Abstract
Background
The incidence and prevalence of diabetes is increasing worldwide and it is the fifth leading cause of mortality accounting for over 3.8 million deaths annually. Despite the enormity of the diabetes-related health burdens, very few studies have evaluated the factors associated with mortality among people with diabetes in India. We sought to study the causes and predictors of mortality among urban Asian Indians with and without diabetes.
Methods and findings
Of 2273 adults (27,850 person-years of follow-up) from the 10-year follow-up of the Chennai Urban Rural Epidemiology Study (CURES), the cause of death could be ascertained in 552 individuals out of the 671 who had died (response rate 82.3%). Verbal autopsy was obtained from the family members of the deceased and this was adjudicated by trained physicians. The age-standardized mortality rate was 28.2 (95%CI 25.9–30.6) per 100,000 population. Mortality rates were significantly higher in individuals with diabetes compared to those without [27.9(95% CI 25.5–30.6) vs. 8.0 (6.6–9.9) per 1000 person years]. Compared to individuals of normal body mass index, underweight individuals had higher risk of mortality (Hazard ratio 1.49; 95% CI 1.11–2.0), whereas overweight and obese individuals did not show a higher risk. The population-attributable risk for all-cause mortality in the entire study cohort was highest for ischemic heart disease and diabetes. The excess mortality attributable to diabetes was highest in the age group of 51 to 70 years, and was mostly accounted for by renal disease (Rate ratio 5.68, 95%CI 2.43–6.23), ischemic heart disease (4.23,2.78–6.67), and cerebrovascular disease (4.00,1.87–9.81).
Conclusion
Underweight (but not overweight or obesity) was strongly associated with mortality in this Asian Indian population. Ischemic heart disease and diabetes contributed the most to risk for all cause mortality. Excess mortality due to diabetes was higher in relatively younger individuals and was mostly accounted for by renal disease.
Introduction
The incidence and prevalence of diabetes is increasing worldwide, with the prevalence estimated to almost double by 2030 [1]. Diabetes is the fifth leading cause of mortality accounting for over 3.8 million deaths annually [2]. It has been estimated that one individual dies of diabetes or its complications every 10 seconds. Most of the excess mortality due to diabetes is attributable to cardiovascular disease (CVD) and renal failure [3]. Individuals with diabetes have an increased risk of all-cause mortality and morbidity related to CVD compared with individuals without diabetes [4–5].
South Asia is one of the epicenters of the diabetes pandemic. Asian Indians with diabetes have been shown to have higher mortality rates compared to other ethnic groups [6]. Despite the enormity of the diabetes-related health burdens, very few studies have evaluated the factors associated with mortality among people with diabetes in India.
In the present study, we attempt to estimate the mortality rates, the causes of death among individuals with and without diabetes, the excess risk of death associated with diabetes and also the population attributable risk (PAR) for death associated with various modifiable risk factors in the follow-up cohort of a large epidemiological survey, conducted on a representative population of Chennai, the largest city in South India.
Research design and methods
Baseline studies
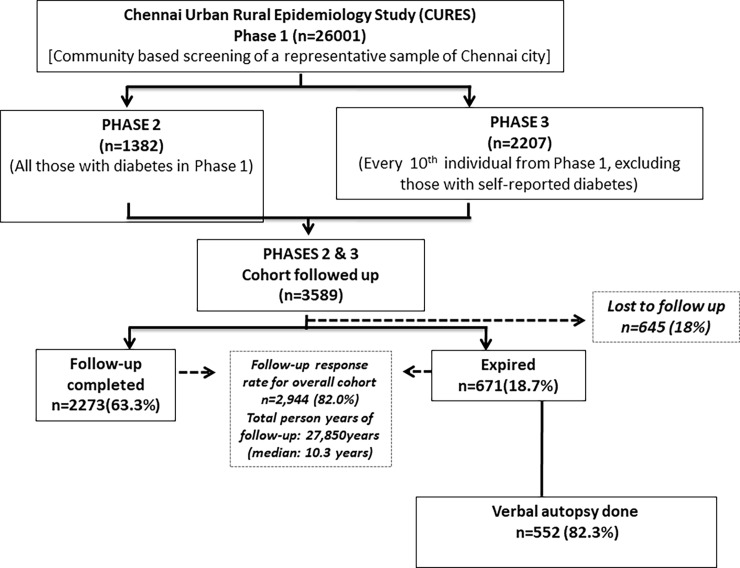
The present paper reports on the mortality rates in the 10-year follow-up of the Chennai Urban Rural Epidemiology Study (CURES) cohort. The methodology of CURES has been published elsewhere [7]. In brief, CURES was done on a representative sample of 26001 adults from Chennai city, aged ≥20 years. In the baseline survey carried out between 2001 and 2003, all 26001 individuals were screened for diabetes. Of these, all individuals who had diabetes (n = 1382) and one in every tenth individual (n = 2207) underwent further detailed anthropometric and biochemical investigations and these constituted the cohort for this follow-up study (n = 3589) [8] [Fig 1]. Madras Diabetes Research Foundation Institutional Ethics Committee approval was obtained, and written informed consent to use anonymized medical data was obtained from all study subjects before the start of the study. There were no minors in the study.
Fig 1. Flow chart of the study cohort.
