ABSTRACT
Objective: Thirteen-valent pneumococcal conjugate vaccines (PCV13) was licensed for optional use in mainland China since 2017, but the uptake is low. To update the research evidence for the pneumococcal serotype distribution of pre-PCV era and to estimate the potential impact of PCVs, we performed a meta-analysis on the relevant publications concerning the Chinese population.
Methods: This systematic review and meta-analysis were conducted on the pneumococcal serotype distribution publications in mainland China from 2000 to 2016. The literature was searched in PubMed, Ovid-EMBASE, Web of Science, CNKI and Wanfang. Heterogeneity and publication bias were tested by I2, meta-regression, Egger's and Begg's test. The pneumococcal serotype and vaccine serotype coverage rates were pooled using the random-effects model in Stata SE 12.0.
Results: In total, 85 publications were included. Of all 16,945 included pneumococcal isolates, the most common serotypes/serogroups were 19F, 19A, 23F, 14, and 6B, that from children were the same as above, that from adults≥18 years were 19, 3, 6, 23, and 14. Among isolates from children <18 years, the pooled coverage for PCV10 serotypes was 52.3%, that for PCV13 was 68.4% and that for PPSV23 was 65.5%. Regarding individuals ≥18 years, the pooled coverage for PCV10 serotypes was 29.7%, that for PCV13 was 49.5% and that for PPSV23 was 50.7%. Serotype prevalence and vaccine serotype coverage varied by age group, source, and region.
Conclusions: The most common pneumococcal serotype in mainland China was 19F. The serotype coverage rates of PCV13 and PPSV23 were 50%–68% in mainland China.
KEYWORDS: Streptococcus pneumoniae, serotype, pneumococcal conjugate vaccine, pneumococcal polysaccharide vaccine, China
Introduction
Streptococcus pneumoniae is an important cause of community acquired infections and is associated with significant morbidity and mortality worldwide. By the end of the 20th century, pneumonia was the first and second leading cause of death among children aged under 5 years in the rural and urban areas of China, respectively.1 S. pneumoniae causes at least 18% of severe episodes and 33% of deaths from pneumonia worldwide.2 The burden of invasive pneumococcal diseases (IPD) has decreased substantially due to the widespread usage of pneumococcal conjugate vaccines (PCVs) worldwide.3,4 However, S. pneumoniae still poses a significant burden on individuals and healthcare systems because of the high costs of PCVs and the serotype shift after immunization.5
S. pneumoniae has more than 90 serotypes, which vary by age and different regions. Only when the distribution of S. pneumoniae and the serotype coverage of PCVs or pneumococcal polysaccharide vaccine (PPSV) are well-known can useful information be offered to guide the vaccination program. In mainland China, 7-valent pneumococcal conjugate vaccine (PCV7) was licensed as type II self-paid vaccine for optional use in 2008 but the extent of adoption was very low. PCV13 has been licensed for optional use since November 2016. However, it won't be widely used due to low awareness and high price. In 2013, WHO provided a new plan that the completed vaccination coverage rate of PCVs should reach 90% to avoid severe pneumonia in children by 2025.6 Before the use of PCV13 around China, it is important to update the research evidence for pneumococcal disease. Currently, many papers have reported on pneumococcal serotypes in mainland China, but there is a lack of evidence of the pneumococcal serotype distribution countrywide and in all age groups. A recently published manuscript has reviewed the pneumococcal serotype distribution and coverage among Chinese children, but they did not include isolates from adults or provide detailed information regarding the serotype distribution and vaccine serotype coverage by age group.7 Thus, to provide a comprehensive view of the pneumococcal isolate characteristics and estimate the potential impact of vaccines in China, we performed a systematic review and meta-analysis of publications on serotype distributions of pneumococcal infections in mainland China from 2000 to 2016.
Results
Literature characteristics
In total, 1,848 potentially related articles were identified, and 384 articles were duplicated. Of these articles, 123 were identified as potentially relevant articles according to the screening of the titles and abstracts. Six articles were excluded because they were reviews, 16 articles shared the same data, and 4 articles had a sample size that was too small. Finally, 85 articles were included in our meta-analysis (Fig. 1). The characteristics of the included articles were listed in Table 1. The regional distribution of the enrolled articles and pneumococcal isolates are shown in Fig. 2.
Figure 1.
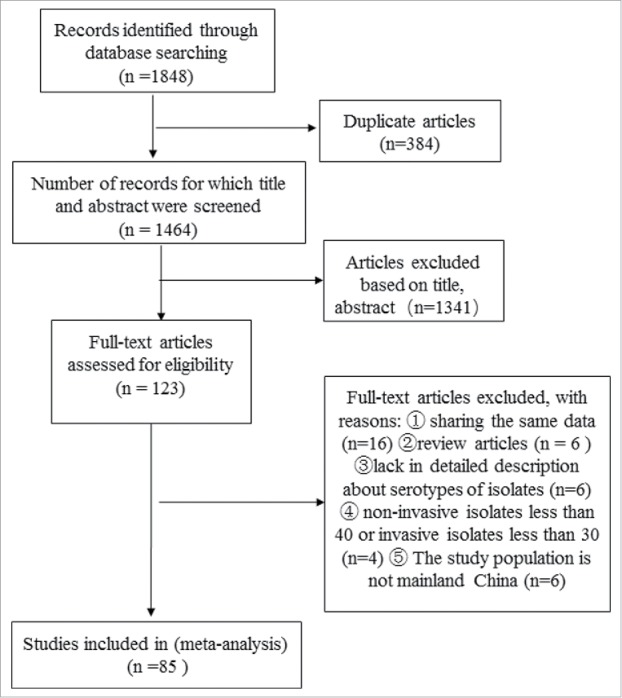
Selection of Articles for Meta-analysis.
Table 1.
Characteristics of the included studies published from 2000 to 2016 in mainland China.
| Vaccine Coverage Rate a |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First Author | Study Year | Age (y or m) | Location in China | Source | Number of strains | Serotype method | PCV10 | PCV13 | PCV23 | |
| South | ||||||||||
| Yang F20 | 1996–1999 | All age | Shanghai | Non-invasive | 111 | Quellung | 50.5% | 71.2% | 70.3% | |
| Yang F21 | 1997–1998 | ≤5 y | Shanghai | Non-invasive | 222 | Quellung | 56.8% | 73.9% | 60.8% | |
| Li ZF22 | 1999–2001 | 2–14 y | Guangzhou | Non-invasive | 84 | Quellung | 32.1% | 46.4% | 39.3% | |
| Zhao GM23 | 2000-2001 | ≤3 y | Shanghai | Non-invasive+invasive | 112 | Quellung | 72.3% | 81.3% | 72.3% | |
| Wang CQ24 | 2000–2001 | <18 y | Shanghai | Non-invasive | 96 | Quellung | 61.5% | 71.9% | 62.5% | |
| Wang CQ25 | 2000-2002 | 1m-15 y | Shanghai | Non-invasive | 111 | Quellung | 64.9% | 74.8% | 64.9% | |
| Luo XM26 | 2003 | All age | Zhongshan | Non-invasive | 266 | Quellung | 37.6% | 53.0% | 48.1% | |
| Sun ZY27 | 2003-2004 | <5 | Wuhan | Non-invasive | 133 | Quellung | 5.3% | 6.0% | 6.0% | |
| Zhang J28 | 2004 | unknown | Wuhan | Non-invasive | 152 | Quellung | 4.6% | 6.6% | 7.2% | |
| Zhang J29 | 2004 | <18 y | Wuhan | Non-invasive | 114 | Quellung | 6.1% | 7.0% | 7.0% | |
| Liu YK30 | 2004-2005 | All age | Wuhan | Non-invasive | 304 | Quellung | 4.6% | 6.6% | 7.2% | |
| Yang F31 | 2004–2005 | >18 y;<12 y | Shanghai | Non-invasive | 103 | Quellung, PCR | 71.8% | 84.5% | 86.4% | |
| Ren HY32 | 2004–2006 | <18 y | Chengdu | unknown | 123 | Quellung | 52.0% | 60.2% | 68.3% | |
| Zhang XH33 | 2004–2009 | ≥18 y | Hunan | Non-invasive+invasive | 822 | Quellung | 5.1% | 20.6% | 20.6% | |
| Pan W34 | 2005–2012 | <18 y | Nanjing | invasive strain | 155 | Quellung | 61.3% | 80.6% | 85.8% | |
| Yang T35 | 2005–2013 | All age | Guangdong | Non-invasive+invasive | 383 | Quellung | 16.4% | 21.9% | 21.9% | |
| Zhao RZ36 | 2006–2007 | ≤5 y | Shenzhen | Non-invasive+invasive | 90 | Quellung | 95.6% | 98.9% | 100.0% | |
| Deng QL37 | 2006-2007 | 1m一6 y | Guangzhou | Non-invasive | 79 | Quellung | 94.9% | 94.9% | 97.5% | |
