Abstract
Introduction
Understanding the geographic patterns of suicide can help inform targeted prevention efforts. Although state-level variation in age-adjusted suicide rates has been well documented, trends at the county-level have been largely unexplored. This study uses small area estimation to produce stable county-level estimates of suicide rates to examine geographic, temporal, and urban–rural patterns in suicide from 2005 to 2015.
Methods
Using National Vital Statistics Underlying Cause of Death Files (2005–2015), hierarchical Bayesian models were used to estimate suicide rates for 3,140 counties. Model-based suicide rate estimates were mapped to explore geographic and temporal patterns and examine urban–rural differences. Analyses were conducted in 2016–2017.
Results
Posterior predicted mean county-level suicide rates increased by >10% from 2005 to 2015 for 99% of counties in the U.S., with 87% of counties showing increases of >20%. Counties with the highest model-based suicide rates were consistently located across the western and northwestern U.S., with the exception of southern California and parts of Washington. Compared with more urban counties, more rural counties had the highest estimated suicide rates from 2005 to 2015, and also the largest increases over time.
Conclusions
Mapping county-level suicide rates provides greater granularity in describing geographic patterns of suicide and contributes to a better understanding of changes in suicide rates over time. Findings may inform more targeted prevention efforts as well as future research on community-level risk and protective factors related to suicide mortality.
INTRODUCTION
Suicide is a complex public health problem, influenced by multiple individual, community, and societal risk and protective factors.1 Since 2008, suicide has ranked as the tenth leading cause of death in the U.S.,2 and in 2015 accounted for more than 44,000 deaths.3
State differences in age-adjusted suicide rates (SRs) have been well documented, with Western states generally showing higher rates.4,5 Although a more detailed understanding of geographic variation may be useful, attempts at estimating county-level SRs have been limited because the majority of counties report fewer than 20 suicide deaths per year. Direct estimates of SRs based on small numbers can be unstable and highly variable year to year, making it difficult to discern trends.6 To produce stable estimates, studies7 and web-based mapping tools3,8 often aggregate over multiple years or states, potentially masking important trends and within-state variation, including urban–rural differences.9,10
Previous studies have described urban–rural gradients in SRs and suggested that urban–rural differences may be widening, with SRs increasing more rapidly from 2000 to 2015 in less urban areas compared with more urban areas.10 However, county-level variation in SRs remains largely unexplored. More detailed examination of county-level patterns and trends, including urban–rural differences, can shed light on where SRs may have increased more rapidly and inform more targeted prevention efforts at the community level.1
Small area estimation methods11–14 can be used to produce stable estimates of mortality rates at the county level, borrowing strength from nearby counties and over time, and overcoming limitations related to aggregating data over time or larger geographic units. The objective of this study is to apply these methods to generate estimates of annual county-level SRs for 2005 through 201515 in order to examine how SRs vary across counties in the U.S. and whether these patterns are consistent over time. Additionally, this study describes urban–rural disparities and trends, and the percentage of counties within each urban–rural category reporting larger or smaller increases in SRs over time.
METHODS
Details about the statistical models and the advantages of the methods used are described elsewhere.15 A short description is provided below.
Data
The 2005–2015 National Vital Statistics System Underlying Cause of Death Files3 were used to extract the number of suicides by county of residence and year. Suicide deaths were identified using the ICD-10 underlying cause codes U03, X60–X84, Y87.0. Annual county-level population denominators were drawn from the U.S. Census intercensal (2005–2009), decennial (2010), and postcensal (2011–2015) population estimates.16
To ensure a consistent set of geographic boundaries across the study period (2005–2015), several counties in Alaska were merged and Bedford City, Virginia was merged with Bedford County, Virginia, resulting in a combined national file that included 3,140 counties.17
Urbanization level was determined using the National Center for Health Statistics Urban–Rural Classification Scheme for Counties from 2006 (applied to data years 2005–2012) and 2013 (applied to data years 2013–2015).18 The six levels of urbanization include four metropolitan and two nonmetropolitan categories (Appendix Table 1, available online) representing a continuum from most urban to most rural. From the most urban to the most rural, the categories are: large central metro (most urban), large fringe metro (i.e., suburban), medium metro, small metro, micropolitan, and noncore. Hereafter, urban refers to the four metropolitan categories (large central, large fringe, medium, and small metro).