Anthropometric and biochemical assessment
At baseline, details pertaining to demography, medical history, family history, tobacco and alcohol use and physical activity were elicited using a structured, pretested and validated interviewer-administered questionnaire. Smokers were defined as those who were currently smoking and alcohol use was defined as current alcohol consumption. Anthropometric details (such as height, weight, waist circumference, hip circumference) and blood pressure were measured using standardized techniques and body-mass index (BMI) calculated as weight in kilograms divided by height in meters squared. A venous blood sample was drawn in the fasting state and 2 hours after oral administration of 75 g of glucose in all individuals who did not give a history of diabetes. Biochemical analyses were done in a laboratory certified by the National Accreditation Board for testing and calibration Laboratories (NABL) and the College of American Pathologists (CAP) on a Hitachi—912 Autoanalyser (Hitachi, Germany) using kits supplied by Roche Diagnostics (Basel, Switzerland), for estimation of plasma glucose (GOD-POD method), serum cholesterol (CHODPAP method), serum triglycerides (GPO-PAP method) and HDL cholesterol (direct method). Glycated hemoglobin (HbA1C) was estimated by high pressure liquid chromatography using the Variant machine (Bio-Rad, Hercules, Calif., USA). The intra and inter-observer coefficients of variation for the biochemical assays ranged from 3.1 to 7.6%.
Definitions
Diabetes was diagnosed, if the venous plasma glucose 2 hours after oral glucose load (2-hr plasma glucose [2Hr PG]) was ≥200 mg/dl (11·1 mmol/l) and/or the fasting plasma glucose (FPG) levels were ≥126 mg/dl (7·0 mmol/l) [9]
Underweight was defined as a BMI <18.5 kg/m2 for both genders (based on the Asia Pacific Guidelines and World Health Organisation criteria) [10,11].
Overweight was defined as a BMI ≥23 but <25 kg /m2 (based on the Asia Pacific Guidelines) and ≥ 25 but < 30 kg /m2 for both genders (based on the WHO criteria) [10, 11].
Obesity was defined as a BMI ≥ 25 kg/m2(Asia Pacific Guidelines) and >30 kg/m2 (WHO criteria) for both genders [10,11].
Grade I obesity was defined as a BMI ≥ 25 but < 30 kg/m2 (Asia Pacific Guidelines) and ≥ 30 but < 35 kg/m2 (WHO criteria) [10, 11].
Grade II obesity was defined as a BMI >30 kg/m2 (Asia Pacific Guidelines) and >35 kg/m2 (WHO criteria) [10, 11].
Excess mortality was defined according to the World Health Organization criteria in which excess mortality can be expressed as a mortality rate, which is the risk of dying from that condition in a specific population “or” a total number of excess deaths [12].
Assessment of diabetes complications, including retinopathy, microalbuminuria, macroalbuminuria, neuropathy, peripheral vascular disease (PVD) and coronary artery disease (CAD), was performed as described below.
Retinopathy
A comprehensive ocular examination was performed and visual acuity was recorded using an illuminated Snellen chart. A detailed retinal (fundus) examination using direct and indirect ophthalmoscopy was performed by a retinal specialist trained in grading of retinal lesions. Retinal (fundus) photography was performed using four-field stereo color retinal photography (model FF 450 Pluscamera; Carl Zeiss, Jena, Switzerland) whenever possible. An Early Treatment Diabetic Retinopathy Study grading system that has been modified and standardized in other population-based studies was used for the diagnosis of diabetic retinopathy [13].
Nephropathy
Urinary albumin concentration was measured in a fasting urine sample using an immunoturbidometric assay (Hitachi 902 autoanalyzer; Roche Diagnostics). Microalbuminuria was diagnosed if the albumin excretion was between 30 and 299 g/mg creatinine. Macroalbuminuria was diagnosed if albumin excretion was ≥300 g/ mg creatinine. Nephropathy was defined as presence of either micro- or macroalbuminuria [14]
Neuropathy
Neuropathy was assessed using a biothesiometer. Vibratory perception threshold of the great toes was measured in a standardized manner by a single observer, and neuropathy was diagnosed if the mean vibratory perception threshold was ≥20 V [15].
Peripheral vascular disease
PVD was diagnosed by measurement of ankle-brachial pressure index (ABPI) using a Doppler probe. Blood pressure recordings were made of the brachial pulses in the upper limb. Similar recordings were made of the dorsalis pedis and posterior tibial pulses in the lower limb by inflating the cuff proximal to the ankle, and the mean of these two readings was taken as the ankle pressure. ABPI <0.9 was considered diagnostic of PVD [16].
Coronary artery disease
CAD was diagnosed based on a documented past history of myocardial infarction or drug treatment for coronary artery disease and/or Minnesota codes 1-1-1 to 1-1-7, [Q wave changes] 4–1 to 4–2 [ST segment depression] or 5–1 to 5–3 [T wave abnormalities] on the ECG [17].
Follow up data on mortality
The follow-up survey was done in 2012–2014 after a median of 10.3years (27,850 person-years of follow-up). Out of 3589 individuals in the follow-up cohort, 645 individuals were lost to follow-up (18%). This included 636 individuals who had migrated and were not traceable and 9 who refused to participate even after repeated attempts. It was found that 671 individuals had died, in 552 of whom (82.3%) the cause of death could be ascertained. Information on death was obtained from the study participant’s family members. The cause of death was ascertained through medical records, death certificates or discharge summaries from hospitals. Verbal autopsy was used for estimating cause specific mortality in cases without medical death certification. Data on symptoms reported by caregivers along with the cause of death were collected from a medical facility, and the cause-of-death distribution was estimated in the population where only symptom data were available. These documents were adjudicated by trained physicians.
Deaths in the cohort that occurred between 2001 and 2014 were recorded. The primary endpoint for this study was mortality from all causes, CVD, renal failure, cancer and other causes. Causes of death were coded as ischemic heart disease, renal failure, cerebrovascular disease, diabetes, cancer, chronic obstructive lung disease, liver failure, circulatory system diseases, tuberculosis, congestive heart failure, accident/suicide and unspecified causes of death according to the International Classification of Diseases, Tenth Revision (ICD-10).
