Abstract
Mild traumatic brain injury (mTBI) patients may have trauma-induced brain lesions detectable using CT scans. However, most patients will be CT-negative. There is thus a need for an additional tool to detect patients at risk. Single blood biomarkers, such as S100B and GFAP, have been widely studied in mTBI patients, but to date, none seems to perform well enough. In many different diseases, combining several biomarkers into panels has become increasingly interesting for diagnoses and to enhance classification performance. The present study evaluated 13 proteins individually—H-FABP, MMP-1, MMP-3, MMP-9, VCAM, ICAM, SAA, CRP, GSTP, NKDA, PRDX1, DJ-1 and IL-10—for their capacity to differentiate between patients with and without a brain lesion according to CT results. The best performing proteins were then compared and combined with the S100B and GFAP proteins into a CT-scan triage panel. Patients diagnosed with mTBI, with a Glasgow Coma Scale score of 15 and one additional clinical symptom were enrolled at three different European sites. A blood sample was collected at hospital admission, and a CT scan was performed. Patients were divided into two two-centre cohorts and further dichotomised into CT-positive and CT-negative groups for statistical analysis. Single markers and panels were evaluated using Cohort 1. Four proteins—H-FABP, IL-10, S100B and GFAP—showed significantly higher levels in CT-positive patients. The best-performing biomarker was H-FABP, with a specificity of 32% (95% CI 23–40) and sensitivity reaching 100%. The best-performing two-marker panel for Cohort 1, subsequently validated in Cohort 2, was a combination of H-FABP and GFAP, enhancing specificity to 46% (95% CI 36–55). When adding IL-10 to this panel, specificity reached 52% (95% CI 43–61) with 100% sensitivity. These results showed that proteins combined into panels could be used to efficiently classify CT-positive and CT-negative mTBI patients.
Introduction
Biomarkers have been intensively studied for their potential as diagnostic tools in cases of mild traumatic brain injury (mTBI): to allow accurate diagnosis, improve patient management speeds and reduce medical costs.[1, 2] mTBI is diagnosed from its clinical symptoms and a Glasgow Coma Scale (GCS) score between 13 and 15.[3] Determining whether patients have a trauma-induced brain lesion requires a head CT scan.[4, 5] However, CT scans are widely overused, as only 10% of mTBI patients who undergo one will be diagnosed with a brain lesion.[6, 7] In an attempt to reduce the high numbers of CT scans performed, several proteins have been investigated as potential triage markers. These include S100 calcium binding protein B (S100B) and glial fibrillary acidic protein (GFAP) both astrocyte damage markers, heart fatty acid binding protein (H-FABP) an intracellular vascular and brain fatty-acid transporter and interleukin 10 (IL-10) an anti-inflammatory protein. [8–21] The wide range of biomarker types investigated so far can be explained by the complex pathophysiological nature of TBI.[1] The mechanical forces of a trauma can lead to cell damage due to the shearing, tearing and stretching of neurons, axons, glial and blood vessels, and this damage will further induce biochemical alterations such as excitotoxicity, necrosis and apoptosis, oxidative stress and inflammation.[4, 22] Similar pathophysiological alterations can also be observed in other acute brain injury disorders, such as stroke.[22] A wide range of proteins, of different origins and from different pathways, have been studied as biomarkers for stroke diagnostics and prognostics.[23] However, despite the similarities between these conditions, the performances of several of these biomarkers have never been studied in relation to mTBI.
Regardless of the condition, single markers have been shown to lack the specificity and sensitivity necessary for their use as diagnostic tools in clinical settings.[4, 24] Indeed, to be a useful biomarker, the sensitivity needs to be very high in order to safely discharge patients without performing a CT scan. [7, 10] Furthermore, high specificity would reduce the harmful radiation exposure and it has been shown that a 10% CT scan reduction could save $20 million annually.[7, 18] Despite this, most mTBI biomarker research has been performed with single biomarkers. Combining different markers into a panel has been suggested in order to increase diagnostic performance.[1, 24] Panels have previously been shown to significantly increase diagnostic performance in several different diseases, e.g. sleeping sickness, aneurysmal subarachnoid haemorrhage and lung cancer, and in differentiating between mTBI patients and controls.[25–31] Furthermore, it has been suggested that combinations of different clinical parameters, such as age and even biomarker types, e.g. inflammation proteins and brain damage proteins, can improve classification.[24, 31]
We hypothesized that previously discovered stroke biomarkers could, due to the similarity in pathophysiology, be used as biomarkers also in mTBI patients. A total of 13 proteins—H-FABP, the matrix metalloproteinases 1, 3 and 9 (MMP-1, MMP-3 and MMP-9 respectively), the vascular and intravascular cell adhesion molecules (VCAM and ICAM respectively), IL-10, the inflammatory proteins serum amyloid A (SAA) and C-reactive protein (CRP), the oxidative stress proteins glutathione S-transferase pi (GSTP), nucleoside diphosphate kinase A (NKDA) and peroxiredoxin 1 (PRDX1) and the parkinson disease protein 7 (PARK7/DJ-1)—were chosen.[10, 16, 23, 32–37] These proteins were investigated for their individual performances as CT-scan triage biomarkers in mTBI patients with a GCS score of 15 and at least one clinical symptom. The best-performing proteins were then compared with the two most studied mTBI biomarkers: S100B and GFAP. Furthermore, we hypothesized that proteins combined into panels could increase the capacity to predict CT scan results.
