Abstract
The aim of therapeutic neovascularization is to repair ischemic tissues via formation of new blood vessels by delivery of angiogenic growth factors, stem cells or expansion of pre-existing cells. For efficient neovascularization, controlled release of growth factors is particularly necessary since bolus injection of molecules generally lead to a poor outcome due to inadequate retention within the injured site. In this regard, injectable hydrogels, made of natural, synthetic or hybrid biomaterials, have become a promising solution for efficient delivery of angiogenic factors or stem and progenitor cells for in situ tissue repair, regeneration and neovascularization. This review article will broadly discuss the state-of-the-art in the development of injectable hydrogels from natural and synthetic precursors, and their applications in ischemic tissue repair and wound healing. We will cover a wide range of in vitro and in vivo studies in testing the functionalities of the engineered injectable hydrogels in promoting tissue repair and neovascularization. We will also discuss some of the injectable hydrogels that exhibit self-healing properties by promoting neovascularization without the presence of angiogenic factors.
Keywords: Injectable hydrogels, Neovascularization, Tissue regeneration, Angiogenic factors, Cell-therapy
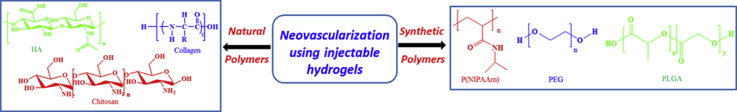
Graphical abstract
Highlights
-
•
Discuss the development of injectable hydrogel from natural and synthetic precursors and their applications.
-
•
In vitro and in vivo studies in testing the functionalities of the injectable hydrogels.
-
•
Highlight the efficacy of injectable hydrogels as the carrier of angiogenic growth factors in promoting neovascularization.
-
•
Discuss about several self-healing injectable hydrogels that promote neovascularization in absence of angiogenic factors.
1. Introduction
During the past few decades, scholars have extended significant effort to develop minimally invasive injectable remedies, using catheters or syringes, for targeted cell therapy and drug delivery [1]. At the same time, hydrogels have gained importance as suitable scaffolding biomaterials for cell/drug delivery and regeneration of damaged tissues or organs [2]. Hydrogels are two-component semi-solid system, composed of polymer and water, where the polymer forms an extensive network and water is trapped in it. Based on their rheological properties, hydrogels are viscoelastic in nature. Injectable hydrogels belong to a class of biomaterial that are frequently injected in liquid state, and then form a solid gel in situ. These types of hydrogels can be categorized based on their chemical or physical crosslinking property. The polymer networks can be formed either by the physical interactions between the polymer molecules or by forming a covalent chemical bond between one or more polymers or by a combination of these modes [[3], [4], [5]] Structural, mechanical, and biological properties of injectable hydrogels are strongly influenced by the material cross-linking (type and concentration of physical or covalent bonding) properties. Injectable hydrogels should be porous, nontoxic, biocompatible (not harmful to living tissue), and have proper mechanical stability and biodegradability. Injectable hydrogels with higher mechanical stability exhibit improved cell-based tissue regeneration [6] and serve as better delivery platforms due to their ability to control the diffusion of entrapped growth factors, nutrients or metabolites [7]. The gelation kinetics of injectable hydrogels also plays an important role in its efficiency as a delivery scaffold. If the gel forms too fast, then it is difficult to inject and if it forms too slowly, then the network formation, adaption, and recovery may be too slow for effective 3D cell encapsulation as the solution can flow away from the injected site [8]. Moderate to rapid rates of gel formation is desirable for most tissue engineering or drug/cell delivery applications as it facilitates a homogeneous cell distribution during encapsulation by preventing cell sedimentation or aggregation [8]. Additionally, it prevents undesirable diffusion of the polymers away from the injection site before the gel formation [9].
A newer approach of regenerative tissue engineering, involving injectable hydrogels, is based on shape memory polymers [[10], [11], [12], [13], [14]]. Shape memory polymers are able to recover their original shapes after large deformation when subjected to external stimuli such as temperature, magnetism, moisture, or light [10]. Previous reports have demonstrated that shape memory polymers can be promisingly used as injectable scaffolds in cell therapy [12], cardiac tissue engineering [13], bone tissue engineering [14] etc. Another alternate strategy to enhance the therapeutic efficacy of injectable hydrogels is based on the use of shear thinning materials [15,16]. In a shear thinning hydrogel, the gel has lower viscosity and flows under shear of injection. Once the shear stress is removed, gel restores its rigidity and remains localized at the point of injection [15,16]. Colloid gels, derived from colloid particles, also displays shear thinning behavior [[17], [18], [19]].
In the past few years, injectable hydrogels have gained notable attention for a wide range of clinical therapeutic applications, among them cardiovascular, endovascular, orthopedic, and dental [20]. In this regard, one of the significantly important applications of injectable hydrogels is in neovascularization of ischemic tissues/organs such as ischemic heart, musculoskeletal, etc. [21,22]. This specific application of injectable hydrogels is critically important, as vascularization remains to be one of the major bottlenecks in regenerative medicine. Neovascularization can take place by three processes: angiogenesis, vasculogenesis and arteriogenesis [23]. Angiogenesis is the formation of new blood vessels from the existing blood vessels via migration, growth, and differentiation of endothelial cells (ECs) inside wall of blood vessels, whereas vasculogenesis is the formation blood vessel via de novo assembly of ECs [23]. On the other hand, arteriogenesis is the increase in the diameter of existing arterial vessels. Injectable hydrogels derived from natural polymers such as fibrin and gelatin can promote neovascularization without incorporation of angiogenic factors or stem cells, due to their natural binding sites for solubilized growth factors and cellular integrin receptors [21]. Neovascularization can be also triggered by incorporation of growth factors such as vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), platelet derived growth factor (PDGF), angiopoitin-1 [23], as well as VEGF mimetic synthetic peptides. Therapeutic neovascularization is expected to take place for several weeks or months with persistent stimulation of growth factors [24]. However, the delivery of angiogenic growth factors alone based on a bolus injection results in a burst and short period of biological activity within the injured zone [21]. With respect to cell-based therapies, in the majority of clinical trials, stem cells are injected directly in the ischemic area, which result in around 90% cell loss during injection [22], and poor viability. Therefore, to prohibit cell loss and achieve prolonged and sustained release of angiogenic factors, injectable hydrogels have been at the center of attention for efficient delivery of growth factors or cells. In this review article, we report recent advancements in the development of injectable hydrogels, derived from natural and synthetic biomaterials, with an emphasis on their application in neovascularization via controlled delivery of angiogenic factors or cells (see Table 1).
Table 1.
Brief summary of the injectable hydrogels and their effects during assay.
| Hydrogels | Assay | Factors | Effect |
|---|---|---|---|
| Chitosan | In vivo | FGF-2 | Neovascularization by controlled growth factor release [35]. |
| In vitro & | Acellular | Better spreading and assembly of cultured HUVECs in the in vitro study [36] and branching of capillary networks in the subcutaneous area [36]. | |
| In vivo | |||
| In vivo | Acellular | Increase of M2 macrophage response and neovascularization [34]. | |
| In vitro & | Acellular | Increased vasculogenesis in the in vitro study [37] confirmed by significant angiogenesis and better blood circulation in the in vivo study [37]. | |
| In vivo | |||
| In vivo | ESC/bFGF | Improvement of myocardial ischemia (MI) [[38], [39], [40]]. | |
| In vivo | Acellular | Better angiogenic activity in peptide modified gel [41]. | |
| HA | In vivo | EPC | Significant increase of vascularization leading to improvements in myocardial remodeling [45] |
| In vivo | ESA | Retention of the infarcted tissue by vasculogenesis [46]. | |
| In vivo | Acellular & ADSC | Significant healing of the damaged skin by rapid cell proliferation and angiogenesis [47,48]. | |
| In vivo | HADSC | Wound healing in the ischemic heart due to angiogenesis [49]. | |
| In vivo | Acellular | Functional recovery of infarcted heart due to the increased number of arterioles and capillaries [50] | |
| In vivo | bFGF | Considerable increase of neovascularization [51]. | |
| Collagen | In vivo | Acellular | Angiogenesis in the infarcted region of myocardium [53]. |
| In vivo | CAC | Increased mechanical stability as well as expression level of proangiogenic cytokine [54]. | |
| In vivo | PC | Higher arteriole and capillary density in the hindlimb muscle [55]. | |
| Gelatin GHPA GelMA |
In vivo | bFGF | Significant prolonged and transient neovascularization from bFGF loaded acidic and basic gelatin hydrogel respectively [66]. |
| In vivo | bFGF | Significant increase of the collateral vessel formation with bFGF loaded AGHMs in the ischemic hindlimb [67]. | |
| In vitro & | VEGF | Sustained release of VEGF from the gel with high bioactivity [68] | |
| In vivo | Significant angiogenesis by the increase of blood vessel density [68]. | ||
| In vivo | bFGF and BDNF | Higher vessel density and LVEF in the ischemic myocardium [69]. | |
| In vivo | bFGF and hCDC | Neoangiogenesis and significant retention of transplanted hCDCs in the ischemic area leading to improved cardiac function [70]. | |
| In vivo | CM | Efficient engraftment of CMs with the host and significant increase of angiogenic cytokines [71]. | |
| In vivo | MSC | Extensive neovascularization [72]. | |
| In vivo | VEGF | Angiogenesis in VEGF loaded GelMA hydrogel [73]. | |
| In vivo | VEGF | Vascularization by significant increase of capillary and arteriole density in the infarct region, resulting in improved cardiac function [75]. | |
| Fibrin | In vivo | With and without SM | Neovascularization causing the reduction of infarcted myocardium both with or without SM [78] as well as significant increase of cell survival [79]. |
| In vivo | Acellular | Neovascularization resulting improvements in cardiac function by reducing infarct scar percentage [80]. Significant increase of neovascularization of the bone-defect area [72,83]. | |
| In vitro & | bFGF | Decreased bFGF release rate in the in vitro study was confirmed by increased neovascularization in the ischemic sites [84]. | |
| In vivo | |||
| In vitro | VEGF | Increased growth of cells in the presence of VEGF modified fibrin gel [85]. | |
| In vivo | VEGF | Angiogenesis in the muscle indicated by significant increase in the vessel length density due to the controlled release of VEGF [86]. | |
| PNIPAAm | In vivo | bFGF | Increased angiogenesis resulting in a 2-fold improvement in relative blood flow to the infarcted myocardium [89]. |
| Considerable recovery of cardiac function in the chronic infarcted myocardium due to increased angiogenesis [90]. | |||
| PEG | In vivo | VEGF | Significant neovascularization due to the sustained release of VEGF [91]. |
| In vivo | C16 and Ac-SDKP | Promotion of angiogenesis, muscle regeneration and minimized detrimental inflammation in the peripheral artery disease [92] | |
| In vivo | VEGF | Neovascularization by the sustained release of VEGF in the infract region [93]. | |
| In vivo | VEGF | Enhanced angiogenesis and space filling of the cornea micropocket [94]. | |
| In vivo | HGF and VEGF | Significant increase in angiogenesis, stem cell recruitment, and decrease in fibrosis was observed in the dual growth factor delivery group [95]. | |
| In vivo | CPC | Non-adhesive RDG gels codelivered with CPCs showed improved cardiac function whereas ECM-derived adhesive peptide-presenting gels failed to show the recovery of cardiac function [96]. | |
| In vivo | VEGF | Lowest degradation time for in situ polymerized hydrogel and highest vascularization from the injectable microbeads due to the VEGF release [97]. | |
| PLGA | Significant enhancement of angiogenic activity due to the controlled release of bFGF in the ischemic tissue [99]. | ||
| Synthetic peptide | In vitro & | IGF-1C | Increased stem cell viability in presence of IGF-1C hydrogel in the in vitro and in vivo study resulting in the increase of in vivo angiogenesis [100]. |
| In vivo | ADSC | ||
| In vivo | Acellular | Increased blood vessel formation in the VEGF memetic peptide than non angiogenic peptide [101]. Formation of mature blood vessels and preservation of ischemic tissue structure and function [102]. |
2. The classes of injectable hydrogels
Injectable hydrogels are derived from biomaterials, that can be natural or synthetic or a combination of these referred to as hybrid. Chemical structures of a few of these natural and synthetic polymers have been presented in Fig. 1, Fig. 2. These biomaterials are used alone or in mixtures, can give rise to the formation of polymers with various properties [25]. The choice of biomaterial for the injectable hydrogel is a critical aspect for a specific target application. The biomaterial should be non-toxic, biodegradable and able to integrate with the host tissue. Natural polymers such as chitosan, gelatin, fibrinogen, hyaluronic acid and collagen have advantages over synthetic polymer as they promote cellular adhesion and infiltration due to the presence of cell adhesion moieties. Natural polymers also contain specific bioactive molecular domains that can enhance biological interactions between the material and the host [[26], [27], [28]]. These polymers, including injectable hydrogels, have already been used in clinical applications [27,28].
