower lumbar spine structures and soft tissue with light palpation. Increase in pain with repeated forward bending Directional provocation related to loaded lumbar spine flexion postures and movements |
Hyperalgesia at L5-S1 and L4-L5 with palpation Increase in pain with repeated forward bending Provocation of pain with anterior pelvic tilt in sitting and standing Directional provocation related to postures and movements linked to active extension of lumbar spine |
Widespread hyperalgesia of thoracolumbar spine on left side (with light palpation) No clear directional pattern of pain provocation with spinal movement |
| Observation of pain-provoking functional behaviors | Sitting was associated with flexed lower lumbar spine and extended thorax with bracing of abdominal wall Sit to stand and forward bending were initiated with lumbar flexion, thoracic extension, bracing of abdominal wall, and propping up with the hands Returning to upright from forward bending was associated with bracing of abdominal wall and thoracic extension on flexed lumbar spine Avoidance of left leg loading during load transfer and standing |
Lying, sitting, and standing postures as well as forward bending and lifting were all associated with maintaining lumbar lordosis Bracing of abdominal wall with breath holding was noted during sit to stand, forward bending, and lifting When picking up a pen and when lifting a weight off the floor, he squatted, maintained lordosis, and reported LBP |
Sitting erect and tense (back and abdominal wall muscles) Autonomic responses (rapid apical breathing, eyelid flickering, restlessness) Spine range of movement full with minimal report of pain |
| Guided behavioral experiments | Relaxing thoracic spine into flexion, enhancing lumbar lordosis via anterior pelvic tilt, and diaphragmatic breathing reduced pain in sitting Initiating sit to stand and forward bending via accentuating hip flexion (to reduce lumbar flexion), flexing thoracic spine, breathing, and avoiding propping up with the hands reduced pain Body perception: he perceived that back was extended when it was flexed |
Relaxing back posture with reduced lordosis in sitting reduced LBP Posterior tilt in standing reduced LBP Relaxing abdominal wall and back with forward bending reduced LBP Repeated bending without bracing abdominal wall reduced LBP Lifting with relaxed back reduced tension and pain Body perception: he perceived that back was flexed when it was in lordosis |
Visualization of cycling over a bump caused her to jump and become tense Slow diaphragmatic breathing and relaxation of spine posture (sinking into a chair) reduced resting pain |
| Conditioning | Deconditioning of legs and back muscles observed with sustained squat holds (limited to 10-s hold) | Generalized deconditioning specific to lifting and gardening | Generalized deconditioning |
| CFT intervention | |||
| No. of sessions | 8 sessions over 3 mo | 5 sessions over 3 mo | 3 sessions over 3 mo |
| Making sense of pain | Explain how negative beliefs, distress, lack of sleep, activity avoidance, and protective muscle guarding set up a vicious cycle of pain sensitivity and disability Behavioral experiments demonstrated that reducing his protective guarding decreased his pain and enhanced his functional capacity Reinforce that the spine is resilient and that the natural history of modic changes is good Education regarding healthful sleep habits Goals: enhanced pain control during functional tasks, return to activity, social engagement, and graduated return to work duties |
Explain that the combination of “postural and lifting” beliefs and behaviors, bracing abdominal wall, loss of hope, fear avoidance, worry, lack of confidence, and pain hypervigilance set up a vicious cycle of pain sensitivity and disability Behavioral experiments demonstrated that relaxing his spine into flexion reduced his pain and enhanced his functional capacity Reinforce that his back is structurally sound, that pain does not equal harm, and that spinal flexion and relaxation of abdominal wall are healthful and safe Goals: enhanced pain control in sitting, standing, bending, and lifting and increased confidence in the spine to return to bending, lifting, and gardening |
Explain that pain is associated with sensitization of spinal structures linked to a posttraumatic stress response, pain-related anxiety, vigilance, high levels of autonomic responses, muscle tension, poor sleep, and mixed endurance/avoidance coping behaviors Behavioral experiments demonstrated that body relaxation reduced her pain and enhanced her functional capacity Reinforce that hurt does not equal harm Change response to pain: when you hurt or feel stressed, relax posture and breathe into your belly Goals: learn to relax muscles; pain control during sitting, standing, and shopping; return to cycling |
| Exposure with control | Training of postural control strategies in sitting with anterior pelvic tilt, relaxed thoracic spine, and lateral costal breathing Training of sit to stand, forward bending, and lifting movements with flexed and relaxed thoracic spine and accentuation of hip flexion; integration of this training with focus on lateral costal diaphragmatic breathing, relaxation of abdominal wall, and leg drive rather than propping up with the hands Visual feedback with mirror, video, and written instructions Integration of new patterns into functional tasks, such as bending and lifting Reduction of rest periods during the day in a time-contingent manner until abolished Graduated conditioning focusing initially on legs, with sustained and repeated squats and lunges and with focus on pelvic control, thoracic flexion, and control of lateral costal breathing |
Teach abdominal wall and back muscle relaxation (abdominal breathing) and relaxed (flexed) spinal postures in previously provocative sleeping, sitting, standing, bending, and lifting positions Graduated exposure to lumbar flexion with control (progressing from supine [posterior pelvic tilt, hip flexion] to sitting relaxed [slouched] in chair, bending, and lifting with relaxed back and without muscle guarding and breath holding) Visual feedback with mirror and written instructions Positive reinforcement that movements are safe Integrate relaxed and flexed spinal postures into aggravating activities, such as driving, bending, lifting, gardening, and housework |
Replace bracing core muscles with diaphragmatic breathing in sitting (breathing into the pain); focus on slow, relaxed nose breathing Relaxation of spine posture in sitting (sinking into a chair) Integrate relaxation of the spine into sitting at work, driving, shopping, and cycling |
| Lifestyle change | Sleep habits: aim for 7 h/night, regular sleep time, and no alcohol or screen time before bed Physical activity: daily exercise bike, walking program progressing to gym on the basis of the patient's preference Social reengagement and return to work in a time-contingent manner over 3 mo |
Maintain walking program Graduated resumption of gardening and lawn mowing Sleep: diaphragmatic breathing relaxation techniques to “switch off” |
Sleep habits: aim for 7 h/night and regular sleep time Focus on relaxed breathing and body relaxation with stressful and painful activities and integrate these with mindfulness breathing techniques Daily cardiovascular activity: walking and graduated return to cycling on the basis of the patient's preference |
| Outcome | “I don’t fear my back anymore.” “I have my life back.” Full-time manual work duties Physically active in gym and playing touch rugby Sleep and mood normalized Some pain exacerbation with sleep deprivation and stress, but he manages this with positive coping strategies Not seeking care Follow-up MRI revealed resolution of modic changes |
“I now realize my back pain was linked to all the bad advice I was given previously about my posture and core.” “I don’t fear my pain now.” “I have control over the pain.” Greater confidence and self-efficacy in his back for the future Physically active (gardening and housework) Minimal pain and disability Not seeking care |
“I became mindful of my response to pain.” “The breathing reduced my pain instantly.” “After 3 months the pain eased right off.” “I don’t worry and think about my pain now.” “I can do the things I want to do.” “I can ride my bike without pain.” Not seeking care |
aMRI = magnetic resonance imaging.
bA full video of the examination can be accessed at https://enrol.apacpdguide.com.au/courses/masterclasses-in-musculoskeletal-clinical-reasoning-peter-osullivan.
cAn abridged video of the clinical journey can be accessed at https://www.youtube.com/watch?v = QCOKLuEirHM&feature = share&app = desktop.
