Abstract
Objective
In this study, we aimed to estimate the updated incidence and mortality rate of stomach cancer based on the cancer registration data in 2014, collected by the National Central Cancer Registry of China (NCCRC).
Methods
In 2017, 339 registries’ data were qualified based on the criteria of data quality control of the NCCRC. Cases of stomach cancer were retrieved from the national database. We estimated numbers of stomach cancer cases and deaths in China using age-specific rates and corresponding national population stratified by area, sex, age-group (0, 1–4, 5–9, 10–14, …, 85+). Chinese standard population in 2000 and Segi’s world population were applied for age-standardized incidence and mortality rates.
Results
In 2014, 410,400 new stomach cancer cases and 293,800 cancer-associated deaths were estimated to have occurred in China. The crude incidence rate of stomach cancer was 30.00/100,000, age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) were 19.62/100,000 and 19.51/100,000, respectively. The crude mortality rate of stomach cancer was 21.48/100,000, age-standardized mortality rates by Chinese (ASMRC) and by world standard population (ASMRW) were 13.44/100,000 and 13.30/100,000, respectively. Incidence and mortality rates in rural areas were both higher than that in urban areas. Stomach cancer has a strong relationship with gender and age. The disease has occurred more frequently among men than women with a male to female ratio of 2.4 for ASIRC. After age group of 40−44 years, incidence rates are substantially higher in men than in women, same pattern was seen for age-specific mortality rates.
Conclusions
There is still a heavy burden of stomach cancer in China. The incidence and mortality patterns of stomach cancer show substantial gender and regional disparities. Great effort is needed to provide more accessible health services, sufficient financial resources, and adequate cancer-care infrastructure for the Chinese population, especially for people living in rural areas.
Keywords: Incidence, mortality, population-based, stomach cancer
Introduction
Stomach cancer is the fifth most common malignancy diagnosed worldwide, after cancers of the lung, breast, colorectum, and prostate. There were an estimated 952,000 new cases and 723,000 stomach cancer-related deaths in 2012 worldwide. Although its incidence has been declining in the last decades in most settings, stomach cancer remains common among many populations of East Asia, Central and Eastern Europe, and South America (1). Each year, the National Central Cancer Registry of China (NCCRC) estimates the number of new cancer cases and deaths in the country. In 2012, stomach cancer caused more than 320,000 deaths in China, accounting for about 45% of stomach cancer-related deaths worldwide, representing a heavy disease burden of stomach cancer in the country (2). In this article, we extracted data for stomach cancer from the database of the NCCRC and estimated the number of new cases and deaths for stomach cancer, nationally and for rural and urban areas, based on the most current population-based data of China in 2014.
Materials and methods
Data source
We used data collected and evaluated by the NCCRC from 339 local population-based cancer registries in 2017. All data submitted to the NCCRC are subject to quality control based on criteria of the Chinese Guideline for Cancer Registration (3) and Cancer Incidence in Five Continents Volume XI (4). We extracted and analyzed individual tumor records for patients who were diagnosed with primary, invasive cancer of the stomach [International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) codes C16.0–C16.6 and C16.8–C16.9]. The overall population coverage was 288,243,347 (146,203,891 males and 142,039,456 females), accounting for 21.07% of the national population (5).
Population data sources
We obtained overall population data for 2014 from the National Bureau of Statistics of China by area and sex. We obtained fifth and sixth National Population Census data of the entire population for 2000 and 2010, by age group (0, 1−4, 5−84 by 5 years, 85+ years), sex and area (urban/rural) (http://data.stats.gov.cn/). The method to further estimate age-specific population in a specific year (2014 in the present study) has been described in detail elsewhere (6). In brief, age-specific population was calculated using the estimated age structure, which was established using the estimated death probability in each age group.
Data quality control
IARCcrgTools (version 2.05) issued by the International Agency for Research on Cancer/International Association of Cancer Registries (IARC/IACR) were used for data checking and evaluation (7). The completeness, comparability and validity of the data were evaluated using a series of standards including the mortality to incidence (M/I) ratio, the percentage of case morphological verified (MV%), the percentage of death certificate-only cases (DCO%) and the percentage of the diagnosis of unknown basis (UB%) (8,9). The corresponding quality control indicators of the data for stomach cancer in our study were 0.71, 76.66%, 2.28%, and 0.48%, respectively (Table 1).
1.
