Highlights
-
•
We report a rare case of pelvic pain in adult.
-
•
The pelvic pain was caused by Herlyn-Werner-Wunderlich Syndrome.
-
•
The main diagnostic tool was MRI.
-
•
The problem was overcame with excision of the septum.
-
•
We report a complete investigation and management of Herlyn-Werner-Wunderlich Syndrome.
Keywords: Mullerian dysgenesis, Dysmenorrhea, Urogynecology, Case report, Pelvic pain
Abstract
Introduction
Herlyn-Werner-Wunderlich Syndrome (HWWs) is a rare congenital anomaly. This abnormality has 5% percentage of the total Mullerian dysgenesis. The symptomatic patients come with varies condition, such as urinary incontinence, urinary retention endometriosis, pelvic infection and acute pelvic pain. Here we present investigation and management of HWWs with pelvic pain in adult woman.
Presentation of case
A 23 years old woman came with pelvic pain. We found abnormalities of HWW syndrome i.e. uterus didelphys with obstructed hemivagina and right renal agenesis through ultrasound imaging, CT scan and MRI. After concluding the diagnosis, the patient underwent vaginal septum excision and vaginoplasty procedures to relieve obstruction which was the cause of pelvic pain. The symptom was improved after surgery and she felt no more pain after a year of follow up.
Discussion
The main symptom of HWWs is dysmenorrhea associated with obstruction mass or endometriosis. MRI with capability of tissue differentiation is the gold standard for diagnostic. The primary purpose of surgery is to release the obstruction and to prevent further complication.
Conclusion
Rarely, HWWs causes an acute pelvic pain with secondary cystic mass finding. Surgery aimed to release obstruction will improve this symptom.
1. Introduction
HWW syndrome is classified as Class III Mullerian dysgenesis, which involves uterus didelphys, obstructed hemivagina and unilateral kidney agenesis This abnormality has 5% percentage of the total Mullerian dysgenesis [1,2]. The prevalence of Mullerian dysgenesis is unclear, because many of them are asymptomatic. Based on some researches the prevalence varies from 0.4%–6.7 % [1]. Several cases have been reported to be associated with urinary incontinence, urinary retention, endometriosis, pelvic infection and acute pelvic pain [[3], [4], [5]]. In this case, we presented the investigation and management of HWWs which was the cause of a rare pelvic pain in adult woman. We reported and checked this case based on SCARE guidelines [6].
2. Presentation of case
A 23-years-old woman came to the clinic with complaint of menstrual pain. The patient is unmarried and has never had sexual intercourse before, she has normal activity and works at a state company every day. She has no history of smoking or other metabolic diseases. She reported a normal menstruation since it started at 12 years old. There had been no menstrual pain until she felt it in the last one year with VAS 3–4 each time of menstruation. However, the pain was getting worse lately, so she went to hospital for consultation. There were no family members who had similar complaint.
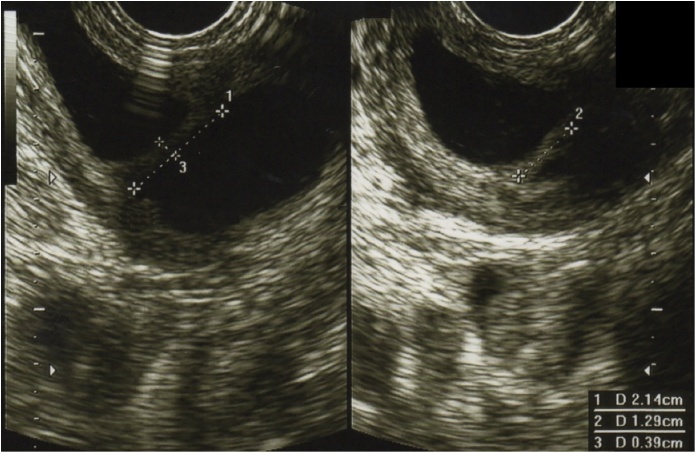
Physical examination found no significant abnormalities. Secondary sex growth was normal for her age. External gynaecology examination was also within normal limits. Further internal genital examination through the rectum found a cystic mass with a smooth surface in the right lateral region of the midline with proximal border and its origin was difficult to be determined. The uterus was slightly enlarged and there was no solid mass palpable around the cervix. Moreover, ultrasound examination was performed, exhibiting two anteflexed uteri with homogenous myometrium that were fused at the precede to the cervix. Further evaluation showed dilatation of vagina consisting of smooth, mobile hypoechoic mass; the vaginal septum lied from anterior to posterior at the middle of the vagina (Fig. 1). Both ovaries were normal; each was connected to a fallopian tube. It was difficult to define the cervix-whether single or double- while amount of blood was present in the vagina, corresponding to haematocolpos. We found left kidney in normal size, however there was no right kidney. From these findings, we concluded that the presence of uterus didelphys with obstructed right hemivagina was consistent with our suspicion of HWWs. Through ultrasound, we had not been able to assess other kidney-related abnormalities as well as the cervix and its association with the obstruction in the distal area of vagina.