Statistical analyses
Mortality rates were calculated by dividing number of deaths by total person-years observed. Person-years were calculated from the baseline examination until the event (death) occurred. Standardized mortality rates were calculated by dividing sum of products (age specific rate per 100,000 population X weight in the standard population.) across all age groups by sum of weight in standard population (World Health Organization) [18] for persons ≥ 20 years. Statistical analysis was carried out using the SPSS PC Windows version 15.0 [Chicago, IL]. Students “t” test was used to compare means and Chi Square or Fischer’s exact test to compare proportions.
To assess risk for all cause mortality, cox proportional hazard model was used. The variables which were found to be significant when taken individually in the model were considered in the multiple cox proportional hazard model for estimating the hazard ratio and 95% confidence intervals.
Partial PAR and 95% confidence intervals for single modifiable factors adjusted for confounders were estimated for the overall cohort using the method described by Spiegelman [19]. PAR is said to be partial when one or more risk factors are considered to be eliminated while others are allowed to remain unchanged. In our analysis, the fixed factors included age and gender. The following formula [17] was used to calculate the PARp.
In the formula mentioned above, t denotes a stratum of distinct combinations of levels of all background risk factor (t = 1, 2, 3,…,T) that are not considered in the study whereas s indicates an index exposure group defined by each of the unique combinations of the levels of the index risk factors for which the PARp applies (s = 1,2, 3,…,S). RR1s is the relative risk analogous to combinations relative to the lowest risk combination, RR1,1 = 1. The combined prevalence of exposure group s and stratum t is designated by Pst and pst and [19].
Results
The overall all-cause mortality rate was 19.8per 1000 person years [95% Confidence Interval (CI) 18.2–21.5].The age standardized mortality rate was 28.2 (95%CI 25.9–30.6.) per 100,000 population. The death rate was significantly higher among individuals with diabetes compared to those without [27.9 (95% CI 25.5–30.6) vs 8.0 (95% CI 6.6–9.9) per 1000 person years].
The clinical and biochemical parameters of the study population with and without diabetes is shown in Table 1. [both those who were alive at the time of follow up (n = 2276) and those who were deceased (n = 552)]. The mean age at time of death did not differ significantly between individuals with and without diabetes (65.0±11.2 vs. 66.1±16.5 years respectively). Among individuals with diabetes, significantly more females than males died. Baseline BMI, waist circumference, fasting plasma glucose, HbA1c, serum cholesterol and serum triglycerides were significantly higher among deceased individuals with diabetes compared to those without (p<0.001 for all parameters). The mean duration of diabetes at the time of death was 10.7 ± 6.6 years. Smoking and alcohol consumption were significantly more frequent among deceased individuals without diabetes than those with diabetes. Among those who were alive at follow-up, mean age at the time of follow-up, blood pressure. BMI, waist circumference, fasting plasma glucose, HbA1c, serum cholesterol and serum triglyceride levels were significantly higher among those with diabetes. Prevalence of abdominal obesity, hypercholesterolemia and hypertriglyceridemia were higher among both deceased and alive individuals with diabetes compared to those without.
Table 1. Baseline characteristics of subjects with and without diabetes among the study cohort.
| Variables | Deceased | Alive | ||||
|---|---|---|---|---|---|---|
| Individuals without diabetes (n = 92) | Individuals with diabetes (n = 460) | p value | Individuals without diabetes (n = 1032) | Individuals with diabetes (n = 1244) | p value | |
| Age at the time of death (years) | 66.1 ± 16.5 | 65.0 ± 11.2 | 0.56 | – | – | – |
| Age at the time of follow up (years) | – | – | – | 46.6 ± 12.0 | 55.7 ± 10.8 | <0.001 |
| Gender (male) n (%) | 54 (58.7) | 205 (44.6) | 0.03 | 437 (42.3) | 531 (42.7) | 0.87 |
| Duration of diabetes at the time of death (years) | – | 10.7 ± 6.6 | – | – | – | – |
| Duration of diabetes at the time of follow up (years) | – | – | – | – | 8.9 ± 6.4 | – |
| Systolic blood pressure (mm/Hg) | 130 ± 25 | 133 ± 23 | 0.22 | 117 ± 17 | 126 ± 20 | <0.001 |
| Diastolic blood pressure (mm/Hg) | 78 ± 12 | 77 ± 12 | 0.32 | 73 ± 11 | 77 ± 11 | <0.001 |
| Body mass index(kg/m2) | 21.6 ± 4.3 | 24 ± 4.6 | <0.001 | 23.5 ± 4.7 | 25.6 ± 4.2 | <0.001 |
| Waist circumference (cm) | 82.0 ± 11.3 | 87.9 ± 11.4 | <0.001 | 83.0 ± 12.2 | 90.6 ± 10.0 | <0.001 |
| Fasting blood glucose (mg/dl) | 86 ± 8 | 177 ± 88 | <0.001 | 84 ± 8 | 135 ± 59 | <0.001 |
| Glycated haemoglobin (%) | 5.7 ± 0.4 | 9.1 ± 2.6 | <0.001 | 5.5 ± 0.5 | 7.7 ± 2.1 | <0.001 |
| Serum cholesterol (mg/dl) | 184 ± 37 | 205 ± 46 | <0.001 | 175.8 ± 37.7 | 195 ± 38 | <0.001 |
| Serum triglyceride* (mg/dl) | 105.5 | 154.3 | <0.001 | 99.5 | 144.5 | <0.001 |
| Smoking (yes) n(%) | 29 (33.0) | 90 (20.0) | 0.01 | 165 (16.0) | 193 (15.5) | 0.76 |
| Alcohol (yes) n(%) | 27 (30.3) | 88 (19.6) | 0.02 | 210 (20.3) | 237 (19.1) | 0.44 |
| Risk Factors | ||||||
| Physical inactivity n(%) | 78 (87.6) | 395 (88.0) | 0.930 | 846 (82.0) | 1031 (82.9) | 0.57 |
| Abdominal obesity n(%) | 490 (47.6) | 916 (74.2) | <0.001 | 34 (37.4) | 279 (61.7) | <0.001 |
| Hypertension n(%) | 140 (13.6) | 355 (28.6) | <0.001 | 30 (32.6) | 190 (41.4) | 0.12 |
| Hypercholesterolemia n(%) | 232 (22.5) | 527 (42.4) | <0.001 | 25 (27.2) | 243 (53.2) | <0.001 |
| Hypertriglyceridemia n(%) | 188 (18.2) | 558 (44.9) | <0.001 | 14 (15.2) | 234 (51.3) | <0.001 |
* Geometric mean; data are mean ± SD.
