Abstract
This retrospective study evaluated the effect of using neuromuscular electrical stimulation (NMES) for the treatment of post-stroke urinary incontinence (PSUI) among female population in China.
A total of 163 eligible patients with PSUI were included in this study. Of these, 103 patients were assigned to a treatment group, and 60 subjects were assigned to a control group. All patients in both groups received bladder training. In addition, patients in the treatment group also received NMES. All patients were treated for a total of 8 weeks. The outcome measurements included the amount of urine leakage, urinary symptoms and quality of life. The urinary symptoms were measured by the Bristol Female Urinary Symptoms Questionnaire (BFUSQ) score, and the quality of life was assessed by the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) score. In addition, adverse events were also documented in this study.
After 4-week treatment, patients who received NMES did not exert better outcomes in the amount of urine leakage, urinary symptoms, measured by BFUSQ scale, and the quality of life, assessed by ICIQ-SF scale. However, after 8-week treatment, patients in the treatment group showed greater effect in reducing the amount of urine leakage (P < .01), enhancing urinary symptoms, as measured by BFUSQ scale (P < .01), and improving the quality of life, as assessed by ICIQ-SF scale (P < .01), compared with patients in the control group. In addition, no adverse event was recorded during the period of 8-week treatment in this study.
The results of this study indicated that NMES may benefit for patients with PSUI after 8-week treatment. Future studies should focus on warranting the results of this study.
Keywords: effect, neuromuscular electrical stimulation, post stroke, urinary incontinence
1. Introduction
Urinary incontinence (UI) is one of the most common complications after stroke.[1–4] It often presents as the involuntary leakage of urine.[5–7] One study reported that about 40% to 60% of patients after stroke experienced UI condition.[8] The other studies also reported that the prevalence of post-stroke UI (PSUI) ranges between 32% to 79% at admission and 25% at hospital discharge.[9–11] Additionally, it still increases to 15% one year later.[11] This condition can result in the physical and psychological issues for patients with PSUI.[12] It is estimated that the daily cost for the treatment of such condition is about $185.60 for each patient with PSUI.[13] Most importantly, it can also lead to moderate or severe disability and high mortality.[14] It has been reported that such patients often experience 52% death by discharge, and 60% within 6 months after stroke.[14]
Several management options have been reported to treat this condition, including behavioral therapy, supportive device, pharmacological intervention, and surgical treatment.[15–18] Behavioral therapies mainly consist of healthy bladder habits and training techniques.[19] It helps patients to change their lifestyle, and to teach them to control and enhance continence ability. Supportive devices are often used as the first-line intervention for patients, who have difficulties in moving or using pads or catheters.[20] Additionally, pharmacological therapies usually result in a variety of side effects.[21] As for surgical treatment, most patients rarely received it, especially in neurological injury patients.[22] Thus, more safe and efficacious interventions are urgently needed to treat PSUI.
It has been reported that alternative treatments, such as herbal medicine, acupuncture, moxibustion, and neuromuscular electrical stimulation (NMES) are used to treat this condition.[23–26] However, no data on the effect of NMES for treating patients with PSUI are available among Chinese female population. Therefore, this retrospective study assessed the effect of NMES for PSUI.
2. Patients and methods
2.1. Ethics
This retrospective study was approved by the ethics medical committee of Yulin No.2 Hospital. It was conducted at this hospital between June 2014 and July 2017. All subjects provided the written informed consent.
2.2. Design
Two investigators independently selected the patient cases from Yulin No.2 Hospital. A total of 163 eligible adult female patients with PSUI were included in this retrospective study. All these included patients were divided into a treatment group (n = 103), and a control group (n = 60). All patients in both groups administered bladder training. In addition, patients in the treatment group also underwent NMES. Both groups received a total of 8 weeks intervention. The outcomes consisted of the amount of urine leakage, urinary symptoms, and quality of life. All the outcomes were evaluated before and after 4-week and 8-week treatment respectively. The data analyst was blinded in this study.
2.3. Patients
All patients were confirmed diagnosed with PSUI by the diagnosis criteria of the American Stroke Association and the International Continence Society. However, this study excluded patients if they were pregnancy, unconsciousness, psychiatric problems, severe organ diseases, having a cardiac pacemaker, or failed to have normal communication ability and recognition. In addition, the cases were also excluded if the patients were administered electrical stimulation therapy, including electroacupuncture 1 month before the study. Furthermore, the cases with incomplete information were also excluded.
2.4. Treatment schedule
All patients in both groups administered bladder training by pelvic muscle exercises, which is a very important form of behavior therapy. It may help patients manage urinary incontinence, and change their urination habits. Each patient was asked to practice this exercise for 5 minutes each session, 1 session daily for a total of 8 weeks.
