Abstract
Bile is aseptic; under conditions of no external influx, there is a less than 30% chance of isolating bacteria even in acute cholecystitis. This study was conducted to evaluate the incidence of biliary microflora and most common biliary microflora and resistance to antibiotics in patients with cholecystitis, as well as predict situations that do not require the use of prophylactic antibiotics.
Bile samples were collected for culture using standard methods during all cholecystectomies performed from January 2015 to December 2015 in the Department of Surgery, Pusan National University Hospital. A total of 366 laparoscopic cholecystectomies were performed during the study period. In 215 patients, bile culture was performed and cultures were positive in 54 cases. Prophylactic antibiotics with 2nd-generation cephalosporin were administered once 30 minutes before surgery. According to the results of bile culture, patients were divided into 2 groups, culture-negative and culture-positive groups. Preoperative, intraoperative, and postoperative factors were compared between groups.
The culture positive group was older (P = .000). The number of patients with performance of endoscopic retrograde cholangiopancreatography (ERCP), performance of percutaneous transhepatic gallbladder drainage (PTGBD), presence of symptoms, presence of operative complications, and hospital stay was significantly higher in the culture-positive group than in culture-negative group. In multivariate analysis of factors associated with positive culture, age, ERCP, and symptoms were independent factors affecting positive bile culture. Eighty-five bacteria were identified in 54 patients. Escherichia coli and Klebsiella were common in gram-negative bacteria. Enterococcus was the most common in gram-positive bacteria. Less than 5% resistance was observed against carbapenem, beta-lactam antibiotics, glycopeptide antibiotics, and linezolid.
The bile of patients with laparoscopic cholecystectomy may contain microorganisms, particularly elderly patients, those with symptoms, and those who undergo preoperative ERCP. When ERCP was performed, multiple bacteria culture-positive results were more likely to be found. Although carbapenem, beta-lactam antibiotics, glycopeptide antibiotics, and linezolid may be suitable prophylactic antibiotics, additional studies of the clinical aspects of culture-positive bile is needed to determine the importance of bacterial growth in bile.
Keywords: bile culture, endoscopic retrograde cholangiopancreatography, laparoscopic cholecystectomy, prophylactic antibiotics
1. Introduction
With the development of laparoscopic techniques, laparoscopic cholecystectomy has become a standard procedure. Several studies of the postoperative course have demonstrated that this procedure is relatively safe, with complications occurring in 35 to 6% of cases (mainly biliary injuries and surgical site infections).[1] Acute cholecystitis and emphysematous cholecystitis are known to increase the incidence of complications and, to some extent, bacteria in the bile may increase the risk of adverse intra- and post-operative outcomes.[2] Therefore, the role of prophylactic antibiotics in cholecystectomy may be related to the extent of bacterial proliferation in the bile, making the choice of prophylactic antibiotic, if any, for cholecystectomy a controversial issue.[3,4] Bactibilia is a risk factor for poor operative outcome; if it can be recognized before surgery, patients who do not require prophylactic antibiotics can be identified.
Previous studies investigated the effects of bactibilia on acute cholecystitis, while a few studies have examined uncomplicated gallstone disease or cholecystectomy after endoscopic retrograde cholangiopancreatography (ERCP). This study was designed to evaluate the incidence of biliary microflora and most common biliary microflora and resistance to antibiotics in patients performed laparoscopic cholecystectomy, as well as to determine predictors of situations that do not require the use of prophylactic antibiotics.
1. Methods
1.1. Study group
All patients undergoing laparoscopic cholecystectomy from January 1, 2015 to December 31, 2015 in the Department of Surgery at Pusan National University Hospital in Busan, Korea were included in the study. A total of 366 laparoscopic cholecystectomy procedures were performed during the study period. Except for cases in which bile was not obtained during surgery, bile culture was performed for 215 patients. Preoperative diagnosis included all cases of cholecystectomy, including acute and chronic cholecystitis, cholecystectomy after removal of common bile duct stone with ERCP, and cholecystectomy after percutaneous transhepatic gallbladder drainage (PTGBD). Prophylactic antibiotics with second-generation cephalosporin were administered once 30 minutes before surgery. Oral antibiotics were not used. This retrospective study was approved by the institutional review board at Pusan National University Hospital Clinical Trial Center (IRB No. H-1801-019-063), and written informed consent was obtained from all participants.
