SUMMARY
In Botswana, where one quarter of the adult population is infected with the human immunodeficiency virus and the annual tuberculosis (TB) incidence is among the highest globally, intensified TB case finding is needed in health care facilities to detect and treat TB cases early and prevent transmission. During August-December 2009, TB screening was implemented among adults at patient intake in five clinics in Francistown. Among 11 779 TB screenings at intake, 926 were positive. Nineteen patients were diagnosed with TB. Routine TB screening at intake was operationally feasible, but had low yield. Innovative case-finding strategies are needed in Botswana.
Keywords: tuberculosis, Botswana, HIV/AIDS, intensified case finding
RÉSUMÉ
Au Botswana, où un quart des adultes sont infectés par le virus de l’immunodéficience humaine et où l’incidence annuelle de la tuberculose (TB) se situe parmi les plus élevées du monde, un dépistage intensifié des cas de TB s’impose dans les services de soins de santé afin de détecter et de traiter précocement les cas de TB et de prévenir sa transmission. Au cours de la période août-décembre 2009, on a mis en œuvre un dépistage de la TB chez les adultes à l’admission dans cinq dispensaires de Francistown. Parmi les 11 779 dépistages de TB à l’ad-mission, 926 ont été positifs. On a diagnostiqué la TB chez 19 patients. Le dépistage de routine de la TB lors de l’admission est opérationnellement réalisable, mais ne permet qu’un rendement minime. Des stratégies innovantes de dépistage des cas s’imposent au Botswana.
RESUMEN
En Botsuana, donde un cuarto de la población adulta padece de la infección por el virus de la inmunodeficiencia humana, se observa una incidencia anual de tuberculosis (TB) de las más altas del mundo. Es preciso intensificar la búsqueda de casos en los centros de atención sanitaria, con el fin de detectar y tratar en forma temprana los casos de TB y evitar la transmisión de la enfermedad. Entre agosto y diciembre del 2009 se introdujo una forma de detección sistemática de la TB en los adultos, en el momento de su recepción en cinco consultorios generales de Francistown. Se practicaron 11 779 detecciones sistematicás y se obtuvieron 926 resultados positivos. Se estableció el diagnostico de TB en 19 pacientes. La detección sistemática de la TB en el momento de la admisión al consultorio fue operativamente factible, pero ofreció un bajo rendimiento diagnóstico. Es preciso encontrar estrategias innovadoras de busqueda de casos de TB en Botsuana.
BOTSWANA has one of the highest tuberculosis (TB) incidence rates worldwide,1 and an estimated 24% of adults aged 15–49 years are human immunodeficiency virus (HIV) infected nationally.2 In 2010, approximately 70% of TB patients in Botswana were HIV-infected.3
The World Health Organization (WHO) recommends screening for TB signs and symptoms in settings where persons living with HIV/acquired immunedeficiency syndrome (PLWHA) are concentrated.4 In Botswana, public medical clinics are integrated service delivery settings providing many health services. Individuals with undiagnosed and potentially infectious TB are often seen in these settings, where PLWHA, pregnant women and children also receive care. To date, few clinics have implemented routine TB screening. Current strategies to prevent transmission in clinical settings rely heavily on passive case finding. To more quickly identify patients with TB signs and symptoms, provide prompt diagnosis and treatment, and reduce transmission, additional active TB case-finding strategies are needed.
ASPECT OF INTEREST
A TB symptom checklist was piloted in five general medical clinics in Francistown, Botswana, from August to December 2009 to assess the feasibility and yield (i.e., number of TB cases identified) of routine TB screening among adult patients during clinic visits. Clinics with varying patient loads and staffing patterns were chosen to ensure the availability of adequate staff to perform both project activities and regular duties during the study period.
