Abstract
The aim of this study was to evaluate the early and sustained effects of tinnitus educational counseling on chronic primary tinnitus and related problems. A descriptive longitudinal cohort study was conducted with 159 adult patients suffering from chronic primary tinnitus and sleep problems. All patients received tinnitus educational counseling, sleep adjustment, and vegan dietary advice. At short-term assessment within 3 months and long-term follow-up at 6–26 months, perceived changes in tinnitus were assessed with the Tinnitus Handicap Inventory (THI) and the Tinnitus Evaluation Questionnaire (TEQ), respectively. In TEQ, the volume of subjective tinnitus was scored according to realistic environments in which tinnitus could be heard. Sleep quality was assessed with questionnaires developed in our laboratory. Most of the subjects showed significant early improvement in their THI scores (96/159, 60.38%; from 46.11 ± 22.74 to 31.94 ± 20.41, t = 11.16, p < 0.001, Cohen's d = 0.66). Tinnitus volume (39/159, 24.53%, from 2,2 to 2,1, z = -3.56, p < 0.001) and sleep quality (68/159, 42.77%; from 7.13 ± 3.11 to 6.31 ± 2.75, t = 3.73, p < 0.001, Cohen's d = 0.28) were also improved. Long-term follow-up TEQ results indicated that tinnitus loudness, the impact of tinnitus on sleep, concentration, and emotional state were all improved since the prior consultation (p = 0.001, 0.026, 0.012, and <0.001). Short-term improvement of tinnitus severity correlated directly with improvement of sleep quality (odds ratio (OR) = 0.30, 95% confidence interval (CI): 0.14–0.64, p = 0.002), initial THI score (OR = 1.02, 95% CI: 1.01 to 1.04, p = 0.006), compliance with sleep advice (OR = 2.27, 95% CI: 1.02–5.05, p = 0.044), and nervous disposition (OR = 2.80, 95% CI: 1.25–6.30, p = 0.013). A future randomized controlled trial would be carried out to examine the effect of sole tinnitus educational counseling.
1. Introduction
Tinnitus is the persistent and bothersome perception of sound in the absence of an external source. The prevalence of tinnitus lasting for more than 5 min at a time is reported to range from 11.9% to 30.3% [1]. Traditional approaches to the treatment of tinnitus are largely ineffective [2]. Tinnitus educational counseling is a form of psychological therapy that is cost-effective [3], even in the long term [4]. Such counseling, which includes the provision of general information about the physiology of hearing, pathophysiology of tinnitus, audiometric testing, and strategies for the minimization and control of tinnitus, has been found to be as effective as tinnitus masking and tinnitus retraining therapy within periods as short as 6 months [4]. Patients have also included counseling and education, as well as cognitive behavioral therapy (CBT), among tinnitus therapy methods that they have found to be most effective [5].
The provision of advice regarding sleep and lifestyle modifications is another form of psychological therapy for tinnitus [6], as even relatively healthy people with chronic tinnitus may suffer from sleep-related problems [7]. Sleep disturbances increase the risk of tinnitus [8] and associated functional impairment [9, 10]. Insomnia increases patients' negative reactions to tinnitus [7, 11], leading to depression [12]. The association between functional impairment and sleep disturbance becomes more noticeable over time [13]. The evaluation and treatment of sleep disturbances help reduce patients' subjective handling of tinnitus [11] and are important components of tinnitus management, resulting in improved outcomes [10, 14]. The role of diet has also been mentioned in some studies [15, 16].
However, studies regarding the impact of sleep on tinnitus management are relatively scarce compared with those examining the control of other subjective symptoms, such as pain [17–19]. Tinnitus and pain have similar characteristics, such as their subjective nature, the limited success of interventions, and being characterized by hypersensitivity to sensory stimulation [20]. We analyzed the impact of sleep adjustment and sleep quality on tinnitus severity. We also examined the potential influence of personality characteristics on tinnitus [21]. Tinnitus educational counseling and sleep adjustment in tinnitus sufferers were included in this study. Early and long-term (>6 months) effects of tinnitus educational counseling were monitored together with the influence of personality characteristics on these effects.
2. Materials and Methods
2.1. Subjects
The demographic and clinical details of 159 adult (age > 18 years) patients who attended special clinics for tinnitus, hearing loss, and vertigo at the Hearing Center, Department of Otolaryngology-Head and Neck Surgery, West China Hospital of Sichuan University, between January 2015 and February 2017 were analyzed prospectively. Our institutional review board had no ethical concerns and approved this study, which was implemented in accordance with the board's medical-ethical standards. Subjects included in the study population provided consent for the use of their clinically obtained data.
The criteria for patient selection were the following: (a) primary complaint of tinnitus lasting more than 6 months, with or without sensorineural hearing loss [3]; (b) clinical evaluation including medical history, physical examination, and comprehensive audiological examination; (c) availability of complete evaluation records and lifestyle questionnaires; (d) unhealthy sleep habits, such as going to bed late and rising late and/or insufficient or excessive duration of sleep, and dissatisfaction with sleep quality; and (e) receipt of oral and written sleep and lifestyle advice in addition to one-on-one tinnitus educational counseling.
