ABSTRACT
Background: This study aimed to evaluate the cost-effectiveness of the 13-valent pneumococcal conjugate vaccine (PCV-13) compared to a no vaccination strategy in Chinese infants.
Methods: A Markov process model was developed to examine the outcomes of PCV-13 against a no vaccination strategy using data and assumptions adapted for relevance to China. Outcomes over a lifetime horizon are presented. One-way and probabilistic sensitivity analyses were performed to determine the uncertainty.
Results: Compared to no vaccination, a PCV-13 vaccination program would provide a gain of 0.009 additional quality-adjusted life years (QALYs) per subject. From the health care and societal perspectives, the incremental costs per QALY were $20,709 and 18,483, respectively. When herd effect was included, the cost effectiveness of the PCV-13 vaccination strategy was notably improved. The lower price of PCV-13 will improve the cost-effectiveness.
Conclusions: The PCV-13 vaccination is likely to be cost-effective at the current Chinese prices and ceiling threshold ($8,382).
KEYWORDS: Cost-effectiveness analysis, PCV-13, pneumococcal disease, Chinese infant, Decision model
Introduction
Streptococcus pneumoniae (S. pneumonia) infection is a major cause of morbidity and mortality in infants and young children,1 and it can lead to invasive pneumococcal diseases (IPD), meningitis and bacteremia, as well as non-invasive pneumococcal diseases, such as pneumonia and acute otitis media (AOM). The World Health Organization (WHO) reported that approximately 476,000 (333,000–529,000) annual deaths worldwide were attributable to pneumococcal infections.2 In China, nearly 30,000 deaths per year were associated with pneumococcal disease.3 The high economic burden, in terms of the cost of managing infections caused by S. pneumonia, is a worldwide concern.4
New pneumococcal conjugate vaccines (PCV), such as the 13-valent PCV (PCV-13, Prevnar 13, Pfizer, Pearl River, New York, USA), have been developed to protect infants and young children from pneumococcal diseases.5 PCV-13 covers serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14,18C, 19A, 19F and 23F, which cause most invasive pneumococcal diseases globally in Children.6 Several large-scale clinical trials have demonstrated the clinically effective and safety profile of PCV-13 in infants and children,7,8 demonstrating that vaccination programs could notably decrease the incidences of IPD, pneumonia, and otitis media. Furthermore, the direct effect can also extend the benefit to unvaccinated populations by decreasing the nasopharyngeal carriage of S. pneumonia in vaccinated children. One recent systematic review has shown that childhood PCV-13 programs could substantially protect across the whole population within a decade through “herd immunity”.9
In 2014, we reported the findings of our investigation of the cost-effectiveness of PCV-7 vaccinations versus no vaccinations in China, which showed that a universal vaccination program using PCV-7 is not cost-effective due to the high cost of PCV-7.10 At present, PCV-13 has been licensed for use in Chinese infants and young children. Since then, the situation has changed, in terms of the price and higher serotype coverage of PCV-13. Here, we report an updated economic analysis of a universal vaccination program with PCV-13 from a Chinese heath care and societal perspective based on the Consolidated health economic evaluation reporting standards (CHEERS).11 Because PCV-7 was withdrawn by the producer and PCV-10 vaccines are not available in Chinese market, they will not be included in the current analysis.
Methods
Model structure
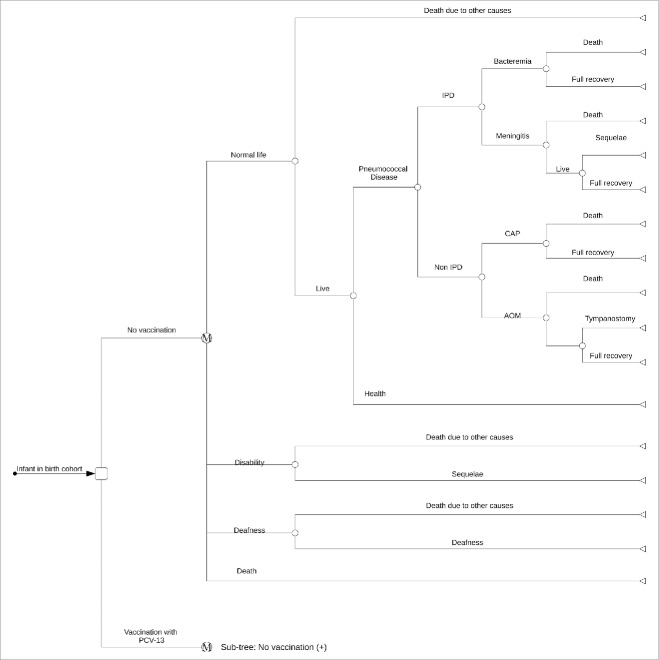
An age-stratified static multiple-cohort model was developed to compare lifetime (that is, until death at a maximum of 100 years of age) costs and outcomes associated with a PCV-13 vaccination program for Chinese infants. The children might incur the following four initial pneumococcal-associated diseases: meningitis, bacteremia, community acquired pneumonia (CAP) and acute otitis media (AOM), which could result in long-term complications, including deafness, disability, or death from S. pneumoniae infection (Fig. 1). The model was reviewed and validated by Chinese experts, including epidemiologists, health economists, pediatricians, and policy decision makers. The Markov cycle lengths in the time horizons 0–10 years and 11–100 years were set to 1 month and 1 year, respectively. Natural mortality could occur at any point. The life expectancy tables for China from the life tables of the World Health Organization (WHO) member states (2011) were used in the analysis. When indirect effects (herd immunity) are included in the model, the population without vaccination is considered to be at risk of developing IPD. The model was developed using R statistical software (version 3.3.1; R Development Core Team, Vienna, Austria).