Fig. 1.
Vaginal septum size 2.14 × 1.29 × 0.39 cm obstructing distal part of vagina.
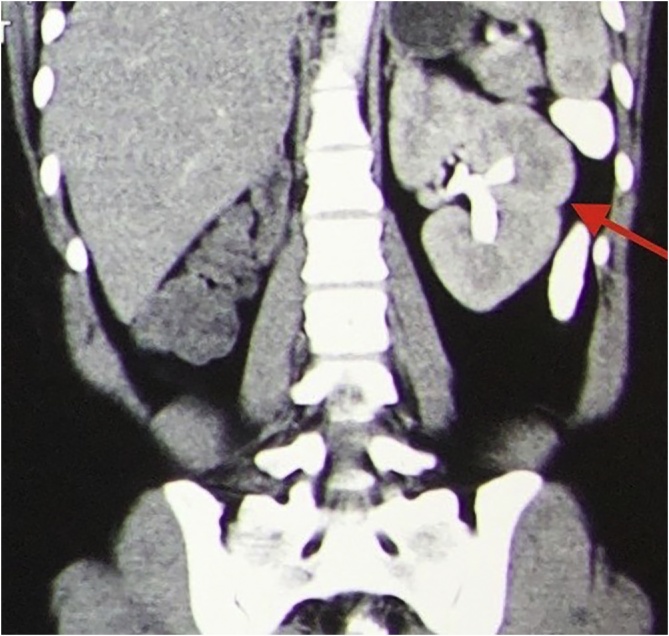
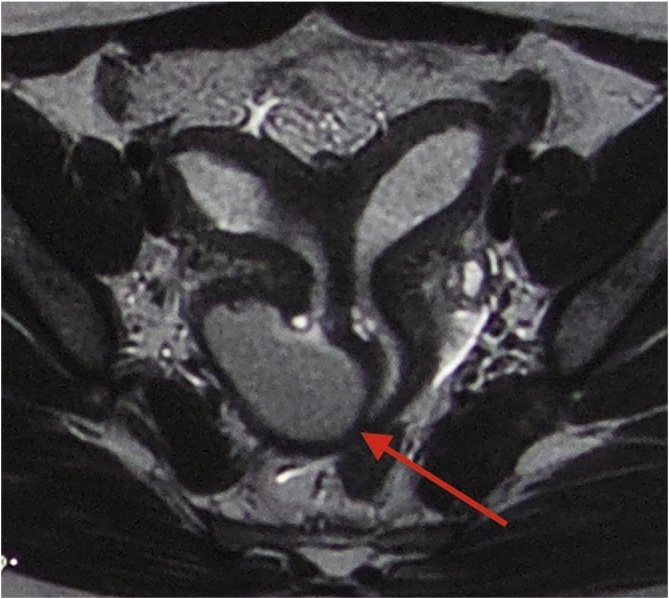
Next, as the gold standard of tissue examination, we planned Magnetic Resonance Imaging (MRI) examination for the abdominal and pelvic areas. However, due to MRI limitation in our hospital and insurance issues, we only did one MRI examination for the pelvic by sending it to another affiliated hospital. As for assessing the abdomen, we did a Computerized Tomography (CT) scan examination in our facility. The results of CT scan showed the right renal agenesis. The left kidney had normal structure and normal ureter (Fig. 2). We performed MRI scan, which has demonstrated its importance in the diagnosis of HWW syndrome. Two complete sets of uteruses were found, each with its own corpus and cervix. The results also showed a cystic mass connected with the uterine cavity and cervical canal, obstructing the distal part of the vagina (Fig. 3). Finally, this finding highlights the accuracy of MRI scan in diagnosing HWWs
Fig. 2.
