Abstract
Background:
This study aimed to evaluate the effectiveness and safety of percutaneous neuromuscular electrical stimulation (PNMES) for treating neck pain in patients with cervical spondylosis (CS).
Methods:
One hundred and twenty four patients with neck pain of CS were included, and then they were randomly divided into a PNMES group and a control group in a ratio of 1:1. All patients received PNMES or sham PNMES 30 minutes daily, 3 times weekly for 12 weeks. The primary outcome was assessed by the visual analog scale (VAS). The secondary outcomes were evaluated by the cervical range of motion (ROM), neck disability index (NDI) score, as well as the adverse events (AEs). All outcome measurements were measured at the end of 12-week treatment, and 4-week follow-up after treatment.
Results:
At the end of the 12-week treatment, and 4-week follow-up, the patients receiving PNMES exhibited more decrease in the mean VAS (P < .01), and NDI (P < .01) respectively, compared with the patients receiving sham PNMES. Additionally, the increase in the mean ROM was also significantly higher in the PNMES group than that in the sham PNMES group at the end of the 12-week treatment, and 4-week follow-up, respectively (P < .01). No AEs were found in either group.
Conclusions:
The results of this study demonstrated that PNMES is more effective than Sham PNMES for neck pain relief in patients with CS.
Keywords: cervical spondylosis, clinical trial, effect, neck pain, percutaneous neuromuscular electrical stimulation, safety
1. Introduction
Cervical spondylosis (CS) is a very common age-related chronic disc degeneration condition.[1–4] It often involves the unspecified degenerative changes of the muscles, tendons, joints, and bones of the neck and shoulder.[5–9] Many etiological factors can lead to this condition, including poor posture, anxiety, depression, neck strain, and sporting activities.[10–13] It mainly manifests with neck pain, neck stiffness, and sometimes accompanied by numbness and radicular pain in the shoulders, arms, and fingers. It is reported that the overall prevalence of neck pain ranges from 0.4% to 86.8%, and its incidence varies from 10.4% to 21.3% in a high-risk population.[14] For example, previous UK study reported that around two-thirds of adults experienced the neck pain at some time in their lives.[15] Other study in Hong Kong found that its prevalence was from 15% to 17%, and the lifetime prevalence was 30% to 50%.[16]
Presently, although a variety of treatments are available for neck pain relief of CS, such as nonsteroidal anti-inflammatory drugs,[17] physiotherapy,[18,19] analgesics,[20,21] among others, those therapies have limited efficacy in relieving neck pain and many of them are associated with cumbersome side effects. It has been reported that alternative medicine, such as acupuncture,[22] neck exercise,[18,23] percutaneous neuromuscular electrical stimulation (PNMES),[24] herbal medication,[25] and so on, has been widely used to treat neck pain of CS, and with few adverse events (AEs), or even without AEs. However, no randomized controlled trials focused to explore the effectiveness and safety of PNMES for neck pain relief in patients with CS.
In this study, we hypothesized that PNMES therapy for neck pain relief in patients with CS after 12 weeks of treatment would be superior to the effectiveness of sham PNMES intervention. Thus, we designed this double-blinded, randomized, sham-controlled trial to assess the effectiveness of PNMES therapy for neck pain relief in patients with CS.
2. Methods
2.1. Study design
A 2-arm, double-blinded, randomized, sham-controlled trial compared a PNMES group with a control group were consisted in this study. This trial was approved by the ethics committee of The People's Hospital of Yan’an and it was also conducted at the same hospital from November 2014 to October 2016. One hundred and twenty-four patients with neck pain of CS were included and were randomly allocated to a PNMES group and a control group in a 1:1 ratio. The participants in the PNMES group were given PNMES, whereas the patients in the control group received sham PNMES at the same administration of treatment schedule as the PNMES group. The outcome measurements were assessed at the end of 12-week treatment, and 4-week follow-up after the treatment. All patients were required to provide written informed consent.