| Dong YS38 | 2006–2008 | All age | Chongqing | Non-invasive+invasive | 143 | Quellung | 8.4% | 10.5% | 15.4% | |
| Dong YS39 | 2006–2008 | unknown | Chongqing | Non-invasive+invasive | 133 | Quellung | 4.5% | 4.5% | 4.5% | |
| Zhang H40 | 2007–2008 | ≤5 y | Shanghai | Non-invasive | 338 | Quellung | 57.7% | 81.1% | 80.5% | |
| Xu F41 | 2007–2010 | <18 y | Nanjing | invasive | 48 | Quellung | 70.8% | 93.8% | 95.8% | |
| Miao DQ42 | 2007–2011 | <18 y | Nanjing | Non-invasive+invasive | 323 | PCR | 44.0% | 73.7% | 62.8% | |
| Hu JY43 | 2009 | 12–18 m | Shanghai | Non-invasive | 102 | Quellung | 63.7% | 77.5% | 71.6% | |
| Zhao DF44 | 2009 | 12–18 m | Wuhan | Non-invasive | 75 | Quellung | 38.7% | 54.7% | 46.7% | |
| Zhang C45 | 2009–2010 | All age | Sichuan | Non-invasive+invasive | 166 | Quellung | 10.2% | 12.0% | 16.9% | |
| Li JP46 | 2009–2010 | <18 y | Zhejiang | Non-invasive | 106 | Quellung | 59.4% | 95.3% | 92.5% | |
| Ying QH47 | 2009–2010 | All age | Shaoxing | Non-invasive+invasive | 103 | Quellung | 62.1% | 62.1% | 62.1% | |
| Zhang B48 | 2009-2010 | All age | Chongqing | Non-invasive+invasive | 91 | Quellung, PCR | 61.5% | 75.8% | 81.3% | |
| Chen DL49 | 2009-2011 | All age | Maanshan | Non-invasive+invasive | 80 | Quellung | 55.0% | 83.8% | 82.5% | |
| Ma X50 | 2009-2012 | <14 y | Shenzhen | invasive | 87 | Quellung | 72.4% | 81.6% | 81.6% | |
| Lin XF51 | 2009-2013 | ≥18 y | Wenzhou | invasive | 52 | Quellung | 59.6% | 90.4% | 86.5% | |
| Zhou K52 | 2009-2013 | <12 y | Nanjing | invasive | 51 | Quellung | 76.5% | 96.1% | 98.0% | |
| Jing CM53 | 2009-2014 | <18 y | Chongqing | Non-invasive+invasive | 600 | Quellung | 53.0% | 62.8% | 62.8% | |
| Kang LH54 | 2010-2013 | ≤11 y | Chongqing | Non-invasive+invasive | 83 | Quellung, PCR | 51.8% | 79.5% | 73.5% | |
| Lu C55 | 2010-2013 | ≤14 y | Shenzhen | invasive | 76 | Quellung | 72.4% | 94.7% | 97.4% | |
| Liu MJ56 | 2010-2013 | ≤11 y | Chongqing | Non-invasive+invasive | 46 | PCR | 52.2% | 84.8% | 78.3% | |
| Song XQ57 | 2010-2014 | 0-6 y | Taizhou | Non-invasive | 322 | Quellung | 82.9% | 95.7% | 95.7% | |
| Li M58 | 2011-2012 | ≤5 y | Humen | Non-invasive | 229 | Quellung | 95.2% | 97.4% | 97.8% | |
| Huang SY59 | 2011-2013 | All age | Guangzhou | Non-invasive+invasive | 94 | Quellung | 50.0% | 67.0% | 67.0% | |
| Ding YF60 | 2011-2013 | < 18 y | Suzhou | Non-invasive | 79 | PCR | 55.7% | 93.7% | 93.7% | |
| Jiang QH61 | 2011-2013 | >18 y | Shanghai | Non-invasive+invasive | 37 | Quellung, PCR | 37.8% | 48.6% | 51.4% | |
| Wang JR62 | 2011-2014 | 0-107m | Wenling | unknown | 284 | Quellung | 60.6% | 85.9% | 80.6% | |
| Wang LM63 | 2011-2015 | 0-6 y | Jinhua | Non-invasive | 302 | Quellung | 83.8% | 97.7% | 97.7% | |
| Li ST64 | 2012 | 1-10 y | Nanjing | Non-invasive | 584 | Quellung | 64.7% | 92.3% | 96.4% | |
| Fen P65 | 2012 | 0-14 y | Shanghai | Non-invasive | 328 | Quellung, PCR | 58.2% | 84.1% | 77.4% | |
| Yuan YT66 | 2012-2013 | <7 y;>50 y | Xiamen | Non-invasive+invasive | 265 | Quellung | 62.6% | 77.4% | 67.5% | |
| Geng Q67 | 2012-2013 | ≤5 y | Suzhou | Non-invasive | 175 | PCR | 66.3% | 84.6% | 84.6% | |
| Fen P68 | 2013 | ≤14 y | Shanghai | Non-invasive+invasive | 284 | Quellung, PCR | 58.1% | 81.0% | 79.9% | |
| Peng YJ69 | 2015 | ≤12 y | Chongqing | Non-invasive | 267 | Quellung | 49.1% | 72.7% | 66.7% | |
| North | ||||||||||
| Yu SJ70 | 1997 | ≤5 y | Beijing | Non-invasive | 190 | Quellung | 31.6% | 44.7% | 31.6% | |
| MCGEE L 71 | 1997-1998 | ≤5 y | Beijing | Non-invasive | 376 | Quellung | 47.1% | 74.7% | 55.1% | |
| Li J72 | 1999 | ≤5 y | Beijing | Non-invasive | 97 | Quellung | 8.2% | 10.3% | 11.3% | |
| Yao KH73 | 2000-2002 | <5 y | Beijing | Non-invasive | 63 | Quellung | 4.8% | 4.8% | 6.3% | |
| Yao KH74 | 2000-2004 | ≤5 y | Beijing | Non-invasive | 129 | Quellung | 7.0% | 7.0% | 7.8% | |
| Yu S75 | 2000-2005 | ≤5 y | Beijing | Non-invasive | 519 | Quellung | 8.3% | 8.5% | 11.6% | |
| Tong YJ76 | 2004 | ≤5 y | Beijing | Non-invasive | 137 | Quellung | 10.2% | 10.2% | 14.6% | |
| Wu JX77 | 2008-2010 | ≤6 y | Linyi | Non-invasive | 124 | Quellung | 29.8% | 48.4% | 71.8% | |
| Liu CF78 | 2009-2011 | 3m-5 y | Shenyang | invasive | 61 | Quellung | 52.5% | 93.4% | 100.0% | |
| Zhou L79 | 2010 | ≤5 y | Beijing | Non-invasive | 140 | Quellung | 37.1% | 44.3% | 37.1% | |
| Wang TW80 | 2010-2013 | ≤5 y | Dalian | Non-invasive | 131 | PCR | 60.3% | 60.3% | 60.3% | |
| Cao XH81 | 2012 | <18 y | Luohe | Non-invasive+invasive | 134 | Quellung | 48.5% | 48.5% | 59.0% | |
| Li J82 | 2012-2014 | <18 y | Beijing | Non-invasive+invasive | 103 | Quellung | 59.2% | 86.4% | 80.6% | |
| Liu ZW83 | 2013-2014 | ≤3 y | Taian | Non-invasive+invasive | 320 | Quellung | 75.0% | 82.8% | 75.0% | |
| Dong F84 | 2013-2014 | <18 y | Beijing | Non-invasive+invasive | 258 | Quellung | 43.0% | 65.5% | 64.0% | |
| Yao KH85 | 2013-2014 | ≤14 y | Beijing | Non-invasive+invasive | 187 | Quellung | 25.7% | 55.1% | 46.0% | |
| Yu SJ86 | 2013-2014 | ≤16 | Beijing | Non-invasive | 100 | Quellung | 39.0% | 51.0% | 44.0% | |
| Zhou MJ87 | 2013-2015 | All age | Baoding | Non-invasive+invasive | 210 | PCR | 35.2% | 62.9% | 51.9% | |
| Wang Q88 | 2013-2016 | 3m一7.5 y | Beijing | invasive | 30 | Quellung | 56.7% | 96.7% | 93.3% | |
| Wang JF89 | 2014 | <18 y | Zhengzhou | Non-invasive+invasive | 134 | Quellung | 48.5% | 48.5% | 59.0% | |
| Wang YT90 | 2014 | ≤8 y | Hebei | invasive | 43 | PCR | 48.8% | 65.1% | 67.4% | |
| Zhang M91 | 2014-2015 | <18 y | Jinan | Non-invasive | 42 | Quellung | 9.5% | 9.5% | 23.8% | |
| Multicenter | ||||||||||
| Yao KH92 | 2000-2002 | <5 y | Multicenter | Non-invasive | 625 | Quellung | 6.6% | 6.6% | 6.6% | |
| Li MC93 | 2004-2009 | unknown | Multicenter | unknown | 144 | Quellung | 8.3% | 9.0% | 10.4% | |
| Li MC94 | 2004-2011 | unknown | Multicenter | Non-invasive+invasive | 241 | Quellung | 58.9% | 76.8% | 74.3% | |
| Liu YD95 | 2005-2006 | ≤4 y | Multicenter | Non-invasive+invasive | 451 | Quellung | 63.6% | 75.4% | 75.4% | |
| Xiao SK96 | 2005-2008 | All age | Multicenter | Non-invasive+invasive | 580 | Quellung | 31.7% | 52.6% | 52.6% | |
| Liu CL97 | 2005-2008 | All age | Multicenter | invasive | 148 | Quellung | 36.5% | 67.6% | 66.2% | |
| Zhao CJ98 | 2005-2011 | All age | Multicenter | Non-invasive+invasive | 240 | Quellung | 34.6% | 63.8% | 63.8% | |
| Yao KH99 | 2006-2007 | ≤5 y | Multicenter | Non-invasive+invasive | 279 | Quellung | 81.4% | 92.8% | 93.9% | |
| Yao KH100 | 2006-2008 | ≤5 y | Multicenter | Non-invasive+invasive | 338 | Quellung | 74.0% | 87.9% | 87.9% | |
| Ma X101 | 2006-2008 | <14 y | Multicenter | invasive | 171 | Quellung | 63.2% | 80.7% | 80.7% | |
| Zhang YJ102 | 2007-2011 | All age | Multicenter | Non-invasive+invasive | 39 | Quellung | 64.1% | 87.2% | 89.7% | |
| Chen C103 | 2008-2010 | unknown | Multicenter | Non-invasive+invasive | 277 | Quellung | 45.5% | 51.6% | 64.6% | |
| Wang Q104 | 2010-2011 | All age | Multicenter | Non-invasive+invasive | 471 | Quellung | 39.1% | 67.5% | 62.6% | |
Notes:
Vaccine Coverage Rate was calculated as the percentage of isolates from each study that belonged to the serogroups/serotypes included in the PCVs.