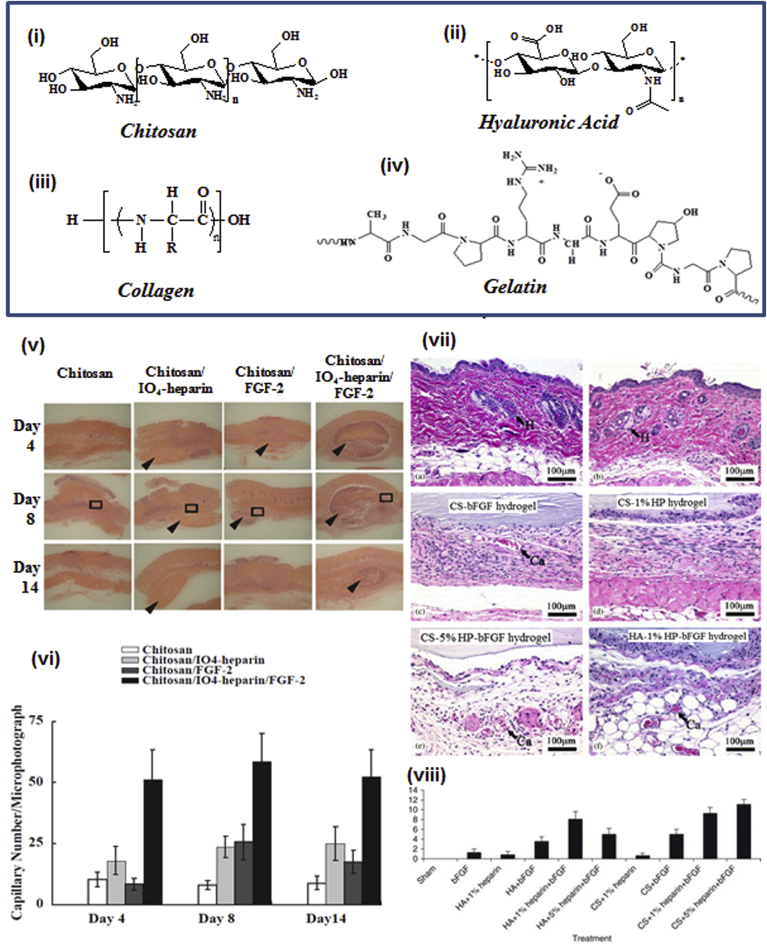
Fig. 1.
(i-iv) Chemical structure of natural polymers being used as injectable hydrogel scaffold. (v) Representative H&E stained histological images of the vascularization for the different groups of injected chitosan hydrogel using rat model on day 4, 8, and 14 post-injection. (vi) Quantification of capillary number for different injection groups on Day 4, 8 and 14. (Adapted with permission from Elsevier [Biomaterials] copyright (2004)[35]. (vii) Representative H&E stained histological images of skin and subcutaneous tissue after 14 days of surgery with different groups of implantation. (vii) Neovascularization index after day 14 of the surgery. (Adapted with permission from Elsevier [Biomaterials] copyright (2005) [51].
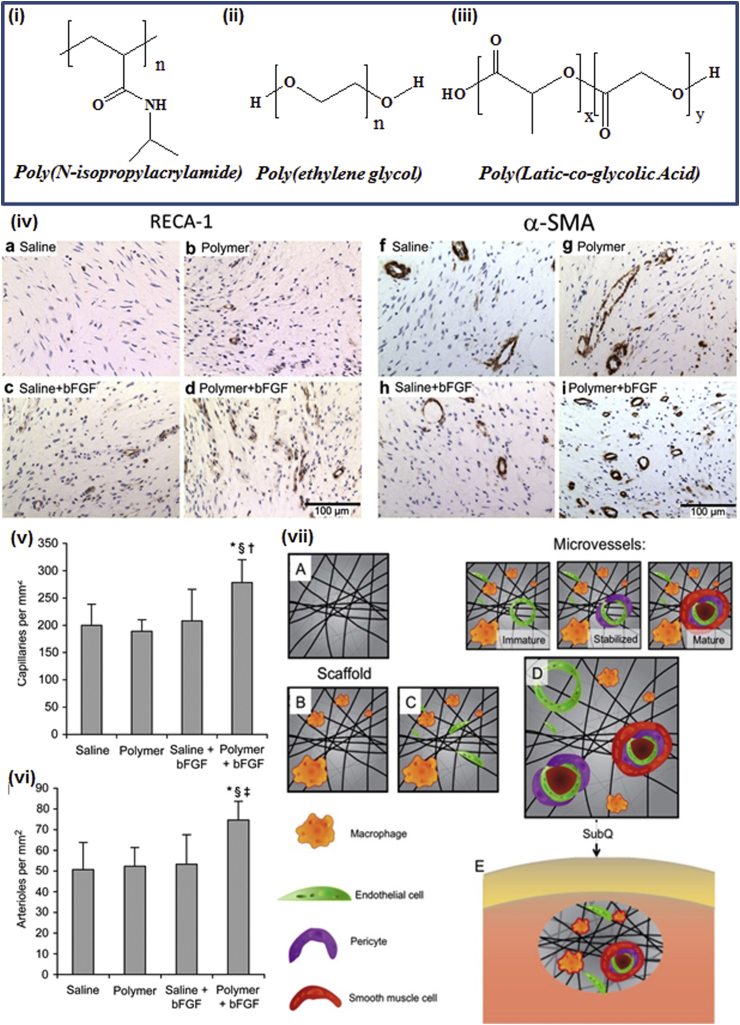
Fig. 2.
(i-ii) Chemical structures of synthetic polymers being used as injectable hydrogel scaffold. (iv) Angiogenic effects due to the release of bFGF from pH-responsive p (NIPAAm-co-PAA-co-BA) hydrogel. Representative images of the histological sections of the tissues with rat endothelial cell antigen-1 (RECA-1) staining (a-d) and smooth muscle α-actin (α-SMA) staining (f-i). Quantification of capillary density by RECA-1 (v) and arteriolar density by α-SMA (vi) staining. (Adapted with permission from Elsevier [Biomaterials] copyright (2011)[89]. (vii) Schematic representation of proposed mechanism of wound healing using nanofibrous SLanc hydrogels (A-D). (Adapted with permission from ACS Publications [ACS Nano] copyright (2015) [101].
On the other hand, synthetic hydrogels have several advantages over natural hydrogels. Synthetic hydrogels readily allow precise control over critical material properties including polymerization, degradation and mechanical stiffness. Synthetic polymers have been hybridized with natural biopolymers to engineer native like extracellular matrix (ECM) with controlled biophysical and biochemical properties. In the following sections we will cover different types of natural and synthetic injectable hydrogels, which have been used for neovascularization application [28].
2.1. Natural injectable hydrogels for neovascularization
2.1.1. Chitosan
Chitosan (CS) is a linear polysaccharide composed of d-glucosamine and N-acetyl-d-glucosamine. It is prepared by deacetylation of chitin from crustacean shells [29] with an alkaline substance like sodium hydroxide. CS has been widely used in several biomedical applications [[30], [31], [32], [33]] because of its biocompatibility, biodegradability, antimicrobial property, nontoxicity, and proper cell binding capability. However, the poor solubility of chitosan in physiological solvents, such as phosphate buffer saline (PBS) makes it challenging for the use in the form of an injectable hydrogel scaffold [34]. To address this problem, investigators have produced hydrogels by mixing chitosan with other natural polymers [28] for the formation of bio-hybrid injectable scaffolds. Apart from poor solubility, fast biodegradation in situ and possible allergic reactions of the residual proteins during chitosan preparation are some of the other major disadvantages of chitosan-based biomaterials [29].
To date, several chitosan-based hydrogels have been developed for delivery of growth factors and stem cells for neovascularization. For example, an injectable chitosan/heparinoid hydrogel was used by Fujita et al. for entrapment and sustained release of FGF-2 for neovascularization in a mouse model [35]. Significant increase in the formation of capillary networks after the injection of FGF-2 loaded hydrogel as compared to the injection of FGF-2 alone confirmed that the promotion of neovascularization was due to controlled growth factor release (Fig. 1v and vi).