Coronal section of CT scan revealed normal structure of left kidney and agenesis of right kidney.
Fig. 3.
MRI result revealed two normal uterine corpuses with normal endometrium and normal cervix. The distal part of vagina seen obstructed with right cystic mass (haematocolpos) appearance.
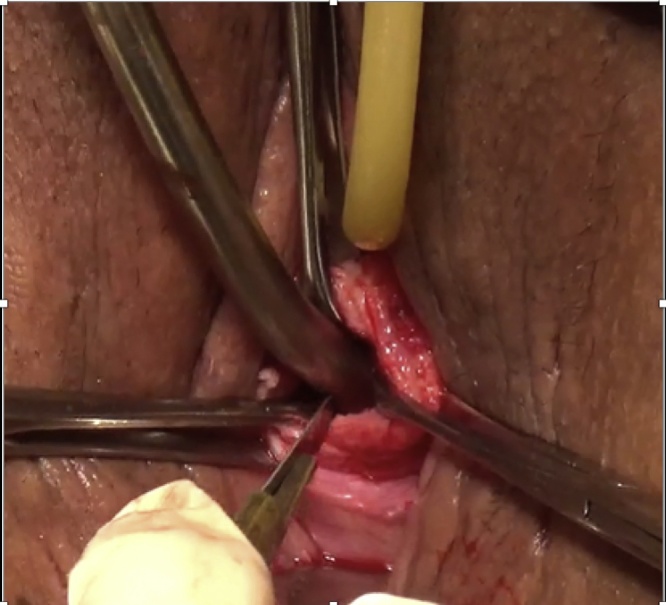
We prepared the vaginal septum excision to release the obstruction causing the pelvic pain, with informed consent about hymen damage during the procedure. The perioperative examination was unremarkable and spinal anaesthesia was used during the surgery. We performed gynaecology examination after urinary catheter insertion and found a bulging cystic mass with smooth surface from the right lateral vagina with unclear upper border (Fig. 4). A needle puncture was performed through the mass and shown blood (haematocolpos due to distal obstruction of the vaginal septum). Furthermore, 1 cm incision in the puncture area was made and widened to 3 cm. We evacuated 500 cc of blood clot. Vaginal septum with 5 mm thickness was found and excised with a diameter of 3 cm followed by vaginal reconstruction (Fig.5). There was no complication during surgery. After 3 days, the patient was in good condition and had been discharged. In the next follow-up, the patient did not complain any menstrual pain, but there was an increasing amount of menstrual blood. In one year follow up, she had no complain of pelvic pain. The mount of menstrual blood was much more than before as consequences of two functional uteruses.
Fig. 4.
Cystic mass with smooth surface originated from right anterior vagina.
Fig. 5.
The septum was incised, and 500 cc of blood clot was evacuated. Procedure was continued with excision of a 3 cm diameter of the septum and ended with vaginal reconstruction.
3. Discussion
The Mullerian ducts migrate to the midline then fuse to form the uterus and cervix and upper vagina at 8 weeks of pregnancy. Incomplete or non-existent merging will result in two uteruses. Renal agenesis usually follows the Mullerian ducts dysgenesis because kidneys, fallopian tubes, cervix and proximal vagina are derived from the same ureteritic buds [7]. The reported variations are 72.4% with classical variants of uterus didelphys and 27.6% rare variants with uterus septum or cervical agenesis [8]. According to Tong et al, 60% of the abnormalities have occurred on the right side [9]. This syndrome is rarely found at the age of less than 5 years [10]. HWWs diagnosis are often delayed after puberty because emerging symptoms of obstruction are also associated with a connection between two uterus and incomplete reabsorption of the vaginal septum.