The most frequent causes of mortality among individuals with diabetes were ischemic heart disease [34.3%], renal failure [10.7%] and cerebrovascular disease [10%], while among individuals without diabetes, ischemic heart disease [28.3%], circulatory disease [9.8%] and chronic obstructive lung disease [9.8%], were the most frequently cited causes of death. There were no significant differences in the frequency of various causes of death between the two groups, except for suicide, which was more frequent in individuals without diabetes (Table 2).
Table 2. Causes of death in those with and without diabetes.
| Causes of death (With ICD codes) |
Individuals without diabetes n (%) | Individuals with diabetes n (%) |
p value |
|---|---|---|---|
| Ischemic heart disease (I 20—I 52) | 26 (28.3) | 158 (34.3) | 0.26 |
| Renal failure (N 17-N 19) | 6 (6.5) | 49 (10.7) | 0.23 |
| Diabetes (E 10—E 14) | 0 | 43 (9.3) | <0.001 |
| Cancer (C 00—C 96) | 7 (7.6) | 35 (7.6) | 1.00 |
| Circulatory disease (I 00—I 99) | 9 (9.8) | 33 (7.2) | 0.39 |
| Chronic obstructive lung disease(J40-J47) | 9 (9.8) | 27 (5.9) | 0.16 |
| Chronic liver disease (K 70-K 77) | 3 (3.3) | 13 (2.8) | 0.74 |
| Tuberculosis (A 15—A19) | 3 (3.3) | 9 (2.0) | 0.43 |
| Congestive heart failure (I 50) | 4 (4.3) | 6 (1.3) | 0.05 |
| Others–accident (W 00—W 19) | 7 (7.6) | 16 (3.5) | 0.07 |
| Others–suicide (X 60 -X 84) | 8 (8.7) | 6 (1.3) | <0.001 |
| Unspecified causes of death(R 45—R 99) | 2 (2.2) | 19 (4.1) | 0.55 |
Table 3 shows the hazard ratios (HR) associated with various risk factors for all-cause mortality in the overall study cohort. Increasing age [HR1.008, 95% CI 1.007–1.009, p<0.001], smoking [HR 1.338, 95% CI 1.009–1.775, p = 0.04] and higher glycated hemoglobin [HR 1.264, 95% CI 1.223–1.306, p<0.001] were all independent risk factors for all-cause mortality in this cohort. Among individuals with diabetes, additionally gender, abdominal obesity (Table 4) and presence of any three or above chronic complications was associated with an increased risk of mortality. When the HR between groups were compared, only gender, smoking and alcohol were found to be significant with an interaction test p value < 0.05.
Table 3. Hazard ratios of various risk factors for all-cause mortality in the overall study cohort.
| Variables | Hazard Ratio (95%CI) | P value |
|---|---|---|
| Age (years) | 1.008 (1.007–1.009) | <0.001 |
| Gender (Male) | 0.804 (0.644–1.004) | 0.05 |
| Hypertension(≥140/90 mmHg or using drug treatment) | 1.199 (0.995–1.444) | 0.06 |
| Hypercholesterolemia(≥200 mg/dL) | 1.111 (0.923–1.338) | 0.26 |
| Hypertriglyceridemia (≥150mg/dL) | 1.142 (0.946–1.377) | 0.17 |
| Smoking (Yes) | 1.338 (1.009–1.775) | 0.04 |
| Alcohol (Yes) | 1.154 (0.870–1.531) | 0.32 |
| HbA1c (%) | 1.264 (1.223–1.306) | <0.001 |
Table 4. Hazard ratios of various risk factors for all-cause mortality among subjects with and without diabetes.