Materials and methods
Study population
Patients were recruited from three different European sites: Geneva, Seville and Barcelona. The study was approved by the local ethics committees: Geneva’s Human Research Ethics Committee (CER: 12–194 / NAC 12–074); Barcelona’s Hospital Universitari Vall d’Hebron Ethics Committee (PR_AG_195–2012); and Seville’s Virgen del Rocío University Hospital Institutional Review Board (2012PI/120). Prior to inclusion, written informed consent was obtained from each patient or their legal representatives. Detailed inclusion and exclusion criteria have been specified elsewhere.[10] For inclusion, patients were diagnosed with mTBI and had a GCS score of 15 and at least one additional clinical symptom (vomiting or nausea, loss of consciousness, amnesia, an equilibrium disorder or a headache) and age above 14 years old. Each patient had a blood sample taken at hospital admission ≤ 6 h post trauma and a CT scan was performed within 24h post trauma. Exclusion criteria were no CT scan, no clinical symptoms, GCS score below 15, pregnancy and no signed informed consent form.
Analysis of proteins
Heparin plasma samples, collected in Geneva, and serum samples, collected in Seville and Barcelona, were centrifuged and stored at -80°C. The NDKA protein was analysed using a custom-made ELISA previously described in detail elsewhere.[35] The remaining proteins were quantified using commercial immunoassay kits (S1 Table) according to their manufacturers’ recommendations.
Statistical analysis
Due to the study population’s heterogeneity, both in terms of the samples (plasma/serum) and assays used, biomarker results were normalised using their medians as correction factors. The study population was divided into two larger two-centre cohorts. Cohort 1 was used for discovery and verification; Cohort 2 was used for validation. Within each cohort, patients were dichotomised into CT-negative and CT-positive groups for statistical analyses. Non-parametric tests were used hence all proteins were non-parametrically distributed, as indicated by the Kolomogorov-Smirnov test (p < 0.05). The non-parametric Mann–Whitney U test was used to establish differences between the groups, and Fisher’s exact test and the Chi-squared test were used for statistical analyses of the clinical data. Statistics were calculated using IBM SPSS software, version 24.0 (SPSS Inc., Chicago, IL, USA). The performances of individual proteins were tested using receiver operating characteristic (ROC) curves using TIBCO Spotfire S+® version 8.2 software (TIBCO Software Inc., Palo Alto, CA, USA).
Panel development
Panel experiments were performed using the Panelomix toolbox, which uses the iterative combination of biomarkers and thresholds (ICBT) method.[38] In brief, Panelomix selects cut-offs for each biomarker or clinical parameter to create the optimal panel performance. The panels’ maximum size was set to four parameters. The panel’s performance was investigated when sensitivity reached 100%.
Results
Single-marker performances
Cohort 1 included 132 patients, of whom 21 were CT-positive (16%). The two most common findings detected using CT scan were subarachnoid haemorrhage (43%) and skull fracture (38%) (Table 1). Most patients were male, had loss of consciousness or amnesia as clinical symptoms and had an isolated brain trauma (Table 2). Falls and traffic accidents were the most common mechanisms of injury in both CT-positive and CT-negative patients. The only significantly different clinical factor was age, with CT-positive patients being older than CT-negative patients (p < 0.01).
Table 1. Brain lesion findings in CT-positive mTBI patients.
Patients may have suffered from more than one lesion type, thus making the total percentage exceed 100%.
| CT scan results | n (%) |
|---|---|
| Epidural haemorrhage | 2 (10) |
| Subdural haemorrhage | 5 (24) |
| Subarachnoid haemorrhage | 9 (43) |
| Intracerebral haemorrhage | 4 (19) |
| Contusion with haemorrhage | 6 (29) |
| Skull fracture | 8 (38) |
Table 2. Cohort 1 mTBI patient characteristics ≤ 6 h post trauma.
| Cohort 1 | CT-negative | CT-positive | p-value† |
|---|---|---|---|
| CT scan, n (%) | 111 (84) | 21 (16) | |
| Time, trauma to blood, (min) | 0.367‡ | ||
| Mean (SD) | 195 (86) | 177 (100) | |
| Median (IQR) | 195 (120–255) | 160 (83–255) | |
| Age, mean (SD) | 46 (21) | 63 (24) | 0.003‡ |
| Male, n (%) | 82 (74) | 14 (67) | 0.496 |
| Symptoms, n (%) | |||
| Amnesia | 68 (61) | 15 (71) | 0.377 |
| Loss of consciousness | 93 (84) | 20 (95) | 0.307 |
| Nausea/vomiting | 27 (24) | 6 (29) | 0.680 |
| Headache | 55 (50) | 7 (33) | 0.172 |
| Mechanism of injury, n (%) | |||
| Traffic accident | 30 (27) | 8 (38) | 0.304 |
| Fall | 51 (46) | 10 (48) | 0.888 |
| Assault | 15 (14) | 2 (10) | 1 |
| Sports | 3 (3) | - | 1 |
| Others | 8 (7) | 1 (5) | 1 |
| NA | 4 (4) | - | |
| Isolated trauma, n (%) | 89 (81) | 15 (71) | 0.378 |
| NA, n (%) | 1 (1) | - |
†Chi-square test or Fisher’s exact test
‡Mann–Whitney U test
SD: standard deviation, IQR: interquartile range, NA: not available
Thirteen proteins—H-FABP, MMP-1, MMP-3, MMP-9, VCAM, ICAM, IL-10, SAA, CRP, GSTP, NKDA, PRDX1 and DJ-1—were evaluated individually for their CT-scan result prediction capacity. Analyses were performed on the first 62 patients recruited in the 132 mTBI patients of Cohort 1, of whom were 48 CT-negative and 14 CT-positive. Among the 13 biomarkers, only the H-FABP and IL-10 proteins were found at significantly higher levels in CT-positive patients than in CT-negative patients (p < 0.05) (Table 3). Each protein’s individual performance was established at 100% sensitivity, and specificity reached 33% for H-FABP and 27% for IL-10.