In addition, patients in the treatment group also underwent NMES therapy at bilateral acupoints Baliao (BL31, over the first sacral foramen; BL32, over the second sacral foramen; BL33, over the third sacral foramen; BL34, over the fourth sacral foramen) and Huiyang (BL35, 0.5 cun lateral to the posterior midline, on the level of the tip of the coccyx) for 30 minutes daily, each pair of points 6 minutes, 3 times weekly for a total of 8 weeks. The NMES device (HANS-100, Nanjing Jisheng Medical Technology Co., Ltd) was applied at a frequency of 2 to 100 Hz. The current intensity of NMES was gradually increased to the maximum tolerance according to each patient. Each device had 2 gel pads attached to a silicon patch. The patches were attached to the local selected acupoint area.
2.5. Outcome measurements
The amount of urine leakage, urinary symptoms and quality of life were utilized to assess the effect of NMES therapy. The amount of urine leakage was measured by the 1 hour pad test. Urinary symptoms were measured by the Bristol Female Urinary Symptoms Questionnaire (BFUSQ) score, with a higher score meaning poorer condition or quality of life,[27] and quality of life was measured by the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) score.[28] It ranges from 0 to 21, with a higher score indicating greater severity. Both scales of BFUSQ and ICIQ-SF were validated before they were utilized in this study. In addition, adverse events were also recorded during the treatment period.
2.6. Statistical analysis
The outcome data was analyzed by the SAS package (Version 9.1; SAS Institute Inc., Cary, NC). Mann–Whitney U test or t test were applied to analyze the continuous data, while χ2 test was used to analyze the categorical data. The statistical significance level was set at P < .05.
3. Results
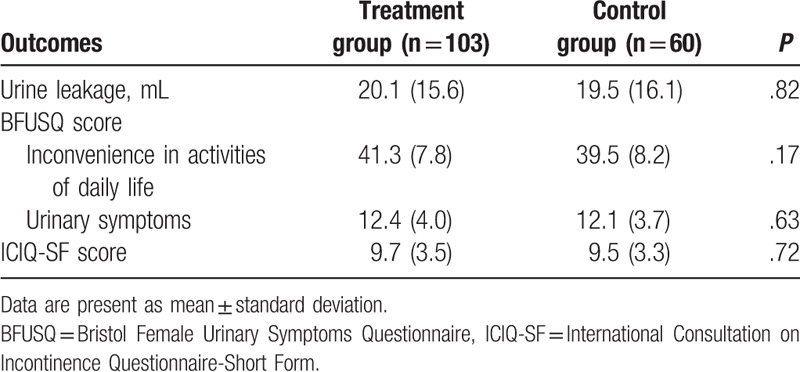
The general characteristics of patients in both groups are listed in Table 1. The comparison did not show significant differences in all characteristics, as well as the outcome measurements before the study (Table 2) between 2 groups. Those characteristics consisted of age, race, and body mass index, duration of post stroke, duration of PSUI, and comorbidities (Table 1).
Table 1.
General characteristic of the included patients.
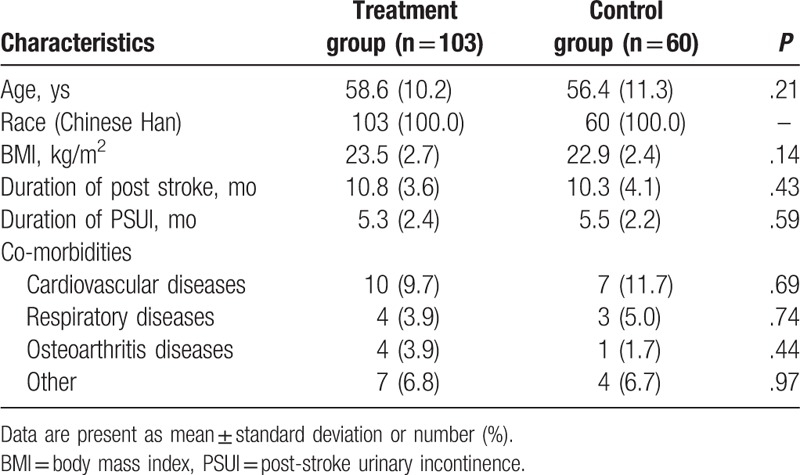
Table 2.
Comparison of outcomes measurements before the treatment.