1.2. Bile culture techniques
Intraoperative biliary samples were collected under aseptic conditions at the time of operation for bacteriologic examination. The cultures were carefully evaluated for aerobic, anaerobic, and fungal organisms by routine biochemical reactions. Different panels of antimicrobials were used depending on the type of organism isolated, and the results were reported as susceptible, intermediate, or resistant according to the Clinical and Laboratory Standards Institute document M47-A (2007), principles and procedures for blood cultures.
1.3. Data collection
Preoperative data included sex, age, body mass index (BMI), presence of ERCP, presence of PTGBD, and symptoms. Operative and postoperative data included operative complications, length of hospital stay, and result of aerobic and anaerobic cultures. The types of cultured bacteria were examined, and data were also collected for antibiotic resistance in each species. All collected information was entered into a database as either continuous (quantitative data) or categorical (quantitative data) variables. According to the results of bile culture, culture-negative and culture-positive groups were divided into 2 groups, which were compared according to preoperative, intraoperative, and postoperative factors.
1.4. Statistical analysis
To compare the 2 groups, χ2 analysis and Fisher exact test were used when appropriate for qualitative data, and the student t test (for normal variables) or Mann–Whitney U test (for non-normal variables) for quantitative data. For multivariate analysis, the logistic regression technique was applied. A probability of 0.05 or less was accepted as statistically significant. SPSS version 23 (SPSS, Inc., Chicago, IL) was used for all statistical analyses.
2. Results
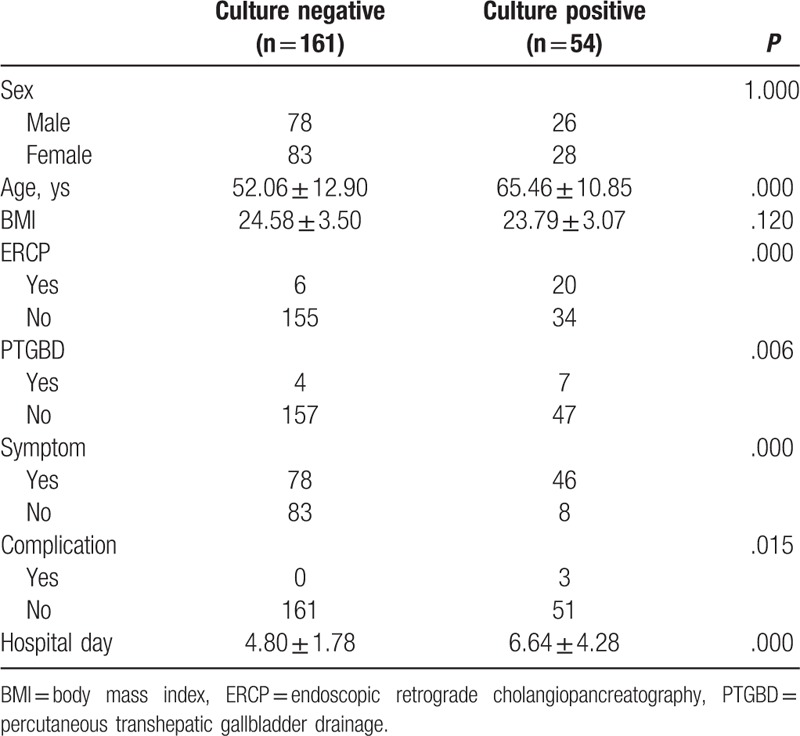
All patients underwent laparoscopic cholecystectomy without conversion to open surgery. Of the 215 patients, 161 (74.9%) were culture-negative and 54 cases (25.1%) were culture-positive. Three patients (1.4%) suffered from complications such as 2 with wound problems and a retained CBD stone in the culture-positive group. The culture-positive group was older (P = .000). The number of patients with performance of ERCP (P = .000), performance of PTGBD (P = .006), presence of symptoms (P = .000), presence of operative complications (P = .015), and hospital day (P = .000) was significantly higher in the culture-positive group (Table 1). ERCP was performed in 26 cases and PTGBD in 11 cases before operation. Thirty of 54 patients visited the emergency room.
Table 1.
Comparative analysis of the patients in the culture-negative and culture-positive group.