Figure 2.
The regional distribution of enrolled studies and pneumococcal isolates.
Of the included articles, 72 articles used the capsular Quellung test for serotyping, 7 used multiplex PCR, 6 used both capsular Quellung test and multiplex PCR; 58 articles only included isolates from children, and 3 articles only reported isolates from adults; 12 articles studied the invasive isolates, and 32 reported both invasive and non-invasive isolates.
Pneumococcal serotypes
Pneumococcal isolates
In total, 16,945 S. pneumoniae isolates were eventually included in this meta-analysis; 11,987 (70.7%) isolates were from children younger than 18 years, 1,963 (11.6%) isolates were from adults, and the other 2,995 isolates were from children or adults. There were 896 (5.3%) invasive isolates, 7,577 (44.7%) non-invasive isolates (the stratification analysis on invasive / non-invasive isolates were only done for children), and the other 8,503 isolates could not be stratified. Stratifying by geographical regions, 9,442 (55.7%) strains were from the south, 3,608 (21.3%) strains were from the north, and the other 3,895 isolates were from multicenter that could not be stratified.
Serotype distribution and vaccine serotype coverage
Of all the included isolates, the most common serotypes were 19F, 19A, 23F, 14, 6B, 6A, 3, 15B, 9V, and 5. The main difference of serotype distribution between children and adults was that serotype 3 was more prevalent in adults than in children. For those isolated from sterile sites in children, the most common serotypes/serogroups were 19F, 19A, 14, 23F, and 6B. Although serotype 19A and serotype 14 were more prevalent in invasive strains than in non-invasive strains, serotype 6A in invasive strains was far less than in non-invasive strains.
Fifty-five point seven percent of the included isolates were from the south of mainland China, and 21.3% were from the north. Serotype 19A and serotype 6B were more prevalent in south region than in north region, though fewer strains of serotype 6A in south region. (Table 2).
Table 2.
Serotype distribution and vaccine-serotype coverage of the pneumococci isolated from 2000 to 2016 in mainland China.
| Strains | Serotype /Serogroup | Number (n) | Proportion (%) | 95% CI | I2(%) a | P b |
|---|---|---|---|---|---|---|
| Strains from children<18y (N = 11,711) | ||||||
| 19F | 3487 | 29.8 | 28.3–30.0 | / | / | |
| 19A | 1192 | 10.2 | 9.3–10.4 | / | / | |
| 23F | 1089 | 9.3 | 8.6–9.7 | / | / | |
| 14 | 859 | 7.3 | 7.9–8.9 | / | / | |
| 6B | 581 | 5.0 | 6.8–7.7 | / | / | |
| 6A | 500 | 4.3 | 3.9–4.6 | / | / | |
| 19 | 446 | 3.8 | 3.5–4.2 | / | / | |
| 23 | 280 | 2.4 | 2.1–2.7 | / | / | |
| 6 | 277 | 2.4 | 2.1–2.6 | / | / | |
| 15 | 207 | 1.8 | 1.5–2.0 | / | / | |
| PCV10 | / | 52.3 | 44.3–60.3 | 99.1 | <0.001 | |
| PCV13 | / | 68.4 | 60.8–76. | 99.5 | <0.001 | |
| PPSV23 | / | 65.5 | 58.0–73.0 | 99.4 | <0.001 | |
| Strains from adults≥18y (N = 1,963) | ||||||
| 19 | 248 | 12.6 | 11.2–14.1 | / | / | |
| 3 | 242 | 12.3 | 10.9–13.8 | / | / | |
| 6 | 178 | 9.1 | 7.8–10.3 | / | / | |
| 19F | 172 | 8.8 | 7.5–10.0 | / | / | |
| 23 | 146 | 7.4 | 6.3–8.6 | / | / | |
| 19A | 122 | 6.2 | 5.1–7.3 | / | / | |
| 14 | 106 | 5.4 | 4.4–6.4 | / | / | |
| 23F | 71 | 3.6 | 2.8–4.4 | / | / | |
| 15 | 52 | 2.6 | 1.9–3.4 | / | / | |
| 17 | 25 | 1.3 | 0.8–1.8 | / | / | |
| PCV10 | / | 29.7 | 19.2–40.3 | 97.0 | <0.001 | |
| PCV13 | / | 49.5 | 32.6–66.3 | 98.6 | <0.001 | |
| PPSV23 | / | 50.7 | 34.6–66.9 | 98.3 | <0.001 | |
| Invasive strains (N = 896) | ||||||
| 19F | 210 | 23.5 | 20.6–26.3 | / | / | |
| 19A | 201 | 22.2 | 19.4–25.0 | / | / | |
| 14 | 146 | 16.4 | 13.9–18.9 | / | / | |
| 23F | 59 | 6.7 | 5.0–8.4 | / | / | |
| 6B | 44 | 5.1 | 3.6–6.6 | / | / | |
| 9V | 32 | 3.6 | 2.4–4.8 | / | / | |
| 1 | 17 | 1.9 | 1.0–2.8 | / | / | |
| 8 | 15 | 1.7 | 0.8–2.5 | / | / | |
| 7F | 13 | 1.5 | 0.7–2.2 | / | / | |
| 5 | 10 | 1.1 | 0.4–1.8 | / | / | |
| PCV10 | / | 61.4 | 55.2–67.7 | 70.6 | <0.001 | |
| PCV13 | / | 87.4 | 82.7–92.0 | 79.4 | <0.001 | |
| PPSV23 | / | 86.9 | 81.7–92.2 | 84.6 | <0.001 | |
| Non-invasive strains (N = 7,577) | ||||||
| 19F | 2,006 | 26.5 | 25.5–27.5 | / | / | |
| 19A | 637 | 8.4 | 7.8–9.0 | / | / | |
| 23F | 600 | 7.9 | 7.3–8.5 | / | / | |
| 14 | 499 | 6.6 | 6.0–7.1 | / | / | |
| 19 | 439 | 5.8 | 5.3–6.3 | / | / | |
| 6A | 371 | 4.9 | 4.4–5.4 | / | / | |
| 6B | 350 | 4.6 | 4.1–5.1 | / | / | |
| 23 | 299 | 3.9 | 3.5–4.4 | / | / | |
| 6 | 241 | 3.2 | 2.8–3.6 | / | / | |
| 15 | 171 | 2.3 | 1.9–2.6 | / | / | |
| PCV10 | / | 43.2 | 33.2–53.2 | 99.4 | <0.001 | |
| PCV13 | / | 55.7 | 43.5–67.8 | 99.7 | <0.001 | |
| PPSV23 | / | 53.4 | 41.5–65.3 | 99.7 | <0.001 | |
| Strains from the south of China(N = 9,442) | ||||||
| 19F | 2452 | 26.0 | 25.1 -26.9 | / | / | |
| 19A | 852 | 9.0 | 8.4 -9.6 | / | / | |
| 23F | 811 | 8.6 | 8.0 -9.2 | / | / | |
| 19 | 747 | 7.9 | 7.4–8.5 | / | / | |
| 14 | 609 | 6.4 | 6.0–6.9 | / | / | |
| 6B | 452 | 4.8 | 4.4–5.2 | / | / | |
| 6 | 382 | 4.0 | 3.6–4.4 | / | / | |
| 6A | 348 | 3.7 | 3.3–4.1 | / | / | |
| 23 | 312 | 3.3 | 2.9–3.7 | / | / | |
| 3 | 237 | 2.5 | 2.2–2.8 | / | / | |
| PCV10 | / | 50.1 | 40.5–59.6 | 98.2 | <0.001 | |
| PCV13 | / | 64.5 | 54.8–74.2 | 99.3 | <0.001 | |
| PPSV23 | / | 62.8 | 53.2–72.4 | 98.7 | <0.001 | |
| Strains from the north of China (N = 3,608) | ||||||
| 19F | 508 | 14.1 | 12.9–15.2 | / | / | |
| 23F | 343 | 9.5 | 8.5–10.5 | / | / | |
| 19 | 289 | 8.0 | 7.1–8.9 | / | / | |
| 14 | 264 | 7.3 | 6.5–8.2 | / | / | |
| 6A | 233 | 6.5 | 5.7–7.3 | / | / | |
| 19A | 191 | 5.3 | 4.6–6.0 | / | / | |
| 23 | 143 | 4.0 | 3.3–4.6 | / | / | |
| 6 | 113 | 3.1 | 2.6–3.7 | / | / | |
| 6B | 105 | 2.9 | 2.4–3.5 | / | / | |
| 15 | 92 | 2.5 | 2.0–3.1 | / | / | |
| PCV10 | / | 36.3 | 26.7–45.9 | 98.2 | <0.001 | |
| PCV13 | / | 50.5 | 36.2–64.8 | 99.3 | <0.001 | |
| PPSV23 | / | 47.8 | 35.7–59.9 | 98.7 | <0.001 |
Notes:
I2 means the total variation across studies that were due to heterogeneity.