| Individuals with diabetes | Individuals without diabetes | |||
|---|---|---|---|---|
| Variables | Hazard ratio | p value | Hazard ratio | p value |
| (95% CI) | (95% CI) | |||
| Age (years) | 1.008 (1.007–1.009) | <0.001 | 1.010 (1.008–1.012) | <0.001 |
| Gender (Male) | 0.709 (0.550–0.913) | 0.008 | 1.037 (0.587–1.831) | 0.9 |
| Hypertension | 1.181 (0.968–1.442) | 0.102 | 1.089 (0.656–1.807) | 0.741 |
| (≥140/90 mmHg or using drug treatment) | ||||
| Physical inactivity | 0.990 (0.740–1.324) | 0.945 | 0.541 (0.283–1.036) | 0.064 |
| Abdominal obesity | 0.607 (0.491–0.751) | <0.001 | 0.629 (0.388–1.020) | 0.06 |
| HbA1c %) | 1.023 (1.018–1.029) | <0.001 | 1.346 (0.836–2.167) | 0.221 |
| Hypercholesterolemia | 1.155 (0.946–1.411) | 0.156 | 0.807 (0.472–1.380) | 0.433 |
| (≥200 mg/dL) | ||||
| Hypertriglyceridemia | 1.112 (0.911–1.357) | 0.297 | 0.718 (0.378–1.365) | 0.312 |
| (≥150 mg/dL) | ||||
| Smoking (Yes) | 1.232 (0.900–1.687) | 0.194 | 1.898 (0.957–3.766) | 0.067 |
| Alcohol (Yes) | 1.107 (0.807–1.518) | 0.53 | 1.357 (0.687–2.679) | 0.38 |
| Complications*¤ in those with diabetes | ||||
| Any one complication | 1.123 (0.857–1.471) | 0.4 | ||
| Any two complications | 1.106 (0.827–1.479) | 0.498 | ||
| Any three complications | 2.236 (1.615–3.094) | <0.001 | ||
| All four complications | 2.605 (1.516–4.475) | <0.001 | ||
*¤Adjusted for age and gender
¤Complications include—retinopathy, nephropathy, neuropathy, peripheral vascular disease and coronary artery disease.
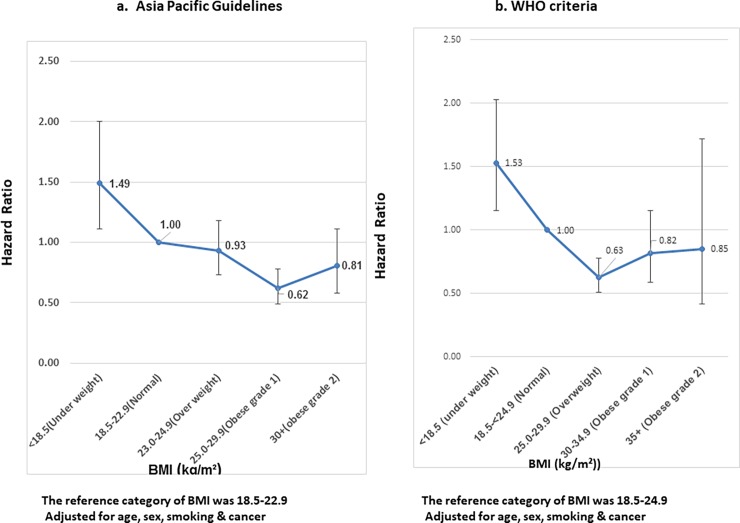
Fig 2 show the adjusted hazard ratios for all-cause mortality based on BMI categories (as defined by the Asia Pacific guidelines and WHO criteria) in the overall study population. The risk of death from any cause was higher among individuals with lower-than-normal BMI. Compared to individuals with normal BMI, individuals defined as underweight had a hazard ratio for mortality of 1.49 (95% CI 1.11–2.0) (when the Asia Pacific guidelines were used) and 1.53 (95% CI 1.15–2.03) (based on the WHO criteria). Overweight and obesity were not associated with higher hazard of mortality. The magnitude of the association was similar between the guidelines and was not altered by adjustment for age, gender, cancer and smoking status When split by disease status i.e. diabetes and no diabetes this trend did not change significantly.
Fig 2. Hazard ratios for all-cause mortality based on BMI.
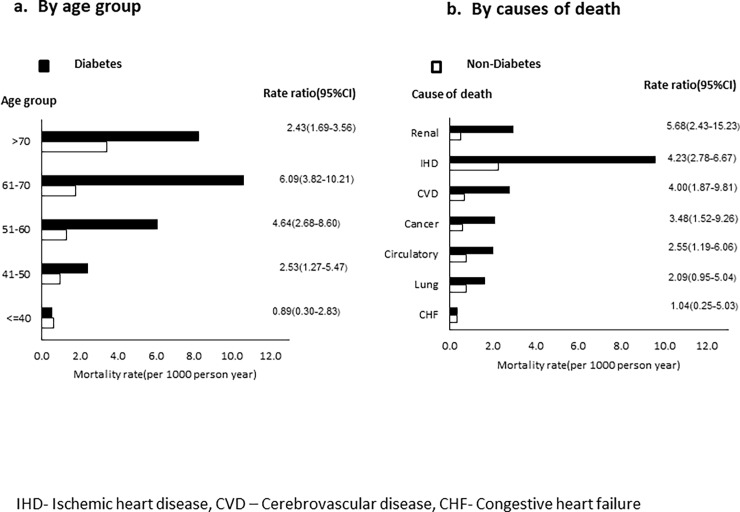
Excess mortality among individuals with diabetes was highest in the age group of 61–70 years (rate ratio 6.09, 95% CI 3.82–10.21) followed by 51–60 years (4.64, 2.68–8.60) (Fig 3). Among the various causes of death, excess mortality among individuals with diabetes was highest for renal disease (rate ratio 5.68, 95% CI 2.43–16.23), followed by ischemic heart disease (4.23, 2.78–6.67) and cerebrovascular disease (4.00, 1.87–9.81)
Fig 3. Excess mortality among individuals with and without diabetes.
Table 5 shows the individual contributions of various modifiable risk factors to the PAR for all cause mortality in the overall study population. Among the modifiable risk factors, physical inactivity was found to contribute most to mortality [PARp 24.7%(4.7–42.8)], followed by hypercholesterolemia, hypertriglyceridemia, smoking, alcohol and least by hypertension [4.1% (7.1–15.2)]. Ischemic heart disease was found to contribute the most to mortality [PARp 53%, (95% CI 25.6–72.5)] followed by diabetes [50.3%, (36.8–61.8)], renal failure [23.6% (4.3–41.1)] and cerebrovascular disease [13.9%(3.4–30.3)].