Hierarchical Bayesian models were developed to generate annual county-level estimates in SRs.15 Models included a set of time-varying county-level covariates representing risk factors demonstrated previously to be associated with SRs. These covariates included demographic and economic factors (e.g., median age, mean household size, median household income, racial/ethnic distribution, education distribution, percent of the county that is urban, unemployment levels, foreclosure rates),19–24 divorce rates,25 prevalence of illicit drug or alcohol abuse/dependence, and prevalence of mental health conditions (e.g., major depressive episode, serious mental illness, suicidal thoughts and behaviors).26 More detailed descriptions of the covariates and data sources can be found elsewhere,15 and are outlined in the Appendix (available online).
Although most values for covariates were measured at the county level, some were measured at the substate level (groupings of counties, e.g., the prevalence of drug use or mental health conditions).27
Statistical Analysis
A series of hierarchical Bayesian spatiotemporal models were fit, using the INLA package for R, version 3.4.2.15,28,29 These models borrow strength across neighboring counties and adjacent years to produce stable estimates of SRs. Delaunay triangulation, a spatial weighting method, was used to ensure that each county has at least one neighbor, but the number of neighbors is determined empirically based on the spatial distribution of the counties.30
The hierarchical Bayesian models included several terms to account for spatial and temporal dependence.15 Annual county-level SRs were modeled as a function of the following:
a spatial random effect, which accounts for county-level spatial dependence (e.g., clustering) of SRs;
a non-spatial random effect, which accounts for any residual county-level variation that is not spatially structured;
an overall temporal random effect, which allows for the value in any given year to depend on the value in a prior year, plus an error term (i.e., type I random walk), accounting for temporal correlation in the data; and
a county- and year-specific random effect, accounting for any residual spatiotemporal variation.
Model fit was evaluated using the Deviance Information Criterion with lower values indicating better fit.31 The best-fitting model included the four random effects described above, plus several county-level covariates. Broadly, factors predictive of SRs at the county level included demographic characteristics (e.g., racial/ethnic distribution, percent of the county that is urban, divorce rates), socioeconomic factors (e.g., median household income, education distribution, unemployment rates), as well as health- and crime-related characteristics (e.g., number of property crimes, prevalence of illicit drug or alcohol abuse/dependence). Additional details about covariates, alternative models, and various model checks can be found elsewhere15 and in the Appendix (available online). Posterior predicted mean county-level SR estimates from 2005 to 2015 from the best-fitting model, including spatial and temporal random effects as well as several covariates, were mapped. Temporal trends were examined for the U.S. overall and by county urban–rural classification. Coefficients of variation (i.e., relative SEs) were used to describe the degree of uncertainty around the model-based SR estimates. All results refer to model-based or estimated posterior predicted mean SRs unless otherwise noted.
This study involved secondary analysis of existing data and did not involve human subjects, therefore, no IRB approval was required. Analyses were conducted in 2016–2017.
RESULTS
In 2005, only 365 of 3,140 (12%) counties reported ≥20 suicide deaths, the threshold under which rate estimates are typically suppressed due to concerns about statistical reliability (i.e., lack of precision because of wide SEs)6; ≅16% of counties were above this threshold in 2015. Model-based SR estimates ranged from 4.76 suicides per 100,000 people to 64.16 suicides per 100,000 people (median county-level SR=13.98 per 100,000) in 2005, and from 5.72 to 89.10 per 100,000 (median county-level SR=17.74 per 100,000) in 2015. In 2005, a total 92% of counties had estimated SRs <20 suicides per 100,000 people (the 90th percentile in 2005 was 19.4 per 100,000), in contrast to 68% of counties in 2015. Nearly all counties (99%) showed increases of >10% from 2005 to 2015 (data not shown). For 87% of counties, SRs increased by >20% from 2005 through 2015, with about one third of counties (34%) exhibiting increases of >30% (data not shown).