Table 3. Blood concentrations of 13 biomarkers in 48 CT-negative and 14 CT-positive mTBI patients, and the individual specificity performances.
| Protein | CT- median (IQR) |
CT+ median (IQR) |
P-value | Cut-off | % SE (95% CI) | % SP (95% CI) |
|---|---|---|---|---|---|---|
| IL-10 | 0.1 (0.06–1.2) |
0.5 (0.2–1.1) |
0.000 | 0.06 | 100 (100–100) | 27.1 (14.6–39.6) |
| H-FABP | 2.8 (1.8–4.4) |
4.4 (2.4–7.6) |
0.030 | 2.0 | 100 (100–100) | 33.3 (20.8–47.9) |
| VCAM | 586.6 (438.6–724.0) |
667.0 (536.8–861.3) |
0.145 | 359.2 | 100 (100–100) | 12.5 (4.2–22.9) |
| GSTP | 211.9 (83.3–469.2) |
224.6 (142.1–609.8) |
0.354 | 42.1 | 100 (100–100) | 10.4 (2.1–18.8) |
| CRP | 1970.5 (687.5–3977.7) |
2875.7 (676.5–15578.9) |
0.363 | 132.4 | 100 (100–100) | 4.2 (0.0–10.4) |
| SAA | 1259.3 (911.8–2555.5) |
2489.2 (563.2–9058.8) |
0.439 | 279.2 | 100 (100–100) | 8.3 (2.1–16.7) |
| DJ-1 | 382.3 (96.6–1867.9) |
468.8 (163.3–5071.6) |
0.501 | 50.8 | 100 (100–100) | 16.7 (6.3–27.1) |
| PRDX1 | 86.0 (40.8–211.8) |
94.0 (56.0–231.3) |
0.643 | 23.5 | 100 (100–100) | 6.3 (0.0–14.6) |
| NDKA | 14.0 (8.0–38.0) |
16.0 (9.0–36.8) |
0.775 | - | 100 (100–100) | - |
| ICAM | 428.3 (345.7–507.3) |
418.0 (332.0–550.9) |
0.814 | - | 100 (100–100) | - |
| MMP-3 | 17.8 (11.0–28.6) |
17.1 (10.7–26.4) |
0.866 | - | 100 (100–100) | - |
| MMP-1 | 19.5 (11.7–45.7) |
20.0 (9.9–33.2) |
0.946 | 5.5 | 100 (100–100) | 10.4 (2.1–18.8) |
| MMP-9 | 200.7 (122.5–370.7) |
198.9 (122.2–358.9) |
0.987 | 505.0 | 100 (100–100) | 8.3 (2.1–16.7) |
All protein concentrations are shown in ng/mL except for IL-10, which is in pg/mL.
IQR: interquartile range, SE: sensitivity, SP: specificity
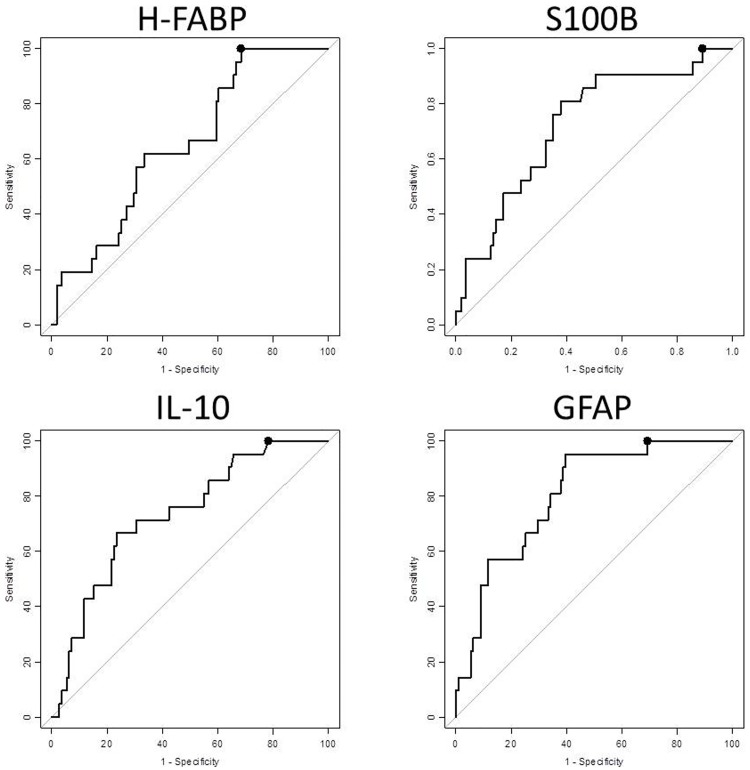
The best performing proteins—H-FABP and IL-10—were further compared to both S100B and GFAP for their individual capacities to predict CT scan results across all the mTBI patients in Cohort 1. All four proteins were found at significantly higher levels in CT-positive patients than in CT-negative patients (p < 0.05). The S100B, IL-10 and GFAP proteins reached specificities of 11%, 22% and 31%, respectively, when sensitivity was at 100%. The best performing protein was H-FABP; it reached 32% specificity and 100% sensitivity (Fig 1).
