Abstract
Introduction
Exercise addiction is characterized by the use of physical activity to cope with emotions and mood, while sports injuries can lead to psychological distress such as depression and anxiety. The aim of the present study was to investigate the association between risk of exercise addiction and psychological distress, and whether this association was modified by injury status.
Methods
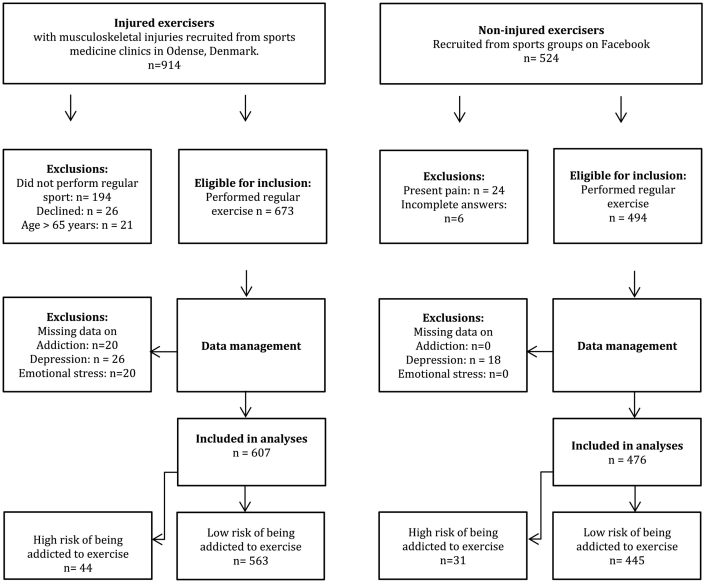
A cross-sectional study with injured and non-injured recreational exercisers (n = 1083). Using the Exercise Addiction Inventory participants were classified into the following groups: High risk of exercise addiction (HREA) with musculoskeletal injury (n = 44); HREA without musculoskeletal injury (n = 31); Low risk of addiction (LREA) with injury (n = 563); LREA without injury (n = 445). The outcomes were depression using the Major Depression Inventory, and emotional stress using the Perceived Stress Scale. Data were analyzed using binomial regression analysis with prevalence proportion difference (PPD) as measure of association.
Results
Compared with LREA-exercisers, more HREA exercisers were depressed (PPD = 13% points [95%CI 3.6; 22.4]) or experienced emotional stress (PPD = 26.2% points [95%CI 14.5; 37.8]). Amongst injured exercisers, more HREA exercisers had depression (PPDHREA-injured = 15.9% points [95%CI 2.5; 29.3]) compared with LREA-exercisers.
Conclusions
Recreational exercisers with high risk of exercise addiction reported more symptoms of depression and emotional stress, and this relationship seemed exacerbated in the presence of musculoskeletal injury. Psychological assessment and counseling may be useful supplements to somatic injury interventions for addressing emotional distress.
Keywords: Exercise addiction, Sport injury, Depression, Stress, Quality of life
Highlights
-
•
Exercisers with high risk of exercise addiction reported more depression and emotional stress.
-
•
Emotional distress was higher in the presence of musculoskeletal injury.
-
•
In addicted exercisers with injuries the prevalence of depression was 26%.
-
•
Evaluation of addiction symptoms helps to identify exercisers at risk of depression.
-
•
Psychological assessment and counseling may complement somatic injury interventions.
1. Introduction
Physical activity can reduce the risk of lifestyle diseases, enhance physical functioning, and improve quality of life (Ekelund et al., 2016; Galper, Trivedi, Barlow, Dunn, & Kampert, 2006; Norris, Carroll, & Cochrane, 1990). In addition, physical activity enhances psychological well-being (Andersen, Mota, & Di Pietro, 2016; Ekelund et al., 2016; Espi-Lopez, Ingles, Ruescas-Nicolau, & Moreno-Segura, 2016; U.S. Department of Health and Human Services, 2000). Less is known about the potential negative aspects of exercise, however, such as psychological distress due to musculoskeletal injury and the harmful consequences of addiction to exercise (Li, Nie, & Ren, 2015; Szabo & Griffiths, 2007; Szabo, Griffiths, de La Vega Marcos, Mervó, & Demetrovics, 2015; Weinstein, Maayan, & Weinstein, 2015).
Based on theories for behavioral addictions (Brown, 1993, Brown, 1997), we can characterize exercise addiction as constantly increasing amounts of exercise, withdrawal symptoms (e.g. restlessness and frustration), using exercise to regulate emotions, conflicts with family, and loss of control over exercise (Adams & Kirkby, 2002; Berczik et al., 2012; Hausenblas & Symons Downs, 2002). Further, theories of exercise addiction suggest that “continuance” is a core symptom of addiction (Hausenblas & Symons Downs, 2002) that drives athletes to continue exercise despite pain and injuries (Ekenman, Hassmen, Koivula, Rolf, & Fellander-Tsai, 2001).
The Exercise Addiction Inventory (EAI) (Terry, Szabo, & Griffiths, 2004) was developed to assess the theoretically defined symptoms of exercise addiction. The EAI can be used to identify exercisers with high risk of being addicted to exercise, and prevalence proportions have been estimated to be 3–9% in different sports settings (Griffiths et al., 2015) and 0.5% in the general population (Mónok et al., 2012).