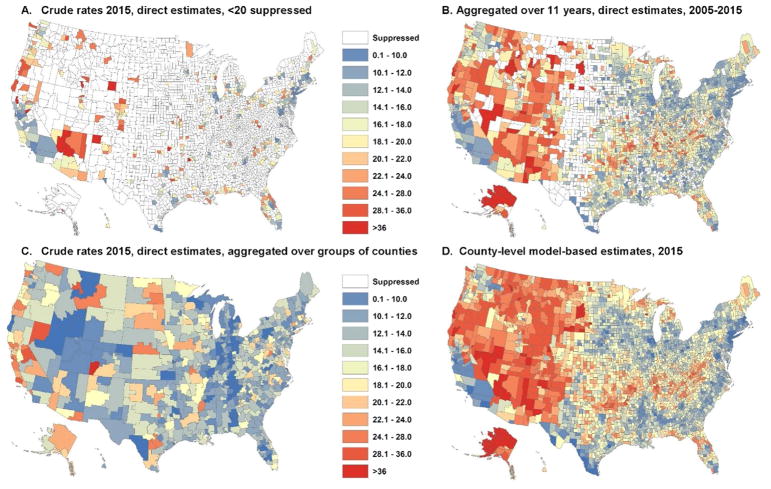
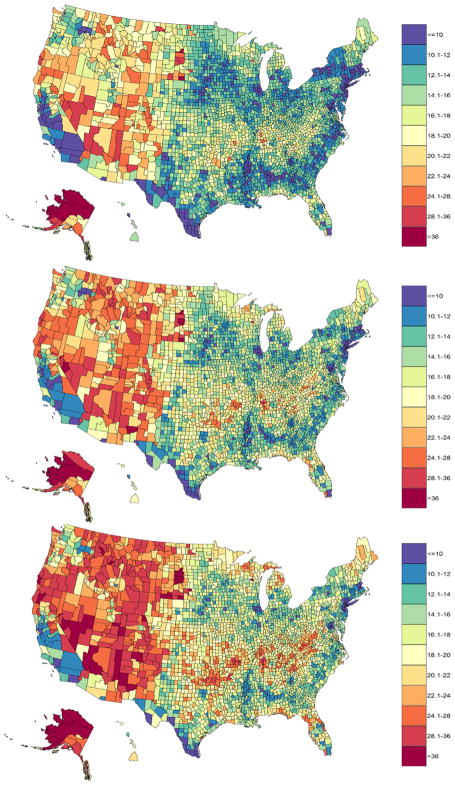
Figure 1 illustrates the value of the model-based estimates compared with other approaches of generating stable rates, namely, aggregating over time and larger geographic units. The model-based estimates indicate that geographic patterns in estimated SRs remained fairly consistent over the study period (Figure 2 and Appendix Figures 1–11, available online). Counties with the highest model-based SRs were consistently located across the western and northwestern U.S. The highest rates across the time period were seen in parts of Alaska, Arizona, northern California, Colorado, Idaho, Montana, New Mexico, Nevada, North and South Dakota, Oregon, and Wyoming (Figure 2). The lowest model-based SRs were consistently seen across southern California, Connecticut, Massachusetts, New York, Rhode Island, New Jersey, along the Mississippi river, western Texas, and along the eastern coast of North and South Carolina. The stability of the geographic pattern was also evident from consistency in the rank ordering of counties from lowest to highest model-based SRs over time (the correlation between the rankings in 2005 and 2015 was high, R2=0.95; Appendix Figure 12, available online). Maps of the uncertainty around the county-level estimates can be seen in Appendix Figure 13 (available online). All of the coefficients of variation (i.e., relative SEs/SDs) were <30%.
Figure 1.
Comparison of model-based versus direct estimates aggregated over larger geographies, or over 2005–2015.
Note: Top left figure shows the county-level suicide rates in 2015 based on direct estimates (not model-based), with white indicating that the rates are suppressed where fewer than 20 deaths were reported. Top right figure shows county-level suicide rates based on direct estimates, aggregated over 2005–2015. Bottom left figure shows county-level suicide rates aggregated to 696 larger geographic units, based on the requirement of having 20 or more deaths in the numerator. The bottom right map shows model-based county-level estimates for 2015.
Figure 2.
Model-based county-level suicide rates in the U.S., 2005 (top), 2010 (middle), and 2015 (bottom).
