Abstract
Background
Neurocognitive status may be a risk factor for anterior cruciate ligament (ACL) injury. Neurocognitive domains such as visual attention, processing speed/reaction time, and dual-tasking may influence ACL injury risk via alterations to neuromuscular performance during athletic tasks. However, the relationship between neurocognition and performance during athletic tasks is not yet established.
Hypothesis
Athletes with low baseline neurocognitive scores will demonstrate poorer jump landing performance compared with athletes with high baseline neurocognitive score.
Study Design
Controlled laboratory study.
Methods
Neurocognitive performance was measured using the Concussion Resolution Index (CRI). Three-dimensional kinematic and kinetic data of the dominant limb were collected for 37 recreational athletes while performing an unanticipated jump-landing task. Healthy, nonconcussed subjects were screened using a computer-based neurocognitive test into a high performers (HP; n = 20; average CRI percentile, 78th) and a low performers (LP; n = 17; average CRI percentile, 41st) group. The task consisted of a forward jump onto a force plate with an immediate rebound to a second target that was assigned 250 milliseconds before landing on the force plate. Kinematic and kinetic data were obtained during the first jump landing.
Results
The LP group demonstrated significantly altered neuromuscular performance during the landing phase while completing the jump-landing task, including significantly increased peak vertical ground-reaction force (mean ± SD of LP vs HP: 1.81 ± 0.53 vs 1.38 ± 0.37 body weight [BW]; P <.01), peak anterior tibial shear force (0.91 ± 0.17 vs 0.72 ± 0.22 BW; P <.01), knee abduction moment (0.47 ± 0.56 vs 0.03 ± 0.64 BW × body height; P = .03), and knee abduction angle (6.1° ± 4.7° vs 1.3° ± 5.6°; P = .03), as well as decreased trunk flexion angle (9.6° ± 9.6° vs 16.4° ± 11.2°; P <.01).
Conclusion
Healthy athletes with lower baseline neurocognitive performance generate knee kinematic and kinetic patterns that are linked to ACL injury.
Clinical Relevance
Neurocognitive testing using the CRI may be useful for identification of athletes at elevated risk for future ACL injury.
Keywords: ACL, biomechanics, motion analysis, injury prevention
Despite the rapid emergence of injury prevention programs, anterior cruciate ligament (ACL) injury rates remain high.1,15,17,20 This may be due in part to the slow adoption of ACL injury prevention interventions among sports programs. Barriers to the adoption of such interventions may include limitations on the time needed for the intervention and the protocol duration and adherence needed for efficacy.16,24 The use of a more targeted approach via neuromuscular-based screening protocols for athletes at highest risk may help improve the efficiency of implementation of these injury prevention programs, but these screening methods currently lack solid evidence in the literature of efficacy in accurately identifying those at high risk for injury.7,26
While affecting alterations in neuromuscular performance remains a promising method to reduce injury risk, maintaining such a focused paradigm may not allow for the consideration of complementary novel approaches to current ACL injury risk identification and prevention models that may increase efficacy and efficiency. The use of neurocognitive performance may represent such a novel approach. Neurocognition refers to cognitive processes and abilities associated with the functioning of cortical and subcortical brain systems. While it is inclusive of domains such as language, intelligence, and social functioning that may not be germane to injury risk, aspects such as visual attention, self-monitoring, agility/fine motor performance, processing speed/reaction time, and dual-tasking may influence injury risk. Limited evidence indicates that poor neurocognitive performance is associated with an elevated risk of ACL injury.11,28 This finding has since been supported by a small number of studies demonstrating a higher risk of lower extremity injury with poorer performance on a reaction time test30 and after temporary alteration of normal neurocognitive performance, such as with a concussion.8,19,22 The mechanisms by which neurocognition affects injury risk are not known but may exert an effect on neuromuscular performance. For example, athletes who have experienced a recent concussion demonstrated altered gait patterns during a dual-attention task, even after the point of return to play.14,23 However, the relationship between baseline neurocognition and complex neuromuscular tasks that would potentially be imposed during athletic competition, such as jump landing, in healthy, active people is not yet known.