Several acellular neovascularization approaches have also explored the use of chitosan based hydrogels. For instance, Deng et al. studied vasculogenesis in vitro by human umbilical vein endothelial cells (HUVECs) using collagen-chitosan injectable hydrogel [36]. In this study, chitosan was added in different ratio to a collagen matrix via 1-Ethyl-3-(3-dimethylaminopropyl) carbodiimide/N-hydroxysuccinimide (EDC-NHS) chemistry. Several studies on the physical properties including injectability, denaturation temperature, and the mechanical strength measurements indicated that the gel strength enhanced with the increased ratio of chitosan, leading to better spreading and assembly of HUVECs. Specifically, the authors suggested that a higher ratio of chitosan in the gel enhanced the tubular network formation by HUVECs by increasing ‘total capillary tube length’ and ‘total area covered’. The result of the in vitro study was supported by in vivo study, performed by acellular implantation of the hydrogel scaffold via subcutaneous injection, where branching of capillary networks was observed only in collagen:chitosan with 1:1 ratio. In another study, Deng et al. used an injectable chitosan-based hydrogel to study the tissue regeneration in the defected abdominal wall of a rat model [34]. The gel was formed via Schiff base reaction of N,O-carboxymethyl chitosan (NOCC) and aldehyde hyaluronic acid (A-HA). The gelation time of this hydrogel was tunable by altering the ratio of NOCC and A-HA and hence it could be optimized for injection in the affected tissue zone. Considerable increase of M2 macrophage response and neovascularization in the defected wall was observed causing anti-inflammation, tissue repair and remodeling of the affected area in response to the injected hydrogel. The authors suggested that vascularization was promoted due to the sufficient supply of nutrients and oxygen to the cells because of the enhanced porosity of the three-dimensional (3D) structure of the hydrogel matrix. Recently, a novel chitosan-fibrin-based self-healing hydrogel was developed by Hsieh et al. [37]. In this study, a chitosan-based interpenetrating polymer network (IPN) hydrogel (composition: 1.5% glycol chitosan, 1% difunctional poly (ethylene glycol) (PEG), 0.005% fibrinogen and 0.002% thrombin) was used to study in vitro vasculogenesis using ECs. Polymerase chain reaction (PCR) data indicated an increased level of ‘vasculogenesis marker gene expression’ leading to significantly increased branch length and branch point density of the endothelial network within the IPN gel compared to control gel (fibrin hydrogel consisting 0.5% fibrinogen and 0.2% thrombin). Also, in an in vivo study, injection of this chitosan-fibrin hydrogel in zebrafish and mice models demonstrated significant angiogenesis in the perivitelline space of zebrafish and enhanced blood circulation in the ischemic hindlimbs of mice.
Chitosan-based injectable hydrogels have also been widely used in cardiac tissue engineering to promote vasculogenesis/angiogenesis. Wang et al. studied the improvement of myocardial ischemia (MI) healing by co-injection of chitosan hydrogel with embryonic stem cell (ESC) or bFGF [[38], [39], [40]]. After MI, the infarcted myocardium undergoes hypoxia due to lack of functional vasculogenesis limiting the supply of oxygen to the injured tissue. A synthetic peptide (RoY) modified chitosan-based injectable hydrogel was prepared by the same group to address this problem [41]. For preparing this hydrogel, chitosan chloride was reacted to the RoY synthetic peptide forming a chitosan-peptide (CS-RoY) conjugate via an amide linkage. Vascularization was studied in vitro with HUVECs under hypoxia as well as in an in vivo rat model. The results showed better angiogenic activity in CS-RoY gel compared to chitosan gel. The authors explained this phenomenon as the activation of Akt and ERK1/2 signaling pathways by the expression of GRP78 receptors of HUVECs, which is related to their survival and proliferation.
2.1.2. Hyaluronic acid
Hyaluronic acid (HA) or hyaluronan, is a unique anionic, nonsulfated glycosaminoglycan, biosynthesized at the plasma membrane which is distributed in connective, epithelial, and neural tissues [42]. It is a linear polymer, comprising of repeated disaccharide unit of d-glucuronic acid and N-acetyl-d-glucosamine. HA is one of the chief components of the ECM, and plays a significant role in cell proliferation and differentiation [43]. A number of approaches have been utilized chemical and physical crosslinking techniques to improve the mechanical properties, biodegradation, and biocompatibility of HA as an injectable hydrogel [44] for cell-based therapies. For instance, in a recent study by Gaffey endothelial progenitor cells (EPC) were delivered into ischemic myocardium using a novel injectable shear thinning HA hydrogel [45]. This hydrogel was assembled by host-guest interaction of both adamantine and β-cyclodextrin modified HA. A significant increase of vascularization was found in EPC embedded gel constructs, leading to improved ventricular function and myocardial remodeling, compared to blank gel or bolus injection of EPCs. MacArthur et al. developed a HA-based injectable hydrogel for sustained release of engineered stromal cell-derived factor (ESA) (4 weeks) to preserve ventricular function after MI in a rat model [46]. The gel was a hydroxyethylmethacrylate modified HA with terminal double bonds which underwent free radical initiated crosslinking. ESA is an EPC chemokine, which induced EPC to retain in the infarcted tissue of rat in an in vivo study and subsequently promoted vasculogenesis. In another study, an HA-chitosan injectable hydrogel was developed by Jiang et al. for promoting skin regeneration in a mouse skin defect model [47]. The aldehyde group modified HA was reacted with chitosan to form the gel network via Schiff base linkage between aldehyde and amine groups of chitosan. The authors observed significant wound healing upon injection of this hydrogel in damaged skin attributed to rapid cell proliferation and angiogenesis. Later, the same group performed a cell therapy study with the same HA-chitosan hydrogel [48]. The synthesized hydrogel was used as a carrier for injection of adipose derived stem cells (ADSC) into a skin defect mouse model. The author claimed that this cell-laden hydrogel accelerated wound closure by enhancing the cell proliferation and angiogenesis. Park et al. also used a HA-based injectable hydrogel as a carrier of human adipose derived stem cell (HADSC) for tissue regeneration in healing of tissue defects [49]. In this study, a catechol functionalized HA-based hydrogel was synthesized by reaction between HA and dopamine hydrochloride via EDC-NHS chemistry and the gel was used to test its efficacy in a tissue defect model. The cell-laden hydrogel was injected in ischemic hind limb of mouse as well as in a critical size bone-defect model. High cellular viability, up to day 7, indicated the biocompatibility of the hydrogel, while the ELISA data confirmed high levels of VEGF secretion from the cell-laden hydrogel. The authors suggested that wound healing within the ischemic area was promoted by angiogenesis, triggered by survival and migration of the ECs. In another study, Yoon et al. developed a HA-based hydrogel that was able to restore the functionalities of infarcted rat heart upon injection without presence of any stem cell or growth factor [50]. The hydrogel was formed using Michael-type addition reaction between acrylated HA and thiolated PEG. From the histological studies, the authors observed that the numbers of arterioles and capillaries were increased by 152% and 148% in the infarcted region upon injection of the HA hydrogel. In another study, Cai et al. developed a thiol modified HA-heparin conjugate along with a thiol modified chondroitin sulfate-heparin hydrogel for tissue vascularization [51]. The role of thiolated heparin was to provide a cross-linkable analog with the thiolated HA or chondroitin sulfate. They incorporated basic fibroblast growth factor (bFGF) within the hydrogel and assessed the efficacy of vascularization in vivo. The synthesized biomaterial was biodegradable, injectable and capable of controlled release of bFGF. Upon injection of the hydrogel into subcutaneous pockets in Balb/c mice, considerable increase of neovascularization was observed with HA and chondroitin sulfate hydrogels containing both bFGF and cross-linked heparin (Fig. 1 vii and viii). In contrast, hydrogels without bFGF and/or cross-linked heparin showed minimal increase in neovascularization.
2.1.3. Collagen
Collagen is the main structural protein of the ECM of skin, bone, tendons, ligaments, and cartilage of mammalian tissues [28]. Collagen type I is the most copious in human body [23]. Collagen is thermo-reversible, biocompatible and amenable to enzymatic (collagenase) degradation. However, high synthesis cost, low physical strength, poor mechanical stability are significant challenges associated with the use of collagen [28]. Collagen has been engineered by chemical cross-linking with different substrates for improvement of its physical strength and cell adhesion capacity [28]. Additionally, collagen has been successfully used as a natural hydrogel for repair of MI in vivo. However, vascular formation is strongly dependent on the concentration of collagen. For example, Dai et al. injected 100 μL of 65 mg/mL collagen hydrogel [52] and Huang et al. injected 50 μL of 1 mg/mL collagen hydrogel [53] in a rat MI model. The first group found no angiogenesis in the infarcted region although the wall thickness increased six-week post injection. On the other hand, the second group found considerable amount of angiogenesis after 5 weeks of injection. Therefore, based on these studies, proper optimizations of the concentration of collagen in the hydrogels could impact the efficiency of vascularization and myocardial repair.
MaBane et al. developed a collagen:chitosan (10:1) injectable hydrogel with and without circulating angiogenic cells (CACs) to generate a pro-angiogenic environment in a type 1 diabetic (T1D) mouse model [54]. The mechanical stability of collagen-chitosan gel was found to be higher than pure collagen gel, with enhanced CACs cellular viability. Within the in vivo experiments, collagen-chitosan gel was implanted subcutaneously in a T1D mouse model. Although the authors observed increased expression of proangiogenic cytokines in collagen-chitosan implants, they did not observe significant neovascularization.
Collagen-derived injectable hydrogels have also been used for cell-based therapies. Suuronen et al. demonstrated a novel technique for expansion and delivery of CD133+ progenitor cells with improved capacity of vascularization [55]. Adult human CD133+ progenitor cells (PC) were loaded in an injectable collagen-based matrix and delivered into the ischemic hindlimb of athymic rats to study vascularization. Immunohistochemistry of hindlimb muscle after 2 weeks of treatment indicated higher density of arterioles and capillaries as compared to other treatment groups receiving injections of phosphate-buffered saline, matrix, or only CD133+ cells.
2.1.4. Gelatin
Gelatin is essentially a denatured collagen, synthesized by acid or alkaline hydrolysis of collagen [23]. Gelatin forms a thermo-reversible, transparent gel below the sol-gel transition temperature (∼40 °C) via physical interactions between collagen molecules [23]. Gelatin-based hydrogels do not enhance thrombogenicity and have pro-angiogenic properties [56]. Therefore they have been used as a scaffolding biomaterial for tissue engineering of ‘highly’ vascularized organs [57] and also in the cell-based therapies after heart failure. Additionally, derivatives of gelatin has shown promising applications for tissue regeneration [[58], [59], [60], [61], [62], [63], [64]], cancer studies [60] as well as for angiogenic growth factor delivery and vascularization [[65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75]] due to the presence of bioactive sequences [23]. Tabata et al. studied the release of bFGF incorporated in both acid and basic gelatin-based hydrogels to promote neovascularization induced by the biodegradation of the hydrogels [66]. For preparing the hydrogel, aqueous solution of bFGF was primarily absorbed in gelatin. bFGF, being positively charged, complexes with acidic gelatin, but not in basic gelatin. Therefore, the release of bFGF from acidic gelatin was better sustained (only 30% in 1 day in PBS at 37 °C) compared to basic gelatin (100% in the same time frame). Significant prolonged neovascularization was observed when bFGF loaded acidic gelatin was injected into ischemic mouse model. The period of neovascularization could be altered by changing the water content in the gelatin hydrogel. On the other hand, only transient neovascularization was observed with the basic gelatin hydrogel. The authors suggested that prolonged vascularization was due to sustained release of bFGF from acidic gelatin hydrogel and transient vascularization was due to the initial burst release of bFGF from basic gelatin hydrogel. This observation was later confirmed in another study by Hosaka et al. [67]. They developed functional collateral vessels by injection of bFGF-loaded acidic gelatin hydrogel microspheres (AGHMs) in a hindlimb ischemia model of rabbit. Percentage of delivered bFGF was dependent on the diameter of the microspheres. Twenty eight days post-injection, a significant increase of collateral vessel formation was observed in bFGF loaded AGHMs as compared to PBS (i.e. control) treated AGHMs. In another study, Li et al. developed a modified gelatin-based hydrogel to study angiogenesis by the release of VEGF in a mouse model [68]. For the hydrogel (G:gelatin/T:tyramine/H:heprin) preparation, gelatin (G) was reacted first with tyramine (T) to provide enzymatic crosslinking points and then with heparin (H) to provide the binding domains to VEGF. In the in vitro studies, the authors observed sustained release of VEGF from the G/T/H gel with high bioactivity for 3 weeks. In the in vivo studies, significant increase of blood vessel density in 2 weeks post-injection of VEGF loaded G/T/H gel at the wound area indicated enhanced angiogenesis by the release of VEGF compared to the controls.