P: The Cochran chi-square (χ2) test of Heterogeneity. A P value of <0.05 was considered statistically significant.
/: Not applicable.
During 1996–1999, the most prevalent serotypes/serogroups were 23F, 6A, 19F, 14, and 6B; during 2005–2009 and 2010–2016, the most prevalent serotypes/serogroups were 19F, 19A, 23F, 14, and 6B. The major changes were the increased frequency of serotype 19A and 19F since 2000–2004. Fig. 3 shows the distribution of vaccine serotypes of pneumococcal isolates from 1996 to 2016 in mainland China.
Figure 3.
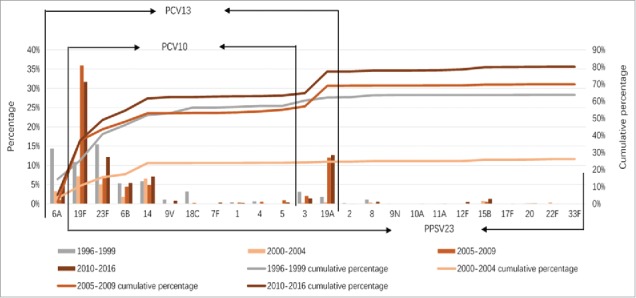
Distribution of vaccine serotypes of pneumococcal isolates from 1996 to 2016 in mainland China.
The range of pooled coverage for PCV10 serotypes was from 29.7% to 62.3%, that for PCV13 was 43.2%–61.4%, and that for PPSV23 was 50.7%–65.5%, depending on different age groups. For different sources, the pooled coverage for PCV10 serotypes ranged from 43.2% to 61.4%, that for PCV13 ranged from 55.7% to 87.4%, and that for PPSV23 ranged from 62.8% to 86.9%. Regarding to different regions, the pooled coverage for PCV10 serotypes varied from 36.3% to 50.1%, that for PCV13 varied from 50.5% to 64.5%, and that for PPSV23 varied from 47.8% to 62.8%. (Table 2) Before 2004, the pooled coverage rates for vaccines serotypes were very low, which were 24.9% (95% CI: 14.8%–35.0%) for PCV10 serotypes, 29.6% (95% CI: 16.2%–43.0%) for PCV13 and 27.1% (95% CI: 15.8%–38.4%) for PPSV23. Since 2005, the pooled coverage for vaccines serotypes increased gradually. During 2010–2016, the pooled coverage for PCV10 serotypes was 54.4% (95% CI: 46.5%–62.3%), that for PCV13 was 73.3% (95% CI: 67.8%–78.8%) and that for PPSV23 was 71.6% (95% CI: 65.9%–77.2%). (Fig. 3)
Heterogeneity and meta-regression
We noticed high heterogeneity between studies (I2 = 70.6%–99.7%) (Table 2). We performed meta- regression analysis and used variables, including age (<18 y vs ≥18 y) region (northern vs southern), source (invasive vs non-invasive), serotype method (PCR vs Quellung), number of strains, and study year. In univariate analysis, we noticed that regions (p = 0.003) and study year (p = 0.016) were associated with the coverage rate of PCV13 serotypes. However, in multivariable analysis, regions, sources and study years explained 41% of the total heterogeneity. (Table 3)
Table 3.
Results of Meta-regression for pneumococcal serotype coverage of PCV13 in mainland China from 2000 to 2016.
| Covariatea | Meta-regression Coefficient | 95% Confidence Interval | P value | Adj R-squaredb |
|---|---|---|---|---|
| Univariate analyses | ||||
| Age (<18y vs ≥18y) | –0.268 | –0.944 to 0.407 | 0.427 | –0.92% |
| Region (northern vs southern) | 0.355 | 0.133 to 0.578 | 0.003 | 25.37% |
| Source (invasive vs non-invasive) | 0.273 | –0.142 to 0.689 | 0.188 | 2.82% |
| Serotype (PCR vs Quellung) | –0.077 | –0.399 to 0.246 | 0.629 | –2.70% |
| Number of strains | 0.000 | –0.001 to 0.001 | 0.663 | –2.13% |
| Study year | –0.515 | –0.865to –0.166 | 0.005 | 35.80% |
| Multivariable analyses | 41.18% | |||
| Age (<18y vs ≥18y) | 0.076 | –0.474 to 0.626 | 0.780 | |
| Region (northern vs southern) | 0.345 | 0.174 to 0.516 | <0.001 | |
| Source (invasive vs non-invasive) | 0.331 | 0.021 to 0.641 | 0.037 | |
| Serotype (PCR vs Quellung) | –0.142 | –0.385 to 0.100 | 0.241 | |
| Number of strains | 0.001 | –0.000 to 0.001 | 0.092 | |
| Study year | –0.370 | –0.665 to -0.076 | 0.016 |
Notes:
The dependent variance of the Meta-regression was the serotype coverage rate (r) of PCV13. The covariates included in the univariate and multivariable models were age (<18 y vs ≥18y), region (northern vs southern), source (invasive vs non-invasive), serotype (PCR vs Quellung), number of strains, and study year.
Adj R-squared was the proportion of variance that can be explained.
Discussion
Of the currently available data from the published papers, serotype 19F pneumococcus was the most common cause of invasive and non-invasive pneumococcal disease (PD) in mainland China, followed by serotype 19A pneumococcus. Among children aged <18 years, serotype 19F pneumococcus was the main cause of IPD, a finding that was different from Johnson's finding that serotype 14 pneumococcus was the most common cause of IPD in Africa, Asia, Europe, and North America etc.8 Thus, the most common serotypes causing IPD may vary slightly across geographic regions.
Among the strains isolated from children aged younger than 18 years, serotypes 19F, 19A and 23F were the most common serotypes, results that were similar to those of Lyu et al.7 In addition, serotype 23F, 14 and 6B were important causes of either PD or IPD in children. This finding was consistent with the results from Western Europe and the USA that serogroups 14, 23, and 6 were common serogroups.9 However, among the strains isolated from adults, the most common serotypes/serogroups were 19, followed by 3, and 6. Similarly, several studies in Asia reported that the prevalence of serotype 3 increased from 14.3% to 24.3 % in adults and even became the most prevalent among patients aged older than 65 years.10,11 Thus, the prevalent serotypes may vary among age groups. The most prevalent serotypes were similar in the north and south, and serotype/serogroup 19F (or 19) was the most frequent in the various regions, though the rate of each serotype is different. Additionally, serotype19A is more frequent in the south than in the north. Thus, the serotypes of S. pneumonia vary in different areas.
For all of the isolates included in our study, the coverage rates of PCV13 and PPSV23 were significantly higher than those of PCV10, with no significant differences between PCV13 and PPSV23, a finding that was s consistent with other study findings in China.7,12 Although the number of serotypes in PPSV23 was more than that in PCV13, the serotype coverage of PPSV23 was slightly lower than that of PCV13, potentially due to the lack of serotype 6A in PPSV23 and the contribution of serotype 6A is higher than the combined contribution of the 11 serotypes unique to PPSV23. PCV13 has higher coverage compared with PCV7,13 and the additional serotypes 1, 5, 7F, 3, 6A and 19A, especially for serotype 19A, account for a large proportion. In our study, PCVs or PPSV coverage among children was higher than that among adults, consistent with the results of a study from China.14 Among the isolates from children, PCVs or PPSV coverage of invasive isolates was higher than that of non-invasive isolates. In the USA, the rate of IPD reduced dramatically after 5 years since the license of PCV13, especially driven by decreases in 19A.15 Considering the comprehensive evidence concerning the effectiveness of PCV13 we could expect a similar reduction of IPD if we have a high vaccination rate of PCV13 in mainland China.
In mainland China, PCV7 was licensed since 2008 and PCV13 was licensed since 2016, but both as self-paid vaccine and the extent of adoption was very low. Thus the natural fluctuation in serotype distribution in China for the last 20 years appears to not have significantly influenced from PCVs introductions. The major changes were the increasing of serotype 19A and 19F since 2000–2004, which may have been mainly due to the selective pressure of antibiotics usage. In the USA, the non-PCV7 serotype 19A increased in prevalence from 2.7% in 1999–2000 to 34.1% in 2010–2011 after 10 years of PCV7 licensed, but these serotype fluctuations have been mainly attributed to serotype replacement following PCV7 immunization.16,17
In other countries, serotype shift is a phenomenon since the use of PCV7.13,14 Although PCV7 is not widely used in China, the increasing of serotype19A was obvious since 2000, and serotype 19A is one of the most common serotypes in most areas of China.15 The serotype shift in China may be due to the selective pressure of antibiotics rather than the use of PCV7, because of the antibiotics were commonly used in China. In the future, we need to keep monitoring the serotype distribution and change.