The main symptom of HWWs is dysmenorrhea and usually established after puberty. This pain will rise due to the increase the volume of haematometrocolpos caused by obstructed vagina. Other causes of pelvic pain, such as endometriosis, inflammation, twisted cysts and appendicitis should be excluded [4,11]. Although it has been accepted that no single theory explaining about endometriosis, Sampson's theory of retrograde menstruation and implantation is supporting most of endometriosis cases due to obstruction of the vagina. Early diagnosis of endometriosis in patients with HWW syndrome can reduce organ damage and fertility function and prevent its recurrence [5]. Another uncommon presentation is urinary retention. The woman’s urethra is short and straight with a large enough diameter; as a result, urinary retention is rare. Urinary retention occurs because the mass of haematocolpos is quite large. At that size, it causes urethra angulation which leads to an obstruction. Another hypothesis has stated that haematocolpos reduces the extrusion capacity of the urethral sphincter by irritating the sacral plexus [12].
Preliminary and accurate diagnosis is important in preventing complications of HWW syndrome. Hysterosalphingography (HSG), ultrasound and MRI are combined to find accurate diagnosis [13]. Mostly in ultrasound examinations uterus didelphys with echoic mass at the vagina or cervix are detected. Hematocolpos image can be found in cystic form, mimicking endometriosis or complex ovarian cysts. Uterus didelphys finding with cystic mass or fluid inside the vagina must be investigated. Ultrasound was reported to have 90–92% accuracy in diagnosing HWW syndrome [13,14]. MRI is the gold standard in diagnosing Mullerian abnormalities. The accuracy of MRI is mentioned up to 100% with the benefit of free radiation, non-invasive, able to assess soft tissue such as mass of endometriosis, pelvic infection and adhesion [14]. It has good accuracy to distinguish the intra and extra uterine anatomy and secondary complex anomalies such as uterine fibroid, endometriosis and hydrosalpinx which offers a better data for appropriate management [12]. In order to reduce the cost, CT scan or HSG can be chosen for diagnostic. Laparoscopy as a gold standard in evaluating internal genitalia has not been used routinely. It is only carried out in certain cases such as MRI limitations or the result of MRI is not very clear. Otherwise, laparoscopy may also be used as to perform drainage such as septectomy or marsupialization [15].
Management of HWW syndrome is resection procedure of the vaginal septum to release obstruction. Smith and Laufer reported of 27 cases, there were six cases underwent two-stages vaginoplasty due to anatomical distortion, infection and stenosis [16]. The septal resection with hysteroscopy with transabdominal ultrasound guiding can be used to maintain hymen integrity. Rarely, Unilateral hysterectomy may be considered in case of recurrent stenosis [4]. Important issues while performing vaginal septum excision, some near organ such as urethra, bladder and rectum are potentially injured [17].
4. Conclusion
Rarely, HWWs causes a severe acute pain with a secondary cystic mass finding. Combined with unilateral kidney agenesis, this finding must be confirmed with MRI to establishes the diagnosis of HWWs. The purpose of the surgery is to overcome the obstruction of the internal genital tract.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Funding source
Authors declare there are no funding resources for this paper.
Ethical approval
Institutional review board approval was exempt because all data were collected from clinical records and imaging systems for routine preoperative planning and follow up.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Author contribution
Lucky Savitry: Performing the surgery and supervision.
Yuyun Lisnawati: Performing Ultrasound.
Sri Pudyastuti: Writing concept and paper revision.
Agrifa Haloho: Writing original paper and software.
Registration of research studies
Name of Registry : Researchregistry.
UIN: researchregistry4012.
Guarantor
Lucky Savitry.
Agrifa Haloho.
Contributor Information
Yuyun Lisnawati, Email: yulisna.er@gmail.com.
Agrifa Hasiholan Haloho, Email: agrifa.hasiholan@gmail.com.