Pathoanatomical Factors
Disabling LBP is associated with specific spinal pathology such as a disk prolapse with radicular pain, neurological loss or cauda equina involvement in 5% to 10% of people.17 Although the natural history of disk prolapse and radicular pain for most people is favorable without surgical intervention,18 cauda equina symptoms and progressive neurology require urgent medical review. In most people with disabling LBP (90%–95%), a single pathoanatomical cause of the pain cannot be accurately determined.17 Although findings on magnetic resonance imaging (such as advanced multilevel disk degeneration and vertebral endplate changes) have a weak to moderate association with disabling LBP, they are increasingly prevalent in people who are aging and pain free19 and correlate poorly with levels of pain intensity and disability.20 This information highlights the fact that even in the presence of nociceptive input, levels of pain, distress, and disability will vary according to an interplay of individual factors.21 The reporting of pathoanatomical findings can also increase patient concerns leading to anxiety and distress as well as iatrogenic disability if they are not communicated carefully.22 Although pathoanatomical factors might often be nonmodifiable, the considerable potential for some pathologies to resolve over time should also be communicated to patients.23 Although consideration of specific pathology is important, it should be regarded as just one part of a multidimensional examination and clinical reasoning process (Tab. 1: case 1). This approach allows the clinician to view disabling LBP through a broad lens and yet not be overwhelmed by the breadth of factors considered.
Physical Factors
Levels, and patterns, of exposure to mechanical spinal loading linked to activities of daily living, work and/or sport, involving heavy and or repeated loading, awkward bending and twisting, are known to be associated with disabling LBP.24,25 These interact with other factors such as habitual movement patterns, levels of conditioning, perceptions of fatigue, general health, and psychological factors, to increase the risk of pain.26,27
Pain-related functional behaviors, on the other hand, are motor responses to pain, the threat of pain, and/or pain-related distress. These behaviors are commonly characterized by stiffer, slower, less variable and more guarded spinal movements,28,29 higher levels of trunk muscle activity, and an inability to relax the back muscles during movements such as forward bending.30 These responses may be protective and adaptive, for example, as sometimes observed in the presence of acute tissue pathology and/or traumatic injury. However, when they are disproportionate to the degree of trauma or tissue pathology or persist beyond tissue healing time, they are usually maladaptive, unhelpful and provocative.
The pain response to mechanical loading may differ between individuals.14,31 For example some people may be sensitized to lumbar flexion (Tab. 1: case 1), extension (Tab. 1: case 2), side bending, or a combination of these.32
There is also individual variability in the functional behaviors observed with these pain responses.14,31 For example, pain provoked during sitting, forward bending, or lifting may be associated with the lumbar spine being actively braced into flexion or extension. In contrast, for others the same tasks may be associated with lateral movement and avoidance of loading the painful side. For some, these pain-related functional behaviors present as subtle movement and postural changes linked to pain during functional tasks. However, with high levels of pain-related distress and disability these often manifest as overt safety behaviors (eg, propping up with the hands and avoidance of loading a limb or spinal movement, repetitive touching, or “checking” the pain) and communicative behaviors (eg, grimacing and wincing) (Tab. 1: case 1).6 Sympathetic nervous system responses are also observable in some (eg, rapid apical breathing, high levels of muscle tension, flickering eyelids, sweating, and restlessness) in distressed individuals and/or when confronted with feared tasks (Tab. 1: case 3).33 These pain-related functional behaviors are linked to factors such as pain-related fear and distress, degree of tissue sensitivity,32 and altered body perception, highlighting the close body-mind relationship.34
Psychological Factors
There is a growing body of evidence that psychological factors, both cognitive and emotional, influence pain processing, perceptions, levels of pain-related distress, and coping responses. Table 2 shows a list of clinician prompts and quotes from patients with disabling LBP illustrating common psychological factors. The individual nature of these factors is observed in Table 1 (cases 1, 2, and 3).
Table 2.
Interview Prompts and Quotes From People With Disabling Low Back Pain That Exemplify Factors Influencing Pain and Behavioral Responses.
| Psychological Factors | Interview Prompts | Examples of Replies |
|---|---|---|
| Cognitive factors (thoughts about pain and coping with pain) | ||
| Cause/meaning | What do you think is the cause of the pain? | There is something damaged. |
| Consequences | Where do you see yourself in the future? | I will always have a weakness that I need to protect. It will get worse as I get older. |
| Vigilance | How much is your mind on your pain? | I can’t stop thinking about the pain. |
| Self-efficacy | How confident are you with your back? | I have no confidence in my back. |
| How confident are you to do the things in life that you value? | I have no confidence to play with my kids. | |
| Pain interference/disability | How has the pain impacted your life? | I can’t garden, work, or socialize because of my pain. |
| Coping with pain | How do you cope with your pain? | There is nothing that I can do for my pain. |
| Have you avoided important activities or modified the way you do them because of your pain? | I avoid anything that hurts my back. | |
| I always protect my back when I lift. | ||
| Catastrophic thoughts | What do you think will happen if you bend your back? | I fear my back is going to break. |
| Where do you see yourself in the future? | I fear I am going to end up in a wheelchair. | |
| Emotional factors (feelings about pain) | ||
| Emotional response to pain | How does the pain make you feel? | It's so intense I can’t think. |
| How does the pain affect you emotionally? | I panic when I get the pain and become hopeless about getting out of it. | |
| Anxiety | Do you worry about the pain? | The pain makes me feel anxious all the time. I worry it won’t get better. |
| Depressed mood | Does it get you down? In what way? | I am in a dark place; I have lost hope, and I see no way out. |
| Frustration/anger | Does the pain make you feel frustrated? What is it that frustrates you? | I feel so frustrated and angry that this has happened to me. |
| Influence of emotions on pain | Does how you feel (mood, worry, stress, fatigue) influence your pain? | My pain gets worse when I am stressed/anxious/down/tired. |
| Fear of damage | How do you feel when you bend and lift? | Every time I bend I am terrified I will prolapse my disk. |
| Fear of pain | How do you feel about the pain? | I am just frightened of the pain and the suffering. |
| When I get the pain I can’t do what I need for hours. | ||
| Pain predictability | Does the pain feel predictable to you? | I can’t predict it. |
| Pain controllability | Do you feel in control of the pain? Are there things you can do to control your pain? | I have little control over my pain. |
Cognitive factors reflect the thoughts that individuals have about their pain or other aspects of their life. These may include negative explicit and implicit beliefs about disabling LBP,35,36 its meaning, and future consequences.37 For some, disabling LBP is associated with catastrophic thoughts, characterized by a fixation on pain that can take the form of hypervigilance and rumination, magnification of its threat, and adoption of an outlook of helplessness.38 Low levels of self-efficacy (lack of confidence in performing pain-provoking or threatening activities) are often linked to these negative cognitions.39 Many negative cognitions originate from encounters with health care practitioners.40,41 They may also be associated with an underlying negative emotional response linked to behavioral conditioning and unhelpful parental responses to pain, as well as cultural and societal attitudes.42
Emotional factors reflect an individual's feelings, which may be driven by underlying pain cognitions, contextual social stressors, and/or comorbid mental health issues.43,44 Fear is a common emotional response to pain when it is linked to beliefs regarding tissue damage and/or fear of pain and suffering.37 Levels of fear are closely related to perceptions of pain controllability, predictability, and intensity. Negative emotional factors may also include high levels of perceived stress and negative responses to social stressors; anxiety about pain; depressed mood linked to the loss of functional capacity and quality of life; and heightened levels of frustration, anger, and perceived injustice.3
Negative cognitions and emotional distress are often associated with pain amplification and unhelpful coping responses leading to disability. For some, coping responses are associated with avoidance of work, social situations, recreation, specific postures, movements, and valued activities.45,46 Others persist with pain-provoking, desired activities in spite of escalation of pain and distress,47,48 while adopting guarded and provocative functional behaviors. However, many people present with a mix of these 2 different coping responses leading to a “boom-bust” cycle of pain persistence and avoidance.