Exercisers who develop injuries that prevent them from being physically active can experience depression, as shown by self-report and on clinical assessment (Appaneal, Levine, Perna, & Roh, 2009). Aidman and Woollard (2003) thus showed that just one day of exercise deprivation can lead to increased tension and depressed mood, while another study found that addicted athletes who were deprived of exercise for two weeks reported higher levels of depression, confusion, anger, fatigue, and decreased vigor (Antunes et al., 2016). Injuries in athletes can be emotionally traumatizing, and even suicidal thoughts have been reported (Smith & Milliner, 1994). Wiese-Bjornstal and colleagues have proposed a theoretical model for the complex psychosocial aspects of sports injury (Wiese-Bjornstal, Smith, Shaffer, & Morrey, 1998), in which both personal and contextual factors impact on injury responses. Exercise addiction was not addressed in this model, but it is plausible that addiction is a risk factor for severely negative post-injury mood due to exercise deprivation (Szabo, Frenkl, & Caputo, 1997). Post-injury psychological distress and quality of life have not previously been explored in regular exercisers with high risk of addiction, nor compared with levels in injured exercisers without addiction.
The aim of the present study was to investigate the association between risk of exercise addiction and psychological distress, and whether this association was modified by injury status. We hypothesized that exercisers with high risk of exercise addiction (HREA) would have higher prevalence proportion of depression and stress symptoms and decreased quality of life compared with exercisers with low risk of exercise addiction (LREA). We further hypothesized that the association between exercise addiction and psychological stress would be exacerbated in the event of injury.
2. Methods
2.1. Study design and settings
The study was designed as a questionnaire-based cross-sectional study and was undertaken as an interdisciplinary collaboration between psychologists at the Mental Health Services in the Region of Southern Denmark and medical doctors at the sports medicine clinic at Odense University Hospital, Denmark. The reporting followed the STROBE guidelines for observational studies (von Elm et al., 2008).
2.2. Participants and procedures
In the present study, ‘exercisers’ were defined as males and females aged 13–65 years who undertook regular physical exercise, i.e. physical activity at least once a week in their spare time e.g. running, fitness, ball sports. Leisure time physical activity once a week is considered sufficient for health benefits such as reduced cardiovascular disease and cancer (O'Donovan, Lee, Hamer, & Stamatakis, 2017). A total of 1083 subjects participated in the study. The mean age was 28 years (standard deviation 19), and males comprised 46% of the sample. Elite athletes were not excluded (n = 24).
Injured exercisers were recruited amongst patients attending a sports medicine clinic for diagnosis and treatment of a musculoskeletal injury that limited their physical functioning. They were asked by a nurse to complete a paper version of the study questionnaire in the waiting room prior to the clinical examination. Data were collected between 16th June 2014 and 1st April 2015. Participants were excluded from data analysis if they did not fulfil the criteria for regular physical exercise or had missing questionnaire data.
Non-injured exercisers were recruited through online sports groups (e.g. fitness center clubs on social media) and were invited to participate by completing an online version of the study questionnaire. Participants responded to the questionnaire from their own digital device and were recruited during May and June 2016. Participants were excluded from data analysis if they had missing questionnaire data or reported current pain.
This online approach has shown to be useful in addiction research, as social networking sites are efficient ways to recruit large numbers of participants with relevant behaviors and conditions (such as substance abuse or mental health issues) and with varied age and socioeconomic status (Thornton, Harris, Baker, Johnson, & Kay-Lambkin, 2016).
2.3. Outcomes
The primary outcomes of interest were depressive symptoms and emotional stress. The secondary outcome was self-rated quality of life in terms of mobility, self-care, usual activities, pain/discomfort, and depression/anxiety.
2.3.1. Primary outcomes
Depressive symptoms were measured with the Major Depression Inventory (MDI), which is compatible with the depression criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD) (Bech, Rasmussen, Olsen, Noerholm, & Abildgaard, 2001; Konstantinidis, Martiny, Bech, & Kasper, 2011). The MDI consists of ten items that are rated on a 6-point Likert scale from 0 (never) to 5 (all the time). The total score ranges from 0 to 50, where a higher score reflects more symptoms of depression within the previous two weeks. The recommended cut-off point for major depression (MD) is ≥26 (Bech, Timmerby, Martiny, Lunde, & Soendergaard, 2015), thus distinguishing between moderate or severe depressive symptoms (MD ≥26) and none or mild depressive symptoms (MD <26). In the current study, we used the cut-off point of 26 to distinguish people at high risk of being depressed from those at low risk. One of the MDI items addresses thoughts of “Life is not worth living”, and we explored the responses to this item more closely to assess feelings of hopelessness. Respondents in this study were classified as having symptoms of depression if MDI score was ≥26 and with none/mild depressive symptoms if MDI score <26. Responses to the MDI item “Life is not worth living” were further dichotomized into “No thoughts” (1) or “Some thoughts” (2) to assess the presence of potential suicidal ideation.
Emotional stress was measured with the 10-item Perceived Stress Scale (PSS) (Cohen, Kamarck, & Mermelstein, 1983) that was developed to measure a person's evaluation of stressful situations in the previous month. The ten items ask about how unpredictable, uncontrollable, or overloaded the respondents feels their lives are, and are rated on a 5-point Likert scale from 0 (never) to 4 (very often). The total score ranges from 0 to 40, where a higher score reflects more emotional stress. Respondents were classified as having symptoms of emotional stress if PSS score was 18–40 and without symptoms of emotional stress if PSS was 0–17.
2.3.2. Secondary outcomes
Health-related quality of life (QOL) was measured with the EQ-5D-5L, a generic health outcome measure (Brooks, 1996; Herdman et al., 2011) that has a descriptive profile with five dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression), each with five levels of severity (no problems, slight/moderate/severe/extreme problems). Responses to the EQ-5D-5L dimensions were dichotomized as “No problems” (level 1) or “Some problems” (levels 2–5). The EQ-5D-5L includes a visual analogue scale (VAS) where the respondents rate their health today with endpoints of “the worst health you can imagine” (0) and the “best health you can imagine” (100). The questionnaire also included an item addressing “fear of new injury” to assess injury-related aspects of anxiety.