Fig 1. The proteins performances at classifying mTBI CT-positive and CT-negative patients.
Performance was investigated at 100% sensitivity, and the specificity (dots) reached 31.5% for H-FABP (95% CI 23.4–39.6; cut-off: 1.99 ng/mL), 10.8% for S100B (95% CI 5.4–17.1; cut-off: 0.06 ug/L), 21.6% for IL-10 (95% CI 14.4–28.8; cut-off: 0.12 pg/mL) and 30.6% for GFAP (95% CI 22.5–39.6; cut-off: 97.31 pg/mL).
Combination of markers in panels
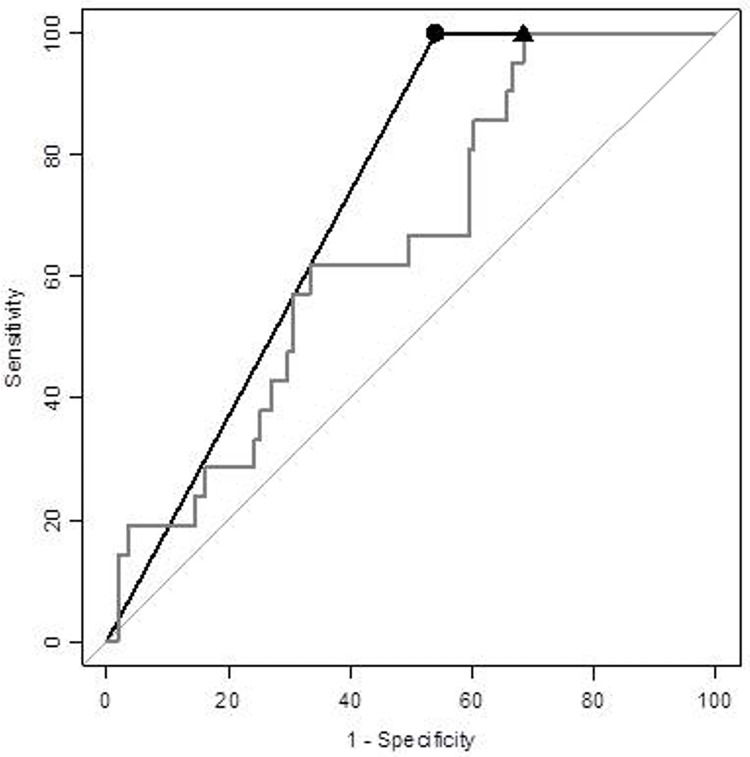
In an attempt to increase specificity, these four proteins were further analysed when combined in panels. All two-protein panels, except for one, showed increased specificity over the best-performing single molecule’s performance: H-FABP’s, at 32%. The best performing panel using two biomarkers was the combination of H-FABP and GFAP, which reached 46% specificity (Table 4 and Fig 2).
Table 4. The best-performing panel combinations for Cohort 1.
| Panel size | Biomarkers (cut-off) |
n CT- | n CT+ | Panel cut-off | % SE (95% CI) |
% SP (95% CI) |
|---|---|---|---|---|---|---|
| 2 parameters |
H-FABP (1.99) GFAP (97.31) |
111 | 21 | 2 | 100 (100–100) | 45.9 (36.0–55.0) |
| 3 parameters |
H-FABP (1.99) GFAP (97.3) IL-10 (0.12) |
111 | 21 | 3 | 100 (100–100) | 52.3 (43.2–61.3) |
| 4 parameters |
GFAP (97.3) H-FABP (1.99) S100B (0.061) IL-10 (0.12) |
111 | 21 | 4 | 100 (100–100) | 55.9 (46.8–64.9) |
The protein concentrations are for H-FABP are shown in ng/mL, S100B in ug/L and IL-10 and GFAP in pg/mL.
Fig 2. The best two-biomarker panel, combining H-FABP and GFAP, at correctly classifying mTBI CT-positive and CT-negative patients compared to the individual best-performing protein: H-FABP.
Performance was investigated at 100% sensitivity, and the panel’s specificity reached 46% (dot, cut-off: 2 parameters, black), compared to the best-performing single marker, H-FABP, which reached 32% specificity (triangle, cut-off: 1.99 ng/mL, grey).
Several studies have highlighted age as a risk factor for brain lesions and, as stated above, age was significantly different and therefore included to the combinations as an additional parameter.[39, 40] The panel combination of a single protein and age only increased specificity by a maximum of 3% over H-FABP alone (S2 Table). An increase in specificity was observed when panel size was expanded. Indeed, when combining three proteins, H-FABP + GFAP + IL-10, specificity reached 52%, which was 6% better than the best two-parameter panel. The best-performing panel included all four proteins, reaching a specificity of 56% at a sensitivity of 100% (Table 4 and S2 Table).