Figure 1.
The structure of the model used to assess the health and economic impact of PCV-13 vaccination and possible subsequent events for each child compared to ‘no vaccination’. The following health states are included: meningitis, bacteremia, pneumonia, AOM and no infection.
A yearly discount rate of 5% for the costs and health benefits was applied, based on recommendations from the Chinese guidelines for pharmacoeconomic evaluations. The costs are shown in US dollars (US $ 1 = 6.8 Chinese Yuan), with 2016 as the reference year. The incremental cost-effectiveness ratio (ICER), presented as the cost per additional QALY gained, was used as the main endpoint. When the ICER was lower than the per capita gross domestic product (GDP) of China per QALY ($8,382), cost-effectiveness was considered.12 Per capita GDP of Shanghai City per QALY ($16,725) would be used in sensitivity analysis for examining the cost-effectiveness in Chinese developed regions.
In this analysis, two competitive policy strategies of vaccination strategies were compared.
-
•
Strategy 1 (universal vaccinations): the Chinese birth cohort will be vaccinated with free PCV-13 vaccines, fully supported by the Chinese government. In this strategy, 4 doses (3+1 schedule) at the ages of 2, 3, 4 and 11 months were considered.13 The vaccine coverage rate was 83.27%, which was assumed to be equivalent to hepatitis B vaccination program because they have a similar vaccination schedule.14
-
•
Strategy 2 (no vaccinations): the Chinese birth cohort will not be vaccinated.
Epidemiology of pneumococcal disease in China
The model inputs for the epidemiology data (Table 1 and appendix Table 1) were obtained from Chinese studies to the greatest possible extent. When local data were unavailable, we justified data from other regions by weighting the geographical and population similarity. Due to the lack of Chinese-specific nationwide epidemiological data, the pre-vaccination rates of all cases of IPD, CAP and AOM, as well as their case-fatality rates, were derived from surveillance data from Chinese Taiwan and Hong Kong,15 which was assumed to be similar in whole Chinese population. The S. pneumonia isolation rates of CAP and AOM in China were 8% and 39.2%, respectively, which were estimated based on studies reporting data from a Chinese population.2,10 The age-specific episodes of all-cause hospitalized CAP were estimated based on Chinese local studies.16,17 The prevalence of disability and deafness caused by pneumococcal meningitis were 7.0% and 13.0%, respectively.18 Because AOM frequently occurs at younger ages,19 the risk of AOM was considered in children younger than 5 years old. Due to the lack of reliable data, no risks of long-term sequelae or deaths caused by AOM were assumed in the present study.
Table 1.
Key inputs of the model.
| Parameters | Expected value | Ranges | Source |
|---|---|---|---|
| Clinical data | |||
| S. pneumoniae isolation rate for pneumonia | 8.0% | 2.0%—26.8% | 2 |
| S. pneumoniae isolation rate for AOM | 39.2% | 29.2%—49.0% | 27 |
| Serotype coverage rates of PCV-13 | — | ||
| IPD | 91.0% | 68.3%—100.0% | 20-22 |
| CAP | 84.2% | 79.6%—86.9% | 20-22 |
| AOM | 71.5% | 67.6%—73.8% | Estimated |
| Efficacy of PCV-13 | — | ||
| IPD | 97.4% | 73.1%—100.0% | 23,24 |
| CAP | 39.2% | 67.5%—100.0% | 23,24 |
| AOM | 69.9% | 29.8%—87.1% | 23,24 |
| Herd effects of PCV-13 for IPD | 38.3% | 0.0%—38.3% | 18,23 |
| Cost data ($) | |||
| Bacteremia per event in children | 3,256 | 1,367—5,719 | 10 |
| Meningitis per event in children | 4,250 | 1,907—9,572 | 10 |
| Pneumonia per hospitalized event | 632 | 443—833 | 10 |
| Pneumonia per outpatient event | 30 | 29—32 | 10 |
| AOM per simple event | 14 | 11—21 | 10 |
| AOM per complex event | 23 | 23—24 | 10 |
| Tympanostomy caused by AOM | 309 | 232—386 | 10 |
| Bacteremia per event in adult | 2,782 | 2,087—3,478 | 10 |
| Meningitis per event in adult | 3,897 | 2,923—4,871 | 10 |
| PCV-13 per course | 235 | 176—471 | Local charge |
| Daily average employment costs | 23 | 7—35 | Local charge |
| Disutility weights* | |||
| Bacteremia | 0.0079 | 0.0060—0.0099 | 28-30 |
| Meningitis | 0.0232 | 0.0174—0.029 | 28-30 |
| Pneumonia | 0.0079 | 0.0060—0.0099 | 28-30 |
| AOM | 0.0050 | 0.0036—0.0063 | 28-30 |
| Tympanostomy caused by AOM | 0.1800 | 0.1350—0.2250 | 28-30 |
| Long-term disability | 0.4000 | 0.3000—0.5000 | 28-30 |
| Long-term deafness | 0.2000 | 0.1500—0.2500 | 28-30 |
CAP: community-acquired pneumonia; AOM: acute otitis media; IPD: invasive pneumococcal disease.