The online and paper versions of the questionnaires were tested for comprehensibility in a pilot study involving 10 non-injured exercisers (online version) and 20 injured patients (paper version). The introductory section of the questionnaire included information about the study's aims and methods, data confidentiality, and the ability to withdraw from completing the questionnaire at any time.
2.4. Exposure
The risk of being addicted to exercise was assessed with the Exercise Addiction Inventory (EAI) (Terry et al., 2004). The EAI is a six-item screening tool that has been translated and validated in several countries (Griffiths et al., 2015), including Denmark with a Cronbach's Alpha coefficient: 0.66 (Lichtenstein, Christiansen, Bilenberg, & Stoving, 2014). Answers are rated on a 5-point Likert scale ranging from “Strongly disagree” (1) to “Strongly agree” (5). A total EAI score of 24–30 is considered to reflect a high risk of being addicted to exercise, while an EAI score of 6–23 reflects a low risk of being addicted to exercise. We supplemented the EAI with two further items to assess potential negative exercise attitudes. 1. “I exercise in spite of pain and injury” was added to measure continuance despite persistent or recurrent physical problems that might have been caused by excessive exercise. 2. “I am too addicted to my exercise” was added as an internal validation of the underlying construct in the EAI.
2.5. Effect-measure modifier
Musculoskeletal injury was defined as pain and physical inhibition that caused the exerciser to seek medical attention from health care professionals at sports medicine clinics treating injuries in foot, knee, or shoulder. Injury (dichotomized into yes/no) was included as an effect-measure modifier on the association between the exercise addiction score (EAI) and symptoms of depression (MDI) or emotional stress (PSS).
2.6. Statistics
Demographic characteristics are reported with mean and standard deviation if normally distributed and with median and interquartile range if non-normally distributed. Scale scores were calculated according to the developers' guidelines. No imputations were made for missing data. t-test was used to compare exercise amounts between HREA and LREA, and chi square analyses were used to compare the percentage of participants who reported exercise despite pain and injury, self-perceived addiction, and fear of new injury.
Binomial regression analyses were used to explore the association between HREA and presence of depressive symptoms (MDI score), emotional stress (PSS score), and problems on EQ-5D-5L dimensions. The differences in prevalence proportions and their 95% confidence intervals between exercisers with and without signs of exercise addiction and with and without injury were estimated with binomial regressions. They are reported according to previous recommendations (Knol & VanderWeele, 2012). Although the significance level was set at <0.05, further evaluation of results included estimates and confidence intervals (Stang, Poole, & Kuss, 2010).
The statistical package STATA (StataCorp, USA, version 14 SE) was used for data analyses.
2.7. Ethics
The research met the required ethical standards and was approved by the Regional Committees on Health Research Ethics for Southern Denmark. By completing the survey, the participants gave consent regarding data for scientific use. The project was registered with the Danish Data Protection Agency (number 2008–58-0035) and contains some of the same participants as a study investigating the prevalence proportion of depression amongst physically active orthopedic patients (Lichtenstein, Gudex, Andersen, Bojesen, & Jørgensen, 2017).
3. Results
After exclusion of 84 respondents with missing data on the exercise addiction questionnaire EAI (n = 20), depression questionnaire MDI (n = 44), or stress questionnaire PSS (n = 20), the final sample consisted of 1083 exercisers classified as: 1) 44 injured HREA exercisers; 2) 563 injured LREA exercisers; 3) 31 non-injured HREA exercisers, and 4) 445 non-injured LREA exercisers (Fig. 1). We found that the prevalence proportion of depression (MDI score ≥26) was 26%, 11%, 13% and 5%, respectively in these four groups. The scores on the MDI-item “life is not worth living” showed the same patterns as 23%, 14%, 16% and 8% reported to have these thoughts to some extent. The demographic characteristics of the participants at high and low risk of depression are presented in Table 1.
Fig. 1.
Flow-chart of participant recruitment and exclusions.
Table 1.
Demographic characteristics of the included participants according to risk of depression based on Major Depression Index (MDI) scores.
| Measure | High risk of depression MDI ≥26 (n = 100) |
Low risk of depression MDI <26 (n = 983) |
All (n = 1083) |
|
|---|---|---|---|---|
| Age, years | Median (iqr) | 25 (9) | 29 (20) | 28 (19) |
| Gender, male | n (%) | 40 (40%) | 462 (47%) | 502 (46%) |
| Body Mass Index, kg/m2 | Median (iqr) | 23.1 (5.2) | 24.0 (4.6) | 23.9 (4.7) |
| PSS emotional stress score | Mean (sd) | 24.3 (4.9) | 12.6 (5.6) | 13.7 (6.5) |
| Self-reported health, EQ-VAS | Median (iqr) | 63 (35) | 82.5 (20) | 80 (20) |
| EQ-5D sub-scales problems: | ||||
| Mobility | n (%) | 63 (63%) | 286 (29%) | 349 (32%) |
| Self-care | n (%) | 36 (36%) | 153 (16%) | 189 (18%) |
| Usual activities | n (%) | 83 (83%) | 464 (47%) | 547 (51%) |
| Pain/discomfort | n (%) | 92 (92%) | 721 (74%) | 813 (75%) |
| Anxiety/depression | n (%) | 82 (82%) | 230 (24%) | 312 (29%) |
iqr = inter-quartile range; sd = standard deviation.