The purpose of this study was to determine if differences in neuromuscular performance during a challenging athletic task exist between athletes with high versus low baseline neurocognitive performance. We hypothesized that athletes with low baseline neurocognitive scores would demonstrate knee kinematic and kinetic patterns associated with elevated ACL injury risk during an unanticipated jump-landing task compared with those with high neurocognitive scores.
METHODS
Participants
Subjects were recruited to complete a screening test to determine eligibility. The subjects included recreational athletes (age, 18–30 years) who (1) participate in jumping/cutting sports (eg, basketball, soccer, volleyball, lacrosse) at least 3 times a week or (2) participate in these sports at least once a month and previously participated at the high school varsity or collegiate club levels. Participants were excluded if they (1) did not meet the age criteria; (2) did not meet the activity level criteria (ie, recreational athlete); (3) had a lower extremity injury that prevented participation in physical activity for longer than 2 weeks over the previous 6 months; (4) possessed cardiovascular, respiratory, neurological, or other conditions that prevented them from participating at maximal effort in sports activities; or (5) had suffered a concussion within the past year. Participants were recruited from the general student population at the University of Virginia. Subjects who completed the study in its entirety were provided with $50 in compensation for their time, and no compensation was provided for subjects who completed the neurocognitive screening test but did not fit inclusion criteria for the remainder of the study. The study was approved by the University of Virginia’s institutional review board. Written consent was obtained from each participant before data collection.
Neurocognitive Screening Test
Neurocognitive testing was performed using the computer-based Concussion Resolution Index (CRI).5,6 The CRI neurocognitive test includes 6 subtest domains:
The Reaction Time subtest consists of a series of geometric shapes on the screen presented at a rate of 1 image per 2250 milliseconds. Individuals are instructed to press the space bar as quickly as possible upon seeing a white circle. Scoring reflects reaction time and false-positive and false-negative errors.
The Cued Reaction Time subtest also presents a series of geometric shapes on the screen at a rate of 1 image per 2250 milliseconds. Individuals are instructed to press the space bar as quickly as possible upon seeing a white circle that immediately follows a black square. Scoring reflects reaction time and false-positive and false-negative errors.
The Animal Decoding subtest presents a key that pairs animals with numbers at the top of the screen. Animals are subsequently presented with empty boxes beneath. On the basis of the legend, individuals must enter the appropriate number into each empty box as quickly as possible using the number keys. Scoring is based on the number of correct responses.
The Visual Recognition 1 subtest presents a series of 60 pictures on the screen at a rate of 3 seconds each. Individuals are instructed to press the space bar upon seeing a picture for a second time. Scoring reflects reaction latency and false-positive and false-negative errors.
The Visual Recognition 2 subtest presents a series of 60 pictures at a rate of 3 seconds each. Twenty items are reproduced from Visual Recognition 1. Individuals are instructed to press the space bar upon recognizing a picture from Visual Recognition 1. Scoring reflects reaction latency and false-positive and false-negative errors.
The Symbol Scanning subtest presents a pair of shapes on the left side of the screen. Eight shapes appear on the right. Individuals must indicate whether one or both of the shapes on the left appear among those on the right, and respond by pressing the number 1 or number 2 key. Scoring is based on speed of response in seconds.
Three indices are created from these subtests, including Simple Reaction Time (composed from the Reaction Time and Cued Reaction Time subtests), Complex Reaction Time (composed from the Visual Recognition 1 and 2 sub-tests), and Processing Speed (composed from the Animal Decoding and Symbol Scanning subtests).
Subjects scoring above the 80th percentile in 1 score and with 2 scores no lower than 60th percentile were included in a higher performers (HP) group. Subjects with 1 subtest score below the 40th percentile and with 2 scores no higher than the 70th percentile, or with at least 2 scores below the 30th percentile, were included in the low performers (LP) group. To prevent any testing bias, the subjects were not informed of the basis, inclusion criteria, or existence of the 2 different study groups, and they were instructed to complete the test to the best of their abilities. The goal enrollment in each group was 20 subjects with an even distribution between male and female subjects to minimize any effects based on sex.