Quality control indices of stomach cancer in China, 2014
| Areas | Sex | M/I | % | ||
| MV | DOC | UB | |||
| M/I, mortality to incidence ratio; MV, morphological verified; DCO, death certificate-only; UB, unknown basis. | |||||
| All | Both | 0.71 | 76.66 | 2.28 | 0.48 |
| Male | 0.71 | 77.41 | 2.24 | 0.46 | |
| Female | 0.72 | 74.90 | 2.39 | 0.53 | |
| Urban areas | Both | 0.70 | 75.64 | 3.08 | 0.78 |
| Male | 0.70 | 76.16 | 3.04 | 0.76 | |
| Female | 0.70 | 74.46 | 3.17 | 0.83 | |
| Rural areas | Both | 0.73 | 77.51 | 1.61 | 0.22 |
| Male | 0.72 | 78.44 | 1.57 | 0.21 | |
| Female | 0.75 | 75.29 | 1.70 | 0.26 | |
Statistical analysis
Crude incidence and mortality rates of stomach cancer were calculated in each stratum by age group, sex and area (urban/rural). The Chinese standard population in 2000 and Segi’s world population were applied to determine age-standardized incidence and mortality rates. All rates were expressed per 100,000 person-years. SAS software (Version 9.4; SAS Institute Inc., Cary, NC, USA) was used for the statistical analysis.
Results
Incidence of stomach cancer
In 2014, an estimated 410,400 new cases of stomach cancer occurred in China, accounting for 10.79% of all cancers combined. The age-standardized rates for stomach cancer (per 100,000 per year) using the Chinese standard population (age-standardized incidence rate China, ASIRC) and world standard population (age-standardized incidence rate world, ASIRW) were 19.62 and 19.51, respectively. The disease occurred more frequently among men than women, with a sex ratio of 2.4 according to ASIRC (Table 2). The ASIRC (per 100,000 per year) of stomach cancer in urban areas was 17.29; the burden was markedly higher in rural areas than in urban ones, with ASIRC (per 100,000 per year) of 22.82 in rural areas. In patients aged 0−74 years, the cumulative incidence rate was 2.42%; the truncated age-standardized incidence rate by world standard population for those aged 35−64 years was 28.80 per 100,000 per year (Table 2).
2.
Stomach cancer incidence in China, 2014
| Areas | Sex | Cases (×104) | Crude rate (1/105) | Ratio (%) | ASIRC (1/105) | ASIRW (1/105) | Cumulative rate 0–74 (%) | TASR 35–64 (1/105) | Rank |
| ASIRC, age-standardized incidence rate adjusted by Chinese standard population; ASIRW, age-standardized incidence rate adjusted by world standard population; TASR, truncated age-standardized rate by world standard population. | |||||||||
| All | Both | 41.04 | 30.00 | 10.79 | 19.62 | 19.51 | 2.42 | 28.80 | 2 |
| Male | 28.79 | 41.08 | 13.62 | 27.88 | 27.94 | 3.52 | 40.91 | 2 | |
| Female | 12.25 | 18.36 | 7.25 | 11.55 | 11.27 | 1.32 | 16.49 | 5 | |
| Urban | Both | 21.06 | 28.11 | 9.30 | 17.29 | 17.17 | 2.10 | 25.36 | 3 |
| Male | 14.67 | 38.66 | 11.94 | 24.50 | 24.56 | 3.06 | 35.82 | 2 | |
| Female | 6.39 | 17.27 | 6.17 | 10.37 | 10.07 | 1.16 | 14.86 | 5 | |
| Rural | Both | 19.98 | 32.29 | 12.97 | 22.82 | 22.73 | 2.85 | 33.59 | 2 |
| Male | 14.12 | 43.93 | 15.94 | 32.45 | 32.51 | 4.13 | 47.85 | 2 | |
| Female | 5.86 | 19.72 | 8.95 | 13.22 | 12.96 | 1.54 | 18.82 | 3 | |
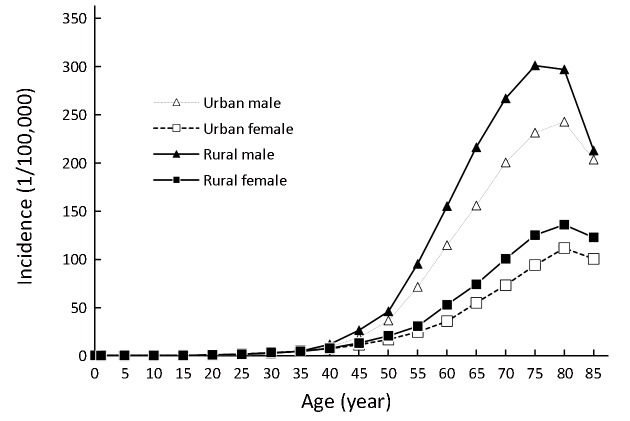
Age-specific incidence of stomach cancer
Stomach cancer has a strong relationship with age. Rates in younger age groups (0–24 years) were less than 1 per 100,000, increasing to 50 per 100,000 by age 55–59 years and peaking in the age group of 80–84 years (185.85 per 100,000). After the age group of 40–44 years, incidence rates were substantially higher in men than in women, especially for age groups of 55–59 and 60–64 years, with approximately two times greater risk for men compared with women. The same patterns of age-specific incidence of stomach cancer were seen in both urban and rural areas (Figure 1, Table 3).