PSS = Perceived Stress Scale (0–40, higher scores reflect more emotional stress); EQ-VAS = EQ-5D-5 L visual analogue scale (0–100, higher scores reflect better self-reported health); EQ-5D sub-scales any problems reported.
In Table 2, the unadjusted association between risk of exercise addiction and the following seven outcomes (dichotomized into yes/no) are presented: depression, emotional stress, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. HREA exercisers reported significantly more psychological distress (in terms of depression and emotional stress) than did LREA exercisers.
Table 2.
Association between high risk of exercise addiction and reporting of psychological distress or problems with health-related quality of life.
| Exposure | Number reporting yes or no | Prevalence proportion difference | 95% confidence interval | p-Value | |
|---|---|---|---|---|---|
| Symptoms of major depression (MDI) | HREA | 16/59 | 13.0% | [3.6%; 22.4%] | 0.007 |
| LREA | 84/924 | 0 (ref) | |||
| Symptoms of emotional stress (PSS) | HREA | 38/37 | 26.2% | [14.5%; 37.8%] | < 0.001 |
| LREA | 247/761 | 0 (ref) | |||
| Any problems on EQ-5D mobility |
HREA | 26/49 | 2.5% | [−8.7%; 13.6%] | 0.661 |
| LREA | 323/681 | 0 (ref) | |||
| Any problems on EQ-5D self-care |
HREA | 13/62 | −0.2% | [−9.1%; 8.7%] | 0.965 |
| LREA | 176/828 | 0 (ref) | |||
| Any problems on EQ-5D usual activities |
HREA | 41/34 | 4.4% | [−7.3%; 16.1%] | 0.464 |
| LREA | 506/500 | 0 (ref) | |||
| Any problems on EQ-5D pain/discomfort |
HREA | 58/17 | 2.3% | [−7.6%; 12.1%] | 0.649 |
| LREA | 755/251 | 0 (ref) | |||
| Any problems on EQ-5D anxiety/depression |
HREA | 34/41 | 17.6% | [6.0%; 29.2%] | 0.003 |
| LREA | 278/726 | 0 (ref) |
HREA = high risk of exercise addiction. LREA = low risk of exercise addiction. Ref = reference.
MDI = Major Depression Index. PSS = Perceived Stress Scale.
Assuming causal relationships, the numbers needed to treat (NNT) to avoid one depression: NNT = 1/0.13 = 7.7 persons. Similarly, the NNT for emotional stress was 1/0,262 = 3.8 persons and for Anxiety 1/0,176 = 5.7 persons.
HREA exercisers reported more frequent weekly exercise (8 h/week) compared to those with low risk of addiction (5 h/week), p < 0.01. In HREA exercisers 80% with injury reported that they exercised despite pain and injury, compared with 26% of LREA exercisers without injury (p < 0.01), and 45% of the HREA with injury considered themselves overly dependent on exercise, compared with 4% of the LREA group without injury (p < 0.01). Finally, we found that 64% of the HREA group with injury reported fear of new sports injuries, compared with 17% of LREA without injury (p < 0.01).
Analyses on the association between risk of addiction and psychological functioning (depression and emotional stress) according to injury status are presented in Table 3. Amongst non-injured exercisers, 8.4% more of the HREA exercisers had risk of depression compared with LREA. Amongst injured exercisers, 15.9% more of the HREA exercisers had risk of depression compared with LREA. Comparisons across injury status showed that these differences were not significant, however, i.e. a non-significant difference in PPD of depression of 7.5% [−10.5%; 25.5%], p = 0.41, and a non-significant difference in PPD of emotional stress of 1.2% [−22.2%; 24.8%], p = 0.91.
Table 3.
Stratified analyses (binomial regression) on the association between exercise addiction and psychological functioning according to injury status.
| Exercise addiction |
PPD within strata of injury | |||||
|---|---|---|---|---|---|---|
| Low risk addiction |
High risk addiction |
|||||
| Dysfunction/no dysfunction | PPD 95% CI | Dysfunction/no dysfunction | PPD 95% CI | |||
| Depression | Non-injured | 20/425 | Reference | 12/27 | 8.4% [−3.5%; 20.4%] p = 0.17 |
8.4% [−3.5%; 20.4%] p = 0.17 |
| Injured | 64/499 | 6.9% [3.6%; 10.1%] p < 0.01 |
4/38 | 22.8% [9.5%; 36.1%] p < 0.01 |
15.9% [2.5%; 29.3%] p < 0.01 |
|
| Emotional stress | Non-injured | 89/356 | Reference | 14/17 | 25.2% [7.3%; 43.1%] p < 0.01 |
25.2% [7.3%; 43.1%] p < 0.01 |
| Injured | 158/405 | 8.1% [2.8%; 13.3%] p < 0.01 |
24/20 | 34.5% [19.4%; 49.7%] p < 0.01 |
26.4% [11.3%; 41.7] p < 0.01 |
|
Participants were categorized into four groups according to their risk of being addicted to exercise and their injury status. Analyses of two psychological distress outcomes are presented: Depression and Emotional stress. The reference risks for the exercisers at low risk of addiction and with no injuries were 4.5% [2.6%; 6.4%] for depression; and 20.0% [16.3%; 23.7%] for emotional distress. CI = confidence interval. Measure of association is prevalence proportion difference (PPD), which is interpreted as percentage points. The test for no difference between the two injury strata revealed a non-significant difference in PPD across strata of 7.5% [−10.5%; 25.5%], p = 0.41. Similarly, no difference was observed for emotional stress across strata of injury = 1.2% [−22.2%; 24.8%], p = 0.91.