2.2. Patients
Patients were included with the following criteria: confirmed diagnosis of neck pain of CS according to the diagnostic criteria published by the International Classification of Diseases, 10th edition code: M47.812;[26] diagnosis of CS supported by a physical examination, and cervical radiographic examination, including anteroposterior and lateral x-rays, or magnetic resonance imaging/computed tomography scans; 18 to 70 years’ old; have a history of neck pain longer than 3 months; and no PNMES or other related treatment has been received 1 month before the study. Exclusion criteria were previous history of neck trauma, cervical facture or surgery, congenital spinal abnormality, spinal tumor or cancer, and other systematic disease of the neck including bones and joints conditions, or other severe neurologic, psychiatric, kidney, digestive system disorders, and pregnancy.
2.3. Randomization and blinding
Randomization scheme was conducted by the computerized number generator with SAS package 8.2 (SAS Institute Inc., Cary, NC. Patients who met the inclusion criteria were allocated randomly into a PNMES group and a control group in a 1:1 ratio. The randomization sequence schedule of group assignments and detail interventions were prepared by a statistician, who was blinded in this study, and were sealed in opaque envelops. The allocations were masked to the patients, investigators, and data analyst and outcome assessors.
2.4. Intervention
Patients received either PNMES or sham PNMES at bilateral acupoints of Jing-jiaji (EX-B2.C4, on the back of the neck, 0.5 cun lateral to the lower border of each spinous process between the fourth and fifth cervical vertebras), Jing-jiaji (EXB2. C5, on the back of the neck, 0.5 cun lateral to the lower border of each spinous process between the fifth and sixth cervical vertebras), and Jing-jiaji (EX-B2.C6, on the back of the neck, 0.5 cun lateral to the lower border of each spinous process between the fifth and sixth cervical vertebras) by using the PNMES device (HANS-100, Nanjing Jisheng Medical Technology Co., Ltd) at a frequency of 2 to 100 Hz for 30 minutes each session, 3 sessions weekly for a total of 12 weeks. Each device had 2 gel pads attached to a silicon patch. The patch was attached to the painful area. The power was turned on in the PNMES group, whereas it was kept off in the control group. The starting time of PNMES and the pain intensity were recorded immediately after its application.
2.5. Outcome measurements
The primary outcome was measured by the visual analog scale (VAS). The secondary measurements included cervical range of motion (ROM), and neck disability index (NDI) score. A ROM tool was used to measure ROM of the cervical spine.[27,28] It consists of flexion, extension, right bending, left bending, right rotation, and left rotation. Pain intensity was measured by a 10-cm VAS scale, with 0 = “no Pain” and 10 = “the worst imaginable pain,”[29] and first section in the NDI (1–100). In addition, NDI was also used to evaluate the functional activity of neck.[30,31] All outcome measurements were evaluated at the end of 12-week treatment, and 4-week follow-up after the treatment. In addition, AEs were also recorded duration the period of treatment.
2.6. Statistical analysis
The data analysis was conducted by using SAS package 8.2 (SAS Institute Inc., Cary, NC). The sample size was calculated based on the designed detection of a between group difference of 2.19 mm in pain intensity of VAS score. It was calculated according to the results of a previous study, with 1.61 mm in the intervention group, and 2.99 mm in the control group.[32] The minimum size of each group was estimated at 54 patients with α = 0.5, β = 0.8. Assuming a 15% drop-out rate, the required sample size of this study was therefore estimated to be 124 patients, with 62 assigned to each group. All outcome data were analyzed by intention-to-treat approach. t Test or Mann–Whitney rank sum test was used to analyze the continuous data. Pearson χ2 test or Fisher exact test was used to analyze the categorical data. The statistical significance level was set at P < .05.
3. Results
The patient's selection process is shown in Figure 1. At first, 197 participants were entered and were screened the study (Fig. 1). Then, 73 patients were excluded because of the failure to meet inclusion criteria (n = 45), rejection to sign informed consent (n = 16), and meeting the exclusion criteria (n = 12). Thus, 124 patients were included in this study, and were randomly and equally divided into 2 groups. Nine patients withdrew from this study because of the consent withdrawal (n = 5), and moved to the other cities (n = 4) (Fig. 1).
Figure 1.

Flowchart of participants throughout the study.
The characteristics of all included patients in both groups are listed in Table 1. No significant differences regarding all characteristics were found between 2 groups (Table 2).
Table 1.
Comparison of patients characteristics at baseline.