Gelatin hydrogel has been also used to study the synergistic effect of multiple growth factor delivery on angiogenesis. For instance, Liu et al. incorporated bFGF and brain-derived neurotrophic factor (BDNF) in a gelatin-based hydrogel to study the simultaneous effect of both factors on angiogenesis in an ischemic myocardium [69]. Upon formation of higher vessel density and higher left ventricular ejection fraction (LVEF) in the hydrogel embedded with bFGF + BDNF as compared to only bFGF, the authors claimed that the former system might become a promising therapeutic strategy for the treatment of ischemic myocardium.
In other studies, gelatin hydrogel has been used as a carrier for cell therapy, along with controlling the delivery of growth factor. For instance, Takehara et al. studied whether the release of bFGF from a gelatin hydrogel could improve human cardiosphere-derived cell (hCDC) therapy in a chronic MI pig model [70]. In one their experimental setting, the authors injected gelatin hydrogel incorporated with or without bFGF. In other experiments, bFGF- gelatin hydrogel with or without hCDC was injected. Neoangiogenesis by increasing arteriolar density was observed in the ischemic myocardium resulting in improved cardiac function. Their findings also revealed significant retention of transplanted hCDCs in the ischemic area, improving the infarct size, when combined with bFGF-loaded hydrogel as compared to hCDC injection alone. In another study by Nakajima et al., gelatin hydrogel was used for transplanting cardiomyocytes (CM) in an infarcted rat myocardium to assess improvement in cardiac function [71]. In this study, rat CM were transplanted with gelatin hydrogel to infarcted hearts and compared with sham operated rats, CM in PBS, only PBS, and only hydrogel transplanted groups. After three weeks of transplantation, pathological analysis showed that in the CM loaded hydrogel group, the cells were efficiently engrafted with the host and angiogenesis was significantly increased in the infarcted area. Also, according to quantitative RT-PCR analysis, significant increase of angiogenic cytokines, such as bFGF, VEGF, and hepatocyte growth factor (HGF), were observed in CM loaded hydrogel group compared to the other experimental groups.
To increase its cross-linking sites, make it more stable at the body temperature and reduce its degradation rate, gelatin has been chemically functionalized with several cross-linkable substrates like hydroxyphenyl propionic acid to produce Gelatin-Hydroxyphenyl Propionic Acid (GHPA) [72] or with unsaturated methacrylate groups to produce gelatin methacrylate (GelMA) [73]. GHPA undergoes in-situ oxidative crosslinking while GelMA undergoes photo-initiated polymerization forming a suitable injectable hydrogel for growth factor or gene delivery as well as cell-based therapy. Lee et al. used mesenchymal stem cell (MSC) loaded GHPA for endothelial differentiation of MSCs and tubule formation in vivo [72]. Extensive neovascularization was observed in two weeks post-injection. In another study, Lai et al. modified a GelMA hydrogel with carboxybetaine methacrylate (CBMA) (i.e. GelMA/CBMA hydrogel) with better mechanical properties, lower degradation rate, and controlled drug release rate in comparison to only GelMA group to promote vascular formation [74]. These properties of GelMA/CBMA hydrogels were tunable by varying the ratio of CBMA. In an in vivo mice model, angiogenesis was observed in VEGF loaded GelMA/CBMA hydrogel. The authors claimed that these properties make the GelMA/CBMA hydrogel a promising material for drug delivery, vascularization and tissue regeneration. In a recent study, Paul et al. used GelMA-graphene oxide hydrogel for angiogenic gene delivery and to promote vasculogenesis and cardiac repair [75]. Graphene oxide and VEGF loaded GelMA hydrogel were injected in a rat MI model. Significant increase in capillary density confirmed vasculogenesis in the infarct region, resulting in improved cardiac function.
2.1.5. Fibrin
Fibrin is a water-soluble fibrous glycoprotein present as a major component in blood clots. Clinical-grade fibrin is obtained by processing blood plasma. Fibrin gel is known to have angiogenic effect, due to its molecular properties [76]. Therefore it has been used as a biodegradable, injectable scaffold for promoting angiogenesis/vasculogenesis in tissue engineering [77].
Christman performed the pioneer work on the use of fibrin gel for cardiac regeneration [78,79]. In an early study, they restored cardiac function in an ischemic rat myocardium by injecting “fibrin glue” with or without skeletal myoblast (SM) [78]. The “fibrin glue” is a fibrin hydrogel which is the mixture of two components, (1) concentrated fibrinogen and aprotinin and (2) thrombin and CaCl2. The authors proposed that a reduction of infarcted myocardium could be induced by neovascularization following injection of fibrin glue, both with or without SM. Later, they studied the survival of SM in the fibrin glue in vitro as well as using an ischemic rat myocardium model in vivo [79]. Cell survival was determined by measuring infracted area, covered by cells. Five weeks after injection, SM loaded fibrin glue was found to cover the infracted area to a significantly higher extent than the control groups including BSA and myoblast loaded BSA. The authors suggested that the increase of cell survival in fibrin glue was due to its function as a temporary extracellular matrix for the transplanted cells. Because of the greater biocompatibility, fibrin glue also induced neovascularization in the infarct region by significant increase of the arteriole density in comparison with the control groups. A comparative study on the therapeutic effects of acellular fibrin and alginate gels was also performed in a rodent model of chronic ischemic cardiomyopathy by Yu et al. [80]. The authors observed improvements in cardiac function by reducing infarct scar percentage and neovascularization with injection of both fibrin and alginate gel compared to the injection of PBS, claiming these gels as potentially effective injectable biopolymers for myocardial repair.
Numerous attempts have been also undertaken for healing irregular bone defects using fibrin-based gels. However, in most cases complete regeneration has not possible due to a lack of vascularization [81]. As fibrin gel is known to have angiogenic property, large quantities of fibrin are required for the use as a scaffolding biomaterial for bone healing, which is not cost effective. Recently, two research groups tried to overcome this problem by introducing fibrin nanoparticle in chitin-based injectable hydrogel [82,83]. Fibrin nanoparticles were prepared using a modified water-in-oil emulsification-diffusion method in absence of any surfactants. Both group observed a significant increase in neovascularization of the bone-defect area in presence of fibrin nanoparticle containing hydrogel as compared to the control groups.
Fibrin gel has also been used to deliver growth factors for vascular formation or transplant cells in clinical applications. However, low binding affinity between fibrin and growth factors as well as fast degradation of the hydrogel often leads to rapid release of growth factors. In this regard, several attempts have been taken to address controlled delivery of growth factors from fibrin gel. For instance, Jeon et al. hypothesized that the rate of bFGF release from fibrin gels can be controlled with the use of heparin and varying concentrations of fibrinogen and thrombin [84]. They observed that bFGF release rate decreased upon addition of heparin and with increased concentrations of both fibrinogen and thrombin. Significant increase of in vitro dermal fibroblast growth in culture containing bFGF-loaded media compared to normal media indicated the bioactivity of bFGF. Therapeutic capacity of the bFGF delivery system was studied by in vivo experiments, where bFGF-loaded fibrin gels were injected into mice ischemic limbs. Four weeks post injection, quantification of capillary density and capillary ratio per muscle fiber, in the ischemic sites, indicated enhanced neovascularization by the injection of bFGF-loaded fibrin gels as compared to the control receiving no treatment.
Zisch et al. introduced an injectable “fibrin glue” by creating mutant α2-PI1-8 –VEGF121 fusion protein (to control the release of VEGF) and incorporating it into fibrin hydrogel to promote its angiogenic activity [85]. Effect of VEGF on EC growth was studied by seeding HUVECs on α2-PI1-8–VEGF121 modified fibrin hydrogel. Increased percent of cell-growth was observed up to day four of culture in the presence of VEGF modified fibrin gel as compared to control non-modified fibrin gel. The authors claimed that the incorporation of increasing amounts of α2-PI1-8–VEGF121 in fibrin hydrogel resulted in dose-dependent enhancement of EC growth that could be applied into an ischemic region to provide angiogenic activity. A few years later, in a similar work, Sacchi et al. developed a less degradable modified fibrin hydrogel to control the dose of VEGF, that is delivered to the tissue, for inducing stable and functional angiogenesis [86]. For controlling the release of VEGF from the hydrogel, murine VEGF164 was fused with α2-plasmin inhibitor (α2-PI1–8) to form α2-PI1–8-VEGF164 and then crosslinked with fibrin. In addition, Aprotinin-α2-PI1–8 was synthesized and incorporated in the gel to control the degradation rate. Intramuscular injection of the hydrogel (combination of Fibrin- α2-PI1–8- VEGF164 and Aprotinin-α2-PI1–8) in a mice model provided stable and functional angiogenesis for four weeks, as indicated by significant increase in the vessel length density due to the controlled release of VEGF.
2.2. Synthetic injectable hydrogels for neovascularization
2.2.1. N-isopropylacrylamide copolymer
N-isopropylacrylamide copolymer (PNIPAAm)-based hydrogels are injectable at room temperature but they solidify in the body due to the increase in the temperature. These gels can efficiently be designed for cellular delivery and promoting cell attachment, spreading and within the target tissue [87]. However, non-resorbability of NIPAAm copolymer limits its application in short term/transient applications due to potential chronic inflammatory response in the body. To address this problem, several groups have made NIPAAm copolymers biodegradable by incorporating biodegradable groups in the polymer [88].