2.2. Intervention
A combination of tinnitus educational counseling and sleep/lifestyle advice was delivered by a trained audiology technician and then by the treating physician during the first consultation. Detailed counseling by the trained audiology technician (1–2 h) and the physician (10–20 min) was ensured for all subjects. Tinnitus educational counseling consisted of three aspects: (a) explanation of the physiology of hearing, pathophysiology of tinnitus, audiometric testing, and strategies for the minimization and control of tinnitus; (b) discussion of the relationship between tinnitus and sleep and the importance of sleep hygiene; and (c) reassurance that “tinnitus is like a well-meaning alarm” and thus a useful health reminder. The concept of sleep hygiene includes the proper timing and sufficient duration of, and subjective satisfaction with, sleep, translating into highly effective sleep and enhanced alertness during daily activities [22]. In the Yellow Emperor's Canon [23], a classic traditional Chinese medicine text, recommendations for healthful sleep include falling asleep by 11 pm and rising between 5 am and 7 am, thereby ensuring an in-bed sleeping window between 10 pm and 6 am. In consideration of daytime sleepiness and nonadaptation in some patients, a short nap before 2 pm for a maximum of 30 min was advised.
2.3. Data Collection
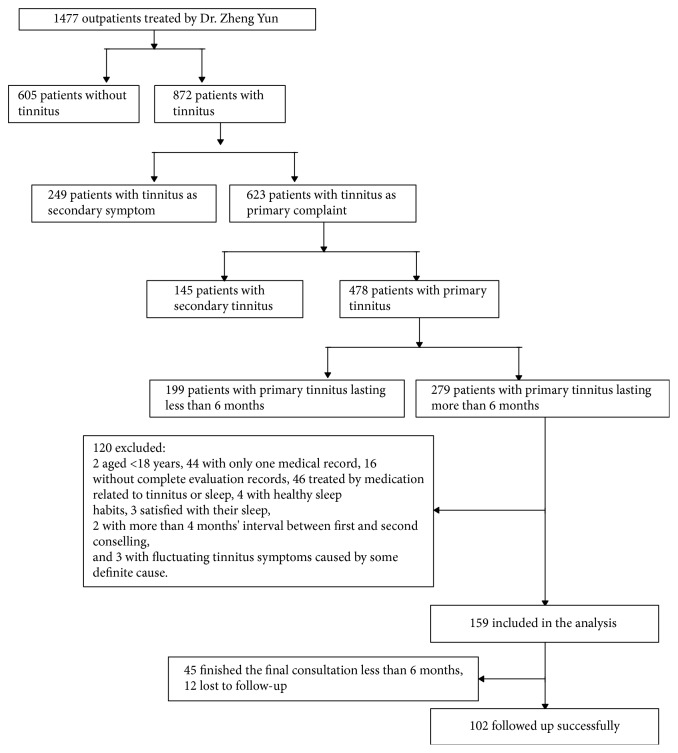
The inclusion of cases into this study is summarized in the flowchart shown in Figure 1. Patients provided informed consent for the use of their deidentified data for education and research. All patients provided their basic personal information, including gender, age, level of education, occupation, marital status, living habits, contact information/address, and nationality. They also provided self-reported personality trait information, underwent audiometry, and assessments of tinnitus and sleep. Hearing assessed with a pure tone hearing threshold test at frequencies in the range of 250–8000 Hz demonstrated that all subjects had thresholds <25 dB hearing level, indicating normal hearing.
Figure 1.
Flowchart of patient enrollment into the study.
At each consultation, patients received 1–2 hours of tinnitus education, sleep hygiene information, and vegan dietary advice (i.e., not to eat any animal products and how to ensure sufficient nutrition from other staple foods). Their self-reported tinnitus status and lifestyle questionnaire responses were recorded. Tinnitus severity, tinnitus volume, and sleep quality were assessed during the first and subsequent consultations (mean interassessment interval, 30.70 ± 19.95 days). Initial and postintervention sleep qualities were described for the periods of 1–3 months before the intervention and 1–4 weeks before the second to last evaluation. The short- and long-term severity of tinnitus, in terms of the extent of impairment caused by the presence of tinnitus, were assessed with the Chinese-Mandarin versions of the Tinnitus Handicap Inventory (THI-CM) [24] and Tinnitus Evaluation Questionnaire (TEQ) [25], respectively, to assess the short-term and long-term changes.
The THI-CM consists of 25 items grouped into functional, emotional, and catastrophic subscales. Its test-retest reliability (Pearson's r = 0.98) and internal validity (Cronbach's α = 0.93) have been documented [24]. Total THI scores were taken to indicate five grades of tinnitus severity: Grade I (score, 0–16), slight tinnitus that is perceived only in a quiet environment and generally benign; Grade II (score, 18–36), mild tinnitus that can be masked easily and interferes with sleep only occasionally but not daily activities; Grade III (score, 38–56), moderate tinnitus that is pervasive but interferes with sleep or daily activities only occasionally; Grade IV (score, 58–76), severe tinnitus that is perceived most of the time and disturbs sleep patterns and daily activities often; and Grade V (score, 78–100), catastrophic tinnitus symptoms that disturb sleep and daily activities consistently [26]. Although a difference ≥ 20 points between pre- and postintervention scores is considered statistically significant [27], a difference of 7 points is accepted as clinically significant [28]. In this study, score changes of ≥7 points were taken to indicate a moderate change, and changes ≥ 20 points were taken to denote strong improvement or serious worsening. Changes of ≤6 points were recorded as “no change.” Subjects with THI-CM score reductions of ≥7 points were designated as the effective group, and all others formed the noneffective group.