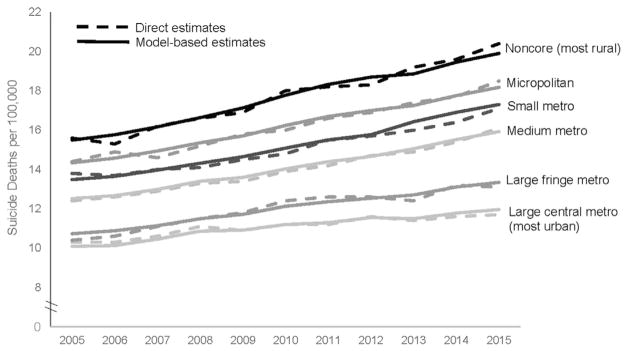
Consistent with prior analyses,10 the most rural counties (i.e., noncore) had the highest model-based SRs, and the most urban areas (i.e., large central metro) had the lowest SRs, across the time frame. Figure 3 shows the mean model-based SR by urban–rural classification, weighted by county population size, and the direct estimates of SRs by urban–rural classification for comparison. In 2005, 13% of the most rural (i.e., noncore) counties had model-based SRs of >20 suicides per 100,000 people, compared with ≤5% for nearly all other urban–rural classifications, with the exception of micropolitan (7.1%). In 2015, nearly half of the most rural (i.e., noncore) counties in the U.S. (45%) had estimated SRs of >20 per 100,000 (Appendix Table 2, available online), while ≅3% of the most urban (i.e., large central metro) counties were above this threshold. The percentages of large fringe metro, medium metro, small metro, and micropolitan counties above this threshold in 2015 ranged from 14% to 28%.
Figure 3.
Increases in suicide rates from 2005–2015 in the U.S., by urban-rural classification. Model-based and direct estimates.
Note: Urbanization level was determined using the NCHS Urban-Rural Classification Scheme for Counties from 2006 (applied to data years 2005–2012) and 2013 (applied to data years 2013–2015). Dashed lines represent direct estimates, solid lines are model-based estimates.
NCHS, National Center for Health Statistics.
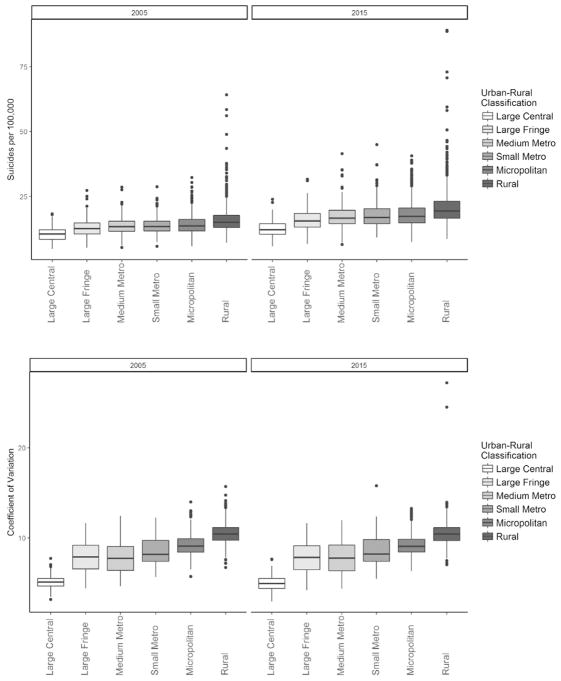
More rural counties also exhibited larger increases over the time period than more urban counties. For example, increases of >20% were seen in 93% of the most rural counties, in contrast to 79% of suburban counties, and 54% of the most urban counties (i.e., large central metro; Appendix Figure 14, available online). Nearly half of the most rural counties (49%) exhibited increases in estimated SRs of >30%, compared with 19% of suburban counties and only 10% of the most urban counties (i.e., large central metro). However, estimates for the most rural areas are also associated with a greater degree of uncertainty due to the sparsity of the data in counties with small populations. For example, the median coefficient of variation was ≅5% for large central metro counties and 10% for the most rural counties (Figure 4).
Figure 4.
Distributions of model-based suicide rates by urban-rural classification, 2005 and 2015. Median model-based suicide rates (top) and coefficients of variation (bottom), by urban-rural classification.
Note: Boxes represent interquartile ranges, points represent outliers.
DISCUSSION
From 2005 to 2015, 99% of counties showed increases in model-based SRs of more than 10%. For 87% of the counties in the U.S., estimated SRs increased by more than 20% from 2005 through 2015, with about one third of counties (34%) exhibiting increases of more than 30%. Although there was substantial geographic variation in SRs over this time period across the U.S., the geographic patterns were relatively consistent over time. Specifically, counties across the western half of the U.S. were continuously among those with the highest SRs (including Alaska), with the exception of several counties in southern California, western Texas, parts of Washington, and Hawaii. Elevated rates were also consistently seen from Oklahoma eastward through the Appalachian region, whereas counties along the eastern coast, New York, parts of the Midwest, southern California, western Texas, and along the Mississippi River tended to have the lowest SRs. In contrast to previous studies that have shown substantial shifts in the geographic patterns of drug overdose deaths and other mortality outcomes over time,32,33 the geographic footprint of SRs remained very consistent over the study period.