References
- 1.Epelman M., Dinan D., Gee M.S., Servaes S., Lee E.Y., Darge K. Müllerian duct and related anomalies in children and adolescents. Magn. Reson. Imaging Clin. N. Am. 2013 doi: 10.1016/j.mric.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 2.Khaladkar S.M., Kamal V., Kamal A., Kondapavuluri S.K. The Herlyn-Werner-Wunderlich Syndrome—a case report with radiological review. Pol. J. Radiol. 2016 doi: 10.12659/PJR.897228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dogan A., Uyar I., Demirtas G.S., Ekin A., Gulhan I., Ertas I.E., Ozeren M. Urinary incontinence in puberty: a rare clinical presentation of the Herlyn-Werner-Wunderlich Syndrome. J. Pediatr. Adolesc. Gynecol. 2016 doi: 10.1016/j.jpag.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Gungor Ugurlucan F., Bastu E., Gulsen G., Kurek Eken M., Akhan S.E. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clin. Imaging. 2014 doi: 10.1016/j.clinimag.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Tong J., Zhu L., Chen N., Lang J. Endometriosis in association with Herlyn-Werner-Wunderlich Syndrome. Fertil. Steril. 2014 doi: 10.1016/j.fertnstert.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016 doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Healey A. Embryology of the female reproductive tract. Imaging Gynecol. Disord. Infants Child. 2012 [Google Scholar]
- 8.Fedele L., Motta F., Frontino G., Restelli E., Bianchi S. Double uterus with obstructed hemivagina and ipsilateral renal agenesis: pelvic anatomic variants in 87 cases. Hum. Reprod. 2013 doi: 10.1093/humrep/det081. [DOI] [PubMed] [Google Scholar]
- 9.Tong J., Zhu L., Lang J. Clinical characteristics of 70 patients with Herlyn-Werner-Wunderlich Syndrome. Int. J. Gynecol. Obstet. 2013 doi: 10.1016/j.ijgo.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Angotti R., Molinaro F., Bulotta A.L., Bindi E., Cerchia E., Sica M. Herlyn-Werner-Wunderlich Syndrome: an “early” onset case report and review of literature. Int. J. Surg. Case Rep. 2015 doi: 10.1016/j.ijscr.2015.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu L., Chen N., Tong J.L., Wang W., Zhang L., Lang J.H. New classification of Herlyn-Werner-Wunderlich Syndrome. Chin. Med. J. (Engl.) 2015 doi: 10.4103/0366-6999.149208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar S., Rajagopal K.V., Karegowda L.H., Chaitanya R.K. Herlyn-Werner-Wunderlich Syndrome: a rare cause of acute urinary retention in an adolescent girl. Case Rep. 2015 doi: 10.1136/bcr-2015-209638. bcr2015209638-bcr2015209638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Troiano R.N., McCarthy S.M. Mullerian duct anomalies: imaging and clinical issues. Radiology. 2004 doi: 10.1148/radiol.2331020777. [DOI] [PubMed] [Google Scholar]
- 14.Yavuz A., Bora A., Kurdoğlu M., Goya C., Kurdoğlu Z., Beyazal M., Akdemir Z. Herlyn-Werner-Wunderlich syndrome: merits of sonographic and magnetic resonance imaging for accurate diagnosis and patient management in 13 cases. J. Pediatr. Adolesc. Gynecol. 2015 doi: 10.1016/j.jpag.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Sharma R., Dey A.K., Mittal K., Kumar P. Use of imaging in diagnosis of Herlyn-Werner-Wunderlich syndrome, a case report. J. Obstet. Gynaecol. 2016;3615 doi: 10.1080/01443615.2016.1188268. [DOI] [PubMed] [Google Scholar]
- 16.Smith N.A., Laufer M.R. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil. Steril. 2007;87 doi: 10.1016/j.fertnstert.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 17.Karaca L., Pirimoglu B., Bayraktutan U., Ogul H., Oral A., Kantarci M. Herlyn-Werner-Wunderlich Syndrome: a very rare urogenital anomaly in a teenage girl. J. Emerg. Med. 2015 doi: 10.1016/j.jemermed.2014.09.064. [DOI] [PubMed] [Google Scholar]