Garbern et al. developed a pH- and temperature-responsive NIPAAm-based hydrogel with a synthetic random copolymer of poly (N-isopropylacrylamide-co-propyl acrylic acid-co-butyl acrylate) (p [NIPAAm-co-PAA-co-BA]), for therapeutic angiogenesis [89]. The developed P(NIPAAm-co-PAA-co-BA) formed gel at pH 6.8 at 37 °C while remained as a solution at pH 7.4 at the same temperature. When the copolymer solution was injected with bFGF in the rat ischemic myocardium, it formed gel in the acidic environment of the ischemic area. Polymer plus bFGF treatment led to 30–40% increase of capillary densities resulting in a 2-fold improvement in relative blood flow toward the infarct region, compared to saline plus bFGF or polymer-only controls in a twenty eight days post injection period (Fig. 2 iv, v and vi). The authors suggested that the improvement of angiogenesis was due to the sustained, local delivery of bFGF. In another study, Fujimoto et al. synthesized a thermo-responsive and biodegradable NIPAAm copolymer hydrogel for repair and healing of chronic infarcted myocardium in a rat model [90]. NIPAAm was modified with poly (trimethylene carbonate) (PTMC) to lower the hydrolysis rate of the injected hydrogel in vivo. Upon eight weeks of injection, considerable recovery of cardiac function took place following enhanced angiogenesis as compared to the control saline injection.
2.2.2. PEG
PEG is a widely used synthetic biomaterial in biomedicine due to its extremely low cytotoxicity and immunogenicity [23]. PEG-based hydrogels are formed by covalent crosslinking between its chains and provide several advantages for regenerating various types of tissues such as bone and blood vessels [16]. Although PEG-based gels are widely used in engineering of patches or tissue constructs, a few research groups have developed injectable PEG based hydrogel for therapeutic angiogenesis. Phelps et al. engineered PEG-based synthetic hydrogel containing protease-degradable sites, cell-adhesion motifs (RGD: arginine-glycine-aspartic acid), and VEGF growth factor for neovascularization [91]. In a mouse model of hind-limb ischemia, significant increase of vessel density was observed at 4 weeks of hydrogel injection as compared to the injection of only VEGF due to the sustained cell-demanded release of VEGF. The lower degradation rate of the hydrogel led to slow release of VEGF, as VEGF release took place during the degradation of the hydrogel. Zachman et al. developed a PEG-based injectable hydrogel that enabled controlled, dual delivery of proangiogenic C16 and anti-inflammatory Ac-SDKP peptides in the mouse model of peripheral artery disease (PAD) [92]. The combined injection of C16 and Ac-SDKP peptides promoted angiogenesis, muscle regeneration and minimized detrimental inflammation by regulating TNF-α pathways separately from MMP-9 mediated pathways of angiogenesis. Rufaihah et al. took a different attempt to achieve controlled release of VEGF [93]. They developed an injectable PEGylated fibrin hydrogel, which could store and sustain release of VEGF. The hydrogel was formed by covalent linkage between fibrinogen and PEG diacrylate. In an in vivo study, the hydrogels were injected in a MI model, where significant increase of arteriole density in infarct and peri-infarct regions indicated neovascularization, through sustained release of VEGF from the loaded fibrin gel. Leslie-Barbick et al. developed a PEG-based hydrogel, covalently linked with QK peptide, a VEGF memetic peptide, (Sequence: Ac-KLTWQELYQLKYKGI-amide) that is known to promote angiogenesis [94]. In an in vivo study, the authors incorporated releasable VEGF alone and in combination with PEG-VEGF or PEG-QK hydrogel which were implanted into the mouse cornea micropocket. Fourteen days after implantation, PEG-QK hydrogel showed enhanced angiogenesis by increasing vessel density and branch points as well as space filling of the cornea micropocket. In another study, Salimath et al. developed a PEG-based hydrogel having protease-degradable crosslinker, which underwent collagenase degradation [95]. In an in vivo study in a rat MI model, the hydrogel, incorporated with either hepatocyte growth factor (HGF) or VEGF or both, was delivered to the infarcted myocardium. Significant increase in angiogenesis, stem cell recruitment, and decrease in fibrosis were observed in the dual growth factor delivery group compared with single growth factor therapy. In a recent study by Bhutani et al., PEG-based hydrogel presenting ECM derived adhesion peptides (RGD and GFOGER -a collagen mimicking peptide) and control scrambled non-adhesive peptide (RDG) were prepared and their effects on behavior of cardiac progenitor cells (CPCs) in vitro as well as cardiac repair in rats undergoing ischemia reperfusion were monitored [96]. GFOGER gels induce differentiation of CPCs toward CMs and lowered the levels of reparative secretive factors. In contrast to expectations, in the in vivo study, improved cardiac function was observed only with the non-adhesive RDG gels co-delivered with CPCs. However, ECM-derived adhesive peptide-presenting gels failed to show the recovery of cardiac function. Increased angiogenesis was observed for both RGD and RDG gels and less for GFOGER gel. Berdichevski et al. performed an interesting comparative in vivo study of biodegradation and angiogenic response with three types of VEGF bearing PEG-fibrinogen hydrogel configurations in a subcutaneous rat implantation model [97]. The three types of implants were made of identical amounts of precursors namely, cylindrical plugs, injectable spherical microbeads and in situ polymerized injectable hydrogels. According to the MRI data, the degradation time of in situ polymerized hydrogel was lowest and cylindrical plug was highest. Significant increase of vascularization (16-fold more capillaries) was resulted by the in vivo VEGF release from the microbeads in comparison with controls. Based on these data, the authors claimed that implantation strategies could have significant effect on neovascularization triggered by localized growth factor delivery.
2.2.3. Poly(Latic-co-glycolic acid)
Poly (Latic-co-glycolic Acid) (PLGA) is a frequently used biodegradable synthetic polymers, utilized as a 3D scaffolding biomaterial, for tissue regeneration and repair. PLGA is a copolymer of two different monomers, glycolic acid and lactic acid. PLGA is one of the usual choices in the fabrication of several FDA approved biomedical devices, such as, grafts, sutures, implants, prosthetic devices, surgical sealant films, micro and nanoparticles. PLGA microspheres have been successfully used for gradual delivery of cells or drugs in experimental stroke models [98]. Injectable PLGA nanospheres/microspheres have been developed for prolonged neovascularization in ischemic models. For instance, Jeona et al. aimed to achieve enhanced angiogenic activity by prolonged release of bFGF from an injectable fibrin gel using PLGA nanospheres. A novel heparin conjugated PLGA nanospheres (HCPNs) was fabricated by reacting aminated PLGA with heparin via EDC/NHS chemistry. bFGF was then entrapped in HCPNs and subsequently was suspended in the fibrin gel. The authors observed prolonged release of bFGF from HCPN loaded fibrin gel as compared to blank fibrin. Significant increase of capillary formation, in an ischemic mouse model, after 4 weeks of injection with HCPN loaded fibrin gel indicated enhanced angiogenic activity due to the controlled release of bFGF [99].
2.2.4. Synthetic peptides
A number of growth factor mimetic peptides have also been developed for induction of angiogenesis through cellular signaling. For instance, VEGF mimetic peptides promote angiogenesis by prolonged stimuli presentation and residence time in situ. Previous works have focused on the development of injectable hydrogel by immobilizing these peptides via covalent bonding in the hydrogel scaffolds [41,100]. Controlled release of peptide will take place during the degradation of the hydrogel. For instance, Feng et al. synthesized a chitosan-based hydrogel by immobilizing the C domain peptide of insulin-like growth factor-1 (IGF-1C) for a successful stem cell therapy in acute kidney injury (AKI) [100]. In vitro studies indicated increased cell viability in chitosan-IGF-1C hydrogel compared to blank chitosan hydrogel. In vivo implantation of the chitosan–IGF-1C hydrogel and ADSCs in ischemic kidneys resulted in enhanced stem cell survival and angiogenesis. The authors claimed that IGF-1C immobilized chitosan hydrogel provides a promising therapeutic approach for AKI. In another study, Kumar et al. synthesized a VEGF memetic peptide [SLanc: K-(SL)3 (RG) (SL)3-K-G-KLTWQE-LYQLKYKGI] and a non-angiogenic mimic peptide [SLc: K2-(SL)3 (RG) (SL)3-K2] to study neovascularization [101]. These peptides could form self-assembled thixotropic, injectable and biodegradable hydrogels, which were injected subcutaneously in a rat model to study angiogenesis. In the case of SLanc peptide, increased vascularization was observed within 7 days of injection as compared to SLc peptide. The authors postulated that the vascularization was promoted due to the easy diffusion of VEGF mimetic peptide from the non-fibrous gel made of SLanc peptide by either simple equilibrium or subsequent proteolysis of the MMP-2 cleavage sites of the peptide (Fig. 2 vii). In another study, the same hydrogel was injected in the hind limb ischemia of mouse [102]. The synthetic peptide-based hydrogel scaffold promoted angiogenesis and recovery of ischemic tissue. Bio-distribution studies indicated that the hydrogel could be injected safely intramuscularly, subcutaneously, or intravenously. Histology of muscle tissue from SLanc-treated mice on day twenty eight demonstrated the formation of mature blood vessels in the injection site and preservation of tissue structure and function [102].
3. Conclusion
The use of injectable hydrogel provides a promising therapeutic pathway to promote neovascularization in ischemic tissues and organs. Injectable hydrogels provide an extensive network structure from which trapped angiogenic growth factors release in a slow and sustained manner and subsequently results in the formation and maturation of blood vessels. In cell-based therapies, injectable hydrogels provide an ECM like microenvironment to enhance cellular retention, survival, proliferation and neovascularization. The synthesis of suitable injectable hydrogels, with respect to their mechanical stability and biodegradability, can be a challenging task for efficient neovascularization. Natural polymers are biodegradable but they have poor mechanical stability upon injection, while synthetic polymers have tunable mechanical property but their biodegradation rates are generally very low. Recent attempts have focused on the use of composite or hybrid hydrogels made of natural and artificial precursors to address these limitations. The use of synthetic polymer-based micro/nanoparticals is also another promising candidate for neovascularization due to their moderate degradability and mechanical stability. We believe that polymer-based micro/nanoparticals and new biohybrid injectable hydrogels will significantly impact the field of controlled drug delivery and cell therapeutics. Extensive research continues to be needed on the design and development of growth factor mimetic synthetic peptide-based hydrogels. After successful neovascularization in animal models, future work will be needed to demonstrat the efficacy of injectable materials for therapeutic angiogenesis in primates and humans.
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
Contributor Information
Brent L. Vernon, Email: Brent.Vernon@asu.edu.
Mehdi Nikkhah, Email: mehdi.nikkhah@asu.edu.