1.
Age-specific incidence rates of stomach cancer in China, 2014.
3.
Age-specific incidence rates of stomach cancer in China, 2014 (1/105)
| Age groups | All areas | Urban areas | Rural areas | ||||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |||
| 0– | 0.51 | 0.65 | 0.35 | 0.79 | 1.04 | 0.50 | 0.13 | 0.12 | 0.14 | ||
| 1– | 0.01 | 0.02 | 0.00 | 0.02 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| 5– | 0.04 | 0.04 | 0.04 | 0.00 | 0.00 | 0.00 | 0.07 | 0.07 | 0.08 | ||
| 10– | 0.03 | 0.03 | 0.04 | 0.07 | 0.07 | 0.07 | 0.00 | 0.00 | 0.00 | ||
| 15– | 0.13 | 0.16 | 0.11 | 0.11 | 0.08 | 0.14 | 0.16 | 0.24 | 0.07 | ||
| 20– | 0.44 | 0.34 | 0.56 | 0.37 | 0.30 | 0.45 | 0.52 | 0.38 | 0.68 | ||
| 25– | 1.22 | 1.05 | 1.40 | 1.16 | 0.81 | 1.51 | 1.29 | 1.32 | 1.27 | ||
| 30– | 2.60 | 2.13 | 3.10 | 2.48 | 1.94 | 3.03 | 2.77 | 2.37 | 3.21 | ||
| 35– | 4.29 | 4.07 | 4.53 | 4.15 | 3.61 | 4.68 | 4.48 | 4.63 | 4.32 | ||
| 40– | 8.78 | 10.11 | 7.40 | 8.07 | 8.87 | 7.27 | 9.67 | 11.63 | 7.58 | ||
| 45– | 17.02 | 22.04 | 11.88 | 14.83 | 18.58 | 11.05 | 19.67 | 26.17 | 12.89 | ||
| 50– | 29.31 | 40.25 | 18.16 | 26.50 | 36.30 | 16.51 | 33.27 | 45.82 | 20.49 | ||
| 55– | 54.36 | 80.90 | 26.79 | 48.07 | 71.21 | 24.36 | 63.66 | 94.99 | 30.44 | ||
| 60– | 87.09 | 131.49 | 42.62 | 74.78 | 114.47 | 35.64 | 104.38 | 154.94 | 52.60 | ||
| 65– | 122.39 | 181.49 | 62.69 | 104.98 | 155.55 | 54.60 | 145.87 | 215.90 | 73.78 | ||
| 70– | 156.03 | 228.97 | 84.34 | 135.20 | 200.23 | 72.86 | 184.12 | 266.64 | 100.28 | ||
| 75– | 179.95 | 260.13 | 106.40 | 158.92 | 231.15 | 93.82 | 210.13 | 300.85 | 124.83 | ||
| 80– | 185.85 | 264.41 | 121.44 | 170.92 | 242.49 | 111.44 | 207.46 | 296.71 | 135.71 | ||
| 85+ | 147.92 | 206.96 | 109.51 | 141.60 | 203.21 | 100.19 | 156.99 | 212.61 | 122.48 | ||
| All | 30.00 | 41.08 | 18.36 | 28.11 | 38.66 | 17.27 | 32.29 | 43.93 | 19.72 | ||
Mortality rate of stomach cancer
In 2014, an estimated 293,800 stomach cancer-associated deaths occurred in China, accounting for 12.80% of all cancer-related deaths combined. The mortality rates of stomach cancer (per 100,000 per year) adjusted by the Chinese standard population (age-standardized mortality rate China, ASMRC) and world standard population (age-standardized mortality rate world, ASMRW) were 13.44 and 13.30, respectively. Stomach cancer was the third most common cause of cancer mortality among males with ASMRC and ASMRW of 19.33 and 19.21 per 100,000, respectively; stomach cancer ranked second among females, with ASMRC and ASMRW of 7.80 and 7.63 per 100,000, respectively. The mortality rate of stomach cancer in rural areas showed a significantly higher rate than that in urban areas, with ASMRC (both sexes combined) 16.12 and 11.51 per 100,000, respectively. In patients aged 0–74 years, the cumulative mortality rate was 1.55% and the truncated age-standardized mortality rate using the world standard population for those aged 35–64 years was 15.77 per 100,000 per year (Table 4).