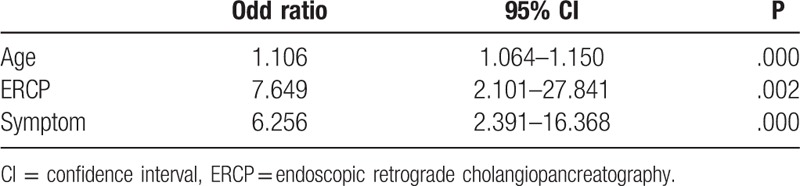
Multivariate analysis of factors associated with positive culture showed that age, performance of ERCP, and presence of symptoms were independent factors of positive bile culture (Table 2).
Table 2.
Mutivariate analysis of factors associated with positive culture.
The culture results are presented in Table 3. Eighty-five bacteria were identified in 54 patients.
Table 3.
Isolated bacteria from bile cultures.
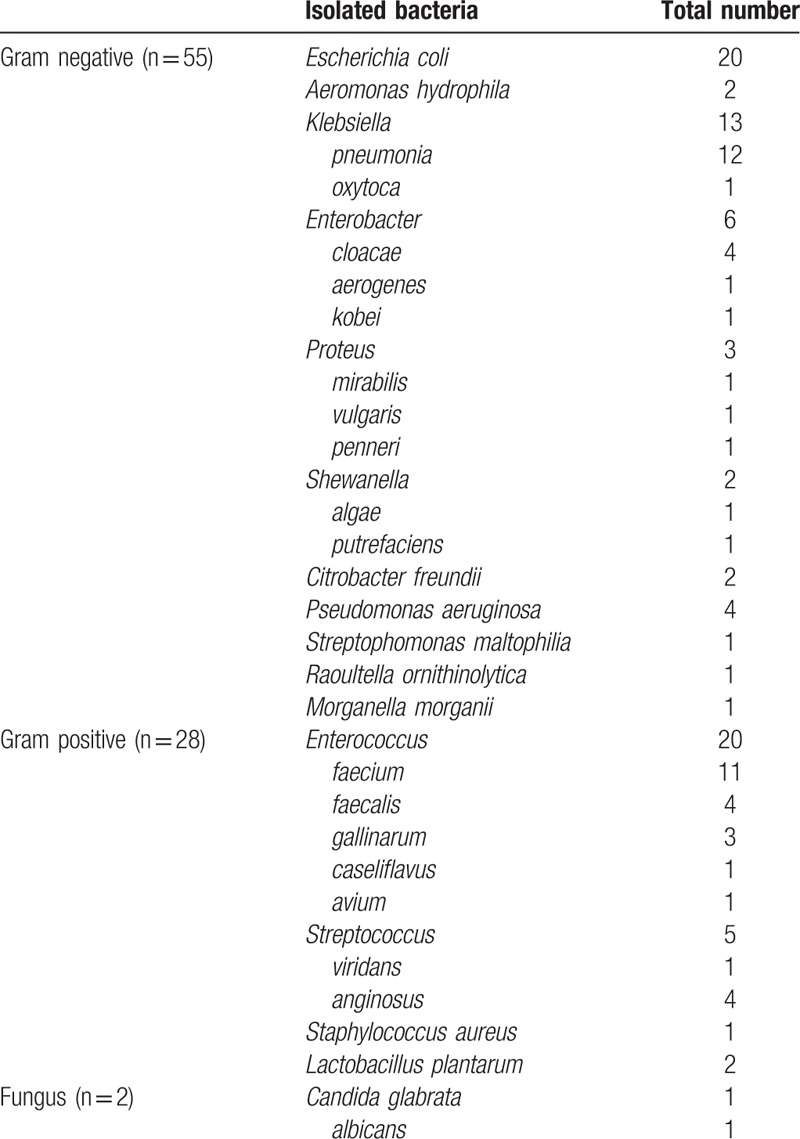
Escherichia coli and Klebsiella were common in gram-negative samples. Enterococcus was the most common in gram-positive cases. Fungus was also cultured in 2 cases. E coli (20 cases) and Enterococcus (20 cases) were the most frequently isolated bacteria in the bile, followed by Klebsiella (13 cases), Enterobacter (6 cases), and Pseudomonas aeruginosa (4 cases) (Table 3).