The TEQ consists of six questions. The first five were the following: when is your tinnitus heard? (responses: no tinnitus, in quiet surroundings, in normal surroundings, and in noisy surroundings); is your tinnitus continuous or intermittent? (responses: no tinnitus, more absence than presence, absence is equal to presence, and less absence than presence); does your tinnitus affect your falling asleep? (responses: never, sometimes, often, and always); does your tinnitus affect your concentration? (responses: never, sometimes, often, and always); and does your tinnitus affect your emotions? (responses: never, sometimes, often, and always). The four possible answers to each of these questions correspond to a 0–3-point scale. The sixth item was a tinnitus severity score of tinnitus assessed by evaluator. The first five questions were used for follow-up evaluation and contrasted with the previous face-to-face assessments. Tinnitus volume was assessed by a combination of psychoacoustic methods [29] and the administration of a visual analogue scale (VAS) [30] and numeric rating scales [31]. The TEQ response to the first item, which reflects broadly accessible real-life situations, was used to evaluate tinnitus loudness.
We developed a five-item sleep quality survey that included the following items: difficulty falling asleep (No. 1), frequency of awakening after sleep onset (No. 2), difficulty returning to sleep after awakening in night sleep (No. 3), daytime sleepiness (No. 4), and number of times of awakening (No. 5). The response options for items 1–4 were “never,” “≤1–2 times per week,” “3–4 times per week,” and “≥5 times per week.” Response options for item No. 5 were “never,” “1 time per night,” “2 times per night,” and “≥3 times per night.” Scores were assigned to these responses in ascending order. The criterion for insomnia was at least three times per week of sleep initiation or maintenance problems [32]. According to the principle of change in health-related quality of life [33], a change of more than half a standard deviation at baseline was taken to indicate improvement or worsening of sleep quality.
To assess the participants' personality characteristics, we developed a brief questionnaire with the following yes/no questions: Are you always impatient? Are you constantly anxious for others? Are you continually irritable? Are you nervous all the time? Are you frequently suspicious? Are you a perfectionist?
2.4. Follow-up Assessment
We contacted by phone the patients who completed counseling within the one-week unified study period. The follow-up period after the last counseling session ranged from 6 to 26 months (16.04 ± 4.56 months). Follow-up by telephone was considered to be more convenient than a clinic visit, e-mail, or online program. The TEQ questions were asked in the phone follow-up. In addition, we asked the following three questions: did you accept any other treatment apart from tinnitus educational counseling? (responses: no, yes); did you follow the advice on sleep adjustment? (responses: no, partly, or absolutely); and did you follow the vegan dietary advice provided? (responses: no, partly, or absolutely).
2.5. Statistical Analysis
Statistical analyses were performed with IBM SPSS Statistics 20, with a significance criterion of p < 0.05 considered to be statistically significant. Data were denoted as means with standard deviations or medians with interquartile ranges (IQRs). The mean total THI scores at the first and last consultations were compared using the paired-samples t-test. Scores for tinnitus volume and sleep quality were compared using the Wilcoxon signed-rank test. Factors related to improvement in tinnitus severity were determined by logistic regression analysis. The effect size (Cohen's d) was calculated according to the formula described previously [34]. The postintervention mean THI scores were deducted from the preintervention mean, and the result was divided by the pooled pre-/postintervention standard deviation. Stepwise logistic regression analysis was used to predict what factors were associated with the change in THI. Firstly, the demographic and clinical characteristics were compared between the effective group and noneffective group in short-term observation. Then, the characteristics with statistical differences in the two groups would be included in the regression analysis to predict the related factors.
3. Results
3.1. Subject Characteristics
This study included 159 patients (77 males and 82 females) with an average age of 44.86 ± 13.44 years. The mean of the pure-tone averages at 0.5 kHz, 1 kHz, 2 kHz, and 4 kHz was 29 dBHL. According to THI scores, 12 (7.55%) patients had Grade I, 50 (31.44%) had Grade II, 48 (30.19%) had Grade III, 29 (18.24%) had Grade IV, and 20 (12.58%) patients had Grade V tinnitus. Tinnitus was bilateral in 56 cases and unilateral in 103 cases (left, 54 cases; right, 49 cases). Nearly half (49.06%, 78/159) of the subjects met the criteria for insomnia, whereas 50.94% (81/159) did not have a serious sleep problem. Of 159 patients, 115 complied strictly with the sleep advice, going to bed before 10 pm and waking before 6 am, up to the time of the short-term assessment; they were classified as subjects who adjusted (group A). The remaining 44 patients did not change their usual sleep habits, which included going to bed after 11 pm and having <6 h sleep or waking after 8 am and having >8 h sleep; they were classified as subjects who did not adjust (group NA).
In total, 114 patients finished the final consultation at ≥6 months. Among them, 102 patients were followed up successfully within the same week (April 22–28, 2017). Thus, 18 patients completed 6–11 months' counseling, 25 patients completed 12–17 months, 30 patients completed 18–23 months, and 29 patients completed 24–26 months' counseling. Twelve patients were lost to follow-up, as they could not be contacted by telephone. The follow-up rate was thus 89.47%.
3.2. Overall Improvement of Tinnitus and Sleep Quality in the Short-Term (30.70 ± 19.95 Days) Assessment Period
Mean THI, tinnitus volume, and sleep quality scores declined from the first to the last assessment in 159 subjects. The mean THI score decreased from 46.11 ± 22.74 to 31.94 ± 20.41 (t = 11.16, p < 0.001). The postintervention effect size relative to preintervention one was moderate (Cohen's d = 0.66). THI score changes indicated that tinnitus became less severe in more than half (96/159, 60.38%) of the subjects. However, THI scores showed moderate worsening in 7 patients and serious worsening in 3 patients.