The disutility weight is the lost utility due to disease. The utility value can be calculated by the formula: 1—disutility weight.
Vaccine efficacy
A surveillance study of Chinese children estimated an 84.2% PCV-13 serotype coverage rate for S. pneumonia and a 91% serotype coverage rate for IPD.20-22 There was no Chinese-specific serotype coverage rate for AOM, thus, the PCV13 serotype coverage rate for AOM was estimated based on the observed PCV-7 serotype coverage rate for AOM, as well as the proportion (i.e., between PCV-7 and PCV-13) of the serotype coverage rates for S. pneumonia because AOM and S. pneumonia are mucosal diseases15; this estimate could be expressed by the following formula: Serotype coverage(AOM)PCV-13 = Serotype coverage(AOM)PCV-7 × (Serotype coverage[S. pneumonia]PCV-13/Serotype coverage[S. pneumonia]PCV-7). The efficacies of PCV-13 for IPD, pneumonia and AOM caused by covered S. pneumonia were 97.4, 90.0 and 69.9%, respectively.23,24 We assumed that the vaccine efficacy would exponentially increase from zero to full efficacy in the first year of vaccination and wane exponentially from full efficacy to zero between 3 and 10 years of age.18,23
Herd protection against IPD following PCV-13 vaccination of sequential birth cohorts was considered for the entire population. Herd protection of PCV-13 against pneumonia and AOM was conservatively assumed to be zero due to the absence of conclusive data regarding the ability of indirect effects of PCV-13 on pneumonia and AOM.25 Because the serotype replacement could impair the indirect protection, a fixed net indirect effect of −38.25% on IPD was applied in the current analysis, according to previously published reports.18,23 The effect of herd protection was checked in scenario analyses.
Costs and utilities
The cost of pneumococcal disease was estimated from a Chinese heath care and societal perspective. All cost parameters are shown in Table 1. The direct medical costs of treating acute episodes in children, including episodes of meningitis, bacteremia, CAP and AOM, were derived from our previously published economic analysis of PCV-7 in China. In these instances, the treatment costs were assumed to be incurred within 1 cycle. The costs of the long-lasting sequelae of meningitis (neurological sequelae and hearing loss) were considered over the remaining lifetime, which was also obtained from our previous report.10,26 The cost of the PCV-13 vaccination per Chinese infant included four doses of PCV-13 vaccines and administration costs. The indirect cost was multiplied by the daily per capita GDP salary in China and the loss of productivity associated with pneumococcal disease, which was estimated by a Chinese clinician panel.
Heath utility values ranging from 1 (perfect health) to 0 (death) were used to estimate QALYs. The disutility weight causing by acute events and long-term sequelaes (neurologic disability and deafness) were obtained from the literature (Table 1). In the current analysis, the long-term sequelaes were assumed to be applied for one month and the remaining lifetimes of the patients, respectively.
Sensitivity analysis
Probabilistic sensitivity analyses were performed using a 1000 second-order Monte Carlo simulation, which was used to generate cost-effectiveness acceptability curves. Probabilistic distribution was defined according to the modeled parameters: beta distribution was used for the incidences, risks, probabilities, proportions and utilities, and the gamma distribution was used for costs. Based on the results of the probabilistic sensitivity analyses, one-way sensitivity analyses were conducted to test the uncertainties of the model variables in a base case analysis setting. The plausible ranges for each variable were determined based on the published sources; when reported data were not available, a range of ±25% of the base-case value was used for the reported values, such as 95% confidence interval (CI), or expert opinion.
Results
Base-case analysis
Under the setting of no herd protection and herd protection, vaccination with PCV-13 averted 0.045% and 0.083% IPD and 0.001% and 0.002% deaths associated with S. pneumonia, and improved 0.009 and 0.010 QALYs compared with no vaccinations (Table 2), respectively. From the heath care perspective, the additional costs of PCV-13 vaccinations versus no vaccinations were $189 and 188 without or with herd protection, respectively, which resulted in ICERs of $20,709 and 18,483/QALY, respectively. From a societal perspective, the additional costs of PCV-13 vaccinations versus a no vaccination strategy were $169 and 166, without or with herd protection, respectively, which resulted in ICERs of $18,483 and 16,106 /QALY, respectively.
Table 2.
Projected base-case health outcomes and costs.