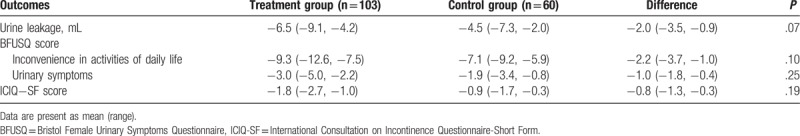
After 4-week treatment, all outcomes in the treatment group did not demonstrate better promising effect in decreasing the amount of urine leakage decrease (P = .82), enhancing the urinary symptoms, as measured by the BFUSQ scale (inconvenience in activities of daily life, P = .17; urinary symptoms, P = .63), and improving the quality of life, as assessed by the ICIQ-SF scale (P = .72), compared to the control group (Table 3).
Table 3.
Comparison of outcome measurements after 4-week treatment (change from before treatment).
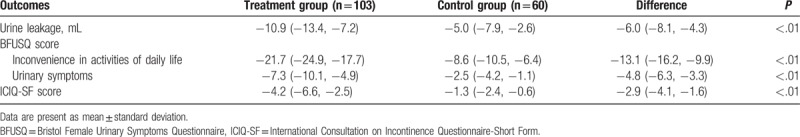
After 8-week treatment, NMES exerted greater outcomes in the amount of urine leakage (P < .01), symptoms decrease, as conducted by the BFUSQ score (P < .01), and quality of life, as evaluated by the ICIQ-SF (P < .01), compared with these outcomes in the control group (Table 4). No adverse event was recorded in both groups during the 8-week treatment period in this study.
Table 4.
Comparison of outcome measurements after 8-week treatment (change from before treatment).
4. Discussion
This retrospective study showed encouraging outcomes after 8-week NMES treatment in patients with PSUI. To our knowledge, no data are available regarding the NMES therapy for treating PSUI in individuals in China presently. In this study, we first utilized NMES intervention for the treatment of PSUI. The findings indicated promising effects of NMES in treating women with PSUI.
Previous related studies have reported promising effects of electroacupuncture for the treatment of patients with PSUI.[4,25] One pilot study found that electroacupuncture may effectively and safely relieve the symptoms and enhance quality of life in women with pure PSUI.[4] The other study reported that acupuncture treatment can contribute to the less urine leakage after 6 weeks in women with stress urinary incontinence.[25]
In this study, our results showed that NMES can significantly reduce the amount of urine leakage; enhance the urinary symptoms, assessed by the BFUSQ scale; and improve the quality of life, measured by the ICIQ-SF scale. Moreover, no adverse event was documented during the period of the treatment. It indicated that NEMS may be safe and efficacious for women with PSUI in China.
This study has several limitations. First, this study had an intrinsic limitation because of the retrospective study. Second, this study only evaluated the effect and safety of NMES for 8-weeks treatment period. Third, this study did not include follow-up assessment after 8-week treatment cessation. All those limitations may impact the results of this study.
5. Conclusion
The results of this study demonstrated that NMES therapy may be efficacious and safety for treating patients with PSUI. Further studies are still needed to warrant the results of this study.
Author contributions
Conceptualization: Shu-Xia Shen, Yun Liu.
Data curation: Shu-Xia Shen, Yun Liu.
Formal analysis: Shu-Xia Shen.
Investigation: Yun Liu.
Methodology: Shu-Xia Shen.
Project administration: Yun Liu.
Resources: Shu-Xia Shen, Yun Liu.
Software: Shu-Xia Shen.
Supervision: Yun Liu.
Validation: Yun Liu.
Visualization: Yun Liu.
Writing – original draft: Shu-Xia Shen, Yun Liu.
Writing – review & editing: Shu-Xia Shen, Yun Liu.
Footnotes
Abbreviations: BFUSQ = Bristol Female Urinary Symptoms Questionnaire, ICIQ-SF = International Consultation on Incontinence Questionnaire-Short Form, NMES = neuromuscular electrical stimulation, PSUI = post-stroke urinary incontinence, UI = urinary incontinence.
The authors declare no conflicts of interest.