The postintervention tinnitus volume score (median, IQR: 2, 1) was also lower than that at baseline (median, IQR: 2, 2; z = −3.56, p < 0.001). Self-assessed tinnitus volume was mitigated in 39 (24.53%, 39/159) cases but worsened in 4 cases.
Sleep quality also improved, as shown by a significant reduction of the score from 7.13 ± 3.11 to 6.31 ± 2.75 (t = 3.73, p < 0.001). The effect size was small (Cohen's d = 0.28). Sleep quality improved in nearly half (42.77%, 68/159) of the subjects. The number of patients meeting the criterion for insomnia declined from 78 at baseline to 64 after intervention. Improvements in difficulty falling asleep, difficulty returning to sleep after awakening, and daytime sleepiness in patients who undertook sleep adjustment are shown in Table 1.
Table 1.
Pre- and postintervention sleep quality scores (N = 159).
| Subjects | Evaluation relative to intervention | Difficulty falling asleep, median (IQR) | Frequency of waking after sleep onset, median (IQR) | No. of times waking after sleep onset, median (IQR) | Difficulty returning to sleep after waking at midnight, median (IQR) | Daytime sleepiness, median (IQR) |
Total, mean ± SD |
|---|---|---|---|---|---|---|---|
| All | Pre | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (1,1) | 7.12 ± 3.07 |
| Post | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (0,2) | 1 (0,1) | 6.31 ± 2.75 | |
| Z | -2.341 | -0.024 | -1.688 | -3.068 | -4.093 | -3.545 | |
| p | 0.019 | 0.981 | 0.091 | 0.002 | <0.001 | <0.001 | |
| A | Pre | 2 (1,2) | 1 (1,2) | 2 (1,2) | 2 (1,2) | 1 (1,2) | 7.39 ± 3.06 |
| Post | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (0,2) | 1 (1,1) | 6.38 ± 2.79 | |
| Z | -2.17 | -0.39 | -1.59 | -2.87 | -4.024 | -3.525 | |
| p | 0.030 | 0.692 | 0.113 | 0.004 | <0.001 | <0.001 | |
| NA | Pre | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (1,2) | 1 (1,1) | 6.41 ± 3.03 |
| Post | 1 (1,2) | 1 (1,2) | 1(1,2) | 1 (0,2) | 1 (0,1) | 6.11 ± 2.68 | |
| Z | -0.938 | -0.593 | -0.632 | -1.143 | -1.091 | -0.897 | |
| p | 0.348 | 0.553 | 0.527 | 0.253 | 0.275 | 0.370 |
A, with sleep adjustment; NA, without adjustment.
3.3. Factors Related to the Improvement of Tinnitus Severity in the Short- Term (30.70 ± 19.95 Days) Assessment Period
The demographic characteristics, initial THI scores, sleep quality at last contact, improvement in sleep quality, compliance with sleep adjustment, and nervous disposition differed significantly between effective group and noneffective group (p < 0.05) (Table 2). These five factors were treated as variables in a stepwise logistic regression analysis with forward selection intended to predict which factors were related to the change in THI. Logistic regression analysis indicated that tinnitus improvement correlated positively with improved sleep quality (OR = 0.30, 95% CI: 0.14–0.64, p = 0.002), initial THI score (OR = 1.02, 95% CI: 1.01–1.04, p = 0.006), compliance with sleep advice (OR = 2.27, 95% CI: 1.02–5.05, p = 0.044), and nervous disposition (OR = 2.80, 95% CI: 1.25–6.30, p = 0.013). Sleep quality determined at last assessment was removed from the model during the process of stepwise regression (p = 0.067).
Table 2.
Demographic and clinical characteristics of the effective and noneffective groups, defined by THI score.
| Characteristic |
Effective (N = 96) |
Noneffective (N = 63) |
P |
|---|---|---|---|
| Gender, no. of males : no. of females | 50 : 46 | 27 : 36 | 0.255 a |
| Mean age ± SD, years | 44.03 ± 13.12 | 46.13 ± 13.93 | 0.338 b |
| Hearing loss, N (%) | 64 (66.7%) | 46 (73.0%) | 0.396 a |
| Education degree, N (%) | 0.197 | ||
| Primary school | 7 (7.3%) | 7 (11.1%) | |
| Junior high school | 24 (25.0%) | 10 (15.9%) | |
| Senior high school | 16 (16.7%) | 18 (28.6%) | |
| University | 44 (45.8%) | 27 (42.9%) | |
| Master's degree or higher | 5 (5.2%) | 1 (1.6%) | |
| Character traits | |||
| Impatient | 49 (51.0%) | 41 (65.1%) | 0.081 a |
| Anxious for others | 43 (44.8%) | 29 (46.0%) | 0.878 a |
| Irritable | 38 (39.6%) | 17 (27.0%) | 0.102 a |
| Nervous | 42 (43.8%) | 12 (19.0%) | 0.001 a |
| Suspicious | 11 (11.5%) | 4 (6.3%) | 0.281 a |
| Perfectionist | 17 (17.7%) | 17 (27.0%) | 0.163 a |
|
| |||
| Median tinnitus duration, months (IQR) | 24 (62) | 24 (48) | 0.798 c |
| Mean initial THI score ± SD | 51.25 ± 20.85 | 38.60 ± 23.15 | <0.001 b |
| Mean first-to-last-contact interval ± SD, days | 35.41 ± 20.86 | 35.10 ± 20.14 | 0.926 b |
| Sleep quality at first contact | 7.38 ± 2.98 | 6.76 ± 3.29 | 0.225 b |
| Sleep quality at last contact | 5.85 ± 2.45 | 7.00 ± 3.05 | 0.010 c |
| Change in sleep quality, N (%) | |||
| Improved | 53 (55.2%) | 15 (23.8%) | <0.001 a |
| Not improved | 43 (44.8%) | 48 (76.2%) | |
| Sleep advice compliance, N (%) | 0.017 a | ||
| Better | 76 (79.2%) | 39 (61.9%) | |
| Worse | 20 (20.8%) | 24 (38.1%) | |
THI, Tinnitus Handicap Inventory.
aChi-squared test, bone-way ANOVA, and cMann–Whitney U test.