Social Factors
Historical and contextual social factors and associated levels of distress are also known to affect disabling LBP.49 These may include cultural and societal conditioning factors (eg, family history of disabling LBP, socioeconomic status, and education); exposure to stressful life events and situations (eg, abuse, financial hardship, poor family functioning, negative work relationships, and being engaged in litigation about disabling LBP), or unhelpful relationships (eg, punishing or solicitous).50,51 Depending on the individual's life story, social factors may not be modifiable, but their contribution to pain should be discussed with the individual to increase understanding of their role.
Lifestyle Factors
Lifestyle factors are known to be important in disabling LBP and to be involved with other domains. Sleep problems and disabling LBP are highly comorbid. Poor sleep predicts the development or worsening of disabling LBP, and disabling LBP predicts sleep problems.52,53 Sleep also influences other domains, such as psychological well-being/emotional distress.54 disabling LBP may be linked to poor sleep habits and/or pain-disrupted sleep.
There is a U-shaped relationship between physical activity and disabling LBP, with both low levels of physical activity/sedentary behaviors (ie, < 90 min/wk) and high levels of physical activity (ie, > 100 minutes of vigorous activity per day) having a relationship with disabling LBP.55,56 Low levels of physical activity and sedentary behavior can negatively affect inflammatory processes as well as physical deconditioning and bone health.57 There is also growing evidence for the role of lifestyle factors linked to abdominal obesity in disabling LBP, influencing both loading and inflammatory processes.58,59 There is also evidence that smoking is an independent risk factor for LBP, although the association is modest and the exact mechanism is unclear.60
General Health Factors
Health comorbidities strongly influence disability levels, as well as providing barriers to management that may require special consideration. They may reflect shared neuroendocrine-immune mechanisms, for example diagnosed mental health disorders, sleep apnea, comorbid pain problems, obesity, and “nonspecific” health complaints such as fatigue, insomnia, and irritable bowel syndrome.61
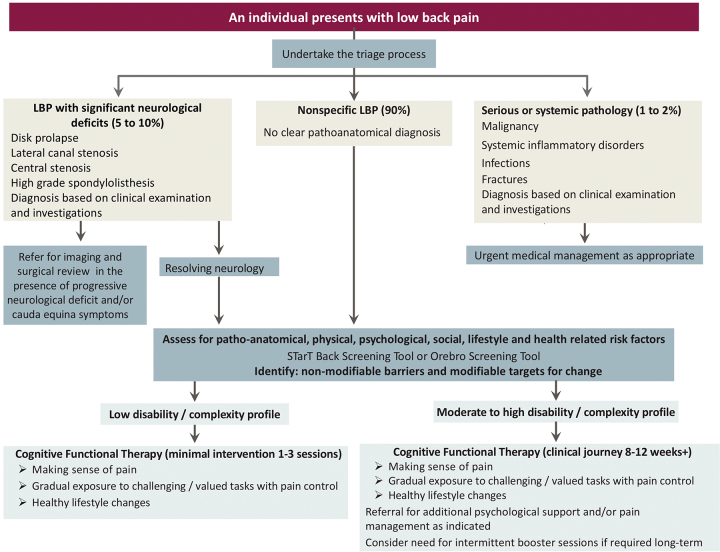
Cognitive Functional Therapy (CFT): Assessment and Treatment
CFT is an integrated behavioral approach for individualizing the management of people with disabling LBP once serious (eg, malignancy, infection, inflammatory disorder, and fracture) and specific pathology (eg, nerve root compression with progressive neurological deficit with or without cauda equina symptoms) has been excluded. Cognitive functional therapy was developed as a flexible, integrated behavioral approach for individualizing the management of disabling LBP.62 Although CFT for disabling LBP is the focus of this article, the principles of CFT can be applied for many people with LBP (Fig. 2). It uses a multidimensional “clinical reasoning framework” to identify key modifiable targets for management on the basis of careful listening to the individual's story and examining the individual's behavioral responses to pain. This approach enables the treating clinician to take individuals on a journey to effectively self-manage their disabling LBP with a program that is tailored to their unique clinical presentation and context.
Figure 2.
Triage of low back pain and the contribution of cognitive functional therapy. LBP = low back pain.
Although some of the language used to describe CFT in this article has evolved, the fundamental components of the intervention remain the same. For example, previously we described CFT63,64 as 4 interrelated components, whereas in this article we have changed the language to better reflect the therapeutic processes we perceive to be important and have condensed these to 3 components. Component 1, formerly “cognitive training,” we now call “making sense of pain,” as we perceive the importance of sense-making processes in facilitating a mind-set change in people with pain.65 Component 2, “functional movement training,” and component 3, “functional integration,” have been combined and renamed “exposure with control,” as we understand the process of change that occurs is best reflected in this manner.62 Component 4, “physical activity and lifestyle training,” is now simplified to “lifestyle change.” Our earlier work also placed more of an emphasis on subgrouping movement patterns, whereas we have shifted toward an individualized multidimensional understanding of disabling LBP,10 in which movement behaviors are just 1 component to consider in a person's presentation. Hence, we have dropped “classification based” before the name CFT to align with this idea.
Three illustrative cases are presented to demonstrate how the clinical reasoning framework can be applied to different individuals with disabling LBP in order to individualize CFT to their unique presentation (Tab. 1). The radar graphs (Fig. 3) provide a simple visual representation of the multidimensional complexity of these cases on the initial examination and how this changes across a CFT intervention.
Figure 3.