The Unanticipated Jump-Landing Task
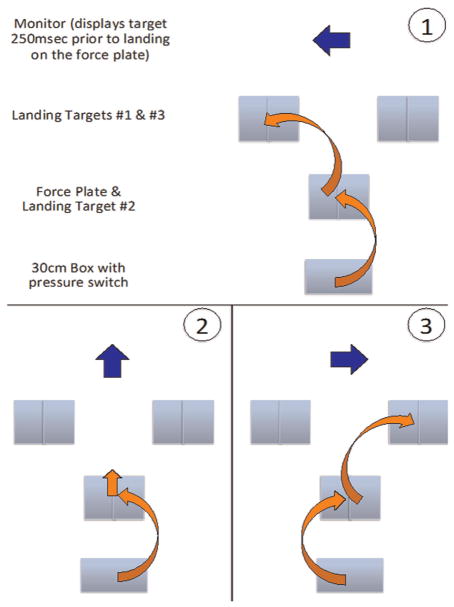
The subjects who qualified for either of these 2 groups were then scheduled for a subsequent data collection session. The subjects were instructed to dress in athletic shorts, sports bra (for female subjects), and the athletic shoes they normally wear when engaging in sports activities. Upon presentation to the laboratory, subjects were instructed regarding the jump-landing task. A 30-cm-tall box was placed at a distance measuring one-half of the subject’s height away from the front edge of a force plate. This force plate served as the initial landing target for the subject’s dominant limb, defined as the leg the subject would prefer to use to kick a soccer ball for maximum distance. A landing target for the non-dominant limb was outlined in the same dimensions as those of the force plate, immediately adjacent to the force plate. The subject was instructed to (1) stand on the box, (2) jump forward off the box with both feet, (3) land on the target as described above, and (4) jump at maximum effort to a second target once he or she hit the initial target (Figure 1).
Figure 1.
Jump-landing task. Reproduced with permission from Padua DA, Marshall SW, Boling MC, et al. The landing error scoring system (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: The JUMP-ACL study. Am J Sports Med. 2009;37(10):1996–2002.
The location of the second landing target was governed by the activation of an explicit directional stimulus. A pressure sensor was placed under the subject’s dominant foot when standing on the 30-cm box. Once the subject jumped from the box, thus relieving pressure from the sensor, a customized Labview program (National Instruments) was activated. The program was timed to randomly display 1 of 3 arrows on a monitor indicating the second landing target at 250 milliseconds before the initial landing. This duration was selected based on the previous literature employing similar unanticipated tasks.2 Subjects were allowed up to 3 practice trials per landing location, each in a fully anticipated landing condition (ie, the landing location was predetermined before the jump).
The monitor was placed at approximately waist level 3 m forward of the initial landing target. The monitor would display arrows corresponding to (1) a secondary landing target 1 m forward and left of the initial landing target at a 45° angle (left-pointing arrow), (2) the initial landing target (vertical arrow), and (3) a secondary landing target 1 m forward and right of the initial landing target at a 45° angle (right-pointing arrow) (Figure 2). The locations of the secondary landing targets were selected to add an unanticipated component to both frontal plane motion (ie, jumping to the left, right, or center) and sagittal plane motion demands (ie, jumping forward as in the case of the left or right arrows, or jumping straight up and down and landing back on the force plates in the case of the vertical arrow). The subject was instructed to land on the initial target (which included the force plate) and to then complete the task by immediately jumping at maximum effort to land on the second target as indicated on the monitor. The left and right secondary landing targets were outlined on the ground with the same size specifications as those of the initial landing target (ie, 1 target for each foot, each the same size as the force plate). The subject completed 5 successful jump landings for each secondary landing target. After completion of all 15 jump landings, the subject’s participation in the study ended.