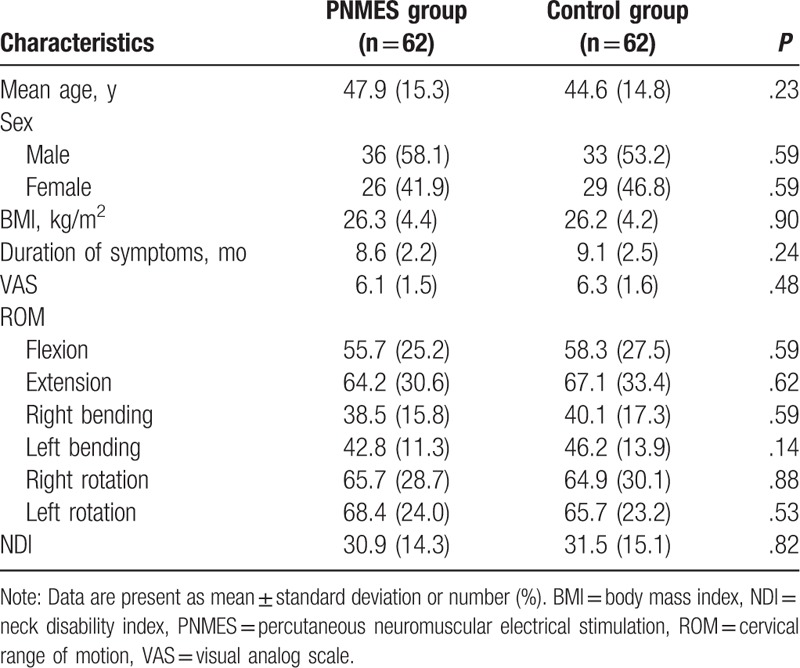
Table 2.
Outcome measurements at the end of the 12-week treatment and 4-week follow-up.

Results of the primary and secondary outcome measurements are shown in Table 2. At the end of the 12-week treatment, the patients in the PNMES group showed more decrease in VAS (P < .01) and NDI (P < .01) (Table 2), when compared patients in the control group. Additionally, it also demonstrated higher increase in ROM in patients receiving PNMES, compared with patients receiving sham PNMES (P < .01, Table 2). Furthermore, the significant differences were also found in VAS (P < .01), NDI (P < .01), and ROM (P < .01) at the end of 4-week follow-up after the treatment between 2 groups (Table 2). No AEs or side effects such as discomfort related to PNMES or sham PNMES intervention occurred in both groups during the period of the treatment and follow-up.
4. Discussion
Previous study investigated the immediate and short-term effects of the combination of the dry needling (DN) and percutaneous electrical nerve stimulation (PENS) compared to DN alone to treat the upper trapezius muscle.[24] It is designed as a 72-hour follow-up single-blinded randomized controlled trial and 62 subjects suffered from chronic myofascial neck pain with active myofascial trigger points in the upper trapezius muscle.[24] The results found that PENS combined with DN therapy was more effective than DN alone for reducing soreness in the short term and decreasing neck pain intensity immediately in patients with chronic neck pain.[24] The results of our study are consistent with this study. However, our study evaluated the effect of PNMES therapy with 12-week treatment and 4-week follow-up after the treatment.
The results of this study confirmed our hypothesis that PNMES intervention showed promising effectiveness for neck pain relief in patients with CS after 12-week treatment compared with sham PNMES intervention. To our knowledge, this study is the first double-blinded, randomized, sham-controlled trial that has been conducted among the Chinese population. It aimed to assess PNMES as an alternative therapy to treat neck pain of CS. Our results showed the encouraging effectiveness of PNMES therapy for neck pain relief in patients with CS.
The decrease in VAS and NDI was significantly greater for patients in the PNMES group compared with sham PNMES-treated patients. These results indicate the promising effect of PNMES for enhancing the symptoms of CS. Furthermore, this kind of intervention also appears encouraging for improving the ROM in patients with CS.
Although the promising effect of PNMES, this study still has 2 limitations. First, this study was conducted in only 1 center, which may impact the generalization of our results to the other hospitals. Second, this study failed to assess the comprehensive outcomes, such as the quality of life of patients in both groups.