There are some limitations in this systematic review and meta-analysis. First, we used different thresholds for a number of invasive (>30) and of non-invasive isolates (>40), which might lead to some bias. In consideration of the common usage of antibiotics, lower bacterial load and the quality of the specimens, it's more difficult to isolate the invasive pneumococcal strains in the fields, but the invasive pneumococcal diseases are more severe than non-invasive pneumococcal diseases. Therefore, we used a lower threshold for invasive isolates to include more meaningful data in this meta-analysis. Second, we observed large heterogeneity of the included articles, but regions, sources, and study years only explained part of the observed heterogeneity, other possible reasons remain unknown. Third, serotype coverage of vaccines may be underestimated in our study, because only serotypes were used in the pooled coverage regardless of serogroup data. Furthermore, most of the included studies came from southeastern of mainland China; few came from northwestern provinces, such as Xinjiang, Qinghai and Ningxia province. To better understand the impact of PCV13 on these areas, more data are needed.
In conclusion, pneumococcal serotype 19F was the most prevalent serotype in mainland China, and the most common serotypes varied among the population, between invasive and non-invasive isolates, and across geographic regions. The serotype coverage rates of PCV13 and PPSV23 were high in mainland China. During and after the introduction of PCV13 in China, more scientific data are required, especially from northwestern China; the serotype distribution should be monitored over an extended time period.
Methods
Literature search
A systematic literature search was conducted in PubMed, Ovid-EMBASE, Web of Science, CNKI, and Wanfang. We searched electronic medical databases for studies (published between January 1, 2000 and December 31, 2016) reporting pneumococcal serotypes from hospitalization patients or isolates from healthy people in mainland China. Strategies were designed to retrieve records that included the following terms: (“Streptococcus pneumoniae” OR “S. pneumoniae” OR “pneumococcus” OR “pneumococci” OR “diplococcus pneumoniae” OR “diplococcus” OR “pneumococcal”) and (“serotype” OR “serotypes” OR “serogroups” OR “serogroup”) and (“China” OR “Chinese”)
Criteria for selection
We included an article if (1) It was an original study, and the isolates were serotyped by multiplex polymerase chain reaction or capsular Quelling reaction methods; (2) the number of isolates was ≥30 for invasive isolates or ≥ 40 for non-invasive isolates; and (3) the strains were isolated from the population in mainland China (except Hong Kong, Macao and Taiwan). We excluded an article if (1) it was a review, case report or lecture; (2) it lack a detailed description about the serotypes of the isolates; (3) it was a duplicate publication. For more detailed information, please refer to Fig. 1.
Data extraction
The following information was extracted from each selected paper: first author's name, study region, age of study population, source of isolates, years of isolates collected, number of isolates, and the serotypes.
Invasive pneumococcal isolates were defined as S. pneumoniae strains identified from a normally sterile site (e.g., blood, cerebrospinal, pleural effusions, or joint fluid, etc.). Non-invasive pneumococcal strains were defined as S. pneumoniae strains isolated from non-sterile sites such as sputum or middle ear effusion. Vaccine serotypes referring to the serotypes included in the pneumococcal conjugate vaccines or pneumococcal polyvalent vaccine (details in Box 1).
Box 1. Serotypes in Pneumococcal conjugate vaccines or polysaccharide vaccine
| PCV7 | 4 | 6B | 9V | 14 | 18C | 19F | 23F | ||||||||||||||||
| PCV10 | 4 | 6B | 9V | 14 | 18C | 19F | 23F | 1 | 5 | 7F | |||||||||||||
| PCV13 | 4 | 6B | 9V | 14 | 18C | 19F | 23F | 1 | 5 | 7F | 3 | 19A | 6A | ||||||||||
| PPSV23 | 4 | 6B | 9V | 14 | 18C | 19F | 23F | 1 | 5 | 7F | 3 | 19A | 2 | 8 | 9N | 10A | 11A | 12F | 15B | 17F | 20 | 22F | 33F |
Data analysis
The collected isolates were stratified by the properties of each study into children or adults, invasive isolates or non-invasive isolates, southern or northern regions. Southern or northern regions were defined by Qinling Mountains and Huai River.
I2 was used to describe the percentage of the total variation across studies that were due to heterogeneity. I2 = 25% was associated with low heterogeneity, I2 = 50% was associated with moderate heterogeneity, and I2 = 75% was associated with high heterogeneity.18 Two-sided p ≤ 0.05 was considered statistically significant.19 Most of our meta-analysis, showed high heterogeneity (I2>75%). Considering the high heterogeneity among studies, we used the random-effects models for the pooled estimation of the serotype coverage rate of PCVs.
To explore which study characteristics explained the large heterogeneity, meta-regression was conducted according to potentially relevant characteristics.
The PCV serotype coverage rate (r) was calculated as the total number of isolates included in the vaccine serotypes divided by the total number of isolates that were serotyped. The standard error (SE) of the coverage rate was calculated as SE = Sqr(r*(1-r)/n). The coverage rate of PCVs from different studies were pooled with using the random-effects model.
All statistical analyses were performed using Stata SE 12.0 (Stata Corp, College Station, TX).
Funding Statement
This study was supported by the National Natural Science Foundation of China [81102166], the Shanghai Municipal Health and Family Planning [GWTD2015S05 and 15GWZK0101], the National Key Research and Development Program of China (2017YFC0211700) and the SINO-US collaborative program on Emerging and Re-Emerging Infectious Diseases [5U2GGH000018].
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.He C, Kang L, Miao L, Li Q, Liang J, Li X, Wang Y, Zhu J. Pneumonia Mortality among Children under 5 in China from 1996 to 2013: An Analysis from National Surveillance System. PLoS One. 2015;10(7):e0133620. doi: 10.1371/journal.pone.0133620. PMID:26186717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker CL, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, O'Brien KL, Campbell H, Black RE. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–16. doi: 10.1016/S0140-6736(13)60222-6. PMID:23582727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902. doi: 10.1016/S0140-6736(09)61204-6. PMID:19748398. [DOI] [PubMed] [Google Scholar]
- 4.Organization WH. Estimated Hib and Pneumococcal Deaths for Children Under 5 Years of Age, 2008. 2013. [Google Scholar]
- 5.Balsells E, Guillot L, Nair H, Kyaw MH. Serotype distribution of Streptococcus pneumoniae causing invasive disease in children in the post-PCV era: A systematic review and meta-analysis. PLOS ONE. 2017;12(5):e0177113. doi: 10.1371/journal.pone.0177113. PMID:28486544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization [WHO] ; United Nations Children's Fund [UNICEF. Ending preventable child deaths from pneumonia and diarrhoea by 2025. The integrated Global Action Plan for Pneumonia and Diarrhoea (GAPPD).[J]. Geneva Switzerland Who, 2013. [Google Scholar]
- 7.Lyu S, Hu HL, Yang YH, Yao KH. A systematic review about Streptococcus Pneumoniae serotype distribution in children in mainland of China before the PCV13 was licensed. Expert Rev Vaccines. 2017;16(10):1–10. [DOI] [PubMed] [Google Scholar]
- 8.Johnson HL, Deloria-Knoll M, Levine OS, Stoszek SK, Freimanis HL, Reithinger R, Muenz LR, O'Brien KL. Systematic evaluation of serotypes causing invasive pneumococcal disease among children under five: the pneumococcal global serotype project. PLoS Med. 2010;7(10):e1000348. doi: 10.1371/journal.pmed.1000348. PMID:20957191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hausdorff WP, Siber G, Paradiso PR. Geographical differences in invasive pneumococcal disease rates and serotype frequency in young children. Lancet. 2001; 357:950–2. doi: 10.1016/S0140-6736(00)04222-7. PMID:11289365. [DOI] [PubMed] [Google Scholar]
