Abstract
Rationale:
Among all dermatomyositis (DM) patients, antimelanoma differentiation-associated gene 5 antibody (anti-MDA5 Ab) positive patients have significantly poor short-term mortality, whereas they experience less relapses over the long term after the remission. We report the case of a patient with anti-MDA5 Ab-positive clinically amyopathic dermatomyositis (CADM) with the recurrence of interstitial lung disease (ILD) after 7 years of remission. There has been no case report of an anti-MDA5 Ab-positive DM patient with the recurrence of ILD after 7 years of long-term remission.
Patient concerns:
A 70-year-old Japanese woman was diagnosed with anti-MDA5 Ab-positive CADM and ILD. After achieving 7 years long-term remission, she was admitted to our department with erythema on the fingers and interstitial pneumonia. Her anti-MDA5 Ab titer was elevated.
Diagnoses:
We diagnosed recurrent CADM complicated with ILD.
Interventions:
We successfully treated her with 1,000 mg of methyl-prednisolone pulse and intravenous cyclophosphamide therapy followed by prednisolone 50 mg/day and an increase of cyclosporine.
Outcomes:
After that treatment, the patient's skin symptoms and interstitial pneumonia were relieved. All laboratory investigations such as ferritin, the serum markers of interstitial pneumonia (i.e., SP-A, SP-D), and the titer of anti-MDA5 Ab showed signs of improvement.
Lessons:
Her case suggests that careful physical examinations and monitoring the serum markers are important even after long-term remission is achieved.
Keywords: anti-MDA5 antibody, clinically amyopathic dermatomyositis, dermatomyositis, interstitial pneumonia
1. Introduction
Dermatomyositis (DM) characterized by amyopathy or hypomyopathy with the typical skin symptoms is defined as clinically amyopathic dermatomyositis (CADM).[1] Among DM patients, antimelanoma differentiation-associated gene 5 antibody (anti-MDA5 Ab) has been identified as a new autoantibody.[2,3] It has been widely recognized that anti-MDA5 Ab-positive DM patients frequently develop rapidly progressive interstitial lung disease (RPILD) with poor prognosis.[2,4]
Among all DM patients, the anti-MDA5 Ab-positive patients have significantly poor short-term mortality over the first 6 months after diagnosis, whereas no significant difference in the long-term mortality over the first 2 years post-diagnosis was observed between anti-MDA5 Ab-positive patients and anti-MDA5 Ab-negative patients, suggesting that anti-MDA5 Ab-positive patients experience less relapses over the long term.[5] However, there have been no sufficient studies of the long-term prognosis and relapse rate of anti-MDA5 Ab-positive DM patients after remission.
We herein report the case of a patient with anti-MDA5 Ab-positive CADM with the recurrence of interstitial lung disease (ILD) after 7 years of remission, treated successfully by a combination of corticosteroids, cyclophosphamide and calcineurin inhibitor.
2. Case report
In October 2010, a 70-year-old Japanese woman was diagnosed with ILD and CADM based on the findings of rash on the fingers of both hands, interstitial pneumonia, and a high titer of anti-MDA5 Ab (148 index). We administered 1000 mg of methyl-prednisolone (mPSL) pulse therapy and intravenous cyclophosphamide therapy (IVCY) followed by prednisolone (PSL) 50 mg/day with tapering and cyclosporine (CyA), and the symptoms were improved by a total of 5 IVCY continuations. After that, the patient maintained long-term remission for approximately 7 years, and she was treated with oral PSL 3 mg/day and CyA 100 mg/day. However, in November 2017, she suffered from nasal discharge, feeling heaviness of her head, and fatigue. In December 2017, she also presented with rash on both her fingers and toes, and she was then admitted to our department.
On admission, her body temperature was 37.1°C; her blood pressure was 141/76 mm Hg, the heart rate was 86 beats/min, and the pulse oximetric saturation (SpO2) was 95% (room air). On physical examination, fine crackles were audible on the dorsal side of the bilateral lower lung regions, and she had erythemas on the nail circumference and both dorsal and palm sides around the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints, suggesting Gottron's sign and inverse Gottron's sign, respectively (Fig. 1). She had no muscle pain, and a manual muscle test showed no abnormalities in the upper and lower limbs.
Figure 1.

Erythemas on the nail circumference and both dorsal and palm sides around the PIP and MCP joints. MCP = metacarpophalangeal (MCP), PIP = proximal interphalangeal.