Consistent with previous studies,9,10 results suggest that SRs were highest in the most rural counties and lowest in more urban counties, and that more rural counties exhibited larger increases over the study period than more urban areas.
Most prior studies of geographic variation in suicide have used data aggregated by time or by state to examine spatiotemporal patterns in SRs. Results are generally consistent with the patterns reported in previous studies, with higher SRs in the western half of the U.S. and increasing over time.3–5,7,8 However, aggregating over larger geographies can mask patterns, such as the presence of both high and low rates within a state (e.g., northern versus southern California, eastern versus western Oklahoma, northern versus southern Florida), and clusters of high or low rates that cross state boundaries (e.g., the Appalachian region, along the Mississippi River). These patterns may have implications for prevention efforts. For example, they may suggest the need for broader regional efforts to address areas with high rates that cross state boundaries. Examination of county-level patterns can also inform more targeted prevention efforts by highlighting areas within a state where rates are high, or areas where protective factors can potentially be identified from counties where SRs are lower than other nearby regions.
One recent study also used small area estimation methods to examine county-level mortality trends from 1980 to 2014,32 and although the authors did not explicitly examine suicide, patterns for the grouping of self-harm and interpersonal violence were largely similar to the geographic patterns observed in this analysis. There were some notable differences between that analysis and the results presented here, however. Specifically, Dwyer-Lindgren et al.32 reported higher mortality rates from self-harm and interpersonal violence along the Mississippi River, whereas in this study’s analysis of SRs, that area stands out as falling along the lower end of the range of SRs compared with other regions of the U.S. These discrepancies could be a function of the different underlying causes of death comprising the self-harm and interpersonal violence category, different small area estimation methodologies, different time periods under study, or a combination of these factors.
Limitations
In terms of study limitations, it is possible that suicide deaths were underestimated, as suicide deaths often require lengthy investigations to determine the cause and manner of death, and are disproportionately represented in the group of deaths where the underlying cause is pending at the time of closure of the data file each year. The degree to which this varies at the county level is unknown, though the model did include state-level covariates for the percentage of records with unknown underlying cause of death or where the manner of death was pending. Additionally, some deaths classified as undetermined intent may be suicides, leading to underestimation of SRs. The magnitude of this underestimation may vary at the state or county level, and may be related to differences in death investigation and certification standards and procedures, including autopsy rates and practices.34 Some of the geographic and temporal variation in estimated SRs may be related to differences in suicide case ascertainment. There is likely variation within counties in SRs, but county is the smallest geography available in the National Vital Statistics System. This analysis used the National Center for Health Statistics Urban–Rural Classification Scheme for Counties,18 but there are other measures of urban–rural gradients that might have led to different results. Finally, there is likely variation across the U.S. in SRs by age, race/ethnicity, sex, and mechanism; more detailed examinations of these different spatiotemporal patterns may better inform prevention efforts.
This study has several strengths, including the use of an innovative method to generate stable county-level estimates of SRs across the U.S. and examine geographic and urban–rural differences, as well as temporal trends from 2005 to 2015. A variety of different models were implemented and evaluated, and results were robust to various model specifications (e.g., including covariates or not, including different random effects to account for spatiotemporal variation).15 Small area estimation methods can be used to overcome many of the challenges associated with examining geographic variation in suicide mortality at the county level. Findings may contribute to a better understanding of the epidemiologic patterns of suicide, including geographic and urban–rural differences in SRs and temporal trends.
Results suggest that there are several counties (and county clusters) across the U.S. that show concentrated regions of high or low SRs. In some cases, these regions cross state borders, whereas in other cases, a single state may contain regions of both high and low rates. Both of these types of patterns may not be evident when using state-based estimates, highlighting the importance of examining substate spatiotemporal variation. Future work examining spatial clustering and spatial outliers may provide further insights. Examining these patterns and trends can provide information to support prevention efforts and targeted interventions at the community level.1,35
CONCLUSIONS
From 2005 to 2015, estimated SRs increased by more than 20% for the majority of counties in the U.S. Counties with the highest SRs in 2005 tended to remain among the highest in 2015 and vice versa. More rural areas exhibited larger increases over the time period than more urban counties; increases of more than 20% were seen in 93% of the most rural counties, in contrast to 79% of suburban (i.e., large fringe metro) counties and 54% of the most urban (i.e., large central metro) counties. Nearly half of the most rural counties exhibited increases in SRs of more than 30% compared with 19% of suburban counties and only 10% of themost urban counties. Results may contribute to a better understanding of the epidemiologic patterns of suicide.