Panel validation
Independent Cohort 2 was used for panel validation on 109 patients, of whom 17 (16%) were CT-positive. The cohort had similar clinical data to Cohort 1, however, age was not significantly different between CT-positive and CT-negative patients (S3 Table). At the single-molecule performance level, when sensitivity was 100%, H-FABP remained the single best-performing protein (S4 Table).
The best-performing panels found using Cohort 1, were validated using Cohort 2. The three panels had a variation in specificity of < 4% between the two cohorts. The panel including all four proteins only increased specificity by 2% in comparison to the best three-parameter panel: H-FABP + GFAP + IL-10. (Table 4 and S5 Table). The most stable combination was H-FABP and GFAP, with only 1% difference in specificity between the cohorts, ranging from 45%–46%, which was 14% higher than the performance observed with a single best molecule: H-FABP (Fig 2).
Discussion
The present multicentre study evaluated 13 biomarkers, all previously investigated in stroke patients, for their capacity to correctly classify CT-positive and CT-negative mTBI patients with a GCS score of 15 and at least one clinical symptom. Among the 13 biomarkers, the H-FABP and IL-10 proteins were the best-performing single markers, and these were then further compared and combined with the well-studied S100B and GFAP markers. H-FABP was the best-performing single marker, but when combined with GFAP, overall performance increased from 32% to 46% specificity, with sensitivity at 100%.
The four proteins—S100B, GFAP, H-FABP and IL-10—have all previously been identified for their potential to differentiate CT-positive and CT-negative mTBI patients, confirming the results found here.[10, 16, 19, 41] The proteins have been shown to be released from or leak out of different types of injured cells. Indeed, S100B and GFAP leak from injured astrocytes, H-FABP leaks from endothelial cells and neuron cell bodies, whereas Il-10 is expressed by monocytes and macrophages.[8, 11–14, 42, 43] The difficulty, for all biomarker research for brain injuries, is to know if the measured proteins really originate from the brain injury. The four proteins measured here have also been shown to be expressed in cells outside CNS or to be increased after orthopaedic trauma.[2, 44–46] Previously, H-FABP performance has been shown higher in isolated mTBI patients compared to those suffering from multiple traumas.[10] This suggests that at least a part of the H-FABP measured originate from the CNS. Furthermore, elevated levels of H-FABP in blood samples after a stroke have been shown to originate from the CNS.[47] The possiblity to measure the presence of brain derived H-FABP in the blood may be, as suggested for S100B and GFAP, due to blood brain barrier damage or through the glymphatic system.[2]
Independent of origin, single biomarkers have been indicated to not display sufficient performance to be turned into diagnostic tests.[17] Combinations of markers, i.e. panels, have been shown to increase diagnostic performance when combining proteins of diverse origins and different pathways.[24] Diagnostic combinations created using GFAP, H-FABP, S100B and IL-10 resulted in an efficient panel constituted of H-FABP and GFAP and reaching 46% specificity and 100% sensitivity. The panel result was confirmed using a second, independent, two-centre cohort. It is interesting to note that even though the individual performance of the biomarkers varied in each cohort, the panel was found to be stable across both cohorts and it increased specificity by 14% compared to the best single biomarker.
Combinations of biomarkers as a CT-scan triage tool have previously been shown to result in high prediction capacity. A combination including matrix metalloproteinase-2 (MMP-2), CRP and creatine kinase B type (CKBB) held an excellent AUC of 96%. However, in contrary to the results shown here, the combination was presented as a model performed using a likelihood ratio approach.[48] This approach highly complicated to be implemented in a clinical setting. This strategy gives an overall probability of the combination performance without cut-off values for each marker that indicate which patients have to be considered as CT-positive. The panels obtained using PanelomiX have all individual cut-offs for each marker and also a panel cut-off indicating how many of the markers need to be classified as positive in order for the panel to be classified as positive. The use of this tool greatly increases the potential clinical application and feasibility. It would be very interesting to investigate the combination model proposed by Sharma et al. using the PanelomiX tool in order to compare both approaches.
The number of parameters included in a panel may vary from two to dozens. However, the test’s cost-effectiveness must be maintained and over-fitting should be avoided. Our panel composed of H-FABP and GFAP reached a specificity of 45%–46% with a sensitivity of 100%. Adding a third protein was shown here to be even more efficient to avoid CT-scans. However, the costs of measuring all the possible parameters may exceed the costs of using a CT scan to diagnose patients with a significant brain lesion. Other large multicentre studies will be needed to reduce the risk of overfitting and to investigate the panel’s cost-effectiveness.
Another interesting field, requiring exploration, would be the use of the panel in a point-of-care testing (POCT) kit. POCT can greatly reduce time spent analysing and deciding, and it can also be used closer to the patients, e.g. at local medical practices.[49] Several companies are currently developing these kinds of tools. The panel, and potentially its corresponding POCT, could also be interesting tools for outcome measurements. Indeed, both H-FABP and GFAP have been shown to be predictive biomarkers for poor outcome in severe TBI patients.[37, 50] It would, therefore, be interesting to evaluate their individual and combined prediction capacities of poor outcome in mTBI patients.
The present study had certain limitations. Patients originated from three different European sites and only mTBI patients with a GCS score of 15, plus one additional clinical symptom, were included. These strict inclusion criteria reduced the number of CT-negative patients, as patients with a GCS score of 15 but no symptoms were excluded from the study. Furthermore, different samples were collected (plasma or serum), and different kits were used to measure the proteins, depending on the cohort. These differences meant that a clear cut-off level for each protein could not be precisely set up, and this would need additional investigation. However, the study’s results were highly reproducible from cohort to cohort, suggesting an extremely low over-fitting bias.