Figure 2.
Unanticipated jump-landing task schematic. The monitor displayed the location of the second jump 250 milliseconds before the initial landing as (1) forward and left, (2) straight up on the force plate, or (3) forward and right.
Kinematic and Kinetic Data Collection
Before completing the unanticipated jump-landing task, 16 retro-reflective markers were placed over the following anatomic landmarks of the trunk, pelvis, and lower extremity: C7 and T4 spinous process, the sternal notch, the bilateral anterior and posterior superior iliac spines, lateral mid-thighs, lateral femoral condyles, lateral midshanks, lateral malleoli, second metatarsal heads, and heels. A cluster of 4 markers was placed on the sacrum and secured with an elastic self-adhesive wrap. The markers placed on the heels and second metatarsal heads were placed on the shoe over the anatomic landmarks located via palpation.
The 3-dimensional positions of each marker were captured at 250 Hz by the use of a 10-camera Vicon 624 motion analysis system (Vicon Peak). Ground-reaction force data were obtained at 1000 Hz from a force plate (AMTI) in synchrony with the motion-capture data. Force plate data were low-pass filtered at 30 Hz by the use of a second-order Butterworth filter before being down sampled and combined with the motion-capture data.
Joint resultant forces and moments at the knee on the tibia were calculated on the dominant limb side through a full inverse-dynamic model implemented by the use of Vicon Plug-in Gait. The estimated joint resultant forces were normalized to the participant’s body weight, and moments were normalized to the product of the participant’s body weight and height. Joint moments are reported as external torques.
The landing was defined as the first time at which the vertical ground-reaction force increased to greater than 5% of the participant’s weight. The takeoff was defined as the first time at which the vertical ground-reaction force decreased to less than 5% of the participant’s weight after landing.
Peak vertical ground-reaction force and peak proximal anterior tibial shear force were sampled during the landing phase. The following remaining variables were sampled at the point of the peak proximal tibial anterior shear force during the landing phase: knee adduction-abduction moment, knee flexion and adduction-abduction joint angles, hip flexion and adduction-abduction joint angles, and the trunk flexion and lateral bending angles. Data from the middle 3 trials of the 5 successful trials using only the task condition with landing target 2 (ie, straight up and down on the force plate) were averaged for each subject.
Data Analysis
An a priori power analysis demonstrated that a sample size of 28 subjects (14 in each group) would provide 95% confidence and 80% power to determine differences in knee abduction moment, knee abduction angle, and knee flexion angle as statistically significant using values derived from Weinhandl et al.29 A goal of 40 subjects was set to account for dropouts. Statistical analysis was completed using analyses of variance with an α level of .05.
RESULTS
A total of 123 subjects were screened using the CRI. Both the HP and LP groups achieved target enrollment (n = 20 for each group; 10 male, 10 female). There were 3 subjects in the LP group who did not report for their subsequent laboratory session, leaving a final LP group size of 17 participants (8 male, 9 female). The remaining subjects who did not qualify for inclusion into 1 of these 2 groups were then excluded from completing the remainder of the study. There were no significant differences between groups in age, height, or weight (P > .05) (Table 1). All subjects qualified for inclusion into the study under the activity criteria of former high school varsity athletes who participate in landing/cutting sports at least once a month; there were no subjects with a history of participation in landing/cutting sports at the club level.
TABLE 1.
Subject Characteristicsa
| Characteristic | HP Group | LP Group | P Value |
|---|---|---|---|
| Height, m | 1.73 ± 0.07 | 1.71 ± 0.12 | .713 |
| Mass, kg | 68.68 ± 9.26 | 70.11 ± 10.12 | .654 |
| Age, y | 21.05 ± 1.54 | 20.81 ± 1.68 | .813 |
Data are reported as mean ± SD. HP, higher performers; LP, low performers.
The LP group demonstrated significantly lower CRI scores in all subtest domains compared with the HP group (P < .01) (Table 2). A much smaller magnitude difference between the 2 groups was noted for the Processing Speed subtest, in which the HP and LP groups were separated by an average of 20.3 percentile, compared with average differences of 42.6 and 47.1 percentiles for Simple Reaction Time and Complex Reaction Time, respectively.