4. Discussion
The aim of this cross-sectional study was to investigate the association between risk of exercise addiction and self-reported depression, emotional stress, and quality of life, and whether this association was modified by musculoskeletal injury.
4.1. Depression
We found that 4.5% in the reference group (non-injured exercisers at low risk of exercise addiction) had MDI scores indicating symptoms of moderate or severe depression. This finding is similar to the prevalence proportion of depression in the general Danish population of approximately 5% (Kessler et al., 2003; Kessler & Bromet, 2013). As expected, musculoskeletal injury in itself was associated with a higher prevalence proportion (12%) of depression in LREA exercisers (results not presented). In comparison, however, 13% of non-injured HREA exercisers had depression, and 26% of injured HREA exercisers had depression. Studies on post-injury depression in exercisers have found 10% with symptoms of major depression one month after injury (Appaneal et al., 2009) and 21% with mild-moderate depression after 3 weeks (Manuel et al., 2002). Depressed mood is the most common emotional reaction to injury (Brewer, 2007) and, if untreated, this can develop into a psychiatric disorder with severe negative consequences and psychosocial disability (Pietrzak et al., 2013).
Suicidal ideation is a symptom of severe depression and has rarely been addressed in post-injury research in exercisers. Our preliminary data of “hopelessness” are based on an MDI-item addressing the thought: “Life is not worth living”. We found that almost one-quarter (23%) of the injured HREA exercisers reported some of these thoughts, compared with only 8% of the non-injured LREA exercisers.
Our stratified analyses showed that amongst non-injured exercisers, 8.4% more of the HREA exercisers had risk of depression compared with LREA exercisers. Amongst injured exercisers, 15.9% more of the HREA exercisers had risk of depression compared with LREA. Although these differences were not statistically significant, they suggest that the risk of depression amongst exercisers with low or high risk of addiction is exacerbated by injury. The results from Table 2 showed that in a clinical psychology context, we would have to offer psychotherapy to 7.7 exercisers with HREA to prevent one case of depression (assuming a causal relationship).
4.2. Emotional stress
Emotional stress was chosen as a primary outcome on the assumption that sports injury can be perceived as a life stressor as it is associated with pain and physical impairment. We found that HREA exercisers reported significantly more emotional distress than LREA exercisers, and that injured exercisers showed more, though not statistically significantly, emotional distress than non-injured exercisers.
More than half of the injured exercisers in the HREA group had clinical stress compared with 28% of the injured LREA exercisers. However, non-injured HREA exercisers reported similar high levels of stress, indicating that HREA in itself may be associated with a high basic level of stress. This is presumably also reflected in the significantly higher proportion of HREA exercisers who reported fear of future injuries compared with the reference group.
Our results from Table 2 showed that in a clinical psychology context we would have to offer psychotherapy to 3.8 exercisers with exercise addiction to prevent one case of emotional stress (assuming a causal relationship).
4.3. Health-related quality of life
The reference group of LREA non-injured exercisers had similar self-rated health (mean VAS score 87) to that reported by the Danish general population (mean VAS score 84) (Szende, Janssen, & Cabases, 2014). Surprisingly, the HREA non-injured exercisers also reported good health (mean score 86). A previous study reported no differences in health-related quality of life (measured with SF-36) in addicted versus non-addicted exercisers, except that the bodily pain score was higher amongst HREA exercisers (Lichtenstein, Christiansen, Elklit, Bilenberg, & Stoving, 2014). Contrary to these findings, Spanish endurance cyclists with HREA displayed worse values of mental quality of life compared to cyclists with LREA (Mayolas-Pi et al., 2017).
As expected, we found that self-rated health was lower in the presence of injury, but more so for HREA exercisers (mean score 60) than for LREA exercisers (mean score 70). The EQ-5D results showed that present injury had negative impact on mobility, self-care, ability to do usual activities, and pain/discomfort in both groups. However, HREA injured exercisers were twice as likely to have emotional problems (anxiety/depression) than LREA non-injured exercisers. These findings support the stratified analysis, where injury status was associated with higher scores of psychological distress. It is not certain whether more depressed and anxious exercisers are more likely to have injuries, or whether the injury causes all the increased distress in HREA exercisers. The latter explanation would fit well with one of the theories of exercise addiction, that exercise is used to regulate emotions and mood. An injury thus inhibits the use of this coping strategy.
Our results suggest that HREA exercisers report good quality of life as long as they can continue scheduled exercise, but that musculoskeletal injury impacts negatively on self-reported health when the emotional coping strategy is impaired.
4.4. Addiction
Based on EAI-scores, we found HREA prevalence proportions of 7.7% in the sample of injured exercisers from a sports medicine clinic and 6.7% in the sample of non-injured exercisers recruited from the Internet. Similar prevalence proportions have been found in other studies using different recruitment methods (Lichtenstein, Christiansen, Bilenberg, & Stoving, 2014; Lichtenstein & Jensen, 2016; Lichtenstein, Larsen, Stoving, & Bredahl, 2014; Lindwall & Palmeira, 2009; Parastatidou, Georgios, Theodorakis, & Vlachopoulos, 2012; Villella et al., 2011). Cronbach's Alpha coefficient in this study was 0.79 in the injury group and 0.74 in the non-injured group.
Our sample of HREA exercisers was characterized by higher levels of weekly exercise, a tendency to exercise in spite of pain and injury, and a feeling of being overly addicted to exercise. These excessive exercise patterns can be perceived as risk factors for overload injuries. Trainers, fitness instructors, and health professionals in clinical settings (especially physiotherapists and psychologists) who assess and treat HREA exercisers would benefit from more knowledge about the psychosocial functioning of these patients and the impact of injury. We assume this would help them to detect and prevent severe emotional post-injury problems related to exercise addiction.