| No Vaccination | PCV-13 Vaccination | Differences | |
|---|---|---|---|
| Health outcomes | |||
| No herd protection | |||
| Probability of IPD | 0.248% | 0.203% | −0.045% |
| Mortality associated with S. pneumonia | 0.003% | 0.002% | −0.001% |
| Discount QALY | 19.669 | 19.678 | 0.009 |
| Expected LY | 73.844 | 73.854 | 0.009 |
| Herd protection | |||
| Probability of IPD | 11.765% | 11.682% | −0.083% |
| Mortality associated with S. pneumonia | 0.318% | 0.316% | −0.002% |
| Discount QALY | 1,173.497 | 1,173.508 | 0.010 |
| Expected LY | 2,957.405 | 2,957.419 | 0.013 |
| Economic outcomes | |||
| No herd protection | |||
| Discount cost ($) from the perspective of heath care | 138 | 327 | 189 |
| ICER ($/QALY) from the perspective of heath care | — | 20,709 | — |
| Discount cost ($) from the perspective of society | 478 | 646 | 169 |
| ICER ($/QALY) from the perspective of society | — | 18,483 | — |
| Herd protection | |||
| Discount cost ($) from the perspective of heath care | 4,485 | 4,673 | 188 |
| ICER ($/QALY) from the perspective of heath care | — | 18,189 | — |
| Discount cost ($) from the perspective of society | 10,127 | 10,293 | 166 |
| ICER ($/QALY) from the perspective of society | — | 16,106 | — |
Sensitivity analyses
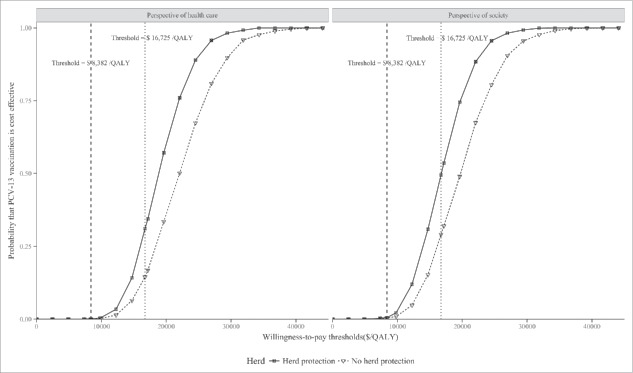
The tornado diagram shows the results of one-way sensitivity analyses with herd protection from a societal perspective (Fig. 2), which showed that the ICER of PCV13 vaccinations versus a no vaccination strategy ranged from $6,177 to 35,120 (Fig. 2). The parameters related to CAP (e.g., the annual incidence of CAP, case-fatality of hospitalized CAP and S. pneumoniae isolation rate for pneumonia) and cost of PCV-13 were identified as the key drivers of the model outputs. Other parameters, such as the utility estimates and vaccine coverage rate, only have median and small impacts.
Figure 2.
A tornado diagram for PCV13 with herd protection versus no vaccinations from a societal perspective. AOM, acute otitis media; Sp, Streptococcus pneumonia; PCV-13, 13-valent pneumococcal conjugate vaccine.
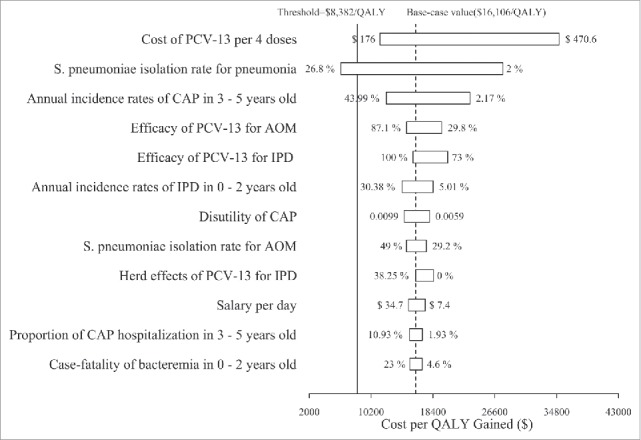
Based on the probabilistic sensitivity analyses, cost-effectiveness acceptability curves (Fig. 3) showed that the cost-effectiveness probabilities of the PCV13 vaccination were lower than 30% at the threshold of per capita GDP in China ($8,382). At the threshold of per capita GDP in Shanghai ($16,725), the cost-effective probabilities of PCV13 vaccination with or without herd protection were 31% and 50% or 15% and 29% from the perspectives of health care and society, respectively.
Figure 3.
Cost-effectiveness acceptability curves for PCV-13 and no vaccination in the perspectives of health care and society.
Discussion
To the best of our knowledge, the current economic study is the first analysis performed using the Chinese-specific price of PCV-13. The results found that at the current PCV-13 pricing and ceiling threshold, a routine vaccination program for Chinese infants would not be cost-effective throughout the country compared to a no vaccination strategy. However, in some wealthy regions in China, such as Shanghai City, introducing universal vaccination with PCV-13 might be a cost-effective option when considering herd protection or a societal perspective. Local decision makers should weigh the economic findings and affordability before implementing PCV-13.