TABLE 2.
Neurocognitive Testing Resultsa
| CRI Subtest | HP Group | LP Group | P Value |
|---|---|---|---|
| Simple Reaction Time (percentile) | 67.1 ± 9.1 | 24.5 ± 14.3 | <.01b |
| Complex Reaction Time (percentile) | 80.6 ± 9.5 | 33.5 ± 15.9 | <.01b |
| Processing Speed (percentile) | 85.8 ± 7.2 | 65.5 ± 16.1 | <.01b |
Data are reported as mean ± SD. CRI, Concussion Resolution Index; HP, higher performers; LP, low performers.
Statistically significant difference between groups.
Regarding jump-landing performance, the LP group demonstrated significantly altered neuromuscular performance during the landing phase while completing the jump-landing task. This included on average 31% higher peak vertical ground-reaction force and 26% higher peak proximal anterior tibial shear force (Table 3). Average differences in knee abduction moments were particularly noteworthy, as the mean value for the LP group was high both in comparison to the HP group and to that of previous investigations studying high-risk groups using similar data reduction approaches.3,9,10 For the kinematic measure, higher values were noted for the LP group in knee abduction angle with a mean difference between the groups of 4.8°, while trunk flexion angle was lower in comparison to the HP group with a mean difference between the groups of 6.8° (Table 3).
TABLE 3.
Jump-Landing Test Resultsa
| HP Group | LP Group | P Value | |
|---|---|---|---|
| Kinetics results | |||
| Peak vertical ground-reaction force (BW) | 1.38 ± 0.37 | 1.81 ± 0.53 | <.01b |
| Peak anterior shear force (BW) | 0.72 ± 0.22 | 0.91 ± 0.17 | <.01b |
| Knee abduction moment (BW 3 BH) | 0.03 ± 0.64 | 0.47 ± 0.56 | .03b |
| Kinematics results, deg | |||
| Knee abduction angle | 1.3 ± 5.6 | 6.1 ± 4.7 | .03b |
| Knee flexion angle | 24.8 ± 6.3 | 27.8 ± 4.4 | .15 |
| Trunk lateral bending angle | 1.1 ± 1.5 | 0.7 ± 0.7 | .26 |
| Trunk flexion angle | 16.4 ± 11.2 | 9.6 ± 9.6 | <.01b |
Data are reported as mean ± SD. BH, body height; BW, body weight; HP, higher performers; LP, low performers.
Statistically significant difference between groups.
DISCUSSION
To the best of our knowledge, this is the first study to explore the relationship between baseline neurocognition and neuromuscular performance in athletes during an athletic task intended to mimic an in-game challenge. The findings of differences between high and low neurocognitive performers in kinetic and kinematic measures largely confirm the study hypothesis; while no differences were observed in knee flexion or trunk lateral bending angles, the remainder of the kinematic variables and all of the kinetic variables demonstrated directional differences matching that of the study hypothesis.