4.
Stomach cancer mortality in China, 2014
| Areas | Sex | Deaths
(×104) |
Crude rate (1/105) | Ratio
(%) |
ASMRC
(1/105) |
ASMRW
(1/105) |
Cumulative rate
0–74 (%) |
TASR 35–64
(1/105) |
Rank |
| ASMRC, age-standardized mortality rate adjusted by Chinese standard population; ASMRW, age-standardized mortality rate adjusted by world standard population; TASR, truncated age-standardized rate by world standard population. | |||||||||
| All | Both | 29.38 | 21.48 | 12.80 | 13.44 | 13.30 | 1.55 | 15.77 | 3 |
| Male | 20.49 | 29.24 | 14.11 | 19.33 | 19.21 | 2.27 | 22.49 | 3 | |
| Female | 8.89 | 13.33 | 10.54 | 7.80 | 7.63 | 0.84 | 8.93 | 2 | |
| Urban | Both | 14.74 | 19.68 | 11.29 | 11.51 | 11.38 | 1.30 | 13.52 | 3 |
| Male | 10.28 | 27.09 | 12.58 | 16.64 | 16.56 | 1.93 | 19.22 | 3 | |
| Female | 4.47 | 12.08 | 9.14 | 6.66 | 6.50 | 0.69 | 7.80 | 3 | |
| Rural | Both | 14.64 | 23.66 | 14.78 | 16.12 | 15.94 | 1.90 | 18.90 | 3 |
| Male | 10.21 | 31.78 | 16.08 | 22.98 | 22.82 | 2.73 | 26.99 | 3 | |
| Female | 4.43 | 14.89 | 12.46 | 9.40 | 9.21 | 1.04 | 10.52 | 2 | |
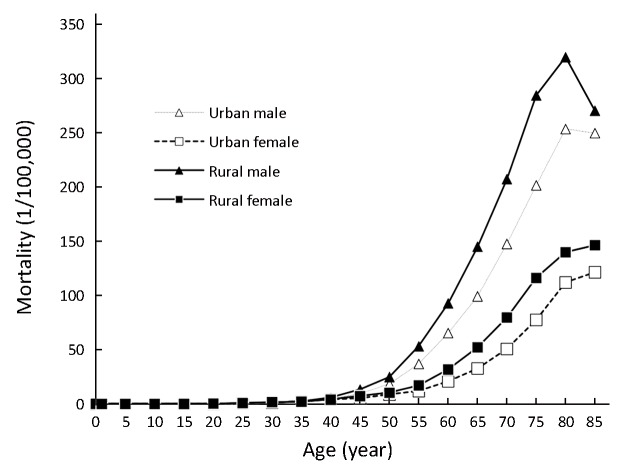
Age-specific mortality rate of stomach cancer
Because of a high fatality rate, the patterns of age-specific mortality rates of stomach cancer were close to those of age-specific incidence rates. After 45 years old, rates among males were significantly higher than those among females, showing a two- to three-times variation between specific age groups. A very small difference was seen by sex when taking the peak age-specific mortality rates into consideration. For males, the age-specific rates reached a peak at age group of 80−84 years (280.45 per 100,000), whereas for females, the peak age group was over 85 years (131.99 per 100,000). In terms of regional variations, age-specific mortality rates of stomach cancer in rural areas were higher than those in urban areas after the age of 15 years (Figure 2, Table 5).