- 10.Kawaguchiya M, Urushibara N, Aung MS, Shinagawa M, Takahashi S, Kobayashi N. Serotype distribution, antimicrobial resistance and prevalence of pilus islets in pneumococci following the use of conjugate vaccines. J Med Microbiol. 2017;66(5):643–650. doi: 10.1099/jmm.0.000479. PMID:28516842. [DOI] [PubMed] [Google Scholar]
- 11.Miyazaki H, Shibuya R, Midorikawa N, Chang B, Ohnishi M, Matsumoto T. Serotype distribution and antimicrobial susceptibility of Streptococcus pneumoniae strains isolated in Japan after introduction of the routine immunization program. J Infect Chemother. 2017;23(4):234–240. doi: 10.1016/j.jiac.2016.12.016. PMID:28161295. [DOI] [PubMed] [Google Scholar]
- 12.Yao KH, Yang YH. Streptococcus pneumoniae diseases in Chinese children: past, present and future. Vaccine. 2008;26(35):4425–33.1999-2011(1.). Emerg Infect Dis. 2013 Jul;19(7):1074-83. doi: 10.1016/j.vaccine.2008.06.052. PMID:18602435. [DOI] [PubMed] [Google Scholar]
- 13.Eliakim M, Levy M, Ehrenfeld M, Reimann HA. Resurgence of the multiresistant pneumococcus in the United States: a commentary. Pediatr Infect Dis J. 2007;26(6):473–474. doi: 10.1097/INF.0b013e3180517b8b. PMID:17529861. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan SL, Barson WJ, Lin PL, Stovall SH, Bradley JS, Tan TQ, Hoffman JA, Givner LB, Mason EOJ. Serotype 19A is the most common serotype causing invasive pneumococcal infections in children. Pediatrics. 2010;125(3):429. doi: 10.1542/peds.2008-1702. PMID:20176669. [DOI] [PubMed] [Google Scholar]
- 15.Balsells E, Guillot L, Nair H, Kyaw MH. Serotype distribution of Streptococcus pneumoniae causing invasive disease in children in the post-PCV era: A systematic review and meta-analysis. PLOS ONE. 2017;12(5):e0177113. doi: 10.1371/journal.pone.0177113. PMID:28486544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butler JC. Epidemiology of pneumococcal serotypes and conjugate vaccine formulations. Microb Drug Resist. 1997 Summer;3(2):125–9. doi: 10.1089/mdr.1997.3.125. [DOI] [PubMed] [Google Scholar]
- 17.Sandra S. Richter, Kristopher P. Heilmann, Cassie L. Dohrn, Fathollah Riahi, Daniel J. Diekema, Gary V. Doern. Pneumococcal serotypes before and after introduction of conjugate vaccines, United States 1999-20111. Emerg Infect Dis. 2013;19(7):1074–83. doi: 10.3201/eid1907.121830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. PMID:12958120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology. 2000;53(11):1119–1129. * Reference of included publications showed in Talbe1: doi: 10.1016/S0895-4356(00)00242-0. PMID:11106885. [DOI] [PubMed] [Google Scholar]
- 20.Yang F, Zhang YY. Drug resistance of Streptococcus pneumoniae isolated from respiratory tract infection. Chinese Journal of anti infection chemotherapy. 2001;1(01):13–16.. [Google Scholar]
- 21.Yang F, Zhang YY, Lesley M, Avril W, Keith K, Wu WH, Zhou L, Zhu DM, Wang F. Population biology of Streptococcus pneumoniae carried by healthy children in Shanghai. Natl Med J China. 2001;81(10):16–19 [PubMed] [Google Scholar]
- 22.Li ZF, Pan SG, Li HW. Drug resistance and serological characteristics of Streptococcus pneumoniae in children. Practical Preventive Medicine. 2002;9(02):115–118. [Google Scholar]
- 23.Zhao GM, Black S, Shinefield H, Wang CQ, Zhang YH. Serotype distribution and antimicrobial resistance patterns in Streptococcus pneumoniae isolates from hospitalized pediatric patients with respiratory infe… Pediatric Infectious Disease Journal. 2003;22(8):739–742. doi: 10.1097/01.inf.0000078373.54515.40. PMID:12913778. [DOI] [PubMed] [Google Scholar]
- 24.Wang CQ, Wang AM, Zhang YH, Zhao GM, Wang DM. Serotyping and resistance of streptococcus pneumoniae isolates from children with respiratory tract infection. Chinese Journal of Infection and Chemotherapy. 2002;2(04):218–220. [Google Scholar]
- 25.Wang CQ, Wang DM, Wang AM. Study on drug resistance of respiratory tract pathogens in 2000∼2002 years. Chinese Journal of laboratory medicine. 2004, 27(2):114–116. [Google Scholar]
- 26.Luo XM, Gu YC, Liang JP, Gao SZ, Li ZQ, Zhou RD. Investigation of drug resistance and serotype distribution of Streptococcus pneumoniae. Practical preventive medicine. 2003;10(06):835–837. [Google Scholar]
- 27.Zhang ZY, Zhang J, Li L, Zhu XH, Wang HW, Ma Y. Epidemiological study of streptoccoccus pneumoniae in the nasopharynx of healthy children under 5 years of age in Wuhan. Chinese Journal of Pediatrics. 2007;45(05):382–386. [PubMed] [Google Scholar]
- 28.Zhang J, Sun ZY, Ma Y, Li JY, Jin SH. Resistance and Serotype of 152 Strains of Streptococcus pneumoniae. Chin J N osocomiol. 2007;17(04):468–471. [Google Scholar]
- 29.Zhang J, Sun ZY. Population biology of streptococcus pneumoniae carried by healthy children. Chinese Journal of Infection and Chemotherapy. 2007;7(02):96–100. [Google Scholar]
- 30.Liu YK. Study on the Serotyping and Resistance to erythromycin of Streptococcus pneumoniae in Wuhan. Journal of Xiangnan University(Medical Sciences). 2006;8(03):4−6+9. [Google Scholar]
- 31.Yang F, Xu XG, Yang MJ, Zhang YY, Klugman KP, McGee L. Antimicrobial susceptibility and molecular epidemiology of Streptococcus pneumoniae isolated from Shanghai, China. Int J Antimicrob Agents. 2008;32(5):386–91. doi: 10.1016/j.ijantimicag.2008.05.004. PMID:18723327. [DOI] [PubMed] [Google Scholar]
- 32.Ren HY, Wang XL, Li MC, Zhang L, Gao Y, Shao ZJ. Resistance and Serotype of 123 Strains of Streptococcus Pneumoniae. Chinese Journal oF Vaccines and Immunization. 2010;16(01):52–55. [PubMed] [Google Scholar]
- 33.Zhang XH, Serotype/serogroup distribution of Streptococcus pneumoniae isolated from clinical patients and surveillance on antimicrobial resistance in 2004—2009, Drug Evaluation Research. 2011;34(02):101–104. [Google Scholar]
- 34.Pan W, Yue YL. Serotype distribution and drug resistance of children with invasive Streptococcus pneumoniae in Nanjing. Zhejiang Clin Med J. 2014;16(11):1811–1812. [Google Scholar]
- 35.Yang T, Li BS, Ke BX, Zeng HH, Peng TH, Ke CW, Wang JJ. Serological typing of Streptococcus pneumoniae clinical isolates from 2005 to 2013 in Guangdong Province. Guangdong Medical Journal. 2015;36(16):2568–2570. [Google Scholar]
- 36.Zhao RZ, Zheng YJ, Deng QL, Wang HM, Chen Q, Deng JG. Serotype/serogroup distribution and antimicrobial resistance of Streptococcus pneumoniae in children with community—acquired pneumonia in Shenzhen area. Chin J Infect Chemother. 2010;10(03):205–208. [Google Scholar]
- 37.Deng QL, Deng L, Hhuang XQ, Xie YQ, Huang Y, Zhou ZW, Yu JL, Zhao CA. Serotype Distribution and Antibiotic Resistance of Streptococcus pneumoniae Isolated from Children in Guangzhou. Journal of Tropical Medicine. 2008;8(11):1130–1133. [Google Scholar]
- 38.Dong YS, Huang WX, Zhang C, Luo T, Zhu WM, Li CZ, Zhang XP. Resistance and serotype of Streptococcus pneumoniae isolated from clinical patients in Chongqing. Chinese Journal of antibiotics. 2010;35(01):59–64. [Google Scholar]
- 39.Dong YS, Huang WX, Luo T, Zhang C, Wu LX. Prevalence of virulence genes in Streptococcus pneumoniae straias isolated from clinical patients. Chin J Microbiol Immunol. 2009;29(2):177–180. [Google Scholar]
- 40.Zhang H, Li WH, Kong J, Wang C, Lu M, Lu Q. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolated from the children in Shanghai. Chin J Infect Chemother. 2011;11(04):287–290. [Google Scholar]
- 41.Xu F, Chi FL, Tan H, Liu XM, Cao T, Pan W, Zhong TY. Study on serotype distribution in 48 isolates of invasive Streptococcus pneumoniae with which children infected. Chinese Journal of biochemical medicine. 2012;33(06):909−910+912. [Google Scholar]
- 42.Miao DQ, Xu F, Li JQ, Liu JJ, Shao ZQ, Zhu T, Zhong TY. Serotype distribution of streptococcus pneumoniae from children's clinical isolates in Nanjing. China Medical Engineering. 2016;24(02):12–15 [Google Scholar]