Supplementary Material
Acknowledgments
This work was performed under employment by the U.S. federal government; the authors did not receive any outside funding.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Center for Health Statistics, Centers for Disease Control and Prevention.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2018.03.020.
References
- 1.HHS Office of the Surgeon General and the National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. Washington, DC: HHS; 2012. [Google Scholar]
- 2.Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016;65(5):1–96. [PubMed] [Google Scholar]
- 3.National Association for Public Health Statistics and Information Systems. [Accessed December 26, 2017];Mortality–Underlying cause of death, all counties. www.naphsis.org/research-requests. Published 2017.
- 4.Karch DL, Dahlberg LL, Patel N, et al. Surveillance for violent deaths–National Violent Death Reporting System, 16 states, 2006. MMWR Surveill Summ. 2009;58(1):1–44. [PubMed] [Google Scholar]
- 5.Kim N, Mickelson JB, Brenner BE, Haws CA, Yurgelun-Todd DA, Renshaw PF. Altitude, gun ownership, rural areas, and suicide. Am J Psychiatry. 2011;168(1):49–54. doi: 10.1176/appi.ajp.2010.10020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tiwari C, Beyer K, Rushton G. The impact of data suppression on local mortality rates: the case of CDC WONDER. Am J Public Health. 2014;104(8):1386–1388. doi: 10.2105/AJPH.2014.301900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson AM, Woodside JM, Johnson A, Pollack JM. Spatial patterns and neighborhood characteristics of overall suicide clusters in Florida from 2001 to 2010. Am J Prev Med. 2017;52(1):e1–e7. doi: 10.1016/j.amepre.2016.07.032. [DOI] [PubMed] [Google Scholar]
- 8.CDC. [Accessed January 24, 2017];Web-based Injury Statistics Query and Reporting System Fatal Injury Mapping Module. www.cdc.gov/injury/wisqars/WISQARS-Mapping-Module.html. Published 2017.
- 9.Chen LH, Ingram DD. QuickStats: Age-adjusted rates for suicide,* by urbanization of county of residence† — United States, 2004 and 2013. MMWR Morb Mortal Wkly Rep. 2015;64(14):401. [Google Scholar]
- 10.Kegler SR, Stone DM, Holland KM. Trends in suicide by level of urbanization—United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):270–273. doi: 10.15585/mmwr.mm6610a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang SS, Sterne JA, Wheeler BW, Lu TH, Lin JJ, Gunnell D. Geography of suicide in Taiwan: spatial patterning and socioeconomic correlates. Health Place. 2011;17(2):641–650. doi: 10.1016/j.healthplace.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Congdon P. Bayesian models for spatial incidence: a case study of suicide using the BUGS program. Health Place. 1997;3(4):229–247. doi: 10.1016/S1353-8292(97)00017-8. [DOI] [Google Scholar]
- 13.Lawson A. Bayesian Disease Mapping: Hierarchical Modeling in Spatial Epidemiology. Boca Raton, FL: Chapman & Hall/CRC Press; 2013. [Google Scholar]
- 14.Khan D, Rossen LM, Hamilton B, Dienes E, He Y, Wei R. Spatiotemporal trends in teen birth rates in the USA, 2003–2012. J R Stat Soc Ser A Stat Soc. 2018;181(1):35–58. doi: 10.1111/rssa.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan D, Rossen LM, Hedegaard H, Warner M. A Bayesian spatial and temporal modeling approach to mapping geographic variation in mortality rates for subnational areas with R-INLA. J Data Sci. 2018;18:147–182. [PMC free article] [PubMed] [Google Scholar]
- 16.CDC, National Center for Health Statistics. National Vital Statistics System. U.S. Census Populations with Bridged Race Categories; [Accessed April 25, 2018]. www.cdc.gov/nchs/nvss/bridged_race.htm. [Google Scholar]
- 17.CDC, National Center for Health Statistics. [Accessed April 25, 2018];County Geography Changes: 1990–2015. www.cdc.gov/nchs/nvss/bridged_race/county_geography-_changes2015.pdf. Published 2016.