References
- [1].Bergman J, Robertson JR, Elia G. Effects of a magnetic field on pelvic floor muscle function in women with stress urinary incontinence. Altern Ther Health Med 2004;10:70–2. [PubMed] [Google Scholar]
- [2].Hasanov E, Hasanov M, Kuria IM, et al. Effects of tamoxifen on urinary incontinence: case report and review of literature. Medicine (Baltimore) 2017;96:e6785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cormio L, Mancini V, Liuzzi G, et al. Surgical management of female pelvic organ prolapse with and without urinary incontinence: a single center experience. Medicine (Baltimore) 2017;96:e7914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Xu H, Liu B, Wu J, et al. A pilot randomized placebo controlled trial of electroacupuncture for women with pure stress urinary incontinence. PLoS One 2016;11:e0150821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zhao Y, Xiao M, Tang F, et al. The effect of water immersion delivery on the strength of pelvic floor muscle and pelvic floor disorders during postpartum period: an experimental study. Medicine (Baltimore) 2017;96:e8124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Choi JB, Yoon BI, Han KD, et al. Urinary incontinence is associated with the development of peptic ulcers in adult women: data from the KNHANES IV. Medicine (Baltimore) 2017;96:e8266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Huang W, Li X, Wang Y, et al. Electroacupuncture for women with stress urinary incontinence: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e9110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 2010;29:213–40. [DOI] [PubMed] [Google Scholar]
- [9].Brittain KR, Peet SM, Potter JF, et al. Prevalence and management of urinary incontinence in stroke survivors. Age Ageing 1999;28:509–11. [DOI] [PubMed] [Google Scholar]
- [10].Marinkovic SP, Badlani G. Voiding and sexual dysfunction after cerebrovascular accidents. J Urol 2001;165:359–70. [DOI] [PubMed] [Google Scholar]
- [11].Booth J, Kumlien S, Zang Y, et al. Rehabilitation nurses practices in relation to urinary incontinence following stroke: a cross-cultural comparison. J Clin Nurs 2009;18:1049–58. [DOI] [PubMed] [Google Scholar]
- [12].Summers D, Leonard A, Wentworth D, et al. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient a scientific statement from the American Heart Association. Stroke 2009;40:2911–44. [DOI] [PubMed] [Google Scholar]
- [13].Green JP, Smoker I, Ho MT, et al. Urinary incontinence in subacute care-a retrospective analysis of clinical outcomes and costs. Med J Aust 2003;178:550–3. [DOI] [PubMed] [Google Scholar]
- [14].Nakayama H, Jørgensen H, Pedersen P, et al. Prevalence and risk factors of incontinence after stroke. The Copenhagen stroke study. Stroke 1997;28:58–62. [DOI] [PubMed] [Google Scholar]
- [15].Dumoulin C, Korner-Bitensky N, Tannenbaum C. Urinary incontinence after stroke: does rehabilitation make a difference? A systematic review of the effectiveness of behavioral therapy. Top Stroke Rehabil 2005;12:66–76. [DOI] [PubMed] [Google Scholar]
- [16].Jundt K, Friese K. Female urinary incontinence. MMW Fortschr Med 2005;147:26–9. [PubMed] [Google Scholar]
- [17].Song QX, Balog BM, Lin DL, et al. Combination histamine and serotonin treatment after simulated childbirth injury improves stress urinary incontinence. Neurourol Urodyn 2016;35:703–10. [DOI] [PubMed] [Google Scholar]
- [18].Johnston S. Stress urinary incontinence treatment: focus should be on identifying best candidates for surgical success in the first place. Can Urol Assoc J 2017;11:281–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wyman JF, Burgio KL, Newman DK. Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. Int J Clin Pract 2009;63:1177–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Khan IJ, Tariq SH. Urinary incontinence: behavioral modification therapy in older adult. Clin Geriatr Med 2004;20:499–509. [DOI] [PubMed] [Google Scholar]
- [21].George A. Management of urinary incontinence. P&T 2012;6:345–61. [PMC free article] [PubMed] [Google Scholar]
- [22].Lum SK, Marshall VR. Results of prostatectomy in patients following a cerebrovascular accident. Br J Urol 1982;54:186–9. [DOI] [PubMed] [Google Scholar]
- [23].Chen YH, Lin YN, Chen WC, et al. Treatment of stress urinary incontinence by cinnamaldehyde, the major constituent of the Chinese medicinal herb ramulus cinnamomi. Evid Based Complement Alternat Med 2014;2014:280204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Yang ZY, Qin X. Moxibustion combined with Chinese medicine for 20 cases of urinary frequence and urinary incontinence in middle aged and elderly women. Zhongguo Zhen Jiu 2012;32:1029–30. [PubMed] [Google Scholar]
- [25].Liu Z, Liu Y, Xu H, et al. Effect of electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. JAMA 2017;317:2493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wang S, Lv J, Feng X, et al. Efficacy of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating female idiopathic urgency urinary incontinence. J Urol 2017;197:1496–501. [DOI] [PubMed] [Google Scholar]
- [27].Brookes ST, Donovan JL, Wright M, et al. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol 2004;191:73–82. [DOI] [PubMed] [Google Scholar]
- [28].Ito H, Hagiwara M, Furuuchi T, et al. Assessments of quality of life in women with urinary incontinence using: King's Health Questionnaire and International Consultation on Incontinence Questionnaire-Short Form. Hinyokika Kiyo 2010;56:255–9. [PubMed] [Google Scholar]