In Botswana clinics, patients are seen by an intake nurse to assess vital signs (e.g., weight, blood pressure) while waiting for consultation with a doctor or nurse. The TB checklist was implemented as part of the routine intake assessment. Staff asked consenting patients aged ⩾ 18 years if they currently had any of the following: cough for ⩾2 weeks, fever, night sweats, unexplained weight loss, coughing with blood, enlarged lymph nodes, history of TB or contact with a person with TB disease. Patients with a positive TB screen (cough for ⩾2 weeks or any combination of 2–8 other signs, symptoms or risk factors) were flagged for further clinical evaluation for TB as part of their routine consultation. An individual could have been screened more than once at different points in time during the study period. For patients with cough, basic infection control practices (i.e., instruction on cough etiquette) were implemented. To standardize implementation, clinic staff were trained to use the checklist, and weekly supervisory visits to clinics were conducted. National guidelines on TB referral for diagnosis and treatment were reviewed.5 Patients determined to be TB suspects based on the clinician’s evaluation were then tracked through the routine system to determine if TB diagnostics (sputum smear microscopy and/or chest radiograph [CXR]) had been ordered, and if they had been started on TB treatment. For TB patients, routine HIV testing was offered per national guidelines; otherwise HIV status was self-reported or based on patient records.
The average time to complete intake screening questions was measured. Screening tool data and program records were analyzed using descriptive statistics.
Ethical review was conducted by the Botswana Ministry of Health Institutional Review Board and by the US Centers for Disease Control and Prevention (CDC), which designated the project a disease control activity, and not human subjects research.
The TB screening questions added on average 22 seconds to intake procedures. A total of 11 779 subjects were screened for TB using the checklist, of which the majority were female (n = 9146, 78%); the average age was 33 years. The three most common reasons for visiting the clinic were illness without cough (55%), antenatal care or prevention of maternal-to-child HIV transmission (22%) and illness with cough (9%). There were 926 (8%) positive TB screens, and 783 (85%) patients received further clinical examination by a medical provider for TB, of whom 328 (42%) had HIV infection; 110 (34%) HIV-infected patients were currently on antiretroviral therapy (ART). HIV status was unknown for almost one third of the patients (n = 238). Based on clinical examination, 456 (58%) patients were determined not to have TB, while among patients referred for further evaluation 327 (42%) were referred for CXR and/or sputum examination; 141 (43%) returned for either examination and 186 (57%) did not.
Nineteen patients were diagnosed with TB, as determined by a medical provider, based on clinical ex-amination, CXR and smear results. Of these, 17 (89%) had pulmonary disease and the remaining two (11%) had extra-pulmonary disease. Ten (53%) were male, 14 (74%) were HIV-positive, and two (11%) had unknown HIV status. TB patients most commonly reported cough for ⩾2 weeks (n = 14, 74%), night sweats (n = 12, 63%) and fever (n = 9, 47%) during TB screening. We also assessed patients screened for TB by primary reason for visit (Figure). Among the 19 patients diagnosed with TB, 14 were among 1009 patients who reported primarily visiting the clinic for an illness with cough, 4 were among 10 563 who attended for other reasons, and 1 was among 207 for whom the reason was unknown.
DISCUSSION
We incorporated universal TB screening into routine clinic activities in Francistown to assess its feasibility and yield. Given the high annual TB incidence rate in Botswana, and in comparison to TB screening among HIV-positive and HIV-negative persons in other settings,6–8 the number of TB cases identified in this study was low. The low yield of TB cases may have been partially due to the substantial loss to followup noted at every step of the screening and diagnostic processes. Less than half of patients referred for further TB diagnostic tests as part of routine care returned to complete them, which may have been in part due to the additional clinic visits required for sputum collection and referral to hospital for radiograph. Such a significant attrition rate among TB suspects has important implications for community TB transmission. Further operational research is needed to understand attrition factors, and systems should be established to ensure symptomatic patients undergo complete diagnostic evaluation.
The yield of TB screening depends on the screening strategy and the population being screened.9 We may have had a lower yield because the general population was screened, and not just individuals at high risk for TB, and our screening strategy may have a lower sensitivity for detecting TB cases. Targeting only symptomatic persons for additional evaluation, and in particular requiring a chronic cough or multiple symptoms for a positive screen, have been shown to be insensitive screening methods in PLWHA.6 In addition, smear microscopy and CXR have been shown to be insufficiently sensitive to diagnose TB in PLWHA.6 Implementation of new technologies, such as the Xpert® TB/RIF assay (Cepheid, Sunnyvale, CA, USA), may help increase sensitivity and re-duce the diagnostic drop-out among PLWHA who report TB symptoms.10
CONCLUSION
Despite the low overall yield, routine TB screening in medical clinics was operationally feasible. Implementing more sensitive TB screening tools, ensuring follow-up for TB-specific diagnostic processes and expanding TB screening to HIV clinics may increase usefulness. Given the high rates of TB and HIV, innovative, accepted and inexpensive strategies are needed for TB case finding in Botswana.