One recent systematic review has reported that an infant PCV vaccination program was a cost-effective strategy in most low- and middle-income countries (LMICs), including 22 economic evaluations conducted in LMICs.31 The PCV-13 price per dose in LMICs varied from $3.50 in GAVI-eligible countries to $30 in GAVI-ineligible countries, except for Thailand (∼$63) and China (∼$58). Our analysis was consistent with the Thai cost-utility analysis, which showed that PCV vaccinations with PCV-10 and PCV13 are not cost-effective even when indirect vaccine effects were considered.32 The findings from the one-way sensitivity analysis indicates that the economic outcome of PCV-13 vaccination was also most sensitive to the cost of PCV-13 when the price of PCV-13 per dose discounted 50% (∼$29 per dose). One recent Chinese survey has shown that the median willingness-to-pay price for pneumococcal conjugate vaccine was $29, and 92% of respondents were not willing to pay the market price for the vaccine.33 One recent report published by Maurer KA and colleagues has reported that adding PCV-7, PCV-10, and PCV-13 through the Chinese Expanded Program on Immunization are cost-effective from a societal perspective.34 In that analysis, the vaccination cost of PCV-7, PCV-10, and PCV-13 per infant was only $148, which is the price of one dose of the vaccines. However, the pneumococcal vaccination schedule consisted of 4 doses per infant to yield the high immunogenicity.8 When the additional cost of one dose of PCV was considered in the Maurer KA and colleagues' analysis, the ICERs of vaccination program with PCV-7, PCV-10, and PCV-13 against no vaccinations were higher than the threshold of 3 × GDP of China, which indicates that the PCV vaccination program was not cost-effective in a Chinese context. Using the assumed cost of PCV-13 per course ($570), Mo X and colleagues have also found that PCV vaccinations for Chinese infants were not cost-effective, and they suggest that the price of the vaccine must be discounted and that financial support should be provided to poor families.35
By reducing the carriage of S. pneumoniae and transmission to contacts, there also has been a concordant decline in the incidence of IPD among the non-vaccinated population.36 As other published economic have reported,15,31 the herd effects of vaccinations have a substantial impact on the economic outcomes of PCV-13. When the herd effect was included, our model outputs found that the ICERs of a PCV-13 vaccination program over a no vaccination strategy become more favorable (decreasing nearly 30%) in a base-case analysis, and the probabilities of cost-effectiveness increased over 50% in PSA compared to the scenario without the herd effect. Although the herd effect PCV data are increasing,36 there is still no confirmed evidence of the impact of herd immunity of universal PCVs vaccination in East Asia, where the environmental risk factors, family structures, mixing patterns, and culture are vastly different compared with Western regions. Therefore, it is still uncertain whether to similar herd effects expand to the whole population, as described in published Western reports. However, note that the economic benefits of PCV-13 achieved through herd effects could be weakened in the regions where pneumococcal polysaccharide vaccines are introduced in adults, such as Shanghai.37 Thus, the impact of herd effects should be carefully explored.
The current analysis still suffers from several limitations, and it should be viewed from that perspective. First, due to the lack of national level epidemiological data associated with S. pneumonia diseases, the analysis incorporated data derived from Chinese Taiwan and Hong Kong surveillance data, which are subject to bias because the variations of these data in the sensitivity analyses, particularly the parameters related to CAP, had a moderate impact on the model outcomes. Thus, such findings should be carefully interpreted. Fortunately, two recent questionnaire surveys indicated that the disease burden in Chinese mainland children was likely to be higher than other regions,38,39 which indicated that PCV vaccinations might have more financial value. Second, a transmission dynamic model can capture the herd effect and serotype replacement,40 which is generally used in cost-effectiveness analyses. However, due to the absence of detailed local epidemiological data, which is more easily understood for local decision makers, a static Markov model was used in this study, and it might not accurately simulate the impact of indirect effects of vaccination and serotype replacement. Third, to simplify the model, the current analysis does not consider all diseases associated with S. pneumonia and vaccine-related adverse events, such as septic arthritis, and also consider the pneumococcal disease in the disabled population. However, because the excluded diseases or events are rare and the excluded population are paucity, the outcomes were too low to be projected by the model. Fourth, antibiotic-resistant S. pneumoniae is becoming a global problem, and the PCV vaccination program could decrease its antibiotic resistance.41 However, the present analysis did not take it into account the health benefits of a vaccination program. This conservative approach might underestimate the economic outcomes of a PCV-13 strategy. Fifth, due to not having a Chinese license, the current study did not evaluate other competitive vaccines, such as the 10-valent pneumococcal nontypeable Haemophilus influenzae protein D conjugate vaccine, which has the additional ability of protecting NTHi-related AOM compared with PCV-13. Sixth, due to lack of reliable estimates, the current analysis did not consider the long-term impact of sequelae associated with AOM as previous study done,18 which might underestimate the benefits of PCV-13 strategy. Finally, utility scores related to pneumococcal disease were extracted from literature published abroad due to the absence of local data. Fortunately, utility scores have no considerable impact on the model output. Despite these weaknesses, our analysis provides insight regarding the introduction of PCV-13 for local decision makers.
In summary, the findings of this analysis indicate that the introduction of PCV-13 in a Chinese vaccination program is not cost-effective compared to a no vaccination strategy, even when herd immunity was considered. The results of the sensitivity analyses suggest that the model outcome is sensitive to the price of PCV-13. Thus, deployment of the PCV-13 vaccine would be of value in some wealthy Chinese regions. To better inform health decision making and policy, active monitoring of the epidemiological data associated with pneumococcal disease is necessary in China.
Supplementary Material
Appendix Table 1.
Chinese epidemiological data associated with pneumococcal disease 1.