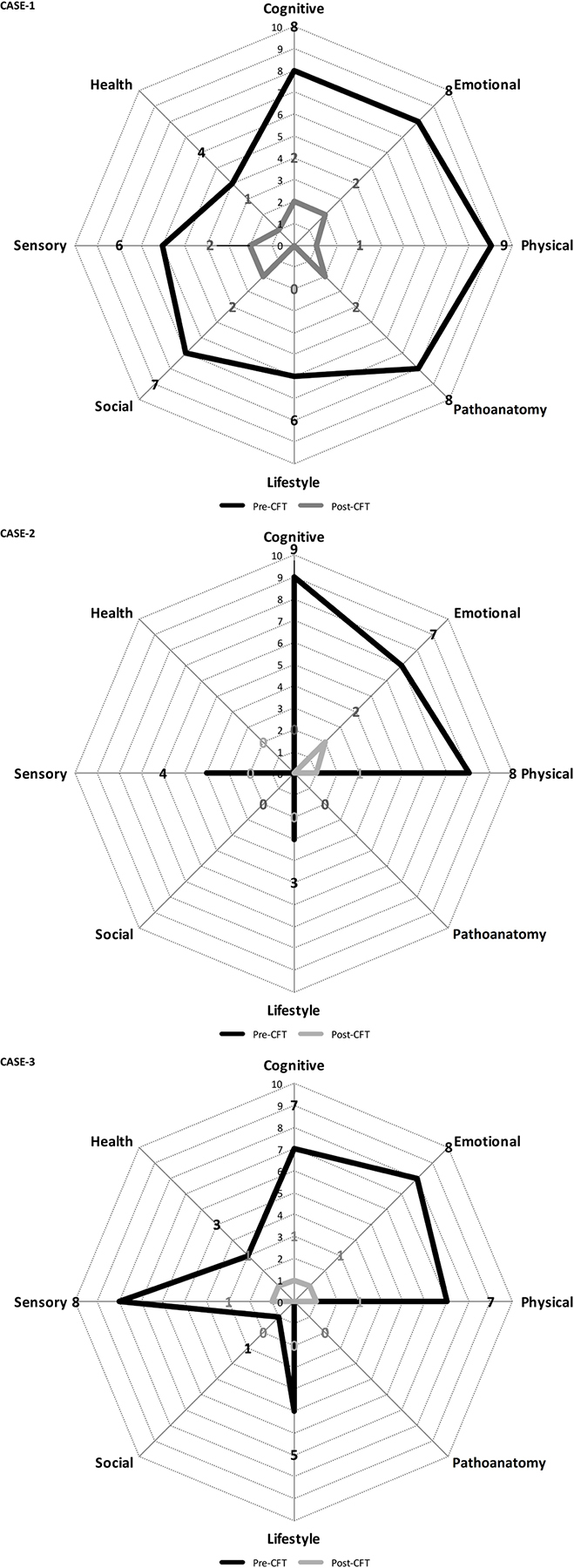
Radar graphs outlining the multidimensional profile of the 3 cases before and after the cognitive functional therapy (CFT) intervention.
Therapeutic Alliance
Central to CFT is a strong therapeutic alliance, underpinned by a motivational approach and characterized by open, reflective, empathetic, and validating communication.66 It facilitates disclosure, reinforces positive health behaviors, and encourages reflection on discrepancies in beliefs and behaviors while “rolling with resistance” (ie, avoiding direct head-on arguments or forcing suggestions on a person) when rigid beliefs dominate in order to avoid unhelpful conflict. Individual factors, such as cultural setting, treatment expectations and preferences, health literacy, levels of acceptance, and readiness for change, are also considered in order to provide care that is tailored to the person's unique presentation and context.
Interview
Prior to the interview, having individuals with disabling LBP complete a body pain chart and a multidimensional screening questionnaire can provide valuable insight into their perception of their pain.67 Although we do not use them as a stand-alone stratification tool, a questionnaire can provide an opportunity to explore pain beliefs and emotional responses to pain in the interview.
The interview then begins with an open question, such as “tell me your story,” allowing individuals to disclose in their own way how they make sense of their pain. Sensitive, nonjudgmental questioning and careful prompting facilitate disclosure of various dimensions, including:
Pain history and the presence of contextual factors (eg, social, cognitive, emotional, physical, lifestyle, and health) around the time pain began. This aspect of the interview helps differentiate acute LBP associated with a traumatic loading event from minor mechanical triggers or an insidious pain onset. This item is important so that the latter are not treated and communicated as an injury.
Pain provocation and easing responses to posture, movement, load, and rest in order to determine any mechanical stimulus–pain response patterns.
Individuals’ schema about their pain, including beliefs regarding the cause of their pain, its future time course, pain controllability, predictability, and severity. Radiological imaging findings are reviewed and discussed, especially if they reinforce negative beliefs.
Emotional responses to pain, such as fear and pain-related distress, and current social context.
Behavioral responses to pain, including strategies for coping with pain, avoidance and/or persistence, protective guarding, postural and movement habits, and lifestyle.
Painful, feared, and avoided valued functional activities are clearly identified.
General health, levels of fatigue, and health comorbidities and their relationships to pain and disability.
Perceived barriers to engaging in a healthful lifestyle.
Personally relevant goals, perceived barriers to achieving goals, and expectations.
At the end of the interview the clinician summarizes the story to check its validity.
Functional Behavioral Assessment
The behavioral assessment is directed toward the valued functional tasks (spinal postures, movements, and activities) nominated during the interview as being painful, feared, and/or avoided.
During this process, careful observation is made of the behavioral strategies adopted during these functional tasks, including the presence of safety and communicative behaviors and sympathetic responses. When these tasks involve loading activities, physical conditioning (strength and endurance) is also considered. Palpation is performed during these tasks to assess levels of tissue sensitivity, trunk muscle guarding, and respiratory patterns. Individuals are questioned regarding their beliefs, feelings, body perceptions, and pain responses while performing these tasks. This approach facilitates assessment of the individual's sensitivity profile (ie, pain responses to palpation, posture, movement, and load).
These observations then form the basis of a series of guided behavioral experiments. These guided experiments explicitly seek to reduce sympathetic responses and abolish safety and communicative behaviors (via relaxed diaphragmatic breathing, body relaxation, awareness, and control), prior to and while gradually exposing individuals to their feared, avoided, and painful tasks. Exposure in individuals who are highly fearful may include visualization before performance of the actual task. This approach is assisted with the use of visual feedback (eg, mirrors, video, and clinician demonstration) and clinician-directed, hands-on feedback using key points for body control and/or relaxation (eg, the legs, pelvis, thorax, and head). Consideration is also given to a person's directional pain responses to movement in order to facilitate exposure of valued and avoided activities in a less pain-provoking manner, when possible (cases 1 and 2). During this process, pain reduction is commonly reported.
During these guided behavioral experiments, attention is brought to discrepancies between pain expectations and actual pain experiences in order to disconfirm the individual's belief that movement is threatening and should be avoided. This approach powerfully demonstrates to the individual that moving and loading the spine without protection and avoidance is safe and that pain responses are controllable. It also provides an opportunity to reflect on the resilience and strength of the spine, and highlights a pathway for achieving valued goals. These experiments provide a powerful experiential learning opportunity for the individual and clear directions for management. Care is taken not to cause undue escalation of pain, emotional distress, or sympathetic responses in this process, so as not to reinforce the belief that pain escalation and functional activation are coupled and uncontrollable.