Table 5. Partial population attributable risk for all-cause mortality in the study cohort.
| Risk Factors | Adjusted PAR(Partial)* |
|---|---|
| Physical inactivity | 24.7(4.7–42.8) |
| Hypercholesterolemia | 11.9 (2.5–2.1) |
| Hypertriglyceridemia | 11.8 (4.3–19.2) |
| Smoking | 10.2 (2.2–1.8) |
| Alcohol | 9.1 (7.6–10.7) |
| Hypertension | 4.1 (7.1–15.2) |
| Causes of Death | |
| Ischaemic heart disease | 53.0 (25.6–72.5) |
| Diabetes | 50.3 (36.8–61.8) |
| Renal failure | 23.6 (4.3–41.1) |
| Cerebrovascular disease | 13.9 (-3.4–30.3) |
| Congestive heart failure | 4.8 (-10.9–20.2) |
Discussion
To our knowledge, this is the first study from India to compare mortality rates in a representative cohort of individuals with and without diabetes, and to assess the effects of various modifiable risk factors on all-cause mortality. The major findings are as follows: (i) mortality rates are more than three times higher in individuals with diabetes compared to those without diabetes; (ii) underweight was associated with a significantly higher risk of all-cause mortality in the overall study cohort, whereas overweight and obesity were not; (iii) excess mortality due to diabetes was most marked in the age group of 51–70 years; and (iv) most of the excess mortality due to diabetes was accounted for by renal disease, ischemic heart disease and cerebrovascular disease.
While several prospective studies have documented increased mortality associated with diabetes [20–21], earlier studies from India do not provide information on death rates in the general population for comparison [22]. In this study, we report that the mortality rate was almost thrice as high in individuals with diabetes compared to those without (27.9 vs 8.0 per 1000 person-years). This figure is comparable with the results of a previous small study done by our group a decade ago in two selected residential colonies in Chennai, in which the mortality rates were found to be18.9and 5.3 per 1000 person-years among persons with and without diabetes respectively [23]. Studies from China have also shown that individuals with diabetes have a threefold higher death rate compared to age-matched controls without diabetes [24]. Studies from the United Kingdom [25–26],Germany [27], the United States [28], Brazil [29] and Australia [30] have shown that individuals with type 2 diabetes have a 1.5–2.5 fold higher risk of mortality compared to those without diabetes depending on the age of the patients studied.
Our results show excess mortality among underweight individuals (but not those who are overweight or obese) in comparison with individuals of normal weight in the overall study population, even after adjusting for age, gender, smoking and cancer. Previous studies and meta-analyses have shown a J or U-shaped relationship between BMI and mortality, such that both underweight and obesity are associated with excess mortality when compared to normal BMI [31–33]. While the paucity of individuals with higher grades of obesity in our study could have skewed our findings, it is also possible that being underweight confers a greater risk of mortality than expected in this population that is likely to have been exposed to chronic undernutrition and its attendant consequences such as infectious diseases and micronutrient deficiency in childhood and youth or even intrauterine growth retardation.
The present paper reports, for the first time, the relative contributions of various individual modifiable risk factors to all-cause mortality. Ischemic heart disease, which contributes 53% to the risk of mortality, is an eminently modifiable risk factor; it has been shown that more than 90% of all cases of acute myocardial infarction can be prevented by favorably modifying nine risk factors [34]. Diabetes, which is an equally significant contributor to the PAR, can also be prevented, or its onset significantly delayed, as has been shown by several large prospective studies [35]. Other important contributors to mortality such as physical inactivity, dyslipidemia, smoking and alcohol use and hypertension are also easily modifiable. Identification and modification of these risk factors will help reduce overall mortality and more importantly, prevent premature mortality in this population.
In the present study, excess mortality due to diabetes was highest in the age group of 51 to 70 years. This is possibly a reflection of the earlier age of onset of diabetes in this South Asian population, whereby patients develop diabetes in the fourth or fifth decade of life, and develop complications and are at risk of dying by the sixth or seventh decade. This has significant implications in that these age groups represent the apex of productive life in many occupations, and illness and death occurring at this time will therefore have a profound impact on the family, society and nation.
Renal failure contributed the most to excess mortality among individuals with diabetes, although it was overall cited as the second most common cause of death in this group, accounting for 10.7% of deaths. Globally, diabetes is the most important risk factor associated with death from renal failure among adults at all ages, and is now the most frequently occurring comorbidity among individuals with renal failure. Studies from different parts of the developed world have shown that declining renal function (indicated by increasing levels of albuminuria or by decreasing glomerular filtration rate) is a strong predictor of all-cause and cardiovascular mortality among individuals with diabetes [36–37]. Indeed, the NHANES data suggests that kidney disease is responsible for the excess mortality found among US adults with diabetes as compared to the general population [38]. Similarly, a study of 150,000 individuals from Mexico showed that renal disease accounted for the largest absolute excess of deaths due to diabetes [39].
CVD was also found to contribute significantly to excess mortality in individuals with diabetes. Globally, coronary artery disease is the leading cause of death and is predicted to remain so for the next 20 years [40–41]. Diabetes mellitus continues to be associated with an approximately 2 to 3 fold increased risk of CVD mortality [42], in spite of advances in diabetes management and preventive cardiology. There is a huge unmet need for therapeutic approaches to ensure global risk reduction so as to prevent premature death due to CVD in this population.