4.5. Limitations
The cross-sectional design of this study means that we could only assess associations and not causal relationships. Thus it is unclear whether post-injury psychological distress is a result of exercise addiction and/or injury itself or reflects pre-injury levels of depression and/or stress. Pre-injury stress has been associated with higher risk of injury and thus may be a contributor to injury rather than an injury response (Ivarsson, Johnson, & Podlog, 2013; Williams & Andersen, 1998). On the basis of the present data, we assume that injury leads to depression and emotional stress in HREA exercisers, and that exercise addiction should be treated to reduce psychological distress.
Another limitation is that our analyses on exercise addiction, depression, and stress are based on self-report data. More reliable assessment and diagnosis would require clinical interviewing by professional mental health specialists. Furthermore, questionnaire data were collected in two different formats, one as a paper questionnaire completed in a hospital outpatient clinic and the other as a web-based version on the Internet. The use of two different approaches may have produced some inconsistencies in responses between the participant groups. Furthermore, the sampling period was different between injured (June–April) and non-injured subjects (May–June). Potential cases of winter depression in the injury group might affect the depression prevalence in the sample.
A strength of this study is that it addresses psychological distress associated with a current injury and does not rely on retrospective data, as in much of the existing literature on emotional response to injury.
5. Conclusion
We conclude that more HREA exercisers face psychological distress in terms of depression, stress, and reduced quality of life compared with LREA exercisers. In the event of injury, the difference in level of depression appears to be more pronounced. Based on this, we recommend special attention to injured HREA exercisers in the somatic assessment and treatment of injury. Systematic evaluation of addiction symptoms (e.g. using the Exercise Addiction Inventory) and psychological distress (e.g. using the Major Depression Inventory and the Perceived Stress Scale) could help to identify exercisers at high and low risk.
Funding sources
The authors have not received any financial support or benefits from commercial sources for this study.
Conflict of interest
The authors report no financial or other relationship relevant to the subject of this article.
Ethics
The research met the required ethical standards and was approved by The Regional Committees on Health Research Ethics in the Region of Southern Denmark and by the Danish Data Protection Agency.
Contributor Information
Mia Beck Lichtenstein, Email: m.lichtenstein@health.sdu.dk.
Rasmus Oestergaard Nielsen, Email: roen@ph.au.dk.
Claire Gudex, Email: claire.gudex@rsyd.dk.
Cecilie Juul Hinze, Email: cecilie.juul.hinze@rsyd.dk.
Uffe Jørgensen, Email: uffe.joergensen@rsyd.dk.
References
- Adams J., Kirkby R.J. Vol. 10. 2002. Excessive exercise as an addiction: A review; pp. 415–438. [Google Scholar]
- Aidman E.V., Woollard S. The influence of self-reported exercise addiction on acute emotional and physiological responses to brief exercise deprivation. Psychology of Sport and Exercise. 2003;4(3):225–236. [Google Scholar]
- Andersen L.B., Mota J., Di Pietro L. Update on the global pandemic of physical inactivity. The Lancet. 2016;388(10051):1255–1256. doi: 10.1016/S0140-6736(16)30960-6. [DOI] [PubMed] [Google Scholar]
- Antunes H.K.M., Leite G.S.F., Lee K.S., Barreto A.T., Santos R.V.T.d., Souza H.d.S.…de Mello M.T. Exercise deprivation increases negative mood in exercise-addicted subjects and modifies their biochemical markers. Physiology & Behavior. 2016;156:182–190. doi: 10.1016/j.physbeh.2016.01.028. [DOI] [PubMed] [Google Scholar]
- Appaneal R.N., Levine B.R., Perna F.M., Roh J.L. Measuring post-injury depression among male and female competitive athletes. Journal of Sport & Exercise Psychology. 2009;31(1):60–76. doi: 10.1123/jsep.31.1.60. http://www.ayfcoaching.com/AcuCustom/Sitename/Documents/DocumentItem/16774.pdf [DOI] [PubMed] [Google Scholar]
- Bech P., Rasmussen N.A., Olsen L.R., Noerholm V., Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. Journal of Affective Disorders. 2001;66(2–3):159–164. doi: 10.1016/s0165-0327(00)00309-8. https://www.ncbi.nlm.nih.gov/pubmed/11578668 [DOI] [PubMed] [Google Scholar]
- Bech P., Timmerby N., Martiny K., Lunde M., Soendergaard S. Psychometric evaluation of the Major Depression Inventory (MDI) as depression severity scale using the LEAD (Longitudinal Expert Assessment of All Data) as index of validity. BMC Psychiatry. 2015;15 doi: 10.1186/s12888-015-0529-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berczik K., Szabo A., Griffiths M.D., Kurimay T., Kun B., Urban R., Demetrovics Z. Exercise addiction: Symptoms, diagnosis, epidemiology, and etiology. Substance Use & Misuse. 2012;47(4):403–417. doi: 10.3109/10826084.2011.639120. [DOI] [PubMed] [Google Scholar]
- Brewer B.W., Tenenbaum G., Eklund R.C. Handbook of sport psychology. John Wiley & Sons, Inc; 2007. Psychology of sport injury rehabilitation; pp. 404–424. [Google Scholar]