The neuromuscular performance differences observed in LP athletes are consistent with elevated risk for experiencing an ACL injury. These most notably include knee abduction angle and moment, which have been demonstrated as having predictive capacity for ACL injury in high school female athletes.12 Other study variables have been repeatedly demonstrated as being altered in populations at high risk for ACL injury.4,27 These findings provide mechanistic support to prior studies that have demonstrated an increased risk of injury with poorer levels of baseline neurocognitive performance and those that have demonstrated an increased risk of injury after experiencing altered neurocognitive states (eg, after concussion).22,28,30
When considering the aspects of neurocognition that are most likely related to athletic performance, the relationship between neurocognition and neuromuscular performance may be mediated through aspects such as visual attention, self-monitoring, fine motor performance, reaction time, and dual-tasking.11 These neurocognitive dimensions are likely critical for the performance and safety of athletes as they attempt to initiate and maintain appropriate neuromuscular responses to the demands of dynamic activities in a constantly evolving competitive environment. For example, quick reaction times may allow the athlete to rapidly adjust to new demands during play while maximizing performance. Conversely, poor reaction times may reduce the athlete’s ability to react to evolving demands during competition in an adequate time frame to allow for a safe and appropriate response. Similarly, an athlete who is poor at dual-tasking may not be able to appropriately monitor the neuromuscular performance associated with the athletic task while at the same time devoting visual attention to an opponent. Thus, an athlete with low neurocognitive performance may be hindered in his or her ability to plan, time, perform, and/or monitor neuromuscular performance during athletic tasks.11
The implications of these findings for ACL injury risk evaluation and injury prevention and rehabilitation have the potential to be profound. Improving our understanding of the relationship between these domains may result in an enhanced capability to engage in preactivity injury risk stratification via use of standard neurocognitive screening tools that are gaining widespread popularity among competitive sports from high school to the professional levels. Athletes who compete in sports that feature contact (including football, soccer, basketball, and lacrosse) commonly complete pre-season baseline testing of neurocognitive performance for use in concussion injury diagnosis and return-to-play decision making. It is noteworthy that there is significant overlap between these sports and those with the highest rates of ACL injury13 (Figure 3). With the possible exceptions of men’s baseball and women’s softball and volleyball, the sports listed in Figure 3 commonly use preseason neurocognitive testing at the collegiate level, with increasing levels of testing in these sports at the high school level.
Figure 3.
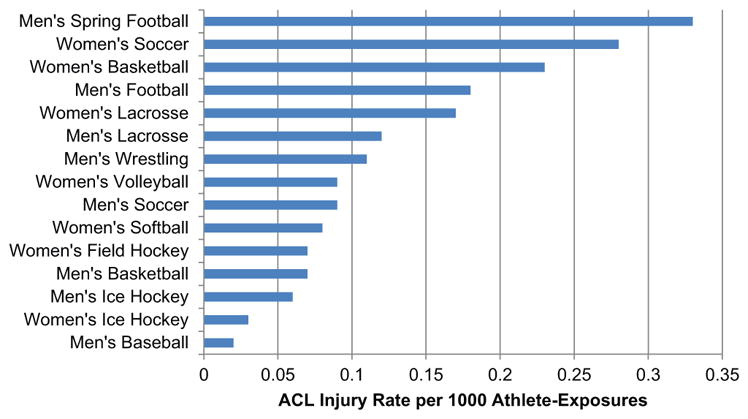
Rates of anterior cruciate ligament injuries in collegiate athletics. Adapted from Hootman et al.13
Given the rates of use of preseason neurocognitive testing, it may be possible to use this information to better inform injury risk assessment models. Improvements to injury risk assessment models are currently a significant need; while those athletes at greatest risk of injury appear to demonstrate greater responses to ACL injury prevention training, easy and accurate identification of such athletes using neuromuscular-based clinical assessment tools such as the Landing Error Scoring System has been elusive.7,26 The results of this study may serve to supplement such models in 2 ways: first, by helping to establish neurocognitive performance as a valid measure for use in identifying athletes at risk for injury and, second, to recommend that future iterations of neuromuscular screening tools incorporate more challenging tasks (eg, a dual-attention task such as used in this study) during assessment. The benefits of using aspects such as dual-attention during clinical assessment are currently being realized in concussion assessment and management,18 and it is logical that this strategy can be successfully co-opted into ACL injury risk screening.
The results of this study may have further utility in the areas of ACL injury prevention training and ACL injury rehabilitation. Given the paradigm of the relationship between neurocognition and neuromuscular performance as described above, it stands to reason that prevention and rehabilitation efforts should also incorporate aspects of neurocognition. Programs may be modified such that athletes at more advanced stages of a given injury prevention or rehabilitation program are to practice tasks with challenges in neurocognitive domains such as dual-tasking, visual attention, and reaction time.