The strengths of our study are the representativeness of the sample and long duration of follow-up, use of standardized verbal autopsies to collect information on death from the community and a good response rate (82%). Ours is the first study to compare mortality rates among Asian Indians with and without diabetes, as also to evaluate the causes and characteristics of excess mortality in Asian Indians with diabetes, and the modifiable risk factors contributing to the PAR for death. The main limitation of the study is that we were unable to collect information on cause of death from those individuals who were ascertained to have died, but whose relatives were not traceable.
In conclusion, the age standardized mortality rate among urban Asian Indians in Chennai was 28.2 per 100, 000 population. Individuals with diabetes had three times higher mortality rates compared to those without. Renal disease, ischemic heart disease, and cerebrovascular disease accounted for most of the excess mortality due to diabetes which was most marked in the age group of 51–70 years. We have also shown that underweight (but not overweight or obesity) was associated with an increased risk of mortality in the overall study cohort. Favorably altering risk factors through increased physical activity, smoking cessation, good glycemic control, blood pressure control and lipid-lowering therapy, and preventing or delaying the onset of diabetes by means of lifestyle modification and judicious use of medications, could help to significantly reduce mortality and prevent premature deaths in this population.
Supporting information
(XLS)
Acknowledgments
The authors thank the staff of Dr. Mohan’s Diabetes Specialities Centre, Chennai and the epidemiology team of the Madras Diabetes Research Foundation for the field work and all the participants who took part in the study. This is the 150th paper from the CURES study (CURES-150).
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The authors received no funding for this work.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004. May; 27(5):1047–53. [DOI] [PubMed] [Google Scholar]
- 2.Yoon U, Kwok LL, Magkidis A. Efficacy of lifestyle interventions in reducing diabetes incidence in patients with impaired glucose tolerance: a systematic review of randomized controlled trials. Metabolism. 2013. February;62(2):303–14. doi: 10.1016/j.metabol.2012.07.009 [DOI] [PubMed] [Google Scholar]
- 3.Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005. September;28(9):2130–5. [DOI] [PubMed] [Google Scholar]
- 4.Ballotari P, Ranieri SC, Luberto F, Caroli S, Greci M, Giorgi Rossi P, et al. Sex differences in cardiovascular mortality in diabetics and nondiabetic subjects: a population-based study (Italy). Int J Endocrinol. 2015; 2015;2015:914057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preis SR, Hwang SJ, Coady S, Pencina MJ, D'Agostino RB Sr, Savage PJ, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009. April 7;119(13):1728–35. doi: 10.1161/CIRCULATIONAHA.108.829176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma S, Cutter J, Tan CE, Chew SK, Tai ES. Associations of diabetes mellitus and ethnicity with mortality in a multiethnic Asian population: data from the 1992 Singapore [DOI] [PubMed]
- 7.Deepa M, Pradeepa R, Rema M, Mohan A, Deepa R, Shanthirani S, et al. The Chennai Urban Rural Epidemiology Study (CURES)—study design and methodology urban component) (CURES-I). J Assoc Physicians India. 2003. September; 51:863–70. [PubMed] [Google Scholar]
- 8.Anjana RM, Shanthi Rani CS, Deepa M, Pradeepa R, Sudha V, DivyaNair,et al. Incidence of Diabetes and Prediabetes and Predictors of Progression Among Asian Indians:10-Year Follow-up of the Chennai Urban Rural Epidemiology Study (CURES). Diabetes Care. 2015. August;38(8):1441–8. doi: 10.2337/dc14-2814 [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33: S62–S69 doi: 10.2337/dc10-S062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Asia Pacific perspective: redefining obesity and its treatment. Regional Office for the Western Pacific (WPRO), World Health Organization. International Association for the Study of Obesity and the International Obesity Task Force St Leonards, Australia; Health Communications Australia Pty Limited; 2000. p. 22–9.
- 11.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. January 10;363(9403):157–63. Review. Erratum in: Lancet. 2004 Mar 13;363(9412):902 doi: 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 12.Lenner P. The excess mortality rate. A useful concept in cancer epidemiology. Acta Oncol. 1990; 29: 573–576. [DOI] [PubMed] [Google Scholar]
- 13.Rema M, Premkumar S, Anitha B, et al. Prevalence of diabetic retinopathy in urban India: the Chennai Urban Rural Epidemiology Study (CURES) eye study, I. Invest Ophthalmol Vis Sci 2005;46:2328–2333 doi: 10.1167/iovs.05-0019 [DOI] [PubMed] [Google Scholar]
- 14.Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: the Chennai Urban Rural Epidemiology Study (CURES 45). Diabetes Care.2007. August;30(8):2019–24. doi: 10.2337/dc06-2554 [DOI] [PubMed] [Google Scholar]
- 15.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: the Chennai Urban Rural Epidemiology Study (CURES-55). Diabet Med. 2008. April;25(4):407–12 doi: 10.1111/j.1464-5491.2008.02397.x [DOI] [PubMed] [Google Scholar]
- 16.Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: the Chennai Urban Population Study. Diabetes Care. 2000. September; 23(9):1295–300. [DOI] [PubMed] [Google Scholar]
- 17.Mohan V, Deepa R, Rani SS, Premalatha G; Chennai Urban Population Study (CUPS No.5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No. 5). J Am Coll Cardiol. 2001. September; 38(3):682–7. [DOI] [PubMed] [Google Scholar]
