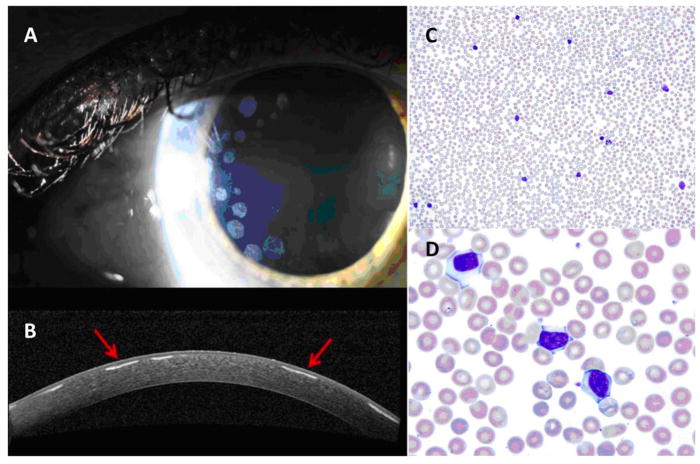
Three years prior to her initial Hematology evaluation, a 53-year-old woman with no significant medical history presented to her local ophthalmologist for a routine eye examination. Slit lamp examination was remarkable for multiple circular anterior stromal deposits with intervening clear spaces, mostly concentrated peripherally (Image 1A,B). Over the course of 3 years, the number of anterior stromal deposits nearly doubled, but they remained outside of the visual axis and the patient maintained excellent visual acuity. After genetic testing excluded an inherited TGFBI corneal dystrophy, she was referred to Hematology for further evaluation.
Image 1.
Slit lamp examination showing multiple, circular, peripherally located anterior corneal stromal deposits (A). Optical coherence tomography of the cornea shows deposits (arrows) with intervening clear spaces (B). Peripheral blood smear at 20× (C) and 100× (D), showing a mild lymphocytosis composed of small- to medium-sized mature lymphocytes with occasional smudge cells.
On initial visit, history and physical examination were unremarkable. Laboratory testing showed a mild, lymphocyte-predominant leukocytosis with a total white blood cell count of 12.4 × 109/L and an absolute lymphocyte count of 7.39 × 109/L. Peripheral blood smear (Image 1C,D) revealed a mild lymphocytosis composed of small- to medium-sized mature lymphocytes with occasional smudge cells. Serum protein electrophoresis/immunofixation electrophoresis revealed a 0.4g/dL IgG kappa paraprotein with normal light chains and immunoglobulins. Peripheral blood flow cytometry demonstrated a CD5+, CD23+, mature B-cell lymphoproliferative disorder. FISH testing and staging CT scans were unremarkable. The diagnosis of Rai stage 0 chronic lymphocytic leukemia with paraproteinemic keratopathy was made.
Corneal immunoglobulin deposition—otherwise known as paraproteinemic or immunotactoid keratopathy—has been described most commonly in the setting of plasma cell dyscrasias, particularly in patients with monoclonal gammopathy of unknown significance and multiple myeloma [1–4]. However, paraproteinemic keratopathy can be associated with any systemic disorder that causes paraproteinemia, including lymphomas, leukemias, and some autoimmune conditions.
Footnotes
Conflict of interest: The authors declare no conflicts of interest.
References
- 1.Garibaldi DC, Gottsch J, de la Cruz Z, et al. Immunotactoid keratopathy: A clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemias. Surv Ophthalmol. 2005;50:61–80. doi: 10.1016/j.survophthal.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Hall RB, Yeung SN, Yenson PR, Moloney G. A series of 4 cases of distinct keratopathy secondary to dysproteinemia: Immunotactoid keratopathy. Can J Ophthalmol. 2014 Aug;49:388–391. doi: 10.1016/j.jcjo.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 3.Lisch W, Saikia P, Pitz S, et al. Chameleon-like appearance of immunotactoid keratopathy. Cornea. 2012 Jan;31:55–58. doi: 10.1097/ICO.0b013e31821ddd0c. [DOI] [PubMed] [Google Scholar]
- 4.Milman T, Kao AA, Chu D, et al. Paraproteinemic keratopathy: The expanding diversity of clinical and pathologic manifestations. Ophthalmology. 2015 Sep;122:1748–1756. doi: 10.1016/j.ophtha.2015.05.029. [DOI] [PubMed] [Google Scholar]