The process can elicit strong emotional responses, anxiety, and occasionally panic. It is important for the clinician in these situations to remain calm and empathetic, acknowledge the individual's distress, reflect on its origin, and reinforce the safety of the individual.
Table 1 illustrates how the examination process was adapted in 3 individuals with different clinical presentations.
CFT for the Management of Disabling LBP
On the basis of the examination, both nonmodifiable and modifiable factors that contribute to the individual's pain, distress, and disability are identified. Some of these factors may act as barriers to recovery, necessitating interdisciplinary care in conjunction with CFT.68 Four examples are pain management, including pharmacology, when pain levels are distressing, uncontrollable, and disrupting sleep; medical management in the presence of health comorbidities (eg, diabetes and sleep apnea); psychiatric and/or psychological management of major depressive disorders, posttraumatic stress disorder, or high levels of social stress; and dietary and psychological support when morbid obesity is present.
CFT Intervention
The primary aims of CFT are to enable the treating clinician to take individuals on an individualized journey to:
Help them “make sense of their pain” from a multidimensional perspective and within the context of their own story.
Develop effective pain control strategies by challenging negative cognitions and emotional responses to pain and modifying how they physically perform tasks (via body relaxation and extinction of safety behaviors) in order to achieve valued goals.
Adopt healthy lifestyle behaviors.
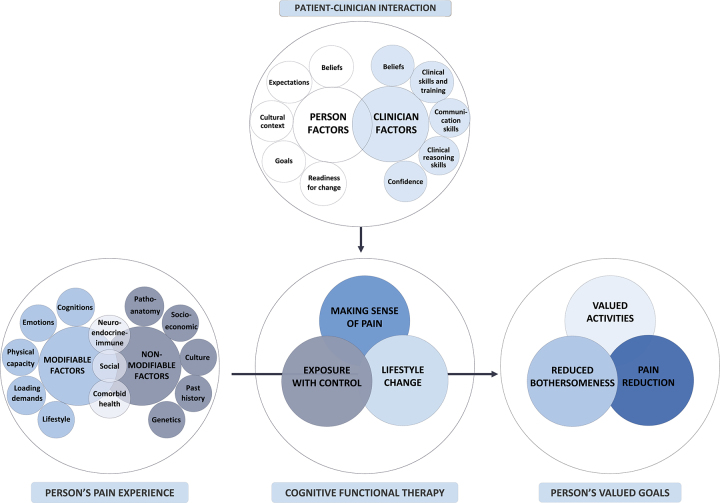
This clinical journey is adapted to the individual's multidimensional profile (illustrated in Tab. 1 and Figs. 3 and 4). The following broadly outlines the various components of CFT.
Figure 4.
Interplay of clinician- and patient-specific factors in the clinical journey with cognitive functional therapy.
Making sense of pain
The process of making sense of pain is reflective and uses individuals’ own story, words, and metaphors combined with their experiences during the guided behavioral experiments to disconfirm their previously held beliefs and provide a new understanding of their pain. This process outlines—in a nonjudgmental way—how contextual factors, negative pain beliefs, and unhelpful emotional and behavioral responses set up a vicious cycle of pain, distress and disability. This vicious cycle in turn acts as a barrier to achieving valued goals. This information is written down and discussed in a collaborative and reflective manner. During this process, different aspects of the schema are discussed while reinforcing the structural integrity of the spine and the meaning of radiological imaging.69 The individuals are then asked to reflect on what they could do to break this vicious cycle in order to reach their valued goals. Through this process, clear and realistic self-motivated strategies for behavioral change directed to their personally relevant goals are identified. Online resources70,71 and patient stories72 are also provided to facilitate this learning process.
Exposure with control
Exposure with control is a process of behavioral change through experiential learning, in which sympathetic responses and safety behaviors that manifest during painful, feared, or avoided functional tasks are explicitly targeted and controlled.62 This approach enables individuals to gradually return to their valued functional activities without pain escalation and associated distress. This process is underpinned by the guided behavioral experiments from the examination, and with consideration of the individual's levels of distress, tissue sensitivity profile (eg, with exaggerated pain responses to minor mechanical stimuli, this process is more gradual), and levels of conditioning. This process powerfully disconfirms fear-avoidance beliefs while reinforcing that valued activities can be safely confronted when performed without safety behaviors and reduced pain vigilance.
For example, prior to exposure, when pain is constant and associated with high levels of emotional distress and sympathetic responses, some strategies that are implemented include targeted body relaxation, slow diaphragmatic breathing and body scanning (Tab. 1: case 3). Once body relaxation and emotional regulation have been achieved, the individual is gradually exposed to movements or activities that they nominated are painful, feared, or avoided. During this process, body control is focused away from pain and toward key points, such as the lower limbs, pelvis, thorax, and head. Pain reduction is frequently reported during this process, disconfirming previously held beliefs that functional activation will result in pain escalation, functional loss, and harm (Tab. 1: cases 1 and 2). Targeted functional conditioning is provided when there are deficits in muscle strength and endurance that act as barriers to achieving personally relevant goals (Tab. 1: case 1). When pain control is not achievable during this process, the focus is placed away from pain and toward body relaxation, replacing safety behaviors while achieving personally relevant functional and lifestyle goals.
These new functional strategies are immediately integrated into activities of daily living in order to generalize the learning and build self-efficacy during these tasks. These are gradually progressed on the basis of the individual's personally relevant goals, level of conditioning, and perceived control over pain. Individuals are initially seen weekly for 2 or 3 sessions, after which sessions are extended to every 2 or 3 weeks in order to build confidence to self-manage over a 12-week period.62–64 During this process, pain flares are seen as an opportunity for reinforcing new ways to respond to pain without safety behaviors and avoidance. An exacerbation plan is provided on discharge in order to positively orientate the individual's emotional and behavioral responses to pain, and booster sessions may be required beyond this time if pain again becomes uncontrollable, distressing and/or disabling.
Rather than being prescriptive, CFT is reflective, in that the individual is encouraged to find new strategies to respond to pain and perform valued activities with confidence and without pain vigilance. Feedback is central to this process. Reinforcement is provided through clear and simple verbal and written explanations and clinician demonstrations. Visual feedback using mirrors and video is used to highlight discrepancies between the actual versus perceived body. Hands-on feedback is used to validate individuals’ pain experience; challenge beliefs that their spine is structurally vulnerable; provide feedback regarding tissue sensitivity, sympathetic responses, and protective muscle guarding; and decrease fear of pain and movement. However, hands-on feedback is never used to promote passive dependence or unhelpful structural beliefs.10 The emphasis of hands-on feedback should be a minimal part of sessions, as it could dilute the effect of more active approaches or reduce the priority people place on active self-management.