- 43.Hu J., Sun X., Huang Z., Wagner A. L., Carlson B., & Yang J., Tang S, Li Y, Boulton ML, Yuan Z. (2016). Streptococcus pneumoniae and haemophilus influenzae type b carriage in chinese children aged 12–18 months in shanghai, china: a cross-sectional study. Bmc Infectious Diseases, 16(1), 149. doi: 10.1186/s12879-016-1485-3. PMID:27080523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhao DF, Hu Q, Xiong Y, Quan YX, Ai YS, Wang JK. Study on the carrying rate and serotype distribution of streptococcus pneumoniae of healthy infants in Wuhan. Modern Preventive Medicine. 2012;39(09):2166–2168. [Google Scholar]
- 45.Zhang C, Dong YS, Huang WX. Streptococcus pneumonia distributed in different serotypes isolated from children and adults, and their antibiotic sensitivity:A study in Zigong, Sichuan. Journal of practical hospital clinical. 2012;9(01):82–85. [Google Scholar]
- 46.Li JP, Ye Q, Shrn YF, Lou YF, Chrn XJ, Hhua CZ, Shang SQ, Chen ZM. Drug resistance and serotype of Streptococcus pneumoniae in children's Hospital of Zhejiang University in 2009∼2010. Chinese Journal of Pharmaceuticals. 2012;47(10):792–795. [Google Scholar]
- 47.Ying QH, Yang L, Ding JL, Song XH, Ma YY, Du W. Serotype distribution and antimicrobial resistance patterns of Streptococcus pneumoniae isolates in Shaoxing area. Chinese Journal of Health Laboratory Technology. 2012;22(01):155–157. [Google Scholar]
- 48.Zhang B, Gertz R, Liu Z, Li Z, Fu W, Beall B.. Characterization of highly antimicrobial-resistant clinical pneumococcal isolates recovered in a Chinese hospital during 2009 – 2010. Journal of Medical Microbiology. 2012;61: 42–48. doi: 10.1099/jmm.0.035675-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen DL, Li MC, Zhou HJ, Liu GJ, Wang Y, Yu BQ, Shi MM, Chen XF, Hong Y. Study of molecular of 80 clinical streptococcus pneumoniae strains in Maanshan area. Chinese Journal of Preventive Medicine. 2015;49(1):56–59. PMID:25876497. [PubMed] [Google Scholar]
- 50.Ma X., Zhao R., Ma Z., Yao KH., Yu S, Zheng Y., Yang Y. Serotype distribution and antimicrobial resistance of streptococcus pneumoniae isolates causing invasive diseases from shenzhen children's hospital. Plos One. 2013;8(6), e67507. doi: 10.1371/journal.pone.0067507. PMID:23840728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin XF, Liu CX, Yang HW, Li FQ, Li XY, Yang JH. Study of serotype distribution and antimicrobial resistance in 52 isolates of invasive Streptococcus pneumoniae. Chin J Health Lab Tec. 2015;25(02):281–283. [Google Scholar]
- 52.Zhou K, Xie GJ, Wang XW, Xu F, Yao KH. Clinical characteristics and serotype distribution of invasive pneumococcal disease. Chinese Journal of hospital infection. 2015;25(15):3392–3394. [Google Scholar]
- 53.Jing CM, Wang C Resistance and serotype of Streptococcus pneumoniae isolates from children in Chongqing from 2009 to 2014, Chinese Journal of antibiotics. 2016;41(01):64–69. [Google Scholar]
- 54.Kang LH, Liu MJ, Xu WC, Cui JJ, Zhang XM. Molecular epidemiology of pneumococcal isolates from children in China. Saudi Medical Journal. 2016;37(4):403–13. doi: 10.15537/smj.2016.4.14507. PMID:27052283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lu C. Investigation of serotype distribution of invasive Streptococcus pneumoniae in children. International Journal of Laboratory Medicine. 2015;36(07):990–992. [Google Scholar]
- 56.Liu MJ, Zhang Q, Wang H. Analysis for serotypes of 46 strains of invasive Streptococcus pneumoniae and their conservation of virulence factors. Chin J Clin Lab Sci. 2013;31(12):934–937. [Google Scholar]
- 57.Song XQ, Duan DR, Lan JX. Serotype and drug resistance of Streptococcus pneumoniae from preschool children with suppurative otitis media. Chinese Journal of Microecology. 2015;27(07):819–823. [Google Scholar]
- 58.Li M, Tan DD, Zhang QT, Zhou Y, Li W, Guo WT, Guo JJ. Seotype distribution and antimicrobial resistance of streptococcus pneumoniae in children in humen area. Chinese Journal of infection and chemotherapy. 2015;15(01):43–46. [Google Scholar]
- 59.Huang S, Liu X, Lao W, Zeng S, Liang H, Zhong R, Dai X, Wu X, Li H, Yao Y. Serotype distribution and antibiotic resistance of Streptococcus pneumoniae isolates collected at a Chinese hospital from 2011 to 2013. BMC Infectious Diseases. 2015;15(1):312. doi: 10.1186/s12879-015-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ding Y, Geng Q, Tao Y, Lin Y, Wang Y. Etiology and Epidemiology of Children With Acute Otitis Media and Spontaneous Otorrhea in Suzhou, China. Pediatric Infectious Disease Journal. 2015;34:e102–e106. doi: 10.1097/INF.0000000000000617. PMID:25379833 [DOI] [PubMed] [Google Scholar]
- 61.Jiang HQ, Chen ML, Li TM, Tian YR, Zhu YJ, Liu H, Li M. Molecular characteristics of Streptococcus pneumoniae in Shanghai, China. Chin J Lab Med. 2015;38(4):256–261. [Google Scholar]
- 62.Wang J, Liu F, Ao P, Li X, Zheng H. Detection of Serotype Distribution and Drug Resistance of Streptococcus Pneumoniae Isolated From Pediatric Patients. Laboratory Medicine. 2016;48(1):39–45. [DOI] [PubMed] [Google Scholar]
- 63.Wang LM, Wu JQ, Fang YF. Epidemiological characteristics and drug resistance changes of Streptococcus pneumoniae in lower respiratory tract infection of preschool children. Chin J Health Lab Tec. 2016;26(09):1349–1352. [Google Scholar]
- 64.Li ST, Yue YL, Sun H, Tang YY, Chen HB, Serotype / serogroup distribution of Streptococcus pneumoniae isolated from sputum of 584 clinical isolates of children Int J Lab Med, September 2014;35(18):2565–2566. [Google Scholar]
- 65.Pan F, Han L, Kong J, Wang C, Qin H, Xiao S, Zhu J, Zhang H. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae causing noninvasive diseases in a Children's Hospital, Shanghai. The Brazilian Journal of Infectious Diseases. 2015;19(2):141–145. doi: 10.1016/j.bjid.2014.08.010. PMID:25636183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang LH, Yuan YT, Wang YF, Zhang JM, Zhang J, Huang JW. Clinical characteristics, serotype and drug resistance of 265 clinical isolates of Streptococcus pneumoniae. Fujian Medical Journal. 2015;37(03):78–81. [Google Scholar]
- 67.Geng Q, Zhang T, Ding Y, Tao Y, Lin Y, Wang Y, Black S, Zhao G. Molecular characterization and antimicrobial susceptibility of Streptococcus pneumoniae isolated from children hospitalized with respiratory infections in Suzhou, China. PLoS One. 2014;9:e93752.. doi: 10.1371/journal.pone.0093752. PMID:24710108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pan F, Han L, Huang W, Tang J, Xiao S, Wang C, Qin H, Zhang H. Serotype Distribution, Antimicrobial Susceptibility, and Molecular Epidemiology of Streptococcus pneumoniae Isolated from Children in Shanghai, China. PLOS ONE. 2015;10(11):e0142892. doi: 10.1371/journal.pone.0142892. PMID:26571373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen CZ, Shi W, Peng YJ, Xiong W, Yuan L, Gao W, Cheng XP, Yao KH. Nasopharyngeal carriage rate, serotype distribution and antibiotic resistance pattern of streptococcus pneumoniae isolates collected from hospitalized children with respiratory tract infections in a single center grade two hospital in western of china: a cross -sectional study. Chinese Journal of Evidence Based Pediatrics. 2016;11(4):241–246. [Google Scholar]
- 70.Yu SJ, Wang JF, Li J, Li Y, Wang XL, Whitney CG, Levine OS, Dowell SF, Yang YH. Resistance, serotypes and “hidden resistant clones” of Streptococcu pneumoniae among children in Beijing. Chin J Pediatr. 2000;38(07):23–26. [Google Scholar]
- 71.Lesley M, Wang H, Avril W, Robin H, Chen M, Klugman KP. Prevalence of SerotypesMolecular Epidemiology of Streptococcus pneumoniae Strains Isolated from Children in Beijing, China: Identification of Two Novel Multiply-Resistant Clones. Microbial Drug Resistance. 2001;7(1):55. [DOI] [PubMed] [Google Scholar]
- 72.Li J, Yuan L, Yu S, Yang Y. Nasal carriage of Streptococcus pneumoniae among children in Beijing. Chin Med J (Engl). 2001;114(11):1196–200. PMID:11729519. [PubMed] [Google Scholar]
- 73.Yao KH, Yu SJ, Shen XZ. Serotype distribution and homology of penicillin insensitive Streptococcus pneumoniae in children from 2000 to 2002 in Beijing. Chin J Microbiol Immunol. 2007, 27(10):960–961. [Google Scholar]
- 74.Yao KH, Shen XZ, Yu SJ, Tong YJ, Gao W, Yuan L, YANG YH. The serotype distribution of penicillin-nonsusceptible streptococcus pneumoniae isolated from children with upper respiratory tract infection in Beijing. Journal of Clinical Pediatrics. 2007;25(4):306–308. [Google Scholar]