References
- 1.Xuetao S., Sara S.N. Overview of hydrogel-based strategies for application in cardiac tissue regeneration. Biomed. Mater. 2015;10(3):034005. doi: 10.1088/1748-6041/10/3/034005. [DOI] [PubMed] [Google Scholar]
- 2.Sgambato A., Cipolla L., Russo L. Bioresponsive hydrogels: chemical strategies and perspectives in tissue engineering. Gels. 2016;2(4):28. doi: 10.3390/gels2040028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vicki Cheng B.H.L., Pauken Christine, Vernon Brent L. Poly(N-isopropylacrylamide-co-poly(ethylene glycol))-acrylate simultaneously physically and chemically gelling polymer systems. J. Appl. Polym. Sci. 2007;106(2):1201–1207. [Google Scholar]
- 4.Lee B.H., West B., McLemore R., Pauken C., Vernon B.L. In-situ injectable physically and chemically gelling NIPAAm-based copolymer system for embolization. Biomacromolecules. 2006;7(6):2059–2064. doi: 10.1021/bm060211h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robb S.A., Lee B.H., McLemore R., Vernon B.L. Simultaneously physically and chemically gelling polymer system utilizing a poly(NIPAAm-co-cysteamine)-based copolymer. Biomacromolecules. 2007;8(7):2294–2300. doi: 10.1021/bm070267r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ifkovits J.L., Tous E., Minakawa M., Morita M., Robb J.D., Koomalsingh K.J., Gorman J.H., Gorman R.C., Burdick J.A. Injectable hydrogel properties influence infarct expansion and extent of postinfarction left ventricular remodeling in an ovine model. Proc. Natl. Acad. Sci. U.S.A. 2010;107(25):11507–11512. doi: 10.1073/pnas.1004097107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu M., Zeng X., Ma C., Yi H., Ali Z., Mou X., Li S., Deng Y., He N. Injectable hydrogels for cartilage and bone tissue engineering. Bone Research. 2017;5:17014. doi: 10.1038/boneres.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang H., Heilshorn S.C. Adaptable hydrogel networks with reversible linkages for tissue engineering. Adv. Mater. (Weinheim, Ger.) 2015;27(25):3717–3736. doi: 10.1002/adma.201501558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patenaude M., Campbell S., Kinio D., Hoare T. Tuning gelation time and morphology of injectable hydrogels using ketone–hydrazide cross-linking. Biomacromolecules. 2014;15(3):781–790. doi: 10.1021/bm401615d. [DOI] [PubMed] [Google Scholar]
- 10.Erkeçoğlu S., Sezer A.D., Bucak S. Smart delivery systems with shape memory and self-folding polymers. In: Sezer A.D., editor. Smart Drug Delivery System. InTech; Rijeka: 2016. p. Ch. 01. [Google Scholar]
- 11.del Valle L., Díaz A., Puiggalí J. Hydrogels for biomedical applications: cellulose, chitosan, and protein/peptide derivatives. Gels. 2017;3(3):27. doi: 10.3390/gels3030027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bencherif S.A., Sands R.W., Bhatta D., Arany P., Verbeke C.S., Edwards D.A., Mooney D.J. Injectable preformed scaffolds with shape-memory properties. Proc. Natl. Acad. Sci. U.S.A. 2012;109(48):19590–19595. doi: 10.1073/pnas.1211516109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montgomery M., Ahadian S., Davenport Huyer L., Lo Rito M., Civitarese R.A., Vanderlaan R.D., Wu J., Reis L.A., Momen A., Akbari S., Pahnke A., Li R.-K., Caldarone C.A., Radisic M. Flexible shape-memory scaffold for minimally invasive delivery of functional tissues. Nat. Mater. 2017;16:1038–1046. doi: 10.1038/nmat4956. [DOI] [PubMed] [Google Scholar]
- 14.Xie M., Wang L., Ge J., Guo B., Ma P.X. Strong electroactive biodegradable shape memory polymer networks based on star-shaped polylactide and aniline trimer for bone tissue engineering. ACS Appl. Mater. Interfaces. 2015;7(12):6772–6781. doi: 10.1021/acsami.5b00191. [DOI] [PubMed] [Google Scholar]
- 15.Haines-Butterick L., Rajagopal K., Branco M., Salick D., Rughani R., Pilarz M., Lamm M.S., Pochan D.J., Schneider J.P. Controlling hydrogelation kinetics by peptide design for three-dimensional encapsulation and injectable delivery of cells. Proc. Natl. Acad. Sci. U. S. A. 2007;104(19):7791–7796. doi: 10.1073/pnas.0701980104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan C., Pochan D.J. Rheological properties of peptide-based hydrogels for biomedical and other applications. Chem. Soc. Rev. 2010;39(9):3528–3540. doi: 10.1039/b919449p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts M.T., Mohraz A., Christensen K.T., Lewis J.A. Direct flow visualization of colloidal gels in microfluidic channels. Langmuir. 2007;23(17):8726–8731. doi: 10.1021/la700562m. [DOI] [PubMed] [Google Scholar]
- 18.Rueb C.J., Zukoski C.F. Viscoelastic properties of colloidal gels. J. Rheol. 1997;41(2):197–218. [Google Scholar]
- 19.Wang Q., Wang L., Detamore M.S., Berkland C. Biodegradable colloidal gels as moldable tissue engineering scaffolds. Adv. Mater. 2008;20(2):236–239. [Google Scholar]
- 20.Vernon B. Elsevier Science; 2011. Injectable Biomaterials: Science and Applications. [Google Scholar]
- 21.Tous E., Purcell B., Ifkovits J.L., Burdick J.A. Injectable acellular hydrogels for cardiac repair. Journal of Cardiovascular Translational Research. 2011;4(5):528–542. doi: 10.1007/s12265-011-9291-1. [DOI] [PubMed] [Google Scholar]
- 22.Li X., Tamama K., Xie X., Guan J. Improving cell engraftment in cardiac stem cell therapy. Stem Cell. Int. 2016;2016:1–11. doi: 10.1155/2016/7168797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chu H., Wang Y. Therapeutic angiogenesis: controlled delivery of angiogenic factors. Ther. Deliv. 2012;3(6):693–714. doi: 10.4155/tde.12.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagarkar R.P., Hule R.A., Pochan D.J., Schneider J.P. De novo design of strand-swapped β-hairpin hydrogels. J. Am. Chem. Soc. 2008;130(13):4466–4474. doi: 10.1021/ja710295t. [DOI] [PubMed] [Google Scholar]
- 25.Delcroix G.J.R., Schiller P.C., Benoit J.-P., Montero-Menei C.N. Adult cell therapy for brain neuronal damages and the role of tissue engineering. Biomaterials. 2010;31(8):2105–2120. doi: 10.1016/j.biomaterials.2009.11.084. [DOI] [PubMed] [Google Scholar]
- 26.Nooeaid P., Salih V., Beier J.P., Boccaccini A.R. Osteochondral tissue engineering: scaffolds, stem cells and applications. J. Cell Mol. Med. 2012;16(10):2247–2270. doi: 10.1111/j.1582-4934.2012.01571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pakulska M.M., Ballios B.G., Shoichet M.S. Injectable hydrogels for central nervous system therapy. Biomed. Mater. 2012;7(2):024101. doi: 10.1088/1748-6041/7/2/024101. [DOI] [PubMed] [Google Scholar]
- 28.Hasan A., Khattab A., Islam M.A., Hweij K.A., Zeitouny J., Waters R., Sayegh M., Hossain M.M., Paul A. Injectable hydrogels for cardiac tissue repair after myocardial infarction. Advanced Science. 2015;2(11):1500122. doi: 10.1002/advs.201500122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Croisier F., Jérôme C. Chitosan-based biomaterials for tissue engineering. Eur. Polym. J. 2013;49(4):780–792. [Google Scholar]
- 30.Upadhyaya L., Singh J., Agarwal V., Tewari R.P. The implications of recent advances in carboxymethyl chitosan based targeted drug delivery and tissue engineering applications. J. Contr. Release. 2014;186(Supplement C):54–87. doi: 10.1016/j.jconrel.2014.04.043. [DOI] [PubMed] [Google Scholar]
- 31.Dragostin O.M., Samal S.K., Dash M., Lupascu F., Pânzariu A., Tuchilus C., Ghetu N., Danciu M., Dubruel P., Pieptu D., Vasile C., Tatia R., Profire L. New antimicrobial chitosan derivatives for wound dressing applications. Carbohydr. Polym. 2016;141(Supplement C):28–40. doi: 10.1016/j.carbpol.2015.12.078. [DOI] [PubMed] [Google Scholar]
- 32.Saurabh A.K.H.P.S.C.K., Nurul Fazita A.A.S.M.R., Syakir M.I., Davoudpour Y., Rafatullah M., Abdullah C.K., Haafiz M.K.M., Dungani R. A review on chitosan-cellulose blends and nanocellulose reinforced chitosan biocomposites: properties and their applications. Carbohydr. Polym. 2016;150(Supplement C):216–226. doi: 10.1016/j.carbpol.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 33.Jayakumar R., Prabaharan M., Nair S.V., Tamura H. Novel chitin and chitosan nanofibers in biomedical applications. Biotechnol. Adv. 2010;28(1):142–150. doi: 10.1016/j.biotechadv.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Deng Y., Ren J., Chen G., Li G., Wu X., Wang G., Gu G., Li J. Injectable in situ cross-linking chitosan-hyaluronic acid based hydrogels for abdominal tissue regeneration. Sci. Rep. 2017;7:2699. doi: 10.1038/s41598-017-02962-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fujita M., Ishihara M., Simizu M., Obara K., Ishizuka T., Saito Y., Yura H., Morimoto Y., Takase B., Matsui T., Kikuchi M., Maehara T. Vascularization in vivo caused by the controlled release of fibroblast growth factor-2 from an injectable chitosan/non-anticoagulant heparin hydrogel. Biomaterials. 2004;25(4):699–706. doi: 10.1016/s0142-9612(03)00557-x. [DOI] [PubMed] [Google Scholar]
- 36.Deng C., Zhang P., Vulesevic B., Kuraitis D., Li F., Yang A.F., Griffith M., Ruel M., Suuronen E.J. A collagen-chitosan hydrogel for endothelial differentiation and angiogenesis. Tissue Eng. 2010;16(10):3099–3109. doi: 10.1089/ten.tea.2009.0504. [DOI] [PubMed] [Google Scholar]
- 37.Hsieh F.-Y., Tao L., Wei Y., Hsu S.-h. A novel biodegradable self-healing hydrogel to induce blood capillary formation. NPG Asia Mater. 2017;9 e363. [Google Scholar]
- 38.Wen-Ning Lu S.-H.L., Wang Hai-Bin, Li De-Xue, Duan Cui-Mi, Liu Zhi-Qiang, Hao Tong, He Wen-Jun, Xu Bin, Fu Ying Qiang, Song C., Xie Xiao-Hua, Wang Chang-Yong. Functional improvement of infarcted heart by Co-Injection of embryonic stem cells with temperature-responsive chitosan hydrogel. Tissue Eng. 2008;15(6):1437–1447. doi: 10.1089/ten.tea.2008.0143. [DOI] [PubMed] [Google Scholar]
- 39.Wang H., Zhang X., Li Y., Ma Y., Zhang Y., Liu Z., Zhou J., Lin Q., Wang Y., Duan C., Wang C. Improved myocardial performance in infarcted rat heart by co-injection of basic fibroblast growth factor with temperature-responsive Chitosan hydrogel. J. Heart Lung Transplant. 2010;29(8):881–887. doi: 10.1016/j.healun.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 40.Liu Z., Wang H., Wang Y., Lin Q., Yao A., Cao F., Li D., Zhou J., Duan C., Du Z., Wang Y., Wang C. The influence of chitosan hydrogel on stem cell engraftment, survival and homing in the ischemic myocardial microenvironment. Biomaterials. 2012;33(11):3093–3106. doi: 10.1016/j.biomaterials.2011.12.044. [DOI] [PubMed] [Google Scholar]
- 41.Shu Y., Hao T., Yao F., Qian Y., Wang Y., Yang B., Li J., Wang C. RoY peptide-modified chitosan-based hydrogel to improve angiogenesis and cardiac repair under hypoxia. ACS Appl. Mater. Interfaces. 2015;7(12):6505–6517. doi: 10.1021/acsami.5b01234. [DOI] [PubMed] [Google Scholar]
- 42.Fraser J.R.E., Laurent T.C., Laurent U.B.G. Hyaluronan: its nature, distribution, functions and turnover. J. Intern. Med. 1997;242(1):27–33. doi: 10.1046/j.1365-2796.1997.00170.x. [DOI] [PubMed] [Google Scholar]
- 43.Moshayedi P., Carmichael S.T. Hyaluronan, neural stem cells and tissue reconstruction after acute ischemic stroke. Biomatter. 2013;3(1) doi: 10.4161/biom.23863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khunmanee S., Jeong Y., Park H. Crosslinking method of hyaluronic-based hydrogel for biomedical applications. J. Tissue Eng. 2017;8:1–16. doi: 10.1177/2041731417726464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gaffey A.C., Chen M.H., Venkataraman C.M., Trubelja A., Rodell C.B., Dinh P.V., Hung G., MacArthur J.W., Soopan R.V., Burdick J.A., Atluri P. Injectable shear-thinning hydrogels to deliver endothelial progenitor cells, enhance cell engraftment, and improve ischemic myocardium. J. Thorac. Cardiovasc. Surg. 2015;150(5):1268–1277. doi: 10.1016/j.jtcvs.2015.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.MacArthur J.W., Purcell B.P., Shudo Y., Cohen J.E., Fairman A., Trubelja A., Patel J., Hsiao P., Yang E., Lloyd K., Hiesinger W., Atluri P., Burdick J.A., Woo Y.J. Sustained release of engineered stromal cell–derived factor 1-α from injectable hydrogels effectively recruits endothelial progenitor cells and preserves ventricular function after myocardial infarction. Circulation. 2013;128(11 0 1):S79–S86. doi: 10.1161/CIRCULATIONAHA.112.000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.C.Q. Junzi Jiang, Gao H, Wen Zhong, Feng Lu, Malcolm Xing, Injectable ADEP Hyaluronic Acid-chitosan Hydrogels Based on Schiff Base Enhance Angiogenesis, Cell Proliferation and Promote Skin Regeneration.