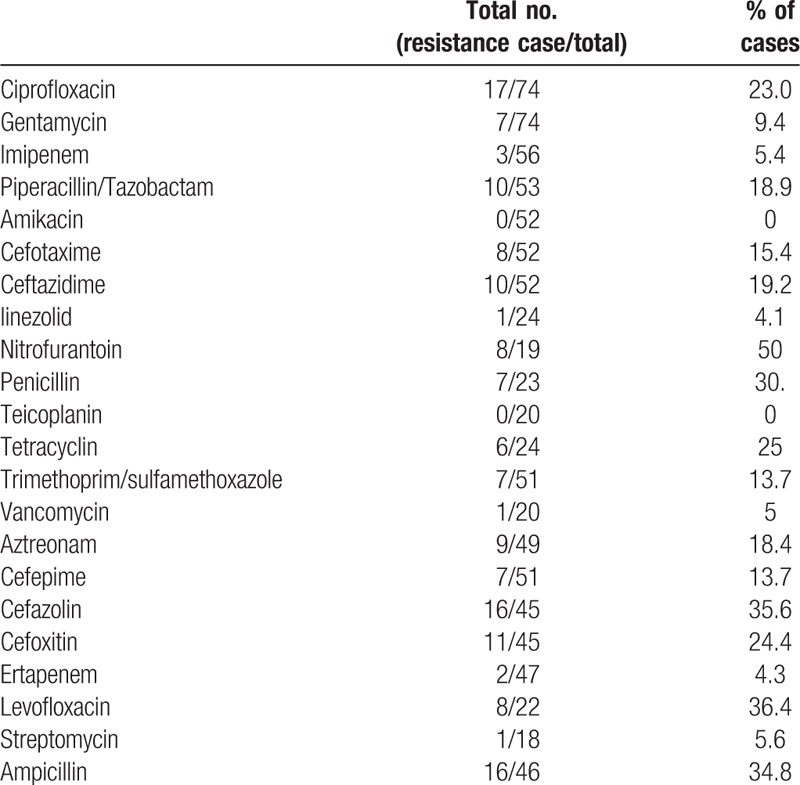
Table 4 shows the antimicrobial resistance results for each bacteria strain. Bacteria were resistant to antibiotics of the 4th-generation cephalosporin series in 13.7% of cases and resistant to antibiotics from generations 1 to 3 in 20% or more of cases. Fluoroquinolone and penicillin series resistance was also observed in 20% of bacteria. Resistance rates of less than 5% were observed against carbapenem, beta-lactam antibiotics, glycopeptide antibiotics, and linezolid. Resistance rates of more than 30% were observed against nitrofurantoin, penicillin, cefazolin, levofloxacin, and ampicillin.
Table 4.
Antibiotics resistance in isolated bacteria.
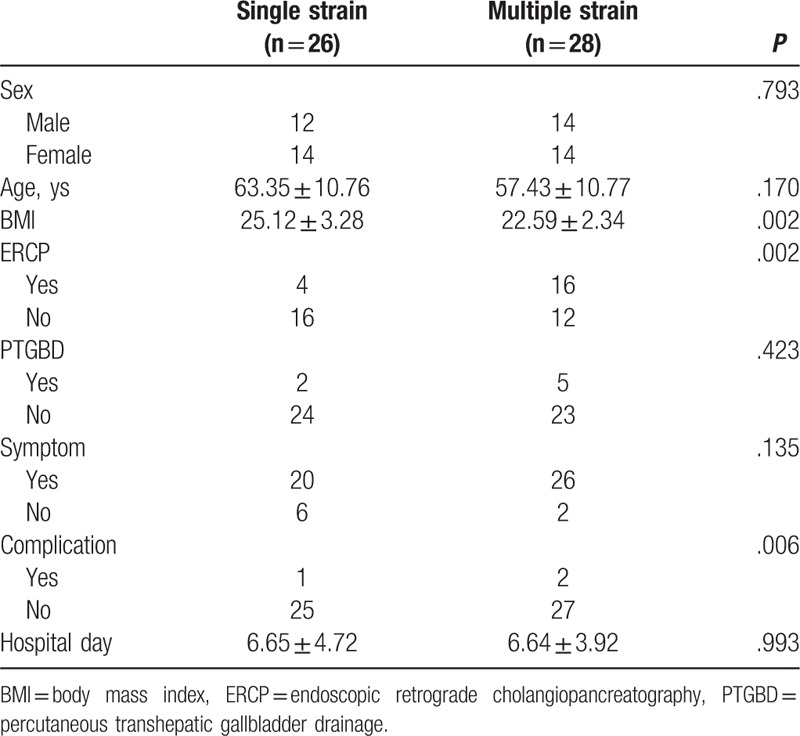
In 54 culture-positive samples, single bacteria-positive culture was observed in 26 patients, while 28 patients had 2 concomitantly positive bile cultures. The number of patients with lower BMI (P = .002), performance of ERCP (P = .002), and presence of operative complications (P = .006) was significantly higher in the multiple strain group according to univariate analysis (Table 5).