Conclusion
This multicentre study showed that combining the measurement of the H-FABP and GFAP proteins into a single panel test could be used to efficiently classify CT-positive and CT-negative patients. The panel significantly outperformed H-FABP alone, the best-performing individual molecule, by reaching 46% specificity and 100% sensitivity. By adding IL-10 to the panel, overall performance reached 52% specificity at 100% sensitivity.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Kulbe JR, Geddes JW. Current status of fluid biomarkers in mild traumatic brain injury. Experimental neurology. 2016;275 Pt 3:334–52. doi: 10.1016/j.expneurol.2015.05.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawata K, Liu CY, Merkel SF, Ramirez SH, Tierney RT, Langford D. Blood biomarkers for brain injury: What are we measuring? Neuroscience and biobehavioral reviews. 2016;68:460–73. doi: 10.1016/j.neubiorev.2016.05.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Definition of mild traumatic brain injury. The Journal of Head Trauma Rehabilitation. 1993;8(3):86–7. [Google Scholar]
- 4.North SH, Shriver-Lake LC, Taitt CR, Ligler FS. Rapid analytical methods for on-site triage for traumatic brain injury. Annual review of analytical chemistry. 2012;5:35–56. doi: 10.1146/annurev-anchem-062011-143105 . [DOI] [PubMed] [Google Scholar]
- 5.Freire-Aragon MD, Rodriguez-Rodriguez A, Egea-Guerrero JJ. Update in mild traumatic brain injury. Medicina clinica. 2017;149(3):122–7. [DOI] [PubMed] [Google Scholar]
- 6.Melnick ER, Szlezak CM, Bentley SK, Dziura JD, Kotlyar S, Post LA. CT overuse for mild traumatic brain injury. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2012;38(11):483–9. . [DOI] [PubMed] [Google Scholar]
- 7.Bogoslovsky T, Gill J, Jeromin A, Davis C, Diaz-Arrastia R. Fluid Biomarkers of Traumatic Brain Injury and Intended Context of Use. Diagnostics. 2016;6(4). doi: 10.3390/diagnostics6040037 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer CA, Brunkhorst R, Niessner M, Pfeilschifter W, Steinmetz H, Foerch C. Blood levels of glial fibrillary acidic protein (GFAP) in patients with neurological diseases. PloS one. 2013;8(4):e62101 doi: 10.1371/journal.pone.0062101 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papa L, Lewis LM, Falk JL, Zhang Z, Silvestri S, Giordano P, et al. Elevated levels of serum glial fibrillary acidic protein breakdown products in mild and moderate traumatic brain injury are associated with intracranial lesions and neurosurgical intervention. Annals of emergency medicine. 2012;59(6):471–83. doi: 10.1016/j.annemergmed.2011.08.021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lagerstedt L, Egea-Guerrero JJ, Bustamante A, Montaner J, Rodriguez-Rodriguez A, El Rahal A, et al. H-FABP: A new biomarker to differentiate between CT-positive and CT-negative patients with mild traumatic brain injury. PloS one. 2017;12(4):e0175572 doi: 10.1371/journal.pone.0175572 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zimmerman AW, Veerkamp JH. New insights into the structure and function of fatty acid-binding proteins. Cellular and molecular life sciences: CMLS. 2002;59(7):1096–116. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veerkamp JH, Paulussen RJ, Peeters RA, Maatman RG, van Moerkerk HT, van Kuppevelt TH. Detection, tissue distribution and (sub)cellular localization of fatty acid-binding protein types. Molecular and cellular biochemistry. 1990;98(1–2):11–8. . [DOI] [PubMed] [Google Scholar]
- 13.Woodcock T, Morganti-Kossmann MC. The role of markers of inflammation in traumatic brain injury. Frontiers in neurology. 2013;4:18 doi: 10.3389/fneur.2013.00018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steiner J, Bernstein HG, Bielau H, Berndt A, Brisch R, Mawrin C, et al. Evidence for a wide extra-astrocytic distribution of S100B in human brain. BMC neuroscience. 2007;8:2 doi: 10.1186/1471-2202-8-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zetterberg H, Smith DH, Blennow K. Biomarkers of mild traumatic brain injury in cerebrospinal fluid and blood. Nat Rev Neurol. 2013;9(4):201–10. doi: 10.1038/nrneurol.2013.9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lagerstedt L, Egea-Guerrero JJ, Rodriguez-Rodriguez A, Bustamante A, Montaner J, El Rahal A, et al. Early measurement of interleukin-10 predicts the absence of CT scan lesions in mild traumatic brain injury. PloS one. 2018;13(2):e0193278 doi: 10.1371/journal.pone.0193278 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeter CB, Hergenroeder GW, Hylin MJ, Redell JB, Moore AN, Dash PK. Biomarkers for the diagnosis and prognosis of mild traumatic brain injury/concussion. Journal of neurotrauma. 2013;30(8):657–70. doi: 10.1089/neu.2012.2439 . [DOI] [PubMed] [Google Scholar]