- 48.Chang Q., Gao H., Bu S., Zhong W., Lu F., Xing M. An injectable aldehyded 1-amino-3,3-diethoxy-propane hyaluronic acid–chitosan hydrogel as a Carrier of adipose derived stem cells to enhance angiogenesis and promote skin regeneration. J. Mater. Chem. B. 2015;3(22):4503–4513. doi: 10.1039/c5tb00027k. [DOI] [PubMed] [Google Scholar]
- 49.Park H.-J., Jin Y., Shin J., Yang K., Lee C., Yang H.S., Cho S.-W. Catechol-functionalized hyaluronic acid hydrogels enhance angiogenesis and osteogenesis of human adipose-derived stem cells in critical tissue defects. Biomacromolecules. 2016;17(6):1939–1948. doi: 10.1021/acs.biomac.5b01670. [DOI] [PubMed] [Google Scholar]
- 50.Yoon S.J., Fang Y.H., Lim C.H., Kim B.S., Son H.S., Park Y., Sun K. Regeneration of ischemic heart using hyaluronic acid-based injectable hydrogel. J. Biomed. Mater. Res. B Appl. Biomater. 2009;91B(1):163–171. doi: 10.1002/jbm.b.31386. [DOI] [PubMed] [Google Scholar]
- 51.Cai S., Liu Y., Zheng Shu X., Prestwich G.D. Injectable glycosaminoglycan hydrogels for controlled release of human basic fibroblast growth factor. Biomaterials. 2005;26(30):6054–6067. doi: 10.1016/j.biomaterials.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 52.Dai W., Wold L.E., Dow J.S., Kloner R.A. Thickening of the infarcted wall by collagen injection improves left ventricular function in rats: a novel approach to preserve cardiac function after myocardial infarction. J. Am. Coll. Cardiol. 2005;46(4):714–719. doi: 10.1016/j.jacc.2005.04.056. [DOI] [PubMed] [Google Scholar]
- 53.J.Y. Ngan F. Huang, Richard Sievers, Song Li, and Randall J. Lee, Injectable biopolymers enhance angiogenesis after myocardial infarction, Tissue Eng. 11(11–12) 1860-1866. [DOI] [PubMed]
- 54.McBane J.E., Vulesevic B., Padavan D.T., McEwan K.A., Korbutt G.S., Suuronen E.J. Evaluation of a collagen-chitosan hydrogel for potential use as a pro-angiogenic site for islet transplantation. PLoS One. 2013;8(10) doi: 10.1371/journal.pone.0077538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suuronen E.J., Veinot J.P., Wong S., Kapila V., Price J., Griffith M., Mesana T.G., Ruel M. Tissue-engineered injectable collagen-based matrices for improved cell delivery and vascularization of ischemic tissue using CD133+ progenitors expanded from the peripheral blood. Circulation. 2006;114(1 suppl) doi: 10.1161/CIRCULATIONAHA.105.001081. I-138-I-144. [DOI] [PubMed] [Google Scholar]
- 56.Dreesmann L., Ahlers M., Schlosshauer B. The pro-angiogenic characteristics of a cross-linked gelatin matrix. Biomaterials. 2007;28(36):5536–5543. doi: 10.1016/j.biomaterials.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 57.Moon J.J., Saik J.E., Poche R.A., Leslie-Barbick J.E., Lee S.-H., Smith A.A., Dickinson M.E., West J.L. Biomimetic hydrogels with pro-angiogenic properties. Biomaterials. 2010;31(14):3840–3847. doi: 10.1016/j.biomaterials.2010.01.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saini H., Navaei A., Van Putten A., Nikkhah M. 3D cardiac microtissues encapsulated with the Co-Culture of cardiomyocytes and cardiac fibroblasts. Advanced Healthcare Materials. 2015;4(13):1961–1971. doi: 10.1002/adhm.201500331. [DOI] [PubMed] [Google Scholar]
- 59.Navaei A., Truong D., Heffernan J., Cutts J., Brafman D., Sirianni R.W., Vernon B., Nikkhah M. PNIPAAm-based biohybrid injectable hydrogel for cardiac tissue engineering. Acta Biomater. 2016;32(Supplement C):10–23. doi: 10.1016/j.actbio.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 60.Peela N., Sam F.S., Christenson W., Truong D., Watson A.W., Mouneimne G., Ros R., Nikkhah M. A three dimensional micropatterned tumor model for breast cancer cell migration studies. Biomaterials. 2016;81:72–83. doi: 10.1016/j.biomaterials.2015.11.039. [DOI] [PubMed] [Google Scholar]
- 61.Navaei A., Saini H., Christenson W., Sullivan R.T., Ros R., Nikkhah M. Gold nanorod-incorporated gelatin-based conductive hydrogels for engineering cardiac tissue constructs. Acta Biomater. 2016;41(Supplement C):133–146. doi: 10.1016/j.actbio.2016.05.027. [DOI] [PubMed] [Google Scholar]
- 62.Aubin H., Nichol J.W., Hutson C.B., Bae H., Sieminski A.L., Cropek D.M., Akhyari P., Khademhosseini A. Directed 3D cell alignment and elongation in microengineered hydrogels. Biomaterials. 2010;31(27):6941–6951. doi: 10.1016/j.biomaterials.2010.05.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Navaei A., Moore N., Sullivan R.T., Truong D., Migrino R.Q., Nikkhah M. Electrically conductive hydrogel-based micro-topographies for the development of organized cardiac tissues. RSC Adv. 2017;7(6):3302–3312. [Google Scholar]
- 64.Nichol J.W., Koshy S., Bae H., Hwang C.M., Yamanlar S., Khademhosseini A. Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials. 2010;31(21):5536–5544. doi: 10.1016/j.biomaterials.2010.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nikkhah M., Eshak N., Zorlutuna P., Annabi N., Castello M., Kim K., Dolatshahi-Pirouz A., Edalat F., Bae H., Yang Y., Khademhosseini A. Directed endothelial cell morphogenesis in micropatterned gelatin methacrylate hydrogels. Biomaterials. 2012;33(35):9009–9018. doi: 10.1016/j.biomaterials.2012.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tabata Y., Ikada Y. Vascularization effect of basic fibroblast growth factor released from gelatin hydrogels with different biodegradabilities. Biomaterials. 1999;20(22):2169–2175. doi: 10.1016/s0142-9612(99)00121-0. [DOI] [PubMed] [Google Scholar]
- 67.Hosaka A., Koyama H., Kushibiki T., Tabata Y., Nishiyama N., Miyata T., Shigematsu H., Takato T., Nagawa H. Gelatin hydrogel microspheres enable pinpoint delivery of basic fibroblast growth factor for the development of functional collateral vessels. Circulation. 2004;110(21):3322–3328. doi: 10.1161/01.CIR.0000147779.17602.18. [DOI] [PubMed] [Google Scholar]
- 68.Li Z., Qu T., Ding C., Ma C., Sun H., Li S., Liu X. Injectable gelatin derivative hydrogels with sustained vascular endothelial growth factor release for induced angiogenesis. Acta Biomaterialia. 2015;13:88–100. doi: 10.1016/j.actbio.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu Y., Sun L., Huan Y., Zhao H., Deng J. Application of bFGF and BDNF to improve angiogenesis and cardiac function. J. Surg. Res. 2006;136(1):85–91. doi: 10.1016/j.jss.2006.04.034. [DOI] [PubMed] [Google Scholar]
- 70.Takehara N., Tsutsumi Y., Tateishi K., Ogata T., Tanaka H., Ueyama T., Takahashi T., Takamatsu T., Fukushima M., Komeda M., Yamagishi M., Yaku H., Tabata Y., Matsubara H., Oh H. Controlled delivery of basic fibroblast growth factor promotes human cardiosphere-derived cell engraftment to enhance cardiac repair for chronic myocardial infarction. J. Am. Coll. Cardiol. 2008;52(23):1858–1865. doi: 10.1016/j.jacc.2008.06.052. [DOI] [PubMed] [Google Scholar]
- 71.Nakajima K., Fujita J., Matsui M., Tohyama S., Tamura N., Kanazawa H., Seki T., Kishino Y., Hirano A., Okada M., Tabei R., Sano M., Goto S., Tabata Y., Fukuda K. Gelatin hydrogel enhances the engraftment of transplanted cardiomyocytes and angiogenesis to ameliorate cardiac function after myocardial infarction. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0133308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee S.H., Lee Y., Chun Y.W., Crowder S.W., Young P.P., Park K.D., Sung H.-J. Situ crosslinkable gelatin hydrogels for vasculogenic induction and delivery of mesenchymal stem cells. Adv. Funct. Mater. 2014;24(43):6771–6781. doi: 10.1002/adfm.201401110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Loessner D., Meinert C., Kaemmerer E., Martine L.C., Yue K., Levett P.A., Klein T.J., Melchels F.P.W., Khademhosseini A., Hutmacher D.W. Functionalization, preparation and use of cell-laden gelatin methacryloyl-based hydrogels as modular tissue culture platforms. Nat. Protoc. 2016;11(4):727–746. doi: 10.1038/nprot.2016.037. [DOI] [PubMed] [Google Scholar]
- 74.Lai T.C., Yu J., Tsai W.B. Gelatin methacrylate/carboxybetaine methacrylate hydrogels with tunable crosslinking for controlled drug release. J. Mater. Chem. B. 2016;4(13):2304–2313. doi: 10.1039/c5tb02518d. [DOI] [PubMed] [Google Scholar]