Table 5.
Comparative analysis of the patients in the single strain and multiple strain group.
3. Discussion
Laparoscopic cholecystectomy can be safely performed even if a drainage procedure is performed first. Bactibilia is one of the most important causes of acute cholecystitis, and thus is the main target of therapy. Positive bile culture rates range from 9% to 42% in electively resected gallbladders; in cases of acute cholecystitis, its incidence is from 35% to 65%.[2,5–7] In this study, a positive bile culture was observed in 25% of cases. The results of this study are comparable to those of previously reported studies.
In previous studies, E coli, Enterococcus, and Klebsiella predominated among pathogens in positive cultures.[2,7,8] In this study, E coli, Enterococcus, and Klebsiella were the predominant causes of positive bile culture, which agrees with previously published studies. Hoed et al[9] reported that multiple strain bile cultures represented approximately 40% of positive bile cultures. Multiple strain bile cultures were detected in 28 (51.9%) patients in this study. Low BMI, previous ERCP, and operative complication were related to multiple strain bile cultures in univariate analysis.
Mahafzah et al[8] demonstrated that significant predictors of positive bile culture in patients undergoing laparoscopic cholecystectomy were age and preoperative ERCP according to multivariate logistic regression analysis. In our study, multivariate analysis of factors associated with positive culture showed that age, performance of ERCP, and presence of symptoms were independent factors associated with positive bile culture. This result is consistent with those of previous studies. The positive bile culture after preoperative ERCP likely occurred because of sphincterotomy and ascending infection of the bile duct because of the direct connection between the duodenum and biliary tree; biliary drainage leaves free access to bacteria and food debris to move into the biliary tree through the stent, possibly resulting in bile contamination.[8,10] Furthermore, some of these patients have common bile duct stones, similar to associated morbidities, representing a risk factor for bile infection.[11,12] Previous studies also reported that the rate of bile contamination in patients with biliary drainage ranges from 30% to 98%, while infected bile is observed in only 7% to 41% of patients without preoperative biliary drain.[10,13–15]
Darkahi et al[7] reported that a positive culture was the only factor significantly associated with the risk of post-operative infectious complications in multivariable logistic regression analysis, while Mahafzah et al[8] found that it does not influence the occurrence of post-operative septic complications. In this study, the number of patients with lower BMI, performance of ERCP, and presence of operative complication was significantly higher in the multiple strain group based on univariate analysis. These results indicate that even with ERCP, culture-positive and multiple concomitantly positive bile cultures are high. Thus, the incidence of infectious complications may be higher when performing cholecystectomy after ERCP.
The role of prophylactic antibiotics in laparoscopic cholecystectomy in low-risk patients is controversial.[3,7,12,16] This issue remains controversial, as some studies recommended antibiotic prophylaxis, particularly for high-risk patients. Because this study used prophylactic antibiotics in all patients, it is difficult to determine the efficacy of prophylactic antibiotics. Although positive bile culture was not associated with postoperative complications, the use of prophylactic antibiotics in patients undergoing ERCP may reduce postoperative infectious complications. According to bile culture results, carbapenem, beta-lactam antibiotics, glycopeptide antibiotics, and linezolid were the most suitable antibiotics, but are limited to actual clinical applications. Notably, 30% of strains were resistant to commonly used prophylactic antibiotics. Therefore, an acceptable approach may be to limit prophylactic antibiotics to patients with risk factors for bile infection. In addition, in choledocholithiasis patients without cholangitis, cholecystectomy might be performed first to prevent culture-positive infection and prevent future infectious complications.
4. Conclusion
In conclusion, the bile of patients with laparoscopic cholecystectomy may contain microorganisms, particularly elderly patients, those with symptoms, and those who undergo preoperative ERCP. This study indicates that even with ERCP, culture-positive and multiple concomitantly positive bile cultures are high. Therefore, the use of prophylactic antibiotics in patients undergoing ERCP may reduce postoperative infectious complications.
Author contributions
Data curation: Sung Pil Yun.