- 75.Yu S, Yao K, Shen X, Zhang W, Liu X, Yang Y. Serogroup distribution and antimicrobial resistance of nasopharyngeal isolates of Streptococcus pneumoniae among Beijing children with upper respiratory infections (2000–2005). European Journal of Clinical Microbiology & Infectious Diseases. 2008;27(8):649–655. doi: 10.1007/s10096-008-0481-y. [DOI] [PubMed] [Google Scholar]
- 76.Tong YJ, Yao KH, Yu SJ. Serotyping/Grouping and Antimicrobial Resistance of Streptococcus Pneumoniae With Upper Respiratory Infection. Chinese Journal of Vaccines and Immunization. 2007, 13(1):75–78. [Google Scholar]
- 77.Wu JX, Zhu DQ, Drug resistance and molecular epidemiology of Streptococcus pneumoniae. International Journal of Laboratory Medicine. 2012;33(3):345–347. [Google Scholar]
- 78.Winkler M, Ringe B, Schneider K, Maibücher A, Färber L, Wietholtz H, Manns M, Pichlmayr R. Serotypes and patterns of antibiotic resistance in strains causing invasive pneumococcal disease in children less than 5 years of age. Plos One. 2013;8(1):e54254. doi: 10.1371/journal.pone.0054254. PMID:23342111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhou L, Yu S, Gao W, Yao K, Shen A, Yang Y. Serotype distribution and antibiotic resistance of 140 pneumococcal isolates from pediatric patients with upper respiratory infections in Beijing, 2010. Vaccine. 2011;29(44):7704–7710. doi: 10.1016/j.vaccine.2011.07.137. PMID:21839135. [DOI] [PubMed] [Google Scholar]
- 80.Wang YW, Niu M. Serotype distribution and antimicrobial susceptibility of streptococcus pneumoniae isolated from the children in Dalian. Chinese Journal of Laboratory Diagnosis. 2014;18(11):1793–1796. [Google Scholar]
- 81.Dou HJ, Gu CG, Cao XH. Drug resistance and serological typing of Streptococcus pneumoniae in pediatric patients. Chinese Journal of disinfection. 2015(01):76–77. [Google Scholar]
- 82.LI J, Ma LJ, Shi W, Zhou L, Xu WJ, Yao KH, Wang LP. Analysis of serotypes and drug resistance of Streptococcus pneumoniae in hospitalized children. Chin J Lab Med. 2015;38(9):622–626. [Google Scholar]
- 83.Liu ZW. Streptococcus pneumoniae serotype and antibiotic resistance in children with respiratory tract infection. Chinese Journal of science and technology database, medical. 2015;0(31):273–273. [Google Scholar]
- 84.Dong F, Zhen JH, Wang Y, Xu BP, Wang Q, Liu G, Yao KH, Song WQ, Shen KL. Analysis of features of streptococcus pneumoniae isolated from the cultured bacteria sample in pediatric patients. Chinese Journal of Practical Pediatrics. 2016;31(03):201–205. [Google Scholar]
- 85.Lyu S, Yao K, Dong F, Xu B, Liu G, Wang Q, Shi W, Tong J, Shen K, Yang Y. Vaccine Serotypes of Streptococcus pneumoniae with High-level Antibiotic Resistance Isolated More Frequently Seven Years After the Licensure of PCV7 in Beijing. The Pediatric Infectious Disease Journal. 2016;35(3):316–321. doi: 10.1097/INF.0000000000001000. PMID:26584056. [DOI] [PubMed] [Google Scholar]
- 86.Yu SJ, Gao W, Shi W, Yuan L, Shen AD, Yao KH, Yang YH. Nasopharyngeal carriage rate, antimicrobial resistance and serotype distribution of Streptococcus pneumoniae among children with upper respiratory infection. Chin J Contemp Pediatr. 2014;16(10):988–992. [PubMed] [Google Scholar]
- 87.Zhou MJ, Li JJ, Zhang L, Wang H, Zhang L, Jia ZY, He BH, Su W, Zheng LW, Sun YQ. Genotyping and drug resistance of Streptococcus pneumoniae in Baoding City. J Med Pest Control. 2016;32(08):854−856+859. [Google Scholar]
- 88.Wang Q, Wu J, Liu J, Dong F, Yao KH, Shen KL, Qian SY. Cliuleal features and outcomes of invasive pneumococeal disease in pediatric intensive care unit. Chinese Journal of Applied Clinical Pediatrics. 2016;31(18):1400–1404. [Google Scholar]
- 89.Wang JF, Huang NN, Wang GZ, Yu FQ. Drug resistance profileserotype of streptococcus of pneumoniae infected pediatric patients. Pakistan Journal of Pharmaceutical Sciences. 2016;29(4 Suppl):1457. [PubMed] [Google Scholar]
- 90.Wang YT, Guo YH, Wang XI, Jia ZY, Zhang WC, Sun YQ, He BH, Liu XL. Serotype Analysis of 43 Strains of Invasive Streptococcus pneumoniae Isolated in Hebei Province, 2014. Chinese Journal of Vaccines and Immunization. 2016;22(01):6–9. [Google Scholar]
- 91.Zhang M, Sun M, Chen K, Yang HX, Hou Q. Serotyping and multilocus sequence typing of Streptococcus pneumoniae in infants with ocular infections. Chin J Nosocomiol. 2016;26(14):3316–3318 [Google Scholar]
- 92.Yao KH, Lu Q, Deng L, Yu SJ, Deng QL, Tong YJ, Gao W, Yuan L, Sheng XZ, Yang YH, serotype distribution and resisitance to β-lactams of streptococcus pnemoniae isolated from children in Beijing, Shanghai, Guangzhou, 2000–2002. CHIN J Pediatr. 2006;44(12):928–932. [PubMed] [Google Scholar]
- 93.Li MC, Zhang Q, Ren HY, Zhou HJ, Li Q, Shao ZJ. Analysis on Pneumococcus Isolated from Part of China Using Serotype and Pulsed-Field Gel Electrophoresis. Chinese Journal of Vaccines and Immunization. 2010;16(03):265–269. [PubMed] [Google Scholar]
- 94.Li MC, Ren HY, Zhu BQ, Shao ZJ. Study on the Antibiotic Resistance and Serotype of 241 Strains of Streptococcus Pneumoniae. Chinese Journal of Vaccines and Immunization. 2013;19(04):336–340. [Google Scholar]
- 95.Ying QH, Yang L, Ding JL, Song XH, Ying-Ying MA, Wei DU. Serotype distribution and antimicrobial resistance patterns of Streptococcus pneumoniae isolated from children in China younger than 5 years. Chinese Journal of Health Laboratory Technology. 2012;22(01):155–157. [Google Scholar]
- 96.Xiao SK, Zhao CJ, Liu CL, Wang H. Resistance and serotype distribufion of Streptococcus pneumoniae among adults and children in China. Chinese Journal of tuberculosis and respiratory. 2010;33(8):601–607. [PubMed] [Google Scholar]
- 97.Liu CL, Zhao CJ, Liu YD, Wang H. Study of serotype distdbufion, antimicrobial resistance patterns and molecular epidemiology in 148 isolates of invasive Streptococcus pneumoniae. Chinese Medical Journal. 2010;90(22):1565–1570. PMID:20973240. [PubMed] [Google Scholar]
- 98.Zhao C, Zhang F, Chu Y, Liu Y, Cao B, Chen M, Yu Y, Liao K, Zhang L, Sun Z, et al. Phenotypic and genotypic characteristic of invasive pneumococcal isolates from both children and adult patients from a multicenter surveillance in China 2005–2011. PLoS One. 2013;8(12):e82361. doi: 10.1371/journal.pone.0082361. PMID:24349263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yao KH, Wang LB, Zhao GM, Zheng YJ, Deng L, Zhao RZ, Deng QL, Hu YH, Yu SJ, Shen XZ. Study on antimicrobial resistance in different serotypes of Streptococcus pneumoniae isolated from pediatric patients hospitalized for pneumonia. J Clin Pediatr. 2009;27(06):524−527+533. [Google Scholar]
- 100.Yao KH, Wang LB, Zhao GM, Zheng YJ, Deng L. Pneumococcal serotype distribution and antimicrobial resistance in Chinese children hospitalized for pneumonia. Vaccine. 2011;9(12):2296–301. doi: 10.1016/j.vaccine.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 101.Xiang MA, Yao KH, Xie GL, Zheng YJ, Wang CQ. Characterization of erythromycin-resistant Streptococcus pneumoniae isolates causing invasive diseases in Chinese children. National Medical Journal of China. 2013;126(8):1522–7. [PubMed] [Google Scholar]
- 102.Zhang YJ, Chen YS, Wang ZW, Li YQ, Wang DX, Shang Y, Fu RR, Hu YH, Geng R, Wei LP and others. Serological and molecular capsular typing, antibiotic susceptibility and multilocus sequence typing of Streptococcus pneumoniae isolates from invasive and non-invasive infections. Chin Med J (Engl). 2013;126(12):2296–303. PMID:23786942. [PubMed] [Google Scholar]
- 103.Chen C, Xiao L, Shi JC, Wang SS, Guo SY, Ye Q. Identifcation and Serotyping Result Analysis of 277 Strains of Streptococcus Pneumoniae. Chinese Journal of Medicinal Guide. 2011;13(10):1774–1775. [Google Scholar]
- 104.Wang Q, Zhang FF, Zhao CJ, Chen HB, Wang ZW, Guo Y, Li HN, Wang H. Antimicrobial resistance and serotype distribufion of Streptococcus pneumoniae isolated from multicenter across China, 2010-2011. Chinese Journal of tuberculosis and respiratory, Chinese Journal of tuberculosis and respiratory. 2013;36(2):106–112. [PubMed] [Google Scholar]