- 18.Ahmad O, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new WHO standard. Geneva, World Health Organization, 2001 [Google Scholar]
- 19.Spiegelman D, Hertzmark E, Wand HC. Point and interval estimates of partialpopulation attributable risks in cohort studies: examples and software. Cancer Causes Control. 2007. June;18(5):571–9. doi: 10.1007/s10552-006-0090-y [DOI] [PubMed] [Google Scholar]
- 20.Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971–1993. Diabetes Care. 1998. July;21(7):1138–45. [DOI] [PubMed] [Google Scholar]
- 21.Lowe LP, Liu K, Greenland P, Metzger BE, Dyer AR, Stamler J.et al. Diabetes, asymptomatic hyperglycemia, and 22-year mortality in black and white men.The Chicago Heart Association Detection Project in Industry Study. Diabetes Care.1997. February;20(2):163–9. [DOI] [PubMed] [Google Scholar]
- 22.Zargar AH, Wani AI, Masoodi SR, Laway BA, Bashir MI. Mortality in diabetes mellitus—data from a developing region of the world. Diabetes Res Clin Pract. 1999. January;43(1):67–74 [DOI] [PubMed] [Google Scholar]
- 23.Mohan V, Shanthirani CS, Deepa M, Deepa R, Unnikrishnan RI, Datta M. Mortality rates due to diabetes in a selected urban south Indian population—the Chennai Urban Population Study [CUPS—16]. J Assoc Physicians India. 2006. February; 54:113–7. [PubMed] [Google Scholar]
- 24.An Y, Zhang P, Wang J, Gong Q, Gregg EW, Yang W, et al. Cardiovascular and All-Cause Mortality Over a 23-Year Period Among Chinese With Newly Diagnosed Diabetes inthe Da Qing IGT and Diabetes Study. Diabetes Care. 2015. July;38(7):1365–71. doi: 10.2337/dc14-2498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA, et al. Mortality in people with type 2 diabetes in the UK. Diabet Med. 2006. May;23(5):516–21 doi: 10.1111/j.1464-5491.2006.01838.x [DOI] [PubMed] [Google Scholar]
- 26.Roper NA, Bilous RW, Kelly WF, et al. Excess mortality in a population with diabetes and the impact of material deprivation: longitudinal, population based study. BMJ 2001, 322:1389–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Panzram G, Zabel-Langhennig R: Prognosis of diabetes mellitus in a geographically defined population. Diabetologia 1981; 20:587–591 [DOI] [PubMed] [Google Scholar]
- 28.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men andwomen with diabetes, 1971 to 2000. Ann Intern Med. 2007. August 7;147(3):149–55. [DOI] [PubMed] [Google Scholar]
- 29.Salles GF, Bloch KV, Cardoso CR. Mortality and predictors of mortality in acohort of Brazilian type 2 diabetic patients. Diabetes Care. 2004. June; 27(6):1299–305. [DOI] [PubMed] [Google Scholar]
- 30.Knuiman MW, Welborn TA, Whittall DE: An analysis of excess mortality rates for persons with non-insulin-dependent diabetes mellitus in Western Australia using the Cox proportional hazards regression model. Am J Epidemiol1992;135:638–64 [DOI] [PubMed] [Google Scholar]
- 31.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005. April 20;293(15):1861–7. doi: 10.1001/jama.293.15.1861 [DOI] [PubMed] [Google Scholar]
- 32.Pednekar MS, Hakama M, Hebert JR, Gupta PC. Association of body mass indexwith all-cause and cause-specific mortality: findings from a prospective cohort study in Mumbai (Bombay), India. Int J Epidemiol. 2008. June;37(3):524–35 doi: 10.1093/ije/dyn001 [DOI] [PubMed] [Google Scholar]
- 33.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo Z, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011. February 24; 364(8):719–29. doi: 10.1056/NEJMoa1010679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. INTERHEART Study Investigators. Effect ofpotentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004. September11-17;364(9438):937–52. doi: 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 35.Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002; 25: 2165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bruno G, Merletti F, Bargero G, Novelli G, Melis D, Soddu A, et al. Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study. Diabetologia. 2007. May;50(5):941–8. doi: 10.1007/s00125-007-0616-1 [DOI] [PubMed] [Google Scholar]
- 37.Svensson MK, Cederholm J, Eliasson B, Zethelius B, Gudbjörnsdottir S; Swedish,et al. National Diabetes Register. Albuminuria and renal function as predictors of cardiovascular events and mortality in a general population of patients with type 2 diabetes: a nationwide observational study from the Swedish National Diabetes Register. Diab Vasc Dis Res. 2013. November; 10(6):520–9. doi: 10.1177/1479164113500798 [DOI] [PubMed] [Google Scholar]
- 38.Afkarian M, Sachs MC, Kestenbaum B, Hirsch IB, Tuttle KR, Himmelfarb J, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013. February;24(2):302–8. doi: 10.1681/ASN.2012070718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alegre-Díaz J, Herrington W, López-Cervantes M, Gnatiuc L, Ramirez R, Hill M, et al. Diabetes and Cause-Specific Mortality in Mexico City. N Engl J Med. 2016. November 17;375(20):1961–1971. doi: 10.1056/NEJMoa1605368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006. November;3(11):e442 doi: 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barr EL, Zimmet PZ, Welborn TA, Jolley D, Magliano DJ, Dunstan DW, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Circulation. 2007. July 10;116(2):151–7. doi: 10.1161/CIRCULATIONAHA.106.685628 [DOI] [PubMed] [Google Scholar]
- 42.Chen YY, Lin YJ, Chong E, Chen PC, Chao TF, Chen SA, et al. The impact of diabetes mellitus and corresponding HbA1c levels on the future risks of cardiovascular disease and mortality: a representative cohort study in Taiwan. PLoS One. 2015. April 13;10 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLS)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.