This investigation is not without its limitations. This study employed a single computerized test of neurocognition, and while this was used with an eye toward clinical application, the 3 indices of the CRI are representative of a broader range of neurocognitive domains. This limits our understanding of the relationship between neurocognition and neuromuscular performance that was seen with our results. Although the CRI was selected due to the increasing clinical use of computer-based neurocognitive screening in sports, thus potentially magnifying the clinical effect of the findings, use of more extensive and in-depth neurocognitive testing protocols may allow for a better understanding of the effects of specific domains of neurocognitive performance. The neurocognitive performance definitions for inclusion into each group were also relatively broad, and a more restrictive definition of low and high performers may have provided additional clarity to the neuromuscular differences between these groups; however, we note that increasing the amount of separation between the neurocognitive inclusion criteria for the 2 groups would likely act to strengthen the findings of this study. As the study was performed in a college-aged recreational athlete population, the magnitude and nature of the relationship between neurocognition and neuromuscular performance may differ significantly depending on the level of skill and maturation of the athlete. We did not control for the specific shoe and age of the shoe used by the subjects during testing, which may have an effect on landing characteristics.25 Finally, the accuracy of the variables assessed in this study may be limited by aspects such as soft tissue artifacts during the landing phase.21
Future research is needed to determine which neurocognitive tests and domains are the most critical for predicting and reducing injury risk; how the relative importance of such tests may change depending on athlete maturation, gender, or sport; and how to best integrate neurocognitive assessment and aspects of training into widespread practice.
CONCLUSION
Athletes with low levels of baseline neurocognitive performance demonstrate poor neuromuscular performance during landing relative to athletes with high levels of baseline neurocognitive performance such that they may be at elevated risk of injury. These results may serve to inform ACL injury risk screening, prevention, and rehabilitation strategies.
Footnotes
Presented at the 41st annual meeting of the AOSSM, Orlando, Florida, July 2015.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by the National Institutes of Health (Grant 5K12HD001097-18), the Foundation for Physical Medicine and Rehabilitation, and Shape America.
References
- 1.Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806–1812. doi: 10.1177/0363546514540862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown TN, Palmieri-Smith RM, McLean SG. Sex and limb differences in hip and knee kinematics and kinetics during anticipated and unanticipated jump landings: implications for anterior cruciate ligament injury. Br J Sports Med. 2009;43(13):1049–1056. doi: 10.1136/bjsm.2008.055954. [DOI] [PubMed] [Google Scholar]
- 3.Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 4.Dai B, Herman D, Liu H, Garrett WE, Yu B. Prevention of ACL injury, part I: injury characteristics, risk factors, and loading mechanism. Res Sports Med. 2012;20(3–4):180–197. doi: 10.1080/15438627.2012.680990. [DOI] [PubMed] [Google Scholar]
- 5.Erlanger D, Feldman D, Kutner K, et al. Development and validation of a web-based neuropsychological test protocol for sports-related return-to-play decision-making. Arch Clin Neuropsychol. 2003;18(3):293–316. [PubMed] [Google Scholar]
- 6.Erlanger D, Saliba E, Barth J, Almquist J, Webright W, Freeman J. Monitoring resolution of postconcussion symptoms in athletes: preliminary results of a web-based neuropsychological test protocol. J Athl Train. 2001;36(3):280–287. [PMC free article] [PubMed] [Google Scholar]