Lifestyle change
Unhelpful lifestyle factors, discussed as part of making sense of pain, form a central part of CFT when relevant. Individually designing73,74 of the exercise program—such that physical activity is based on preference, linked to personally relevant goals, includes home exercise73,74 and considers cost, accessibility issues, and social engagement to encourage enduring behavior change—is implemented. When the person is highly sensitized and has difficulties in self-regulation, this approach may be directed in a graduated, time-contingent manner. If safety behaviors are present during these activities (eg, muscle guarding and/or movement avoidance) a focus is placed on relaxed “normalization” of movement. When an activity is still associated with a distressing escalation of pain, a less provocative activity may first be selected and gradually progressed toward the activity of preference. For those with high levels of sedentary behaviors, activity scheduling is explored. When boom-bust patterns of overactivity and underactivity are present, activity diaries may be beneficial. All individuals are informed of the health-enhancing systemic effects in line with their story (eg, effect of mood and sleep).
Sleep deficits and disturbance may be addressed in a variety of ways on the basis of how they affect people's pain experience, as identified during the interview and examination (eg, poor sleep hygiene, worries about their back and/or life, postural beliefs, pain with rolling, and comorbid sleep apnea). For example, in the case of poor sleep hygiene, ways of engaging in healthful sleep habits are explored (eg, establishing a daily routine and reducing use of electronics in bed). Sleep disturbance due to pain, worry, or stress may be addressed with exploring the influence of body relaxation, breathing regulation, guided meditation techniques, and engaging in physical activity. When sleep is affected by postures and movement in bed, specific training of rolling and posturing in bed in a relaxed manner is explored (Tab. 1 and Fig. 3: cases 1 and 2).
Efficacy of CFT
Different aspects of this multidimensional clinical reasoning framework have shown substantial reproducibility between trained clinicians.75,76 CFT has shown long-term superior efficacy to physical therapist–led exercise and manual therapy in a randomized trial.75 Further research is under way to assess CFT in different geographical settings and to compare it to different interventions.77
Qualitative data and case studies support that people benefiting from CFT report that they have a changed mind-set toward a more multidimensional understanding of their pain, experience increased pain controllability and enhanced self-efficacy about achieving functional and lifestyle goals.78 Although the mediators of change are not yet known, they are likely to be multidimensional reflecting both central and peripheral processes.
Skills Required to Implement CFT
CFT requires specific skills across a number of domains (Fig. 4) as well as a contextual understanding of foundational behavioral psychology and neuroscience. These requirements can seem daunting for clinicians trained to primarily consider physical and pathoanatomical factors and provide passive treatments for the management of disabling LBP.79 Communication skills are required to sensitively explore across the multiple domains and facilitate a strong therapeutic alliance, build self-efficacy, and promote behavior change. Clinical reasoning skills are required to triage the individual patient and synthesize multidimensional data. Observational skills are needed to analyze functional and safety behaviors. Hands-on feedback and movement reeducation skills are required to perform guided behavioral experiments and effectively teach functional behavior change strategies. Confidence is required to discourage safety behaviors, while reintroducing the individual to threatening movements or activities. Understanding that LBP is a common protective response influenced by multidimensional factors rather than a sign of damage, that the spine is a resilient structure, that hurt does not equal harm, that movement and activity are helpful, and that pain and associated behaviors are commonly modifiable, is central to this process. Barriers for clinicians adopting this approach relate to their sense of competence and confidence to deal with psychosocial factors,79 time constraints within their clinical setting, privacy for sensitive conversations, and a shift away from providing passive therapies to treat pain. Although it is common that clinicians feel that people with disabling LBP expect passive therapies, at long-term follow-up a greater proportion of people who received CFT were highly satisfied with care than those who received traditional manual therapy and exercise approaches.63 The barriers for clinicians are similar to those for people with disabling LBP, highlighting that a mind-set shift is also needed in public attitudes and understanding of disabling LBP outside the clinic, such as in the media, schools, sporting clubs, and work environments.
Physical therapists who have been trained to broaden their skill set toward a multidimensional approach to pain report positive changes to their clinical practice and greater confidence to deal with psychosocial factors and complex cases.80 Although an average of 100 hours of training, including supervised clinical sessions was reported in the Norwegian trial,63 ongoing research is investigating the level of training required to be effective.
Conclusion
CFT is a flexible integrated behavioral approach for individualizing care for people with disabling LBP. It is based on a multidimensional clinical reasoning framework designed to identify and target modifiable factors that drive pain, pain-related distress, and disability. CFT takes individuals with disabling LBP on a clinical journey that provides a multidimensional understanding of their pain within the context of their own story. In addition, pain and behavioral control strategies are used to allow individuals to return to valued functional activities and healthful lifestyle behaviors. The aim of this process is to build self-efficacy to break the cycle of pain-related distress and disability. CFT can be integrated with interdisciplinary care when indicated. We consider that this approach is also applicable across a range of other painful musculoskeletal disorders.
Author Contributions
Concept/idea/research design: P. O’Sullivan, J.P. Caneiro, M. O’Keeffe, A. Smith, W. Dankaerts, K. Fersum, K. O’Sullivan
Writing: P. O’Sullivan, JP. Caneiro, M. O’Keeffe, A. Smith, W. Dankaerts, K. Fersum, K. O’Sullivan
Consultation (including review of manuscript before submitting): P. O’Sullivan, JP. Caneiro, M. O’Keeffe, K. O’Sullivan
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest. P. O’Sullivan, JP Caneiro, W. Dankaerts, K. Fersum and K. O’Sullivan reported payment made to them for lectures including service on speakers bureaus for running workshops on cognitive functional therapy (CFT).