- 75.Paul A., Hasan A., Kindi H.A., Gaharwar A.K., Rao V.T.S., Nikkhah M., Shin S.R., Krafft D., Dokmeci M.R., Shum-Tim D., Khademhosseini A. Injectable graphene oxide/hydrogel-based angiogenic gene delivery system for vasculogenesis and cardiac repair. ACS Nano. 2014;8(8):8050–8062. doi: 10.1021/nn5020787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hall H., Baechi T., Hubbell J.A. Molecular properties of fibrin-based matrices for promotion of angiogenesis in vitro. Microvasc. Res. 2001;62(3):315–326. doi: 10.1006/mvre.2001.2348. [DOI] [PubMed] [Google Scholar]
- 77.Li Y., Meng H., Liu Y., Lee B.P. Fibrin gel as an injectable biodegradable scaffold and cell Carrier for tissue engineering. ScientificWorldJournal. 2015;2015:685690. doi: 10.1155/2015/685690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Karen H.H.F., Christman L., Sievers Richard E., Fang Qizhi, Lee Randall J. Fibrin glue alone and skeletal myoblasts in a fibrin scaffold preserve cardiac function after myocardial infarction. Tissue Eng. 2004;10(3–4):403–409. doi: 10.1089/107632704323061762. [DOI] [PubMed] [Google Scholar]
- 79.Christman K.L., Vardanian A.J., Fang Q., Sievers R.E., Fok H.H., Lee R.J. Injectable fibrin scaffold improves cell transplant survival, reduces infarct expansion, and induces neovasculature formation in ischemic myocardium. J. Am. Coll. Cardiol. 2004;44(3):654–660. doi: 10.1016/j.jacc.2004.04.040. [DOI] [PubMed] [Google Scholar]
- 80.Yu J., Christman K.L., Chin E., Sievers R.E., Saeed M., Lee R.J. Restoration of left ventricular geometry and improvement of left ventricular function in a rodent model of chronic ischemic cardiomyopathy. J. Thorac. Cardiovasc. Surg. 2009;137(1):180–187. doi: 10.1016/j.jtcvs.2008.08.036. [DOI] [PubMed] [Google Scholar]
- 81.Kanczler J.M., Oreffo R.O.C. Osteogenesis and angiogenesis: the potential for engineering bone. Eur. Cell. Mater. 2008;15:100–114. doi: 10.22203/ecm.v015a08. [DOI] [PubMed] [Google Scholar]
- 82.Vishnu Priya M., Sivshanmugam A., Boccaccini A.R., Goudouri O.M., Sun W., Hwang N., Deepthi S., Nair S.V., Jayakumar R. Injectable osteogenic and angiogenic nanocomposite hydrogels for irregular bone defects. Biomed. Mater. 2016;11(3):035017. doi: 10.1088/1748-6041/11/3/035017. [DOI] [PubMed] [Google Scholar]
- 83.Arun Kumar R., Sivashanmugam A., Deepthi S., Bumgardner J.D., Nair S.V., Jayakumar R. Nano-fibrin stabilized CaSO4 crystals incorporated injectable chitin composite hydrogel for enhanced angiogenesis & osteogenesis. Carbohydr. Polym. 2016;140(Supplement C):144–153. doi: 10.1016/j.carbpol.2015.11.074. [DOI] [PubMed] [Google Scholar]
- 84.Oju J., Soo Hyun R., Ji Hyung C., Kim B.-S. Control of basic fibroblast growth factor release from fibrin gel with heparin and concentrations of fibrinogen and thrombin. J. Contr. Release. 2005;105(3):249–259. doi: 10.1016/j.jconrel.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 85.Zisch A.H., Schenk U., Schense J.C., Sakiyama-Elbert S.E., Hubbell J.A. Covalently conjugated VEGF–fibrin matrices for endothelialization. J. Contr. Release. 2001;72(1):101–113. doi: 10.1016/s0168-3659(01)00266-8. [DOI] [PubMed] [Google Scholar]
- 86.Sacchi V., Mittermayr R., Hartinger J., Martino M.M., Lorentz K.M., Wolbank S., Hofmann A., Largo R.A., Marschall J.S., Groppa E., Gianni-Barrera R., Ehrbar M., Hubbell J.A., Redl H., Banfi A. Long-lasting fibrin matrices ensure stable and functional angiogenesis by highly tunable, sustained delivery of recombinant VEGF(164) Proc. Natl. Acad. Sci. U.S.A. 2014;111(19):6952–6957. doi: 10.1073/pnas.1404605111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tsou Y.-H., Khoneisser J., Huang P.-C., Xu X. Hydrogel as a bioactive material to regulate stem cell fate. Bioactive Materials. 2016;1(1):39–55. doi: 10.1016/j.bioactmat.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cui Z., Lee B.H., Pauken C., Vernon B.L. Degradation, cytotoxicity and biocompatibility of NIPAAm-based thermosensitive, injectable and bioresorbable polymer hydrogels. J. Biomed. Mater. Res. 2011;98(2):159–166. doi: 10.1002/jbm.a.33093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Garbern J.C., Minami E., Stayton P.S., Murry C.E. Delivery of basic fibroblast growth factor with a pH-responsive, injectable hydrogel to improve angiogenesis in infarcted myocardium. Biomaterials. 2011;32(9):2407–2416. doi: 10.1016/j.biomaterials.2010.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fujimoto K.L., Ma Z., Nelson D.M., Hashizume R., Guan J., Tobita K., Wagner W.R. Synthesis, characterization and therapeutic efficacy of a biodegradable, thermoresponsive hydrogel designed for application in chronic infarcted myocardium. Biomaterials. 2009;30(26):4357–4368. doi: 10.1016/j.biomaterials.2009.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Phelps E.A., Landázuri N., Thulé P.M., Taylor W.R., García A.J. Bioartificial matrices for therapeutic vascularization. Proc. Natl. Acad. Sci. 2010;107(8):3323–3328. doi: 10.1073/pnas.0905447107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zachman A.L., Wang X., Tucker-Schwartz J.M., Fitzpatrick S.T., Lee S.H., Guelcher S.A., Skala M.C., Sung H.-J. Uncoupling angiogenesis and inflammation in peripheral artery disease with therapeutic peptide-loaded microgels. Biomaterials. 2014;35(36):9635–9648. doi: 10.1016/j.biomaterials.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rufaihah A.J., Vaibavi S.R., Plotkin M., Shen J., Nithya V., Wang J., Seliktar D., Kofidis T. Enhanced infarct stabilization and neovascularization mediated by VEGF-loaded PEGylated fibrinogen hydrogel in a rodent myocardial infarction model. Biomaterials. 2013;34(33):8195–8202. doi: 10.1016/j.biomaterials.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 94.Leslie-Barbick J.E., Saik J.E., Gould D.J., Dickinson M.E., West J.L. The promotion of microvasculature formation in poly(ethylene glycol) diacrylate hydrogels by an immobilized VEGF-mimetic peptide. Biomaterials. 2011;32(25):5782–5789. doi: 10.1016/j.biomaterials.2011.04.060. [DOI] [PubMed] [Google Scholar]
- 95.Salimath A.S., Phelps E.A., Boopathy A.V., Che P.-l., Brown M., García A.J., Davis M.E. Dual delivery of hepatocyte and vascular endothelial growth factors via a protease-degradable hydrogel improves cardiac function in rats. PLoS One. 2012;7(11) doi: 10.1371/journal.pone.0050980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bhutani S., Nachlas A.L.Y., Brown M.E., Pete T., Johnson C.T., García A.J., Davis M.E. Evaluation of hydrogels presenting extracellular matrix-derived adhesion peptides and encapsulating cardiac progenitor cells for cardiac repair. ACS Biomater. Sci. Eng. 2018;4(1):200–210. doi: 10.1021/acsbiomaterials.7b00502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Berdichevski A., Simaan Yameen H., Dafni H., Neeman M., Seliktar D. Using bimodal MRI/fluorescence imaging to identify host angiogenic response to implants. Proc. Natl. Acad. Sci. Unit. States Am. 2015;112(16):5147–5152. doi: 10.1073/pnas.1502232112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boisserand L.S., Kodama T., Papassin J., Auzely R., Moisan A., Rome C., Detante O. Biomaterial applications in cell-based therapy in experimental stroke. Stem Cell. Int. 2016;2016:6810562. doi: 10.1155/2016/6810562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jeon O., Kang S.-W., Lim H.-W., Hyung Chung J., Kim B.-S. Long-term and zero-order release of basic fibroblast growth factor from heparin-conjugated poly(l-lactide-co-glycolide) nanospheres and fibrin gel. Biomaterials. 2006;27(8):1598–1607. doi: 10.1016/j.biomaterials.2005.08.030. [DOI] [PubMed] [Google Scholar]
- 100.Feng G., Zhang J., Li Y., Nie Y., Zhu D., Wang R., Liu J., Gao J., Liu N., He N., Du W., Tao H., Che Y., Xu Y., Kong D., Zhao Q., Li Z. IGF-1 C domain-modified hydrogel enhances cell therapy for AKI. J. Am. Soc. Nephrol. 2016;27(8):2357–2369. doi: 10.1681/ASN.2015050578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kumar V.A., Taylor N.L., Shi S., Wang B.K., Jalan A.A., Kang M.K., Wickremasinghe N.C., Hartgerink J.D. Highly angiogenic peptide nanofibers. ACS Nano. 2015;9(1):860–868. doi: 10.1021/nn506544b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kumar V.A., Liu Q., Wickremasinghe N.C., Shi S., Cornwright T.T., Deng Y., Azares A., Moore A.N., Acevedo-Jake A.M., Agudo N.R., Pan S., Woodside D.G., Vanderslice P., Willerson J.T., Dixon R.A., Hartgerink J.D. Treatment of hind limb ischemia using angiogenic peptide nanofibers. Biomaterials. 2016;98:113–119. doi: 10.1016/j.biomaterials.2016.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]