2.
Age-specific mortality rates of stomach cancer in China, 2014.
5.
Age-specific mortality rates of stomach cancer in China, 2014 (1/105)
| Age groups | All areas | Urban areas | Rural areas | ||||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |||
| 0– | 0.03 | 0.00 | 0.06 | 0.00 | 0.00 | 0.00 | 0.06 | 0.00 | 0.14 | ||
| 1– | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| 5– | 0.01 | 0.03 | 0.00 | 0.02 | 0.03 | 0.00 | 0.01 | 0.02 | 0.00 | ||
| 10– | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| 15– | 0.04 | 0.05 | 0.04 | 0.04 | 0.05 | 0.03 | 0.05 | 0.04 | 0.05 | ||
| 20– | 0.25 | 0.23 | 0.26 | 0.24 | 0.27 | 0.20 | 0.26 | 0.19 | 0.33 | ||
| 25– | 0.60 | 0.52 | 0.68 | 0.52 | 0.41 | 0.63 | 0.69 | 0.64 | 0.74 | ||
| 30– | 1.33 | 1.23 | 1.42 | 1.18 | 1.15 | 1.21 | 1.52 | 1.34 | 1.72 | ||
| 35– | 2.08 | 2.08 | 2.09 | 2.05 | 1.97 | 2.13 | 2.13 | 2.21 | 2.04 | ||
| 40– | 4.56 | 5.11 | 3.98 | 4.20 | 4.38 | 4.02 | 5.00 | 6.00 | 3.93 | ||
| 45– | 8.68 | 11.19 | 6.12 | 7.36 | 9.43 | 5.27 | 10.28 | 13.28 | 7.15 | ||
| 50– | 15.22 | 21.04 | 9.31 | 13.51 | 18.35 | 8.58 | 17.64 | 24.83 | 10.33 | ||
| 55– | 29.00 | 43.53 | 13.89 | 24.50 | 36.93 | 11.77 | 35.63 | 53.12 | 17.09 | ||
| 60– | 51.17 | 76.93 | 25.37 | 42.98 | 65.41 | 20.85 | 62.67 | 92.78 | 31.83 | ||
| 65– | 80.16 | 118.97 | 40.96 | 65.96 | 99.30 | 32.75 | 99.31 | 145.07 | 52.21 | ||
| 70– | 117.72 | 173.52 | 62.88 | 98.17 | 147.66 | 50.72 | 144.10 | 207.41 | 79.77 | ||
| 75– | 161.64 | 236.18 | 93.28 | 136.43 | 201.69 | 77.60 | 197.84 | 284.62 | 116.25 | ||
| 80– | 194.24 | 280.45 | 123.56 | 176.33 | 253.65 | 112.06 | 220.16 | 319.94 | 139.95 | ||
| 85+ | 181.71 | 258.15 | 131.99 | 173.13 | 249.90 | 121.55 | 194.03 | 270.58 | 146.52 | ||
| All | 21.48 | 29.24 | 13.33 | 19.68 | 27.09 | 12.08 | 23.66 | 31.78 | 14.89 | ||
Discussion
There were an estimated 952,000 new cases of stomach cancer (7% of total cancer incidence) and 723,000 stomach cancer-related deaths (9% of total cancer mortality) in 2012 worldwide. Cancer of the stomach is the fifth most common type of cancer and the third leading cause of cancer deaths for both sexes globally. Large differences in incidence exist among continents. High incidence rates of this disease are found in East Asia and Central and Eastern Europe, and low incidence rates have been described in Africa and North America (2). Owing to a large population and a high incidence rate, more than 40% of stomach cancer cases worldwide (404,996 cases) have occurred in China, according to GLOBOCAN 2012 (2). In our study, an estimated 410,400 new cases of stomach cancer occurred in China in 2014, accounting for 10.79% and ranking third in incidence of all cancers combined, which indicates that stomach cancer remains a major contributor to the cancer burden among the Chinese population.