References
- 1. Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coenen P, Smith A, Paananen M, O’Sullivan P, Beales D, Straker L. Trajectories of low back pain from adolescence to young adulthood. Arthritis Care Res (Hoboken). 2017;69:403–412. [DOI] [PubMed] [Google Scholar]
- 3. Bunzli S, Watkins R, Smith A, Schütze R, O’Sullivan P. Lives on Hold. Clin J Pain. 2013;29:907–916. [DOI] [PubMed] [Google Scholar]
- 4. Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(Supplement):S90–S98. [DOI] [PubMed] [Google Scholar]
- 5. Karayannis NV, Jull GA, Hodges PW. Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskelet Disord. 2012;13:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. O’Sullivan P, Dankaerts W, O’Sullivan K, Fersum K. Multidimensional approach for the targeted management of low back pain. In: Jull G, Moore A, Falla D, et al, eds. Grieve's Modern Musculoskeletal Physiotherapy. 4th ed London, United Kingdom: Elsevier; 2015:465–469. [Google Scholar]
- 7. Rabey M, Slater H, O’Sullivan P, Beales D, Smith A. Somatosensory nociceptive characteristics differentiate subgroups in people with chronic low back pain. Pain. 2015;156:1874–1884. [DOI] [PubMed] [Google Scholar]
- 8. Rabey M, Beales D, Slater H, O’Sullivan P. Multidimensional pain profiles in four cases of chronic non-specific axial low back pain: an examination of the limitations of contemporary classification systems. Man Ther. 2015;20:138–147. [DOI] [PubMed] [Google Scholar]
- 9. Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014;14:2299–2319. [DOI] [PubMed] [Google Scholar]
- 10. O’Sullivan P, Caneiro JP, O’Keeffe M, O’Sullivan K. Unraveling the complexity of low back pain. J Orthop Sports Phys Ther. 2016;46:932–937. [DOI] [PubMed] [Google Scholar]
- 11. Fillingim RB. Individual differences in pain. Pain. 2017;158(suppl 1):S11–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. O’Sullivan P, Waller R, Wright A et al. Sensory characteristics of chronic non-specific low back pain: a subgroup investigation. Man Ther 2014;19:311–318. [DOI] [PubMed] [Google Scholar]
- 13. Hodges PW, Smeets RJ. Interaction Between Pain, Movement, and Physical Activity. Clin J Pain. 2015;31:97–107. [DOI] [PubMed] [Google Scholar]
- 14. O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10:242–255. [DOI] [PubMed] [Google Scholar]
- 15. Moseley GL, Vlaeyen JW. Beyond nociception. Pain. 2015;156:35–38. [DOI] [PubMed] [Google Scholar]
- 16. Rabey M, Beales D, Slater H, O’Sullivan P. Multidimensional pain profiles in four cases of chronic non-specific axial low back pain: an examination of the limitations of contemporary classification systems. Man Ther. 2015;20:138–147. [DOI] [PubMed] [Google Scholar]
- 17. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389:736–747. [DOI] [PubMed] [Google Scholar]
- 18. Deyo RA, Mirza SK. Herniated lumbar intervertebral disk. N Engl J Med. 2016;374:1763–1772. [DOI] [PubMed] [Google Scholar]
- 19. Brinjikji W, Luetmer P, Comstock B et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol 2015;36:811–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Steffens D, Hancock M, Maher C, Williams C, Jensen T, Latimer J. Does magnetic resonance imaging predict future low back pain? A systematic review. Eur J Pain. 2014;18:755–765. [DOI] [PubMed] [Google Scholar]
- 21. Moseley L. Reconceptualising pain according to modern pain science. Phys Ther Rev. 2007;12:169–178. [Google Scholar]
- 22. Webster B, Bauer A, Choi Y, Cifuentes M, Pransky G. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine (Phila Pa 1976). 2013;38:1939–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92:147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bakker E, Verhagen A, van Trijffel E, Lucas C, Koes B. Spinal mechanical load as a risk factor for low back pain. Spine (Phila Pa 1976). 2009;34:E281–E293. [DOI] [PubMed] [Google Scholar]
- 25. Coenen P, Gouttebarge V, Van Der Burght AS et al. The effect of lifting during work on low back pain: a health impact assessment based on a meta-analysis. Occup Environ Med. 2014;71:871–877. [DOI] [PubMed] [Google Scholar]
- 26. Ng L, Campbell A, Burnett A, Smith A, O’Sullivan P. Spinal kinematics of adolescent male rowers with back pain in comparison with matched controls during ergometer rowing. J Appl Biomech. 2015;31:459–468. [DOI] [PubMed] [Google Scholar]
- 27. Steffens D, Ferreira ML, Latimer J et al. What triggers an episode of acute low back pain? A case-crossover study. Arthritis Care Res (Hoboken). 2015;67:403–410. [DOI] [PubMed] [Google Scholar]
- 28. Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tsang SMH, Szeto GPY, Li LMK, Wong DCM, Yip MMP, Lee RYW. The effects of bending speed on the lumbo-pelvic kinematics and movement pattern during forward bending in people with and without low back pain. BMC Musculoskelet Disord. 2017;18:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Geisser M, Haig A, Wallbom A, Wiggert E. Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain. Clin J Pain. 2004;20:61–69. [DOI] [PubMed] [Google Scholar]
- 31. Dankaerts W, O’Sullivan P, Burnett A, Straker L, Davey P, Gupta R. Discriminating healthy controls and two clinical subgroups of nonspecific chronic low back pain patients using trunk muscle activation and lumbosacral kinematics of postures and movements. Spine (Phila Pa 1976). 2009;34:1610–1618. [DOI] [PubMed] [Google Scholar]
- 32. Rabey M, Smith A, Beales D, Slater H, O’Sullivan P. Pain provocation following sagittal plane repeated movements in people with chronic low back pain: associations with pain sensitivity and psychological profiles. Scand J Pain. 2017;16:22–28. [DOI] [PubMed] [Google Scholar]
- 33. Glombiewski JA, Riecke J, Holzapfel S et al. Do patients with chronic pain show autonomic arousal when confronted with feared movements? An experimental investigation of the fear–avoidance model. Pain. 2015;156:547–554. [DOI] [PubMed] [Google Scholar]
- 34. Karayannis NV, Smeets RJ, van den Hoorn W, Hodges PW. Fear of movement is related to trunk stiffness in low back pain. PLoS One 2013;8:e67779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Darlow B, Dean S, Perry M, Mathieson F, Baxter GD, Dowell A. Easy to harm, hard to heal. Spine (Phila Pa 1976). 2015;40:842–850. [DOI] [PubMed] [Google Scholar]
- 36. Van Ryckeghem DM, De Houwer J, Van Bockstaele B, Van Damme S, De Schryver M, Crombez G. Implicit associations between pain and self-schema in patients with chronic pain. Pain. 2013;154:2700–2706. [DOI] [PubMed] [Google Scholar]
- 37. Bunzli S, Smith A, Watkins R, Shütze R, O’Sullivan P. What do people who score highly on the Tampa Scale of kinesiophobia really believe?. Clin J Pain. 2015;31:621–632. [DOI] [PubMed] [Google Scholar]
- 38. Sullivan MJ, Thorn B, Haythornthwaite JA et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J P. 2001;17:52–64. [DOI] [PubMed] [Google Scholar]
- 39. de Moraes Vieira EB, de Goes Salvetti M, Damiani LP, de Mattos Pimenta CA. Self-efficacy and fear avoidance beliefs in chronic low back pain patients: coexistence and associated factors. Pain Manag Nurs. 2014;15:593–602. [DOI] [PubMed] [Google Scholar]
- 40. Darlow B, Fullen BM, Dean S, Hurley DA, Baxter G, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16:3–17. [DOI] [PubMed] [Google Scholar]
- 41. Bunzli S, Smith A, Schütze R, O’Sullivan P. Beliefs underlying pain-related fear and how they evolve: a qualitative investigation in people with chronic back pain and high pain-related fear. BMJ Open. 2015;5:e008847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O’Sullivan P, Straker L, Smith A, Perry M. Carer experience of back pain is associated with adolescent back pain experience even when controlling for other carer and family factors. Clin J Pain. 2008;42:226–231. [DOI] [PubMed] [Google Scholar]