5. Conclusion
This study found that PNMES can reduce neck pain in patients with CS effectively. However, further studies are still needed to warrant the present results.
Author contributions
Conceptualization: Yan-li Jin, Qiang Miao, Jian-hong Qiang.
Data curation: Yan-li Jin, Qiang Miao, Jian-hong Qiang.
Formal analysis: Qiang Miao.
Investigation: Qiang Miao, Jian-hong Qiang.
Methodology: Qiang Miao.
Project administration: Yan-li Jin, Qiang Miao.
Resources: Yan-li Jin, Jian-hong Qiang.
Software: Qiang Miao.
Supervision: Qiang Miao.
Validation: Yan-li Jin, Jian-hong Qiang.
Visualization: Yan-li Jin, Jian-hong Qiang.
Writing – original draft: Yan-li Jin, Jian-hong Qiang.
Writing – review & editing: Yan-li Jin, Jian-hong Qiang.
Footnotes
Abbreviations: AEs = adverse events, CS = cervical spondylosis, DN = dry needling, NDI = neck disability index, PNMES = percutaneous neuromuscular electrical stimulation, ROM = range of motion, VAS = visual analog scale.
The authors report no conflicts of interest.
References
- [1].Bai C, Li K, Guo A, et al. Indication for hypertrophy posterior longitudinal ligament removal in anterior decompression for cervical spondylotic myelopathy. Medicine (Baltimore) 2017;96:e7043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Liu L, Liu YB, Sun JM, et al. Preoperative deep vein thrombosis in patients with cervical spondylotic myelopathy scheduled for spinal surgery. Medicine (Baltimore) 2016;95:e5269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sun ZR, Yue JH, Tian HZ, et al. Acupuncture at Houxi (SI 3) acupoint for acute neck pain caused by stiff neck: study protocol for a pilot randomised controlled trial. BMJ Open 2014;4:e006236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sun Y, Wang H, Yang D, et al. Characterization of radiographic features of consecutive lumbar spondylolisthesis. Medicine (Baltimore) 2016;95:e5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zhang J, Meng F, Ding Y, et al. Hybrid surgery versus anterior cervical discectomy and fusion in multilevel cervical disc diseases: a meta-analysis. Medicine (Baltimore) 2016;95:e3621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [6].Sun ZR, Yue JH, Zhang QH. Electroacupuncture at Jing-jiaji points for neck pain caused by cervical spondylosis: a study protocol for a randomized controlled pilot trial. Trials 2013;14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wang T, Wang H, Liu S, et al. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion in multilevel cervical spondylotic myelopathy: a meta-analysis. Medicine (Baltimore) 2016;95:e5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhang Q, Yue J, Zeng X, et al. Acupuncture for chronic neck pain: a protocol for an updated systematic review. Syst Rev 2016;5:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yu CC, Gao WJ, Yang JS, et al. Can tranexamic acid reduce blood loss in cervical laminectomy with lateral mass screw fixation and bone grafting: a retrospective observational study. Medicine (Baltimore) 2017;96:e6043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chen C, Zhang X, Ma X. Durability of cervical disc arthroplasties and its influence factors: A systematic review and a network meta-analysis. Medicine (Baltimore) 2017;96:e5947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Xue D, Chen Q, Chen G, et al. Posterior arthrodesis of C1-C3 for the stabilization of multiple unstable upper cervical fractures with spinal cord compromise: a case report and literature review. Medicine (Baltimore) 2017;96:e5841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lu X, Tian Y, Wang SJ, et al. Relationship between the small cervical vertebral body and the morbidity of cervical spondylosis. Medicine (Baltimore) 2017;96:e7557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kong L, Tian W, Cao P, et al. Predictive factors associated with neck pain in patients with cervical disc degeneration: A cross-sectional study focusing on Modic changes. Medicine (Baltimore) 2017;96:e8447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hoy DG, Protani M, De R, et al. The epidemiology of neck pain. Best Pract Res Clin Rheumatol 2010;24:783–92. [DOI] [PubMed] [Google Scholar]