- 18.Heidari K, Vafaee A, Rastekenari AM, Taghizadeh M, Shad EG, Eley R, et al. S100B protein as a screening tool for computed tomography findings after mild traumatic brain injury: Systematic review and meta-analysis. Brain injury. 2015:1–12. doi: 10.3109/02699052.2015.1037349 . [DOI] [PubMed] [Google Scholar]
- 19.Egea-Guerrero JJ, Revuelto-Rey J, Murillo-Cabezas F, Munoz-Sanchez MA, Vilches-Arenas A, Sanchez-Linares P, et al. Accuracy of the S100beta protein as a marker of brain damage in traumatic brain injury. Brain injury. 2012;26(1):76–82. doi: 10.3109/02699052.2011.635360 . [DOI] [PubMed] [Google Scholar]
- 20.Welch RD, Ayaz SI, Lewis LM, Unden J, Chen JY, Mika VH, et al. Ability of Serum Glial Fibrillary Acidic Protein, Ubiquitin C-Terminal Hydrolase-L1, and S100B To Differentiate Normal and Abnormal Head Computed Tomography Findings in Patients with Suspected Mild or Moderate Traumatic Brain Injury. Journal of neurotrauma. 2016;33(2):203–14. doi: 10.1089/neu.2015.4149 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papa L, Brophy GM, Welch RD, Lewis LM, Braga CF, Tan CN, et al. Time Course and Diagnostic Accuracy of Glial and Neuronal Blood Biomarkers GFAP and UCH-L1 in a Large Cohort of Trauma Patients With and Without Mild Traumatic Brain Injury. JAMA neurology. 2016. doi: 10.1001/jamaneurol.2016.0039 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tuttolomondo A, Pecoraro R, Pinto A. Studies of selective TNF inhibitors in the treatment of brain injury from stroke and trauma: a review of the evidence to date. Drug design, development and therapy. 2014;8:2221–38. doi: 10.2147/DDDT.S67655 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maas MB, Furie KL. Molecular biomarkers in stroke diagnosis and prognosis. Biomarkers in medicine. 2009;3(4):363–83. doi: 10.2217/bmm.09.30 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robin X, Turck N, Hainard A, Lisacek F, Sanchez JC, Muller M. Bioinformatics for protein biomarker panel classification: what is needed to bring biomarker panels into in vitro diagnostics? Expert review of proteomics. 2009;6(6):675–89. doi: 10.1586/epr.09.83 . [DOI] [PubMed] [Google Scholar]
- 25.Tiberti N, Matovu E, Hainard A, Enyaru JC, Lejon V, Robin X, et al. New biomarkers for stage determination in Trypanosoma brucei rhodesiense sleeping sickness patients. Clinical and translational medicine. 2013;2(1):1 doi: 10.1186/2001-1326-2-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shan R, Szmydynger-Chodobska J, Warren OU, Mohammad F, Zink BJ, Chodobski A. A New Panel of Blood Biomarkers for the Diagnosis of Mild Traumatic Brain Injury/Concussion in Adults. Journal of neurotrauma. 2016;33(1):49–57. doi: 10.1089/neu.2014.3811 . [DOI] [PubMed] [Google Scholar]
- 27.Hainard A, Tiberti N, Robin X, Lejon V, Ngoyi DM, Matovu E, et al. A combined CXCL10, CXCL8 and H-FABP panel for the staging of human African trypanosomiasis patients. PLoS neglected tropical diseases. 2009;3(6):e459 doi: 10.1371/journal.pntd.0000459 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hainard A, Tiberti N, Robin X, Ngoyi DM, Matovu E, Enyaru JC, et al. Matrix metalloproteinase-9 and intercellular adhesion molecule 1 are powerful staging markers for human African trypanosomiasis. Tropical medicine & international health: TM & IH. 2011;16(1):119–26. doi: 10.1111/j.1365-3156.2010.02642.x . [DOI] [PubMed] [Google Scholar]
- 29.Calderon-Santiago M, Priego-Capote F, Turck N, Robin X, Jurado-Gamez B, Sanchez JC, et al. Human sweat metabolomics for lung cancer screening. Analytical and bioanalytical chemistry. 2015;407(18):5381–92. doi: 10.1007/s00216-015-8700-8 . [DOI] [PubMed] [Google Scholar]
- 30.Turck N, Vutskits L, Sanchez-Pena P, Robin X, Hainard A, Gex-Fabry M, et al. A multiparameter panel method for outcome prediction following aneurysmal subarachnoid hemorrhage. Intensive care medicine. 2010;36(1):107–15. doi: 10.1007/s00134-009-1641-y . [DOI] [PubMed] [Google Scholar]
- 31.Azurmendi Leire, S A, Tiberti Natalia, Kapandji Natacha, Sanchez-Peña Paola, Degos Vincent, Puybasset Louis, Richard Sébastien, Turck Natacha, Sanchez Jean-Charles. Infection prediction for aneurysmal subarachnoid hemorrhage patients at hospital admission: combined panel of serum amyloid A and clinical parameters. J Transl Sci. 2017;3. [Google Scholar]