Formal analysis: Sung Pil Yun.
Investigation: Sung Pil Yun, Hyung-Il Seo.
Supervision: Hyung-Il Seo.
Writing – original draft: Sung Pil Yun.
Writing – review & editing: Sung Pil Yun, Hyung-Il Seo.
Footnotes
Abbreviations: BMI = body mass index, ERCP = endoscopic retrograde cholangiopancreatography, PTGBD = percutaneous transhepatic gallbladder drainage.
The authors declare no conflicts of interest.
References
- [1].Han HJ, Choi SB, Kim WB, et al. Single-incision multiport laparoscopic cholecystectomy: things to overcome. Arch Surg 2011;146:68–73. [DOI] [PubMed] [Google Scholar]
- [2].Galili O, Eldar S, Jr, Matter I, et al. The effect of bactibilia on the course and outcome of laparoscopic cholecystectomy. Eur J Clin Microbiol Infect Dis 2008;27:797–803. [DOI] [PubMed] [Google Scholar]
- [3].Choudhary A, Bechtold ML, Puli SR, et al. Role of prophylactic antibiotics in laparoscopic cholecystectomy: a meta-analysis. J Gastrointest Surg 2008;12:1847–53. [DOI] [PubMed] [Google Scholar]
- [4].Zhou H, Zhang J, Wang Q, et al. Meta-analysis: antibiotic prophylaxis in elective laparoscopic cholecystectomy. Aliment Pharmacol Ther 2009;29:1086–95. [DOI] [PubMed] [Google Scholar]
- [5].Chetlin SH, Elliott DW. Preoperative antibiotics in biliary surgery. Arch Surg 1973;107:319–23. [DOI] [PubMed] [Google Scholar]
- [6].Claesson BE, Holmlund DE, Matzsch TW. Microflora of the gallbladder related to duration of acute cholecystitis. Surg Gynecol Obstet 1986;162:531–5. [PubMed] [Google Scholar]
- [7].Darkahi B, Sandblom G, Liljeholm H, et al. Biliary microflora in patients undergoing cholecystectomy. Surg Infect (Larchmt) 2014;15:262–5. [DOI] [PubMed] [Google Scholar]
- [8].Mahafzah AM, Daradkeh SS. Profile and predictors of bile infection in patients undergoing laparoscopic cholecystectomy. Saudi Med J 2009;30:1044–8. [PubMed] [Google Scholar]
- [9].den Hoed PT, Boelhouwer RU, Veen HF, et al. Infections and bacteriological data after laparoscopic and open gallbladder surgery. J Hosp Infect 1998;39:27–37. [DOI] [PubMed] [Google Scholar]
- [10].De Pastena M, Paiella S, Marchegiani G, et al. Postoperative infections represent a major determinant of outcome after pancreaticoduodenectomy: results from a high-volume center. Surgery 2017;162:792–801. [DOI] [PubMed] [Google Scholar]
- [11].Csendes A, Burdiles P, Maluenda F, et al. Simultaneous bacteriologic assessment of bile from gallbladder and common bile duct in control subjects and patients with gallstones and common duct stones. Arch Surg 1996;131:389–94. [DOI] [PubMed] [Google Scholar]
- [12].Morris-Stiff GJ, O’Donohue P, Ogunbiyi S, et al. Microbiological assessment of bile during cholecystectomy: is all bile infected? HPB (Oxford) 2007;9:225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 2009;37:387–97. [DOI] [PubMed] [Google Scholar]
- [14].Herzog T, Belyaev O, Muller CA, et al. Bacteribilia after preoperative bile duct stenting: a prospective study. J Clin Gastroenterol 2009;43:457–62. [DOI] [PubMed] [Google Scholar]
- [15].Sudo T, Murakami Y, Uemura K, et al. Specific antibiotic prophylaxis based on bile cultures is required to prevent postoperative infectious complications in pancreatoduodenectomy patients who have undergone preoperative biliary drainage. World J Surg 2007;31:2230–5. [DOI] [PubMed] [Google Scholar]
- [16].Rupp C, Bode K, Weiss KH, et al. Microbiological assessment of bile and corresponding antibiotic treatment: a strobe-compliant observational study of 1401 endoscopic retrograde cholangiographies. Medicine (Baltimore) 2016;95:e2390. [DOI] [PMC free article] [PubMed] [Google Scholar]