- Brooks R. EuroQol: The current state of play. Health Policy. 1996;37(1):53–72. doi: 10.1016/0168-8510(96)00822-6. https://www.ncbi.nlm.nih.gov/pubmed/10158943 [DOI] [PubMed] [Google Scholar]
- Brown I. Some contributions of the study of gambling to the study of other addictions. In: Eadington W.R., Cornelius J.A., editors. Gambling behaviour and problem gambling. University of Nevada Press; Reno: 1993. pp. 241–272. (Reprinted from: IN FILE) [Google Scholar]
- Brown I. A theoretical model of the behavioural addictions - Applied to offending. In: Hodge J.E., McMurran M., Hollin R.C., editors. Addicted to crime. Wiley; 1997. pp. 13–65. (Reprinted from: IN FILE) [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Ekelund U., Steene-Johannessen J., Brown W.J., Fagerland M.W., Owen N., Powell K.E.…Lee I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. The Lancet. 2016;388(10051):1302–1310. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- Ekenman I., Hassmen P., Koivula N., Rolf C., Fellander-Tsai L. Stress fractures of the tibia: can personality traits help us detect the injury-prone athlete? Scandinavian Journal of Medicine & Science in Sports. 2001;11(2):87–95PM. doi: 10.1034/j.1600-0838.2001.011002087.x/abstract. 11252466. [DOI] [PubMed] [Google Scholar]
- von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Journal of Clinical Epidemiology. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Espi-Lopez G.V., Ingles M., Ruescas-Nicolau M.A., Moreno-Segura N. Effect of low-impact aerobic exercise combined with music therapy on patients with fibromyalgia. A pilot study. Complementary Therapies in Medicine. 2016;28:1–7. doi: 10.1016/j.ctim.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Galper D.I., Trivedi M.H., Barlow C.E., Dunn A.L., Kampert J.B. Inverse association between physical inactivity and mental health in men and women. Medicine & Science in Sports & Exercise. 2006;38(1):173–178. doi: 10.1249/01.mss.0000180883.32116.28. https://insights.ovid.com/pubmed?pmid=16394971 [DOI] [PubMed] [Google Scholar]
- Griffiths M.D., Urbán R., Demetrovics Z., Lichtenstein M.B., de la Vega R., Kun B.…Szabo A. A cross-cultural re-evaluation of the Exercise Addiction Inventory (EAI) in five countries. Sports Medicine - Open. 2015;1(1):1–7. doi: 10.1186/s40798-014-0005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausenblas H.A., Symons Downs D. Exercise dependence: A systematic review. Psychology of Sport and Exercise. 2002;3(2):89–123. [Google Scholar]
- Herdman M., Gudex C., Lloyd A., Janssen M., Kind P., Parkin D.…Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Quality of Life Research. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivarsson A., Johnson U., Podlog L. Psychological predictors of injury occurrence: A prospective investigation of professional Swedish soccer players. Journal of Sport Rehabilitation. 2013;22(1):19–26PM. doi: 10.1123/jsr.22.1.19. https://www.ncbi.nlm.nih.gov/pubmed/?term=Psychological+predictors+of+injury+occurrence%3A+a+prospective+investigation+of+professional+Swedish+soccer+players (23404909) [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R.…Wang P.S. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Bromet E.J. The epidemiology of depression across cultures. Annual Review of Public Health. 2013;34:119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol M.J., VanderWeele T.J. Recommendations for presenting analyses of effect modification and interaction. International Journal of Epidemiology. 2012;41(2):514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantinidis A., Martiny K., Bech P., Kasper S. A comparison of the Major Depression Inventory (MDI) and the Beck Depression Inventory (BDI) in severely depressed patients. International Journal of Psychiatry in Clinical Practice. 2011;15(1):56–61. doi: 10.3109/13651501.2010.507870. [DOI] [PubMed] [Google Scholar]
- Li M., Nie J., Ren Y. Effects of exercise dependence on psychological health of Chinese college students. Psychiatria Danubina. 2015;27(4):413–419. http://www.hdbp.org/psychiatria_danubina/pdf/dnb_vol27_no4/dnb_vol27_no4_413.pdf [PubMed] [Google Scholar]
- Lichtenstein M.B., Christiansen E., Bilenberg N., Stoving R.K. Validation of the exercise addiction inventory in a Danish sport context. Scandinavian Journal of Medicine & Science in Sports. 2014;24(2):447–453. doi: 10.1111/j.1600-0838.2012.01515.x. [DOI] [PubMed] [Google Scholar]
- Lichtenstein M.B., Christiansen E., Elklit A., Bilenberg N., Stoving R.K. Exercise addiction: A study of eating disorder symptoms, quality of life, personality traits and attachment styles. Psychiatry Research. 2014;215(2):410–416. doi: 10.1016/j.psychres.2013.11.010. [DOI] [PubMed] [Google Scholar]
- Lichtenstein M.B., Gudex C., Andersen K., Bojesen A.B., Jørgensen U. Do exercisers with musculoskeletal injuries report symptoms of depression and stress? Journal of Sport Rehabilitation. 2017 Sep 5:1–22. doi: 10.1123/jsr.2017-0103. [DOI] [PubMed] [Google Scholar]
- Lichtenstein M.B., Jensen T.T. Exercise addiction in CrossFit: Prevalence and psychometric properties of the Exercise Addiction Inventory. Addictive Behaviors Reports. 2016;3:33–37. doi: 10.1016/j.abrep.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein M.B., Larsen K.S., Stoving R.K., Bredahl T.V.G. Exercise addiction in team sport and individual sport: Prevalences and validation of the exercise addiction inventory. Addiction Research and Theory. 2014;22(5):431–437. [Google Scholar]