Figure.
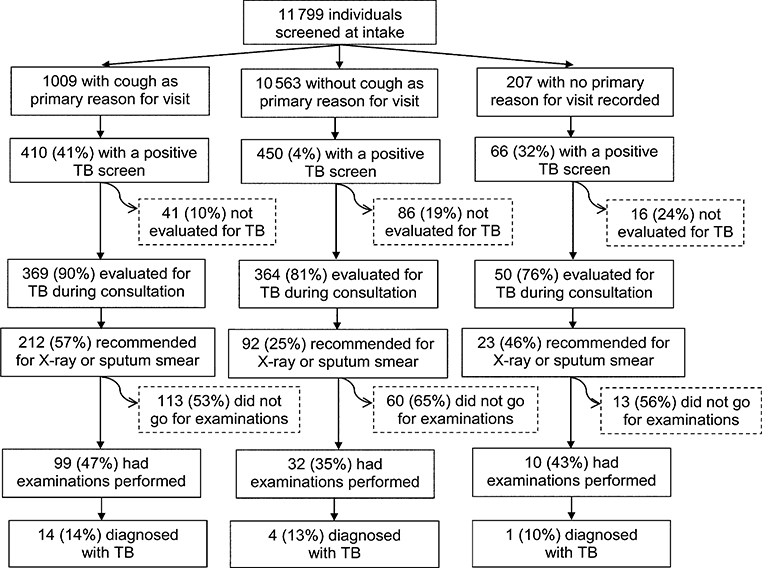
Primary reason for visit and results of TB screening in public medical clinics in Francistown, Botswana. TB = tuberculosis
Acknowledgements
This project was supported by the US Centers for Disease Control and Prevention (CDC) through the President’s Emergency Plan For AIDS Relief. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
References
- 1.World Health Organization. WHO report 2011: global tuberculosis control. WHO/HTM/TB/2011.16. Geneva, Switzerland: WHO, 2011. [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS. 2006 report on the global AIDS epidemic. Geneva, Switzerland: UNAIDS, 2006. http://www.unaids.org/en/KnowledgeCentre/HIVData/ GlobalReport/2006/default.asp Accessed April 2012. [Google Scholar]
- 3.Ministry of Health. Botswana National Tuberculosis Programme manual. Gaborone, Botswana: MOH, 2011. [Google Scholar]
- 4.World Health Organization. Interim policy on collaborative TB/HIV activities. WHO/HTM/TB/2004.330. WHO/HTM/ HIV/2004.1. Geneva, Switzerland: WHO, 2004. [Google Scholar]
- 5.Ministry of Health. Botswana National Tuberculosis Programme manual. Gaborone, Botswana: MOH, 2007. [Google Scholar]
- 6.Cain KP, McCarthy KD, Heilig CM, et al. An algorithm for tuberculosis screening and diagnosis in people with HIV. N Engl J Med 2010; 362: 707–716. [DOI] [PubMed] [Google Scholar]
- 7.Shah S, Demissie M, Lambert L, et al. Intensified tuberculosis case finding among HIV-infected persons from a voluntary counseling and testing center in Addis Ababa, Ethiopia. J Acquir Immune Defic Syndr 2009; 50: 537–545. [DOI] [PubMed] [Google Scholar]
- 8.Ayles H, Schaap A, Nota A, et al. for the ZAMSTAR Study Team. Prevalence of tuberculosis, HIV and respiratory symptoms in two Zambian communities: implications for tuberculosis control in the era of HIV. PLoS One 2009; 4: e5602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kranzer K, Houben RM, Glynn JR, Bekker LG, Wood R, Lawn SD. Yield of HIV-associated tuberculosis during intensified case finding in resource-limited settings: a systematic review and meta-analysis. Lancet Infect Dis 2010; 10: 93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monkongdee P, McCarthy KD, Cain KP, et al. Yield of acid-fast smear and mycobacterial culture for tuberculosis diagnosis in people with human immunodeficiency virus. Am J Respir Crit Care Med 2009; 180: 903–908. [DOI] [PubMed] [Google Scholar]