3.4. Long-Term (16.04 ± 4.56 Months) Change of Tinnitus Indicated by TEQ
Among the 102 patients who received tinnitus counseling (6–26 months), 6 patients were prescribed short rounds of pharmacotherapy by doctors outside the hospital. Tinnitus and its impacts are described in Table 3. Seventy-eight patients reported that tinnitus no longer affected their falling asleep, 96 patients reported that tinnitus had stopped interrupting their concentration, and 64 patients reported that tinnitus no longer influenced their emotions. Tinnitus disappeared in 5 patients (Table 4). In addition, most patients continued to heed the sleep advice, following sleep timetables and adjusting their sleep, after the last consultation. 42 patients continued to go to bed and get up early (including 9 patients who did not change their previous sleep habits), and 38 patients followed either the early bedtime or early awakening routines. 22 patients did not change their late bedtime and awakening patterns.
Table 3.
Short- and long-term changes in tinnitus indicated by TEQ (N = 102).
| Item | Time point | Tinnitus characteristic | P | |||
|---|---|---|---|---|---|---|
| None | Quiet conditions | Normal conditions | Noisy conditions | |||
| Tinnitus loudness | First contact | 0 | 29 | 42 | 31 | 0.098 a |
| Last contact | 0 | 40 | 43 | 19 | ||
| Follow-up | 5 | 60 | 22 | 15 | 0.001 b | |
| Interval > duration | Interval ≈ duration | Duration > interval | Continuity | |||
|
| ||||||
| Tinnitus continuance | First contact | 0 | 2 | 4 | 96 | 0.072 a |
| Last contact | 0 | 7 | 9 | 86 | ||
| Follow-up | 5 | 9 | 8 | 80 | 0.137 b | |
| None | Sometimes | Often | Always | |||
|
| ||||||
| Impact on sleep | First contact | 37 | 21 | 23 | 21 | 0.001 a |
| Last contact | 58 | 27 | 8 | 9 | ||
| Follow-up | 78 | 14 | 6 | 4 | 0.026 b | |
|
| ||||||
| Impact on concentration | First contact | 59 | 30 | 12 | 1 | 0.005 a |
| Last contact | 82 | 15 | 5 | 0 | ||
| Follow-up | 96 | 5 | 1 | 0 | 0.012 b | |
|
| ||||||
| Impact on emotion | First contact | 4 | 58 | 33 | 7 | <0.001 a |
| Last contact | 17 | 70 | 14 | 1 | ||
| Follow-up | 64 | 35 | 2 | 1 | <0.001 b | |
aFirst contact versus last contact; blast contact versus follow-up.
Table 4.
Characteristics of 5 patients with complete tinnitus resolution.
| Characteristic | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Gender | Female | Female | Female | Male | Female |
| Age, years | 44 | 65 | 51 | 24 | 48 |
| Tinnitus side | Right | Bilateral | Right | Left | Bilateral |
| Hearing | Normal | Impaired | Normal | Normal | Impaired |
| Initial THI severity grade | I | II | II | III | II |
| Tinnitus loudness | In quiet | In noise | In quiet | In quiet | In quiet |
|
| |||||
| Durations, months | |||||
| Tinnitus before first contact | 6 | 24 | 13 | 11 | 30 |
| Tinnitus cessation after initial education | 2.7 | 15.5 | 6 | 11 | 7 |
| Total tinnitus before cessation | 11 | 39.5 | 19 | 22 | 37 |
| Follow-up duration after initial education | 16.7 | 22.5 | 22 | 12 | 12.5 |
| Strict sleep adjustment | Until date | Until date | Until date | Until date | Until date |
| Diet adjustment | Controlled partly until date |
Controlled partly until date |
Controlled strictly before tinnitus cessation | Controlled strictly for initial 6 months | Controlled strictly for initial 11 months |
4. Discussion
The intention of this study was to explore the short-term effects of tinnitus educational counseling as solitary therapy for chronic primary tinnitus and its long-term sustainability, taking into account related factors such as sleep adjustment and sleep quality improvement. The results suggest that tinnitus educational counseling is sufficient to satisfy many patients, as corroborated by previous studies [4]. The early and long-term assessments showed decreased severity of tinnitus and sustainment of the improvement. Personality characteristics, adherence to sleep hygiene, and improvement in sleep quality were related to the improvement of tinnitus severity.