| Pneumococcal Disease | 0 – 2 year | 3 – 5 year | 5 – 17 year | 18 – 34 year | 35 – 49 year | 50 – 64 year | over 65 year |
|---|---|---|---|---|---|---|---|
| CAP | |||||||
| Annual incidence (per 10,0000) | 17695(5013 – 30377) | 23082.5(2174 – 43991) | 7229.5(227 – 14232) | 1309(109 – 2509) | 605.5(159 – 1052) | 1139(159 – 2119) | 5325(2165 – 8485) |
| Proportion of hospitalization | 0.072(0.034 – 0.109) | 0.064(0.019 – 0.109) | 0.029(0.013 – 0.045) | 0.088(0.01 – 0.166) | 0.172(0.027 – 0.317) | 0.214(0.05 – 0.378) | 0.377(0.084 – 0.67) |
| Case-fatality of hospitalized CAP | 0.021(0.002 – 0.04) | 0.021(0.002 – 0.04) | 0.003(0.002 – 0.003) | 0.004(0.001 – 0.007) | 0.025(0.017 – 0.032) | 0.031(0.025 – 0.037) | 0.058(0.052 – 0.063) |
| IPD | |||||||
| Annual incidence (per 10,0000) | 13.9(9.8 – 18) | 14.2(12.8 – 15.6) | 1.1(1 – 1.2) | 1.1(1 – 1.2) | 1.1(1 – 1.2) | 1.1(1 – 1.2) | 10(9.8 – 10.2) |
| Proportion of meningitis in IPD | 0.28(0.21 – 0.35) | 0.12(0.09 – 0.15) | 0.33(0.25 – 0.42) | 0.18(0.14 – 0.23) | 0.1(0.08 – 0.13) | 0.09(0.07 – 0.11) | 0.02(0.02 – 0.03) |
| Case-fatality of meningitis | 0.19(0.05 – 0.33) | 0.19(0.05 – 0.33) | 0.07(0.05 – 0.1) | 0.14(0.1 – 0.18) | 0.14(0.11 – 0.18) | 0.14(0.11 – 0.18) | 0.29(0.24 – 0.35) |
| Case-fatality of bacteremia | 0.14(0.05 – 0.23) | 0.14(0.05 – 0.23) | 0.14(0.05 – 0.23) | 0.15(0.13 – 0.18) | 0.15(0.13 – 0.18) | 0.15(0.13 – 0.18) | 0.24(0.13 – 0.35) |
| AOM | |||||||
| Annual incidence(per 10,0000) | 19707(16930 – 22485) | 15488(14355 – 16620) | — | — | — | — | — |
| Complex AOM |
0.104(0.104 – 0.104) |
0.11(0.11 – 0.11) |
— |
— |
— |
— |
— |
| CAP: community-acquired pneumonia; AOM: acute otitis media; IPD: invasive pneumococcal disease. | |||||||
Funding Statement
This study was supported by the Fourth Round of the Three-year Action Plan on Public Health Discipline and Talent Program (Evidence-based Public Health and Health Economics, No. 15GWZK0901) from Shanghai Health and Family Planning Commission. The funding agencies had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Disclosure of potential conflicts of interest
None of the authors have anything to declare.
Authors' contributions
Hua Zhou and Datian Che developed the economic model, performed the analyses and drafted the manuscript. Bin Wu and Datian Che contributed to the conception, design of the primarily model and interpreted the results. Hua Zhou and Jinchun He collected and reviewed data.
References
- 1.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–544. doi: 10.1016/S0140-6736(16)31012-1. PMID:27733281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T, et al.. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374:893–902. doi: 10.1016/S0140-6736(09)61204-6. PMID:19748398. [DOI] [PubMed] [Google Scholar]
- 3.Yao K-H, Yang Y-H. Streptococcus pneumoniae diseases in Chinese children: past, present and future. Vaccine. 2008;26:4425–33. doi: 10.1016/j.vaccine.2008.06.052. PMID:18602435. [DOI] [PubMed] [Google Scholar]
- 4.Ceyhan M, Ozsurekci Y, Aykac K, Hacibedel B, Ozbilgili E. Economic burden of pneumococcal infections in children under 5 years of age. Hum Vaccin Immunother. 2018;14:106–10. doi: 10.1080/21645515.2017.1371378. PMID:28922054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nunes MC, Madhi SA. Review on the immunogenicity and safety of PCV-13 in infants and toddlers. Expert Rev Vaccines. 2011;10:951–80. doi: 10.1586/erv.11.76. PMID:21806394. [DOI] [PubMed] [Google Scholar]
- 6.Ben-Shimol S, Givon-Lavi N, Leibovitz E, Raiz S, Greenberg D, Dagan R. Near-elimination of otitis media caused by 13-valent pneumococcal conjugate vaccine (PCV) serotypes in southern Israel shortly after sequential introduction of 7-valent/13-valent PCV. Clin Infect Dis. 2014;59:1724–32. doi: 10.1093/cid/ciu683. PMID:25159581. [DOI] [PubMed] [Google Scholar]
- 7.Adegbola RA, DeAntonio R, Hill PC, Roca A, Usuf E, Hoet B, Greenwood BM. Carriage of Streptococcus pneumoniae and other respiratory bacterial pathogens in low and lower-middle income countries: a systematic review and meta-analysis. PLoS ONE. 2014;9:e103293. doi: 10.1371/journal.pone.0103293. PMID:25084351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruiz-Aragón J, Márquez Peláez S, Molina-Linde JM, Grande-Tejada AM. Safety and immunogenicity of 13-valent pneumococcal conjugate vaccine in infants: a meta-analysis. Vaccine. 2013;31:5349–58. doi: 10.1016/j.vaccine.2013.09.008. PMID:24055349. [DOI] [PubMed] [Google Scholar]
- 9.Shiri T, Datta S, Madan J, Tsertsvadze A, Royle P, Keeling MJ, McCarthy ND, Petrou S. Indirect effects of childhood pneumococcal conjugate vaccination on invasive pneumococcal disease: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e51–9. doi: 10.1016/S2214-109X(16)30306-0. PMID:27955789. [DOI] [PubMed] [Google Scholar]