- 18.Ingram DD, Franco SJ. NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat 2. 2014:166. [PubMed] [Google Scholar]
- 19.Houle JN, Light MT. The home foreclosure crisis and rising suicide rates, 2005 to 2010. Am J Public Health. 2014;104(6):1073–1079. doi: 10.2105/AJPH.2013.301774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerr WC, Kaplan MS, Huguet N, Caetano R, Giesbrecht N, McFarland BH. Economic recession, alcohol, and suicide rates: comparative effects of poverty, foreclosure, and job loss. Am J Prev Med. 2017;52(4):469–475. doi: 10.1016/j.amepre.2016.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lester D. Explaining regional differences in suicide rates. Soc Sci Med. 1995;40(5):719–721. doi: 10.1016/0277-9536(95)80015-C. [DOI] [PubMed] [Google Scholar]
- 22.Rezaeian M, Dunn G, St Leger S, Appleby L. Do hot spots of deprivation predict the rates of suicide within London boroughs? Health Place. 2007;13(4):886–893. doi: 10.1016/j.healthplace.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Congdon P. Assessing the impact of socioeconomic variables on small area variations in suicide outcomes in England. Int J Environ Res Public Health. 2012;10(1):158–177. doi: 10.3390/ijerph10010158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Congdon P. Latent variable model for suicide risk in relation to social capital and socio-economic status. Soc Psychiatry Psychiatr Epidemiol. 2012;47(8):1205–1219. doi: 10.1007/s00127-011-0429-x. [DOI] [PubMed] [Google Scholar]
- 25.Hempstead K. The geography of self-injury: spatial patterns in attempted and completed suicide. Soc Sci Med. 2006;62(12):3186–3196. doi: 10.1016/j.socscimed.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 26.Crosby AE, Han B, Ortega LA, et al. Suicidal thoughts and behaviors among adults aged ≥18 years–United States, 2008–2009. MMWR Surveill Summ. 2011;60(13):1–22. [PubMed] [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. [Accessed January 24, 2017];Substate Estimates. www.samhsa.gov/samhsa-data-outcomes-quality/major-data-collections/state-reports-NSDUH/2012-2014-substate-reports. Published 2016.
- 28.Bivand RS, Rubio-Gomez V, Rue H. Spatial data analysis with R-INLA with some extensions. J Stat Softw. 2015;63(20) doi: 10.18637/jss.v063.i20. [DOI] [Google Scholar]
- 29.Rue H, Martino S, Chopin N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Series B Stat Methodol. 2009;71(2):319–392. doi: 10.1111/j.1467-9868.2008.00700.x. [DOI] [Google Scholar]
- 30.Bivand R. Creating Neighbours. The Comprehensive R Archive Network; [Accessed January 24, 2017]. https://cran.r-project.org/web/packages/spdep/vignettes/nb.pdf. Published 2017. [Google Scholar]
- 31.Spiegelhalter DJ, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit (with discussion) J R Stat Soc Series B Stat Methodol. 2002;64(4):583–639. doi: 10.1111/1467-9868.00353. [DOI] [Google Scholar]
- 32.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. U.S. county-level trends in mortality rates for major causes of death, 1980–2014. JAMA. 2016;316(22):2385–2401. doi: 10.1001/jama.2016.13645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossen LM, Bastian B, Warner M, Khan D, Chong Y. [Accessed December 11, 2017];Drug poisoning mortality: United States, 1999–2015. www.cdc.gov/nchs/data-visualization/drug-poisoning-mortality/index.htm. Published 2017.
- 34.Claassen CA, Yip PS, Corcoran P, Bossarte RM, Lawrence BA, Currier GW. National suicide rates a century after Durkheim: do we know enough to estimate error? Suicide Life Threat Behav. 2010;40(3):193–223. doi: 10.1521/suli.2010.40.3.193. [DOI] [PubMed] [Google Scholar]
- 35.Stone DM, Holland KM, Bartholow B, Crosby AE, Davis S, Wilkins N. Preventing Suicide: A Technical Package of Policies, Programs, and Practices. Atlanta, GA: National Center for Injury Prevention and Control, CDC; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.