THI scores improved significantly within 3 months in the majority of subjects, although the effect size was moderate. Tinnitus volume was also reduced significantly in nearly a quarter of the subjects. This study differed from other studies [4] with respect to the features of tinnitus educational counseling, which accounts for the better outcomes observed. In addition to conventional tinnitus education, we commented that tinnitus was a well-meaning alarm to remind individuals to attach more importance to health; study participants responded positively, similar to acceptance therapy [35], a psychotherapeutic approach that lessens emotional avoidance and increases the capacity for behavioral change [36]. Acceptance was strongly and inversely related to tinnitus severity causing impairment and attendant anxiety and depression [35]. Another characteristic of the treatment was adherence to sleep hygiene. Clear correlations were observed between sleep problems and erratic sleep hygiene [37]. Thus, a focused approach to participants' sleep schedules was beneficial, as it seemed to enhance the effect of tinnitus educational counseling. The results suggest that outcomes can be improved by a focus on sleep hygiene as a specific intervention in patients with tinnitus and sleep problems. However, the reasons for serious worsening of tinnitus and increased tinnitus volume in three cases each are not clear. The chance for improvement might have been dissipated by the rigidity of the approach [38]. Strict compliance with the specified sleep timing and vegan diet might have resulted in major changes in patients' lifestyles, and maladaptation, frustration, and anxiety might have resulted in worsening of tinnitus. A graduated and personalized approach may thus be more acceptable and yield better outcomes.
The sleep quality of patients with insomnia has been shown to be improved with sleep restriction [39], which involves implementation of a prescribed amount of total time allowed in bed. Subjective sleep quality, indicated by sleep onset latency, awakening time after sleep onset, and sleep efficiency, improved after sleep restriction, and the effect size was moderate to large [39]. Our results showed that sleep quality improved after tinnitus educational counseling in patients with tinnitus-related sleep problems through adherence to sleep hygiene, especially with regard to difficulty falling asleep, going back to sleep again after nocturnal awakening, and daytime sleepiness. Advice on sleep adjustment emphasized the timing of going to bed and awakening, in addition to sleep duration, rooted in the principle of health preservation in traditional Chinese medicine. This form of sleep adjustment was clearly beneficial, improving nocturnal sleep quality and daytime function. These results highlight the easier aspects of sleep improvement by personal adjustments, which were stressed properly during consultations. Nervous individuals seemed to experience greater benefits, suggesting that personality characteristics play influential roles; for example, neuroticism increases and extraversion decreases in patients with subjective idiopathic tinnitus [21]. As patients who are neurotic and introverted may take better advantage of psychiatric consultation, tinnitus education as solitary therapy could be more effective for them. In our daily clinic work, we have observed that some nervous patients were more likely to seek information about their tinnitus online and to be anxious about serious diseases related to it. Counseling could thus alleviate the negative effects of tinnitus. Therefore, personalized and targeted counseling with consideration of personality characteristics is advisable.
In a prospective behavioral therapy study with a 15-year follow-up period, tinnitus disappeared in 13 of 244 (5.3%) patients with chronic tinnitus [40]. In our 6–26-month follow-up of 102 patients by telephone, tinnitus had disappeared within 16 months after the initial contact in 5 (4.81%) patients, a resolution rate similar to that reported in the aforementioned 15-year follow-up study. Prediction of the time point at which tinnitus disappears completely would be difficult. However, these five patients had some common features, such as lesser tinnitus severity (Grades I–III) and occurrence of tinnitus only under quiet conditions (tinnitus could be heard in noisy surroundings in one case). The insistence on early sleep and awakening times also probably contributed to the resolution of tinnitus in these patients because of better motivation and effort on their parts.
The findings of this study suggest that the combination of tinnitus educational counseling and provision of sleep hygiene advice is a feasible management option for tinnitus in primary care, especially in underdeveloped areas. Although CBT or a combination of sound therapy and CBT-based counseling is recommended for tinnitus management [3, 41], these methods may be limited by the scarcity of clinical and trainee psychologists. To overcome this limitation, a simplified version of psychological intervention which can be implemented by other clinical professionals should be developed to enable the holistic treatment of tinnitus [42]. In this study, tinnitus educational counseling and advice on sleep hygiene were delivered primarily by a trainee audiology technician, and this approach may be an alternative for patients in regions without professional psychology services. General practitioners (GPs) are often the first professionals encountered by patients seeking help with their tinnitus, and most otolaryngologists see referred patients, typically from GPs [2]. The addition of therapy such as CBT or sound therapy might lead to greater improvement, and the number of cured patients might increase with longer periods of observation. The combination of tinnitus educational counseling and sleep hygiene, with an emphasis on self-management of sleep problems, is applicable in underdeveloped areas and in primary health care, and may be more cost-effective than sole tinnitus educational counseling for patients with chronic primary tinnitus, especially when accompanied by sleep problems.
4.1. Limitations
Because this study was descriptive and not a randomized controlled trial, it has some inherent limitations. Because the numbers of subjects who underwent sleep adjustment, hearing, and tinnitus assessments were not distributed equally, this work may be considered a pilot study. The timing and duration of follow-up were not consistent across the study sample due to differences in registration dates. In addition, we used a developed-in-house personality, sleep quality, and tinnitus volume survey instead of validated instruments (although the THI is validated). Confounding factors, including those related to lifestyle, diet, and exercise, could not be excluded. Baseline THI scores were <7 in three cases, preventing accurate assessment of the improvement of tinnitus severity.
5. Conclusion
The study results demonstrated that, by tinnitus education counseling, tinnitus severity of THI decreased in short-term observation, and the tinnitus volume and its negative impact on mood, sleep, and concentration had also improved in long-term follow-up. Changes in unhealthy sleep habits can reduce tinnitus severity and improve sleep quality. Patients with less severe tinnitus and healthy sleep patterns tend to be cured more easily. Thus, tinnitus education should not only include sleep hygiene but also emphasize patient compliance. Patient personality is an important factor, and nervous patients are more likely to benefit from educational counseling.