- 7.Goetschius J, Smith HC, Vacek PM, et al. Application of a clinic-based algorithm as a tool to identify female athletes at risk for anterior cruciate ligament injury: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2012;40(9):1978–1984. doi: 10.1177/0363546512456972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herman DC, Jones D, Harrison A, et al. Concussion may increase the risk of subsequent lower extremity musculoskeletal injury in collegiate athletes. Sports Med. doi: 10.1007/s40279-016-0607-9. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herman DC, Onate JA, Weinhold PS, et al. The effects of feedback with and without strength training on lower extremity biomechanics. Am J Sports Med. 2009;37(7):1301–1308. doi: 10.1177/0363546509332253. [DOI] [PubMed] [Google Scholar]
- 10.Herman DC, Weinhold PS, Guskiewicz KM, Garrett WE, Yu B, Padua DA. The effects of strength training on the lower extremity biomechanics of female recreational athletes during a stop-jump task. Am J Sports Med. 2008;36(4):733–740. doi: 10.1177/0363546507311602. [DOI] [PubMed] [Google Scholar]
- 11.Herman DC, Zaremski JL, Vincent HK, Vincent KR. Effect of neurocognition and concussion on musculoskeletal injury risk. Curr Sports Med Rep. 2015;14(3):194–199. doi: 10.1249/JSR.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 13.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 14.Howell DR, Osternig LR, Chou LS. Dual-task effect on gait balance control in adolescents with concussion. Arch Phys Med Rehabil. 2013;94(8):1513–1520. doi: 10.1016/j.apmr.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 15.Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. doi: 10.4085/1062-6050-48.6.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joy EA, Taylor JR, Novak MA, Chen M, Fink BP, Porucznik CA. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J Strength Cond Res. 2013;27(8):2263–2269. doi: 10.1519/JSC.0b013e31827ef12e. [DOI] [PubMed] [Google Scholar]
- 17.Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. doi: 10.1177/0363546514524164. [DOI] [PubMed] [Google Scholar]
- 18.Lee H, Sullivan SJ, Schneiders AG. The use of the dual-task paradigm in detecting gait performance deficits following a sports-related concussion: a systematic review and meta-analysis. J Sci Med Sport. 2013;16(1):2–7. doi: 10.1016/j.jsams.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Lynall RC, Mauntel TC, Padua DA, Mihalik JP. Acute lower extremity injury rates increase following concussion in college athletes. Med Sci Sports Exerc. 2015;47(12):2487–2492. doi: 10.1249/MSS.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 20.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 21.Miranda DL, Rainbow MJ, Crisco JJ, Fleming BC. Kinematic differences between optical motion capture and biplanar videoradiography during a jump-cut maneuver. J Biomech. 2013;46(3):567–573. doi: 10.1016/j.jbiomech.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nordstrom A, Nordstrom P, Ekstrand J. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br J Sports Med. 2014;48(19):1447–1450. doi: 10.1136/bjsports-2013-093406. [DOI] [PubMed] [Google Scholar]
- 23.Parker TM, Osternig LR, Van Donkelaar P, Chou LS. Gait stability following concussion. Med Sci Sports Exerc. 2006;38(6):1032–1040. doi: 10.1249/01.mss.0000222828.56982.a4. [DOI] [PubMed] [Google Scholar]
- 24.Saunders N, Otago L, Romiti M, Donaldson A, White P, Finch C. Coaches’ perspectives on implementing an evidence-informed injury prevention programme in junior community netball. Br J Sports Med. 2010;44(15):1128–1132. doi: 10.1136/bjsm.2009.069039. [DOI] [PubMed] [Google Scholar]
- 25.Shultz SJ, Schmitz RJ, Tritsch AJ, Montgomery MM. Methodological considerations of task and shoe wear on joint energetics during landing. J Electromyogr Kinesiol. 2012;22(1):124–130. doi: 10.1016/j.jelekin.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40(3):521–526. doi: 10.1177/0363546511429776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature, part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69–78. doi: 10.1177/1941738111428281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swanik CB, Covassin T, Stearne DJ, Schatz P. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med. 2007;35(6):943–948. doi: 10.1177/0363546507299532. [DOI] [PubMed] [Google Scholar]
- 29.Weinhandl JT, Joshi M, O’Connor KM. Gender comparisons between unilateral and bilateral landings. J Appl Biomech. 2010;26(4):444–453. doi: 10.1123/jab.26.4.444. [DOI] [PubMed] [Google Scholar]
- 30.Wilkerson G. Neurocognitive reaction time predicts lower extremity sprains and strains. Int J Athl Ther Train. 2012;17(6):4–9. [Google Scholar]