- 10.Che D, Zhou H, He J, Wu B. Modeling the impact of the 7-valent pneumococcal conjugate vaccine in Chinese infants: an economic analysis of a compulsory vaccination. BMC Health Serv Res. 2014;14:56. doi: 10.1186/1472-6963-14-56. PMID:24507480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E, et al.. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16:231–50. doi: 10.1016/j.jval.2013.02.002. PMID:23538175. [DOI] [PubMed] [Google Scholar]
- 12.Wang X, Wang Z-F, Xie Y-M, Zhang W, Liao X, Chang Y-P. Specialty Committee of Evaluation of Postmarketing Chinese Medicines of World Federation of Chinese Medicine Societies. Guideline for postmarketing Chinese medicine pharmacoeconomic evaluation. Chin J Integr Med. 2015;21:473–80. doi: 10.1007/s11655-014-1749-y. PMID:24671571. [DOI] [PubMed] [Google Scholar]
- 13.Wijmenga-Monsuur AJ, van Westen E, Knol MJ, Jongerius RMC, Zancolli M, Goldblatt D, van Gageldonk PGM, Tcherniaeva I, Berbers GAM, Rots NY. Direct Comparison of Immunogenicity Induced by 10- or 13-Valent Pneumococcal Conjugate Vaccine around the 11-Month Booster in Dutch Infants. PLoS ONE. 2015;10:e0144739. doi: 10.1371/journal.pone.0144739. PMID:26658902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ZHENG J, CAI B, LI B, ZHANG F, YANG Z, QI Z, LEI Y, CHEN H. Hepatitis B Vaccine Coverage Rate and Influential Factors among Children in Hubei Province. Journal of Public Health and Preventive Medicine. 2005;16:4–6. [Google Scholar]
- 15.Wu DB-C, Roberts C, Lee VWY, Hong L-W, Tan KK, Mak V, Lee KKC. Cost-effectiveness analysis of infant universal routine pneumococcal vaccination in Malaysia and Hong Kong. Hum Vaccin Immunother. 2016;12:403–16. doi: 10.1080/21645515.2015.1067351. PMID:26451658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu H, Xiao X, Lu J, Chen Z, Luo L, Yang Z. Study on epidemic characteristics and etiology of community acquired pneumonia in Guangzhou from 2009 to 2012. Zhonghua Yu Fang Yi Xue Za Zhi 2013;47:1089–94. [PubMed] [Google Scholar]
- 17.Lee KKC, Rinaldi F, Chan MKU, Chan STH, So TMT, Hon EKL, Lee VWY. Economic evaluation of universal infant vaccination with 7vPCV in Hong Kong. Value Health. 2009;12(Suppl 3):S42–48. doi: 10.1111/j.1524-4733.2009.00626.x. PMID:20586981. [DOI] [PubMed] [Google Scholar]
- 18.De Wals P, Black S, Borrow R, Pearce D. Modeling the impact of a new vaccine on pneumococcal and nontypable Haemophilus influenzae diseases: A new simulation model. Clin Ther. 2009;31:2152–69. doi: 10.1016/j.clinthera.2009.10.014. PMID:19922887. [DOI] [PubMed] [Google Scholar]
- 19.Monasta L, Ronfani L, Marchetti F, Montico M, Vecchi Brumatti L, Bavcar A, Grasso D, Barbiero C, Tamburlini G. Burden of disease caused by otitis media: systematic review and global estimates. PLoS ONE. 2012;7:e36226. doi: 10.1371/journal.pone.0036226. PMID:22558393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang J, Liu F, Ao P, Li X, Zheng H, Wu D, Zhang N, Yu J, Yuan J, Wu X. Detection of Serotype Distribution and Drug Resistance of Streptococcus Pneumoniae Isolated From Pediatric Patients. Lab Med. 2017;48:39–45. doi: 10.1093/labmed/lmw059. PMID:28039377. [DOI] [PubMed] [Google Scholar]
- 21.Huang S, Liu X, Lao W, Zeng S, Liang H, Zhong R, Dai X, Wu X, Li H, Yao Y. Serotype distribution and antibiotic resistance of Streptococcus pneumoniae isolates collected at a Chinese hospital from 2011 to 2013. BMC Infect Dis. 2015;15:312. doi: 10.1186/s12879-015-1042-5. PMID:26243258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Q, Zhang F, Zhao C, Chen H, Wang Z, Guo Y, Li H, Wang H. [Antimicrobial resistance and serotype distribution of Streptococcus pneumoniae isolated from multi-centers across China, 2010 – 2011]. Zhonghua Jie He He Hu Xi Za Zhi. 2013;36:106–12. PMID:23537554. [PubMed] [Google Scholar]
- 23.Delgleize E, Leeuwenkamp O, Theodorou E, Van de Velde N. Cost-effectiveness analysis of routine pneumococcal vaccination in the UK: a comparison of the PHiD-CV vaccine and the PCV-13 vaccine using a Markov model. BMJ Open. 2016;6:e010776. doi: 10.1136/bmjopen-2015-010776. PMID:27903558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black S, Shinefield H, Fireman B, Lewis E, Ray P, Hansen JR, Elvin L, Ensor KM, Hackell J, Siber G, et al.. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J. 2000;19:187–95. doi: 10.1097/00006454-200003000-00003. PMID:10749457. [DOI] [PubMed] [Google Scholar]