Acknowledgments
This work was supported by a grant from the Clinical Study of Standard Diagnosis and Rehabilitation of Tinnitus Patients and a grant from the Health and Family Planning Commission of Sichuan Province (no. 150134).
Data Availability
All data generated or analyzed during this study are included within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.McCormack A., Edmondson-Jones M., Somerset S., Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hearing Research. 2016;337:70–79. doi: 10.1016/j.heares.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Hall D. A., Láinez M. J. A., Newman C. W., et al. Treatment options for subjective tinnitus: Self reports from a sample of general practitioners and ENT physicians within Europe and the USA. BMC Health Services Research. 2011;11, article no. 302 doi: 10.1186/1472-6963-11-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tunkel D. E., Bauer C. A., Sun G. H., Rosenfeld R. M. American Academy of Otolaryngology—Head and Neck Foundation Clinical Practice Guideline: Tinnitus. Otolaryngology—Head and Neck Surgery. 2014;151(1_suppl):P20–P20. doi: 10.1177/0194599814538403a56. [DOI] [PubMed] [Google Scholar]
- 4.Henry J. A., Stewart B. J., Griest S., Kaelin C., Zaugg T. L., Carlson K. Multisite Randomized Controlled Trial to Compare Two Methods of Tinnitus Intervention to Two Control Conditions. Ear and Hearing. 2016;37(6):e346–e359. doi: 10.1097/AUD.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 5.Aazh H., Moore B. C. J., Lammaing K., Cropley M. Tinnitus and hyperacusis therapy in a UK National Health Service audiology department: Patients’ evaluations of the effectiveness of treatments. International Journal of Audiology. 2016;55(9):514–522. doi: 10.1080/14992027.2016.1178400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson D. M., Hall D. A., Walker D.-M., Hoare D. J. Psychological Therapy for People with Tinnitus: A Scoping Review of Treatment Components. Ear and Hearing. 2017;38(2):149–158. doi: 10.1097/AUD.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crönlein T., Langguth B., Pregler M., Kreuzer P. M., Wetter T. C., Schecklmann M. Insomnia in patients with chronic tinnitus: Cognitive and emotional distress as moderator variables. Journal of Psychosomatic Research. 2016;83:65–68. doi: 10.1016/j.jpsychores.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Kim H.-J., Lee H.-J., An S.-Y., et al. Analysis of the prevalence and associated risk factors of Tinnitus in adults. PLoS ONE. 2015;10(5) doi: 10.1371/journal.pone.0127578.e0127578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Attanasio G., Russo F. Y., Roukos R., Covelli E., Cartocci G., Saponara M. Sleep architecture variation in chronic tinnitus patients. Ear and Hearing. 2013;34(4):503–507. doi: 10.1097/aud.0b013e31827bc436. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y. F., Hu J., Streelman M., Guthrie O. W. The epworth sleepiness scale in the assessment of sleep disturbance in veterans with tinnitus. International Journal of Otolaryngology. 2015;2015:9. doi: 10.1155/2015/429469.429469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miguel G. S., Yaremchuk K., Roth T., Peterson E. The effect of insomnia on tinnitus. Annals of Otology, Rhinology & Laryngology. 2014;123(10):696–700. doi: 10.1177/0003489414532779. [DOI] [PubMed] [Google Scholar]
- 12.Xu Y., Yao J., Zhang Z., Wang W. Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China. European Archives of Oto-Rhino-Laryngology. 2016;273(10):3063–3072. doi: 10.1007/s00405-016-3906-8. [DOI] [PubMed] [Google Scholar]
- 13.Folmer R. L., Griest S. E. Tinnitus and insomnia. American Journal of Otolaryngology-Head and Neck Medicine and Surgery. 2000;21(5):287–293. doi: 10.1053/ajot.2000.9871. [DOI] [PubMed] [Google Scholar]
- 14.Crönlein T., Langguth B., Geisler P., Hajak G. Tinnitus and insomnia. Progress in Brain Research. 2007;166:227–233. doi: 10.1016/S0079-6123(07)66021-X. [DOI] [PubMed] [Google Scholar]
- 15.McCormack A., Edmondson-Jones M., Mellor D., Dawes P., Munro K. J., Moore D. R. Erratum: Association of dietary factors with presence and severity of tinnitus in a middle-aged UK population (PLoS ONE (2015) 9:12 (e114711) DOI: 10.1371/journal.pone.0114711) PLoS ONE. 2015;10(4) doi: 10.1371/journal.pone.0114711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glicksman J. T., Curhan S. G., Curhan G. C. A prospective study of caffeine intake and risk of incident tinnitus. American Journal of Medicine. 2014;127(8):739–743. doi: 10.1016/j.amjmed.2014.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith M. T., Finan P. H., Buenaver L. F., et al. Cognitive-behavioral therapy for insomnia in knee osteoarthritis: a randomized, double-blind, active placebo-controlled clinical trial. Arthritis & Rheumatology. 2015;67(5):1221–1233. doi: 10.1002/art.39048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vitiello M. V., McCurry S. M., Shortreed S. M., et al. Cognitive-behavioral treatment for comorbid insomnia and osteoarthritis pain in primary care: The lifestyles randomized controlled trial. Journal of the American Geriatrics Society. 2013;61(6):947–956. doi: 10.1111/jgs.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vitiello M. V., Rybarczyk B., Von Korff M., Stepanski E. J. Cognitive behavioral therapy for insomnia improves sleep and decreases pain in older adults with co-morbid insomnia and osteoarthritis. Journal of Clinical Sleep Medicine. 2009;5(4):355–362. [PMC free article] [PubMed] [Google Scholar]