- [15].Cassidy JD, Carroll L. The Saskatchewan health and back pain survey: the prevalence of neck pain and related disability in Saskatchewan adults. Spine 1998;23:1689–98. [DOI] [PubMed] [Google Scholar]
- [16].Lau EM, Sham A, Wong KC. The prevalence of and risk factors for neck pain in Hong Kong Chinese. J Public Health Med 1996;18:396–9. [DOI] [PubMed] [Google Scholar]
- [17].Day RO, Rowett D, Roughead EE. Towards the safer use of non-steroidal anti-inflammatory drugs. J Qual Clin Pract 1999;19:51–3. [DOI] [PubMed] [Google Scholar]
- [18].Jay K, Brandt M, Jakobsen MD, et al. Ten weeks of physical-cognitive-mindfulness training reduces fear-avoidance beliefs about work-related activity: Randomized controlled trial. Medicine (Baltimore) 2016;95:e3945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Landén Ludvigsson M, Peolsson A, Peterson G, et al. Cost-effectiveness of neck-specific exercise with or without a behavioral approach versus physical activity prescription in the treatment of chronic whiplash-associated disorders: Analyses of a randomized clinical trial. Medicine (Baltimore) 2017;96:e7274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kim DH, Choi JY, Kim BG, et al. Prospective, randomized, and controlled trial on ketamine infusion during bilateral axillo-breast approach (BABA) robotic or endoscopic thyroidectomy: Effects on postoperative pain and recovery profiles: A consort compliant article. Medicine (Baltimore) 2016;95:e5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lee YH, Kim YS, Chung MJ, et al. Soft Tissue Necrosis in Head and Neck Cancer Patients After Transoral Robotic Surgery or Wide Excision With Primary Closure Followed by Radiation Therapy. Medicine (Baltimore) 2016;95:e2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yue JH, Zhang QH, Wang SL, et al. Research progress of electroacupuncture treatment on cervical spondylosis radiculopathy in recent ten years. J Acupuncture Tuina Sci 2011;2:127–32. [Google Scholar]
- [23].Overmeer T, Peterson G, Landén Ludvigsson M, et al. The effect of neck-specific exercise with or without a behavioral approach on psychological factors in chronic whiplash-associated disorders: A randomized controlled trial with a 2-year follow-up. Medicine (Baltimore) 2016;95:e4430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].León-Hernández JV, Martín-Pintado-Zugasti A, Frutos LG, et al. Immediate and short-term effects of the combination of dry needling and percutaneous TENS on post-needling soreness in patients with chronic myofascial neck pain. Braz J Phys Ther 2016;20:422–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hedaya R. Five herbs plus thiamine reduce pain and improve functional mobility in patients with pain: a pilot study. Altern Ther Health Med 2017;23:14–9. [PubMed] [Google Scholar]
- [26].International Statistical Classification of Diseases and Related Health Problems 10th Revision Version for 2007. Available at: http://apps.who.int/classifications/apps/icd/icd10online/. [Google Scholar]
- [27].Tousignant M, Duclos E, Lafleche S, et al. Validity study for the cervical range ofmotion device used for lateral flexion in patients with neck pain. Spine (Phila Pa 1976) 2002;27:812–7. [DOI] [PubMed] [Google Scholar]
- [28].Tousignant M, Smeesters C, Breton AM, et al. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J Orthop Sports Phys Ther 2006;36:242–8. [DOI] [PubMed] [Google Scholar]
- [29].Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227–36. [DOI] [PubMed] [Google Scholar]
- [30].Shaheen AA, Omar MT, Vernon H. Cross-cu2ltural adaptation, reliability, and validity of the Arabic version of neck disability index in patients with neck pain. Spine (Phila Pa 1976) 2013;38:E609–615. [DOI] [PubMed] [Google Scholar]
- [31].Yao M, Sun YL, Cao ZY, et al. A Systematic Review of Cross-cultural Adaptation of the Neck Disability Index. Spine (Phila Pa 1976) 2015;40:480–90. [DOI] [PubMed] [Google Scholar]
- [32].Cerezo-Te’ llez E, Torres-Lacomba M, Fuentes-Gallardo I, et al. Dry needling of the trapezius muscle in office workers with neck pain: a randomized clinical trial. J Man Manip Ther 2016;24:223–32. [DOI] [PMC free article] [PubMed] [Google Scholar]