- 25.van Werkhoven CH. Herd effects of child vaccination with pneumococcal conjugate vaccine against pneumococcal non-invasive community-acquired pneumonia: What is the evidence? Hum Vaccin Immunother. 2017;13:1177–81. doi: 10.1080/21645515.2016.1264548. PMID:27937061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu B, Xu L, Cai H, Jiang L, Luo Y, Gu Y. The design of an m-Health monitoring system based on a cloud computing platform. ENTERPRISE INFORMATION SYSTEMS. 2017;11:17–36. doi: 10.1080/17517575.2015.1053416. [DOI] [Google Scholar]
- 27.Wen R, Deng Q, Sun C, Gao S, Tao J, Luo R. Pathogenic bacteria distribution and drug susceptibility in children with acute otitis media in Pearl River Delta. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011;25:884–7. PMID:22242472. [PubMed] [Google Scholar]
- 28.Bennett JE, Sumner W, Downs SM, Jaffe DM. Parents' utilities for outcomes of occult bacteremia. Arch Pediatr Adolesc Med. 2000;154:43–8. PMID:10632249. [PubMed] [Google Scholar]
- 29.Oh PI, Maerov P, Pritchard D, Knowles SR, Einarson TR, Shear NH. A cost-utility analysis of second-line antibiotics in the treatment of acute otitis media in children. Clin Ther. 1996;18:160–82. doi: 10.1016/S0149-2918(96)80188-3. PMID:8851461. [DOI] [PubMed] [Google Scholar]
- 30.Knerer G, Ismaila A, Pearce D. Health and economic impact of PHiD-CV in Canada and the UK: A Markov modelling exercise. J Med Econ. 2012;15:61–76. doi: 10.3111/13696998.2011.622323. PMID:22026590. [DOI] [PubMed] [Google Scholar]
- 31.Saokaew S, Rayanakorn A, Wu DB-C, Chaiyakunapruk N. Cost Effectiveness of Pneumococcal Vaccination in Children in Low- and Middle-Income Countries: A Systematic Review. Pharmacoeconomics. 2016;34:1211–25. doi: 10.1007/s40273-016-0439-3. PMID:27510721. [DOI] [PubMed] [Google Scholar]
- 32.Kulpeng W, Leelahavarong P, Rattanavipapong W, Sornsrivichai V, Baggett HC, Meeyai A, Punpanich W, Teerawattananon Y. Cost-utility analysis of 10- and 13-valent pneumococcal conjugate vaccines: protection at what price in the Thai context? Vaccine. 2013;31:2839–47. doi: 10.1016/j.vaccine.2013.03.047. PMID:23588084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hou Z, Null Jie Chang, Yue D, Fang H, Meng Q, Zhang Y. Determinants of willingness to pay for self-paid vaccines in China. Vaccine. 2014;32:4471–7. doi: 10.1016/j.vaccine.2014.06.047. PMID:24968160. [DOI] [PubMed] [Google Scholar]
- 34.Maurer KA, Chen H-F, Wagner AL, Hegde ST, Patel T, Boulton ML, Hutton DW. Cost-effectiveness analysis of pneumococcal vaccination for infants in China. Vaccine. 2016;34:6343–9. doi: 10.1016/j.vaccine.2016.10.051. PMID:27810315. [DOI] [PubMed] [Google Scholar]
- 35.Mo X, Tobe RG, Liu X, Mori R. Cost-Effectiveness and Health Benefits of Pediatric 23-Valent Pneumococcal Polysaccharide Vaccine, 7-Valent and Forecasting 13-Valent Pneumococcal Conjugate Vaccines in China. Pediatr Infect Dis J. 2016;35:e353–61. doi: 10.1097/INF.0000000000001288. PMID:27753771. [DOI] [PubMed] [Google Scholar]
- 36.Kim YK, LaFon D, Nahm MH. Indirect Effects of Pneumococcal Conjugate Vaccines in National Immunization Programs for Children on Adult Pneumococcal Disease. Infect Chemother. 2016;48:257–66. doi: 10.3947/ic.2016.48.4.257. PMID:28032483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao D, Gai Tobe R, Cui M, He J, Wu B. Cost-effectiveness of a 23-valent pneumococcal polysaccharide vaccine immunization programme for the elderly in Shanghai, China. Vaccine. 2016;34:6158–65. doi: 10.1016/j.vaccine.2016.11.003. PMID:27838068. [DOI] [PubMed] [Google Scholar]
- 38.Li Y, An Z, Yin D, Liu Y, Huang Z, Ma Y, Li H, Li Q, Wang H. Disease burden of community acquired pneumonia among children under 5 y old in China: A population based survey. Hum Vaccin Immunother. 2017;13:1681–7. doi: 10.1080/21645515.2017.1304335. PMID:28414567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qu F, Weschler LB, Sun Y, Sundell J. High pneumonia lifetime-ever incidence in Beijing children compared with locations in other countries, and implications for national PCV and Hib vaccination. PLoS ONE. 2017;12:e0171438. doi: 10.1371/journal.pone.0171438. PMID:28166256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu DB-C, Chang C-J, Huang Y-C, Wen Y-W, Wu C-L, Fann CS-J. Cost-effectiveness analysis of pneumococcal conjugate vaccine in Taiwan: A transmission dynamic modeling approach. Value Health. 2012;15:S15–19. doi: 10.1016/j.jval.2011.11.013. PMID:22265061. [DOI] [PubMed] [Google Scholar]
- 41.Daana M, Rahav G, Hamdan A, Thalji A, Jaar F, Abdeen Z, Jaber H, Goral A, Huppert A, Raz M, et al.. Measuring the effects of pneumococcal conjugate vaccine (PCV7) on Streptococcus pneumoniae carriage and antibiotic resistance: the Palestinian-Israeli Collaborative Research (PICR). Vaccine. 2015;33:1021–6. doi: 10.1016/j.vaccine.2015.01.003. PMID:25593104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.