- 32.Turck N, Robin X, Walter N, Fouda C, Hainard A, Sztajzel R, et al. Blood glutathione S-transferase-pi as a time indicator of stroke onset. PloS one. 2012;7(9):e43830 doi: 10.1371/journal.pone.0043830 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richard S, Lapierre V, Girerd N, Bonnerot M, Burkhard PR, Lagerstedt L, et al. Diagnostic performance of peroxiredoxin 1 to determine time-of-onset of acute cerebral infarction. 2016;6:38300 doi: 10.1038/srep38300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richard S, Lagerstedt L, Burkhard PR, Debouverie M, Turck N, Sanchez JC. E-selectin and vascular cell adhesion molecule-1 as biomarkers of 3-month outcome in cerebrovascular diseases. Journal of inflammation. 2015;12:61 doi: 10.1186/s12950-015-0106-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allard L, Burkhard PR, Lescuyer P, Burgess JA, Walter N, Hochstrasser DF, et al. PARK7 and nucleoside diphosphate kinase A as plasma markers for the early diagnosis of stroke. Clinical chemistry. 2005;51(11):2043–51. doi: 10.1373/clinchem.2005.053942 . [DOI] [PubMed] [Google Scholar]
- 36.Azurmendi L, Lapierre-Fetaud V, Schneider J, Montaner J, Katan M, Sanchez JC. Proteomic discovery and verification of serum amyloid A as a predictor marker of patients at risk of post-stroke infection: a pilot study. Clinical proteomics. 2017;14:27 doi: 10.1186/s12014-017-9162-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walder B, Robin X, Rebetez MML, Copin JC, Gasche Y, Sanchez JC, et al. The Prognostic Significance of the Serum Biomarker Heart-Fatty Acidic Binding Protein in Comparison with S100b in Severe Traumatic Brain Injury. Journal of neurotrauma. 2013;30(19):1631–7. doi: 10.1089/neu.2012.2791 [DOI] [PubMed] [Google Scholar]
- 38.Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, et al. PanelomiX: A threshold-based algorithm to create panels of biomarkers. Translational Proteomics. 2013;1(1):57–64. http://dx.doi.org/10.1016/j.trprot.2013.04.003. [Google Scholar]
- 39.Borg J, Holm L, Cassidy JD, Peloso PM, Carroll LJ, von Holst H, et al. Diagnostic procedures in mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of rehabilitation medicine. 2004;(43 Suppl):61–75. . [DOI] [PubMed] [Google Scholar]
- 40.Unden J, Ingebrigtsen T, Romner B, Scandinavian Neurotrauma C. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: an evidence and consensus-based update. BMC medicine. 2013;11:50 doi: 10.1186/1741-7015-11-50 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Papa L, Silvestri S, Brophy GM, Giordano P, Falk JL, Braga CF, et al. GFAP out-performs S100beta in detecting traumatic intracranial lesions on computed tomography in trauma patients with mild traumatic brain injury and those with extracranial lesions. Journal of neurotrauma. 2014;31(22):1815–22. doi: 10.1089/neu.2013.3245 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pelsers MM, Hanhoff T, Van der Voort D, Arts B, Peters M, Ponds R, et al. Brain- and heart-type fatty acid-binding proteins in the brain: tissue distribution and clinical utility. Clinical chemistry. 2004;50(9):1568–75. doi: 10.1373/clinchem.2003.030361 . [DOI] [PubMed] [Google Scholar]
- 43.Trifunovic J, Miller L, Debeljak Z, Horvat V. Pathologic patterns of interleukin 10 expression—a review. Biochemia medica. 2015;25(1):36–48. doi: 10.11613/BM.2015.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rutz S, Ouyang W. Regulation of Interleukin-10 Expression. Advances in experimental medicine and biology. 2016;941:89–116. doi: 10.1007/978-94-024-0921-5_5 . [DOI] [PubMed] [Google Scholar]
- 45.Lescuyer P, Allard L, Hochstrasser DF, Sanchez JC. Heart-fatty acid-binding protein as a marker for early detection of acute myocardial infarction and stroke. Molecular diagnosis: a journal devoted to the understanding of human disease through the clinical application of molecular biology. 2005;9(1):1–7. . [DOI] [PubMed] [Google Scholar]
- 46.Posti JP, Hossain I, Takala RS, Liedes H, Newcombe V, Outtrim J, et al. Glial Fibrillary Acidic Protein and Ubiquitin C-Terminal Hydrolase-L1 Are Not Specific Biomarkers for Mild CT-Negative Traumatic Brain Injury. Journal of neurotrauma. 2017. doi: 10.1089/neu.2016.4442 . [DOI] [PubMed] [Google Scholar]
- 47.Zimmermann-Ivol CG, Burkhard PR, Le Floch-Rohr J, Allard L, Hochstrasser DF, Sanchez JC. Fatty acid binding protein as a serum marker for the early diagnosis of stroke: a pilot study. Molecular & cellular proteomics: MCP. 2004;3(1):66–72. doi: 10.1074/mcp.M300066-MCP200 . [DOI] [PubMed] [Google Scholar]
- 48.Sharma R, Rosenberg A, Bennett ER, Laskowitz DT, Acheson SK. A blood-based biomarker panel to risk-stratify mild traumatic brain injury. PloS one. 2017;12(3):e0173798 doi: 10.1371/journal.pone.0173798 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Junker R, Schlebusch H, Luppa PB. Point-of-care testing in hospitals and primary care. Deutsches Arzteblatt international. 2010;107(33):561–7. doi: 10.3238/arztebl.2010.0561 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nylen K, Ost M, Csajbok LZ, Nilsson I, Blennow K, Nellgard B, et al. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. Journal of the neurological sciences. 2006;240(1–2):85–91. doi: 10.1016/j.jns.2005.09.007 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.