- 43. Gatchel R, Peng Y, Peters M, Fuchs P, Turk D. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133:581–624. [DOI] [PubMed] [Google Scholar]
- 44. Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther. 2014;94:1816–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vlaeyen JW, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016;157:1588–1589. [DOI] [PubMed] [Google Scholar]
- 46. Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94 [DOI] [PubMed] [Google Scholar]
- 47. Andrews NE, Strong J, Meredith PJ. Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2012;93:2109–2121.e7. [DOI] [PubMed] [Google Scholar]
- 48. Hasenbring MI, Hallner D, Klasen B, Streitlein-Böhme I, Willburger R, Rusche H. Pain-related avoidance versus endurance in primary care patients with subacute back pain: psychological characteristics and outcome at a 6-month follow-up. Pain. 2012;153:211–217. [DOI] [PubMed] [Google Scholar]
- 49. Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine (Phila Pa 1976). 2000;25:2114–2125. [DOI] [PubMed] [Google Scholar]
- 50. McCracken LM. Social context and acceptance of chronic pain: the role of solicitous and punishing responses. Pain. 2005;113:155–159. [DOI] [PubMed] [Google Scholar]
- 51. Coggon D, Ntani G, Palmer KT et al. Disabling musculoskeletal pain in working populations: Is it the job, the person, or the culture? Pain. 2013;154:856–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Auvinen J, Tammelin T, Taimela S et al. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J. 2010;19:641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lusa S, Miranda H, Luukkonen R, Punakallio A. Sleep disturbances predict long-term changes in low back pain among Finnish firefighters: 13-year follow-up study. Int Arch Occup Environ Health. 2015;88:369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Miró E, Martínez MP, Sánchez AI, Prados G, Medina A. When is pain related to emotional distress and daily functioning in fibromyalgia syndrome? The mediating roles of self-efficacy and sleep quality. Br J Health Psychol. 2011;16:799–814. [DOI] [PubMed] [Google Scholar]
- 55. Heneweer H, Vanhees L, Picavet HSJ. Physical activity and low back pain: A U-shaped relation? Pain. 2009;143:21–25. [DOI] [PubMed] [Google Scholar]
- 56. Heuch I, Heuch I, Hagen K, Zwart JA. Is there a U-shaped relationship between physical activity in leisure time and risk of chronic low back pain? A follow-up in the HUNT Study. BMC Public Health. 2016;16:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dean E, Soderlund A. What is the role of lifestyle behaviour change associated with non-communicable disease risk in managing musculoskeletal health conditions with special reference to chronic pain? BMC Musculoskelet Disord. 2015;13:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. McVinnie DS. Obesity and pain. Br J Pain. 2013;7:163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res. 2015;8:399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123:87e7–87.e35. [DOI] [PubMed] [Google Scholar]
- 61. Hagen EM, Svensen E, Eriksen HR, Ihlebaek CM, Ursin H. Comorbid subjective health complaints in low back pain. Spine (Phila Pa 1976). 2006;31:1491–1495. [DOI] [PubMed] [Google Scholar]
- 62. Caneiro JP, Smith A, Rabey M, Moseley GL, O’Sullivan P. Process of change in pain-related fear: clinical insights from a single case report of persistent back pain managed with cognitive functional therapy. J Orthop Sports Phys Ther. 2017;47:637–651. [DOI] [PubMed] [Google Scholar]
- 63. Vibe Fersum K, O’Sullivan P, Skouen JS, Smith A, Kvåle A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: a randomized controlled trial. Eur J Pain. 2013;17:916–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. O’Sullivan K, Dankaerts W, O’Sullivan L, O’Sullivan P. Cognitive functional therapy for disabling nonspecific chronic low back pain: multiple case-cohort study. Phys Ther. 2015;95:1478–1488. [DOI] [PubMed] [Google Scholar]
- 65. Bunzli S, Smith A, Schütze R, Lin I, O’Sullivan P. Making sense of low back pain and pain-related fear. J Orthop Sports Phys Ther. 2017;47:628–636. [DOI] [PubMed] [Google Scholar]
- 66. O’Keeffe M, Cullinane P, Hurley J et al. What influences patient-therapist interactions in musculoskeletal physical therapy? Qualitative systematic review and meta-synthesis. Phys Ther. 2016;96:609–622. [DOI] [PubMed] [Google Scholar]
- 67. Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of The Örebro Musculoskeletal Pain Questionnaire. Clin J Pain. 2003;19:80–86. [DOI] [PubMed] [Google Scholar]
- 68. O’Sullivan P, Lin I. Acute low back pain: beyond physical therapies. Pain Management Today. 2014;1:8–13. [Google Scholar]
- 69. McCullough BJ, Johnson GR, Martin BI, Jarvik JG. Lumbar MR imaging and reporting epidemiology: do epidemiologic data in reports affect clinical management? Radiology. 2012;262:941–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. O’Sullivan P. Back Pain—Separating Fact From Fiction. YouTube video. Available at: youtube.com/watch?v=Nj6Ik5UuomI. Accessed January 30, 2018. [Google Scholar]
- 71. O’Keefe M, O’Sullivan K, Griffin D. 15 Things You Didn’t Know About Low Back Pain. Irish Independent. https://painhealth.csse.uwa.edu.au/wp-content/uploads/2016/04/15-things-you-didnt-know-about-back-pain-2015.pdf. Published July 13, 2015. Accessed February 5, 2018. [Google Scholar]
- 72. Pain-Ed : http://www.pain-ed.com/public/patient-stories-2/. Accessed January 30, 2018. [Google Scholar]
- 73. O’Keeffe M, Maher CG, O’Sullivan K. Unlocking the potential of physical activity for back health. Br J Sports Med. 2017;51:760–761. [DOI] [PubMed] [Google Scholar]
- 74. Hayden JA, Van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–785. [DOI] [PubMed] [Google Scholar]
- 75. Fersum K, O’Sullivan P, Kvåle A, Skouen J. Inter-examiner reliability of a classification system for patients with non-specific low back pain. Man Ther. 2009;14:555–561. [DOI] [PubMed] [Google Scholar]
- 76. Dankaerts W, O’Sullivan P, Straker L, Burnett A, Skouen J. The inter-examiner reliability of a classification method for non-specific chronic low back pain patients with motor control impairment. Man Ther. 2006;11:28–39. [DOI] [PubMed] [Google Scholar]
- 77. O’Keeffe M, Purtill H, Kennedy N et al. Individualised cognitive functional therapy compared with a combined exercise and pain education class for patients with non-specific chronic low back pain: study protocol for a multicentre randomised controlled trial. BMJ Open. 2015;5:e007156–e007156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bunzli S, McEvoy S, Dankaerts W, O’Sullivan P, O’Sullivan K. Patient perspectives on participation in cognitive functional therapy for chronic low back pain. Phys Ther. 2016;96:1397–1407. [DOI] [PubMed] [Google Scholar]
- 79. Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, O’Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015;61:68–76. [DOI] [PubMed] [Google Scholar]
- 80. Synnott A, O’Keeffe M, Bunzli S et al. Physiotherapists report improved understanding of and attitude toward the cognitive, psychological and social dimensions of chronic low back pain after cognitive functional therapy training: a qualitative study. J Physiother. 2016;62:215–221. [DOI] [PubMed] [Google Scholar]