Stomach cancer incidence rates have been declining in most parts of the world in recent decades. The national stomach cancer standard incidence rates of China were 21.98 and 21.32 per 100,000 in 2012 and 2013, respectively, as reported in our previous study (10,11); this rate was 19.51 per 100,000 in 2014. In South Korea, the disease rate decreased by 0.5% per year from 1999 to 2012. In Beijing, the capital of China, this rate decreased by 24.2% and 49.0% for males and females, respectively, between 1982–1984 and 1995–1997 (12,13). Cancer incidence patterns reflect trends in behaviors associated with cancer risk. Reduction in the prevalence of Helicobacter pylori, improvements in sanitation and in the preservation and storage of foods and increasing consumption of fresh fruit and vegetables may have some role in the observed decline in incidence of stomach cancer worldwide (14,15). However, the risks of stomach cancer generally remain more common in males. Our study shows that the incidence of stomach cancer is 2.4 times higher in men than in women, which is in line with a previous study in China (16). Although the incidence of stomach cancer has decreased year by year with increasing socioeconomic development, inequalities of incidence remain within China (5,17). Stomach cancer incidence rates in rural parts of the country were 1.3 times higher than those in urban areas (22.82 vs. 17.29 per 100,000) in this study. Different primary prevention strategies should be launched based on these substantial regional disparities. The mortality rate of stomach cancer was also higher in rural than in urban areas (16.12 vs. 11.51 per 100,000 per year), which is in line with findings reported in our previous studies. Differences in socioeconomic status and in access to health services are possible explanations for the variations in mortality rate found in this study, which highlights the need to increase access to health services and resources for populations in rural parts of China.
The prognosis of patients diagnosed with stomach cancer remains poor in China, with a 5-year relative survival rate of 35.9% in 2010–2014. In contrast, survival was remarkably high in South Korea (68.9%) and Japan (60.3%) during the same period (18). Survival in those two countries was similar to the average 1-year survival rate for all other countries and about twice the 5-year survival rate in China. Very high survival for patients with stomach cancer in those countries may be partially explained by diagnosis of tumors at earlier stages. Screening for gastric cancer using barium-meal imaging began in Miyagi Prefecture, Japan in 1960 and a nationwide screening program has now been established. The same nationwide screening strategy for stomach cancer was also initiated in South Korea (19). Although screening may detect asymptomatic tumors, most cancers in Japan are detected outside the screening program, indicating that awareness of the benefits of early detection is very high in the Japanese population (20). Currently, China operates a screening program targeting individuals with high risk of stomach cancer (21,22). However, 80% of patients are still diagnosed at an advanced stage and have a lower 5-year relative survival rate than patients in Japan and Korea (18,23). Two principal reasons may contribute to the continued low detection rate of stomach cancer at early stages in China, even after the launch of the government-sponsored screening program. One reason is that awareness of the benefit of endoscopic screening among the population is low and many people are unwilling to take part in screening because they fear physical discomfort from the invasive endoscope procedure (23). Apart from the obstacle of awareness, there is inherent reluctance owing to cultural barriers and fatalism about cancer in the Chinese population, which can also hamper screening efforts, particularly among groups with low socioeconomic status (24). The second reason for low detection in China is that outside of the government-sponsored screening program, the social insurance schemes do not cover the fee for endoscopy as part of a general screening modality in high-risk populations (23). These two reasons result in a lower coverage or participation rate for stomach cancer screening among target populations in China. Substantial regional disparities in stomach cancer treatment play another important role in the variation of prognosis between urban and rural areas in China. Patients in rural areas are more likely to receive suboptimal or non-guideline therapy, which may contribute to lower survival rates (25).
Conclusions
With the increasing ageing population in China, stomach cancer will remain a consistently serious public health issue in the future. Although incidence and mortality rates are declining in the country, both rates remain higher than global average levels, and the disease burden currently shows clear urban-rural inequalities in China. With a large, widely dispersed population and marked variations of socioeconomic status, the disparities in access to cancer screening and receiving treatment for stomach cancer according to the guidelines will remain for some time. Great effort is needed not only to improve public awareness and promote early detection of stomach cancer but also to provide more accessible health services, sufficient financial resources, and adequate cancer-care infrastructure for the Chinese population, especially for people living in rural areas.
Acknowledgements
We gratefully acknowledge the cooperation of the population-based cancer registries for providing cancer statistics, data collection, sorting, verification, and database creation. This work was supported by grants from the Beijing Young Talent Program (No. 2016000021469G189), Special Fund for Health Research in the Public Interest (No. 201502001) and CAMS Innovation Fund for Medical Sciences (CIFMS) (No. 2016-12M-2-004).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.International Agency for Research on Cancer. Cancer Today. Available online: http://gco.iarc.fr/today/
- 3.National Cancer Center. Guideline for Chinese Cancer Registration. Beijing: People’s Medical Publishing House, 2016.