- Lindwall M., Palmeira A. Factorial validity and invariance testing of the exercise dependence scale-revised in Swedish and Portuguese exercisers. Measurement in Physical Education and Exercise Science. 2009;13(3):166–179. [Google Scholar]
- Manuel J.C., Shilt J.S., Curl W.W., Smith J.A., Durant R.H., Lester L., Sinal S.H. Coping with sports injuries: An examination of the adolescent athlete. Journal of Adolescent Health. 2002;31(5):391–393. doi: 10.1016/s1054-139x(02)00400-7. http://www.sciencedirect.com/science/article/pii/S1054139X02004007?via%3Dihub [DOI] [PubMed] [Google Scholar]
- Mayolas-Pi C., Simon-Grima J., Penarrubia-Lozano C., Munguia-Izquierdo D., Moliner-Urdiales D., Legaz-Arrese A. Exercise addiction risk and health in male and female amateur endurance cyclists. Journal of Behavioral Addictions. 2017;6(1):74–83. doi: 10.1556/2006.6.2017.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mónok K., Berczik K., Urbán R., Szabo A., Griffiths M.D., Farkas J.…Demetrovics Z. Psychometric properties and concurrent validity of two exercise addiction measures: A population wide study. Psychology of Sport and Exercise. 2012;13(6):739–746. [Google Scholar]
- Norris R., Carroll D., Cochrane R. The effects of aerobic and anaerobic training on fitness, blood pressure, and psychological stress and well-being. Journal of Psychosomatic Research. 1990;34(4):367–375. doi: 10.1016/0022-3999(90)90060-h. [DOI] [PubMed] [Google Scholar]
- O'Donovan G., Lee I.M., Hamer M., Stamatakis E. Association of “Weekend Warrior” and other leisure time physical activity patterns with risks for all-cause, cardiovascular disease, and cancer mortality. JAMA Internal Medicine. 2017;177(3):335–342. doi: 10.1001/jamainternmed.2016.8014. [DOI] [PubMed] [Google Scholar]
- Parastatidou I.S., Georgios D., Theodorakis Y., Vlachopoulos S.P. Addicted to exercise. Psychometric properties of the exercise dependence scale-revised in a sample of a Greek exercise participants. European Journal of Psychological Assessment. 2012;28(1):3–10. [Google Scholar]
- Pietrzak R.H., Kinley J., Afifi T.O., Enns M.W., Fawcett J., Sareen J. Subsyndromal depression in the United States: Prevalence, course, and risk for incident psychiatric outcomes. Psychological Medicine. 2013;43(7):1401–1414. doi: 10.1017/S0033291712002309. [DOI] [PubMed] [Google Scholar]
- Smith A.M., Milliner E.K. Injured athletes and the risk of suicide. Journal of Athletic Training. 1994;29(4):337–341PM. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317809/pdf/jathtrain00028-0051.pdf 16558297. [PMC free article] [PubMed] [Google Scholar]
- Stang A., Poole C., Kuss O. The ongoing tyranny of statistical significance testing in biomedical research. European Journal of Epidemiology. 2010;25(4):225–230. doi: 10.1007/s10654-010-9440-x. [DOI] [PubMed] [Google Scholar]
- Szabo A., Frenkl R., Caputo A., Seiler R. European yearbook of sport psychology. Vol. 1. Academia Verlag; 1997. Relationship between addiction to running, commitment to running, and deprivation from running: A study on the internet; pp. 130–147. (Reprinted from: IN FILE) [Google Scholar]
- Szabo A., Griffiths M.D. Exercise addiction in British sport science students. International Journal of Mental Health and Addiction. 2007;5(1):25–28. [Google Scholar]
- Szabo A., Griffiths M.D., de La Vega Marcos R., Mervó B., Demetrovics Z. Methodological and conceptual limitations in exercise addiction research. The Yale Journal of Biology and Medicine. 2015;88(3):303–308. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553651/ [PMC free article] [PubMed] [Google Scholar]
- Szende A., Janssen B., Cabases J. 1st ed. Springer; Netherlands: 2014. Self-reported population health: An international perspective based on EQ-5D. [PubMed] [Google Scholar]
- Terry A., Szabo A., Griffiths M. Vol. 12. 2004. The Exercise addiction inventory: A new brief screening tool. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton L.K., Harris K., Baker A.L., Johnson M., Kay-Lambkin F.J. Recruiting for addiction research via Facebook. Drug and Alcohol Review. 2016;35(4):494–502. doi: 10.1111/dar.12305. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, editor. Healthy people 2010: Understanding and improving health. 2nd ed. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- Villella C., Martinotti G., Di Nicola M., Cassano M., La Torre G., Gliubizzi M.D.…Conte G. Behavioural addictions in adolescents and young adults: Results from a prevalence study. Journal of Gambling Studies. 2011;27(2):203–214PM. doi: 10.1007/s10899-010-9206-0. http://link.springer.com/article/10.1007%2Fs10899-010-9206-0 [DOI] [PubMed] [Google Scholar]
- Weinstein A., Maayan G., Weinstein Y. A study on the relationship between compulsive exercise, depression and anxiety. Journal of Behavioral Addictions. 2015;4(4):315–318. doi: 10.1556/2006.4.2015.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiese-Bjornstal D.M., Smith A.M., Shaffer S.M., Morrey M.A. An integrated model of response to sport injury: Psychological and sociological dynamics. Journal of Applied Sport Psychology. 1998;10(1):46–69. [Google Scholar]
- Williams J.M., Andersen M.B. Psychosocial antecedents of sport injury: Review and critique of the stress and injury model. Journal of Applied Sport Psychology. 1998;10:5–25. [Google Scholar]