- 20.Tonndorf J. The analogy between tinnitus and pain: a suggestion for a physiological basis of chronic tinnitus. Hearing Research. 1987;28(2-3):271–275. doi: 10.1016/0378-5955(87)90054-2. [DOI] [PubMed] [Google Scholar]
- 21.Adami Dehkordi M., Javanbakht M., Sarfarazi Moghadam S., Meshkat M., Abolbashari S. Personality Traits in Patients with Subjective Idiopathic Tinnitus. Iranian Journal of Otorhinolaryngology. 2015;27:369–375. [PMC free article] [PubMed] [Google Scholar]
- 22.Buysse D. J. Sleep health: can we define It? does it matter? SLEEP. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yin Y. S., Qin S. 12 o'clock regimen in the Yellow Emperor. Beijing, China: Chemical Industry Press; 2009. [Google Scholar]
- 24.Meng Z., Zheng Y., Liu S., et al. Reliability and validity of the Chinese (Mandarin) tinnitus handicap inventory. Clinical and Experimental Otorhinolaryngology. 2012;5(1):10–17. doi: 10.3342/ceo.2012.5.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu P., GL Xu., Li M., Cao Z. W., Guo E. Q., et al. Study on reliability and validity of the Tinnitus Evaluation Questionnaire. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2012;47:716–719. [PubMed] [Google Scholar]
- 26.McCombe A., Baguley D., Coles R., McKenna L., McKinney C., Windle-Taylor P. Guidelines for the grading of tinnitus severity: the results of a working group commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999. Clinical Otolaryngology & Allied Sciences. 2001;26(5):388–393. doi: 10.1046/j.1365-2273.2001.00490.x. [DOI] [PubMed] [Google Scholar]
- 27.Newman C. W., Sandridge S. A., Jacobson G. P. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. Journal of the American Academy of Audiology. 1998;9(2):153–160. [PubMed] [Google Scholar]
- 28.Zeman F., Koller M., Figueiredo R., et al. Tinnitus handicap inventory for evaluating treatment effects: which changes are clinically relevant? Otolaryngology—Head and Neck Surgery. 2011;145(2):282–287. doi: 10.1177/0194599811403882. [DOI] [PubMed] [Google Scholar]
- 29.Basile C.-É., Fournier P., Hutchins S., Hébert S. Psychoacoustic assessment to improve tinnitus diagnosis. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0082995.e82995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adamchic I., Langguth B., Hauptmann C., Tass P. A. Psychometric evaluation of visual analog scale for the assessment of chronic tinnitus. American Journal of Audiology. 2012;21(2):215–225. doi: 10.1044/1059-0889(2012/12-0010). [DOI] [PubMed] [Google Scholar]
- 31.Landgrebe M., Zeman F., Koller M., et al. The Tinnitus Research Initiative (TRI) database: a new approach for delineation of tinnitus subtypes and generation of predictors for treatment outcome. BMC Medical Informatics and Decision Making. 2010;10(1, article 42) doi: 10.1186/1472-6947-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sateia M. J. International classification of sleep disorders-third edition: highlights and modifications. CHEST. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 33.Norman G. R., Sloan J. A., Wyrwich K. W. Interpretation of changes in health-related quality of life the remarkable universality of half a standard deviation. Medical Care. 2003;41(5):582–592. doi: 10.1097/00005650-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 35.Hesser H., Bånkestad E., Andersson G. Acceptance of tinnitus as an independent correlate of tinnitus severity. Ear and Hearing. 2015;36(4):e176–e182. doi: 10.1097/AUD.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 36.Hayes S. C., Wilson K. G. Acceptance and Commitment Therapy: Altering the Verbal Support for Experiential Avoidance. The Behavior Analyst. 1994;17(2):289–303. doi: 10.1007/BF03392677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suen L. K. P., Tam W. W. S., Hon K. L. Association of sleep hygiene-related factors and sleep quality among university students in Hong Kong. Hong Kong Medical Journal. 2010;16(3):180–185. [PubMed] [Google Scholar]
- 38.Spielman A. J., Yang C. M., Glovinsky P. B. Insomnia: sleep restriction therapy. London: Informa Healthcare; 2010. Insomnia, sleep restriction therapy: London: Informa Healthcare. [Google Scholar]
- 39.Miller C. B., Espie C. A., Epstein D. R., et al. The evidence base of sleep restriction therapy for treating insomnia disorder. Sleep Medicine Reviews. 2014;18(5):415–424. doi: 10.1016/j.smrv.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 40.Goebel G., Kahl M., Arnold W., Fichter M. 15-year prospective follow-up study of behavioral therapy in a large sample of inpatients with chronic tinnitus. Acta Oto-Laryngologica, Supplement. 2006;(556):70–79. doi: 10.1080/03655230600895267. [DOI] [PubMed] [Google Scholar]
- 41.Baguley D., McFerran D., Hall D. Tinnitus. The Lancet. 2013;382(9904):1600–1607. doi: 10.1016/s0140-6736(13)60142-7. [DOI] [PubMed] [Google Scholar]
- 42.Wan Husain W. S., Zakaria M. N., Othman N. A. N., Othman A., Lih A. C., Zainun Z. The effectiveness of psychological interventions among tinnitus sufferers: A review. Medical Journal of Malaysia. 2015;70(3):188–197. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included within the article.