- 4.Bray F, Colombet M, Mery L, et al. Cancer Incidence in Five Continents, Vol. XI (electronic version). Lyon: International Agency for Research on Cancer, 2017.
- 5.Chen W, Sun K, Zheng R, et al. Report of cancer incidence and mortality in different areas of China, 2014. Zhongguo Zhong Liu. 2018;27:1–14. doi: 10.11735/j.issn.1004-0242.2018.01.A001. [DOI] [PubMed] [Google Scholar]
- 6.Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res. 2016;28:1–11. doi: 10.3978/j.issn.1000-9604.2016.02.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferlay J. The IARCcrgTools Programs. Lyon: IARC, 2006. Available online: http://www.iacr.com.fr/index.php?option=com_content&view=article&id=72:iarccrgtools&catid=68&Itemid=445
- 8.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45:747–55. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 9.Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45:756–64. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Zuo T, Zheng R, Zeng H, et al. Epidemiology of stomach cancer in China. Zhongguo Zhong Liu Lin Chuang. 2017;44:52–8. doi: 10.3969/j.issn.1000-8179.2017.01.881. [DOI] [Google Scholar]
- 11.Zhang S, Yang Z, Zheng R, et al. Incidence and mortality of stomach cancer in China, 2013. Zhonghua Zhong Liu Za Zhi. 2017;39:547–52. doi: 10.3760/cma.j.issn.0253-3766.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Jung KW, Won YJ, Oh CM, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017;49:292–305. doi: 10.4143/crt.2017.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Q, Zhu W, Xing X, et al. The trend of cancer incidence in urban Beijing from 1982 to 1997. Zhonguo Zhong Liu. 2001;10:507–9. [Google Scholar]
- 14.Watanabe M, Ito H, Hosono S, et al. Declining trends in prevalence of Helicobacter pylori infection by birth-year in a Japanese population. Cancer Sci. 2015;106:1738–43. doi: 10.1111/cas.12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanaka M, Ma E, Tanaka H, et al. Trends of stomach cancer mortality in Eastern Asia in 1950-2004: comparative study of Japan, Hong Kong and Singapore using age, period and cohort analysis. Int J Cancer. 2012;130:930–6. doi: 10.1002/ijc.26080. [DOI] [PubMed] [Google Scholar]
- 16.Yang L. Incidence and mortality of gastric cancer in China. World J Gastroenterol. 2006;12:17–20. doi: 10.3748/wjg.v12.i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Z, Zheng R, Zhang S, et al. Comparison of cancer incidence and mortality in three GDP per capita levels in China, 2013. Chin J Cancer Res. 2017;29:385–94. doi: 10.21147/j.issn.1000-9604.2017.05.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung WK, Wu MS, Kakugawa Y, et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol. 2008;9:279–87. doi: 10.1016/S1470-2045(08)70072-X. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki H, Gotoda T, Sasako M, et al. Detection of early gastric cancer: misunderstanding the role of mass screening. Gastric Cancer. 2006;9:315–9. doi: 10.1007/s10120-006-0399-y. [DOI] [PubMed] [Google Scholar]
- 21.Dai M, Shi J, Li N. The design and aim of cancer screening programme in urban China. Zhonghua Yu Fang Yi Xue Za Zhi. 2013;47:179–82. doi: 10.3760/cma.j.issn.0253-9624.2013.02.018. [DOI] [Google Scholar]
- 22.You W. Progress in early detection and treatment for gastric cancer. Zhongguo Zhong Liu. 2009;18:695–9. [Google Scholar]
- 23.Zong L, Abe M, Seto Y, et al. The challenge of screening for early gastric cancer in China. Lancet. 2016;388:2606. doi: 10.1016/S0140-6736(16)32226-7. [DOI] [PubMed] [Google Scholar]
- 24.Fan L, Strasser-Weippl K, Li JJ, et al. Breast cancer in China. Lancet Oncol. 2014;15:e279–89. doi: 10.1016/S1470-2045(13)70567-9. [DOI] [PubMed] [Google Scholar]
- 25.Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003-2005: a population-based study. Int J Cancer. 2015;136:1921–30. doi: 10.1002/ijc.29227. [DOI] [PubMed] [Google Scholar]