Laboratory investigations showed the following results: partial pressure of arterial oxygen (PaO2) 73.5 mm Hg, white blood cell count (WBC) 9400 /μL (neutrophils 89.5%, lymphocytes 9.3%), hemoglobin (Hb) 12.1 g/dL, platelet (PLT) 27.0 × 104/μL, C-reactive protein (CRP) 3.4 mg/dL, lactate dehydrogenase (LDH) 231 IU/mL (normal range 124–222), ferritin 319 ng/mL (normal range 6.0–138). The levels of creatinine kinase and aldolase were 79 IU/L and 3.6 IU/L, respectively (= within the normal range). Although the serum Krebs von den lungen (KL)-6 level was 274 U/mL (within the normal range), the levels of surfactant protein (SP)-A and SP-D were 49.3 and 140 ng/mL in slightly high titers. No abnormalities were revealed by a urinalysis, and no liver or renal dysfunction was detected.
The following immunological and serological results were all negative (the exception is anti-MDA5 antibody): rheumatoid factor (RF), antinuclear antibody (ANA), proteinase-3 anti-neutrophil cytoplasmic autoantibodies (PR3-ANCAs), myeloperoxidase anti-neutrophil cytoplasmic autoantibodies (MPO-ANCAs), anti-ARS antibody, anti-transcription intermediary factor 1-gamma (TIF1-γ) antibody, and angiotensin converting enzyme (ACE). The anti-MDA5 antibody titer index was 109 (normal range < 32). The results of assays of β-D-glucan, T-SPOT. TB Legionella pneumophila, Streptococcus pneumonia, Mycoplasma pneumonia, Clamydia psittaci, and Clamydia pneumonia were all negative. A chest computed tomography (CT) examination showed the expression of invasive shadows on lung field under the pleura and on the dorsal side of the bilateral lower lobes (Fig. 2A), suggesting an exacerbation of interstitial pneumonia.
Figure 2.
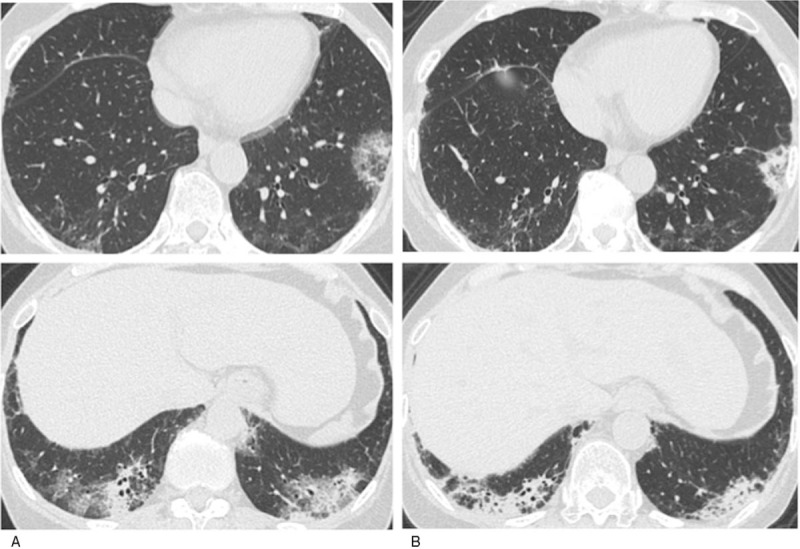
A chest CT on admission showed the expression of invasive shadows on lung field under the pleura and on the dorsal side of the bilateral lower lobes (A), after strengthening treatment it showed contraction of invasive shadows (B).
We diagnosed the patient as having recurrent CADM complicated with ILD based on the findings of the typical skin symptoms, the exacerbation of interstitial pneumonia, and a high titer of anti-MDA5 Ab. We then administered 1,000 mg of mPSL pulse therapy and IVCY followed by PSL 50 mg/day with tapering and an increase of CyA from 100 mg to 150 mg. After that treatment, the patient's skin symptoms and interstitial pneumonia were relieved (Fig. 2B). All laboratory investigations such as ferritin, the serum markers of interstitial pneumonia (i.e., SP-A, SP-D), and the titer of anti-MDA5 Ab showed signs of improvement. We administered a total of 2 sessions of IVCY continuation, and the patient's remission has now been maintained for over 1 months as of this writing (Fig. 3). We measured the antisplicing factor proline/glutamine-rich protein antibody (anti-SFPQ Ab) using her preserved serum and found that anti-SFPQ Ab at the initial diagnosis was negative, but it turned positive at the recurrence.
Figure 3.
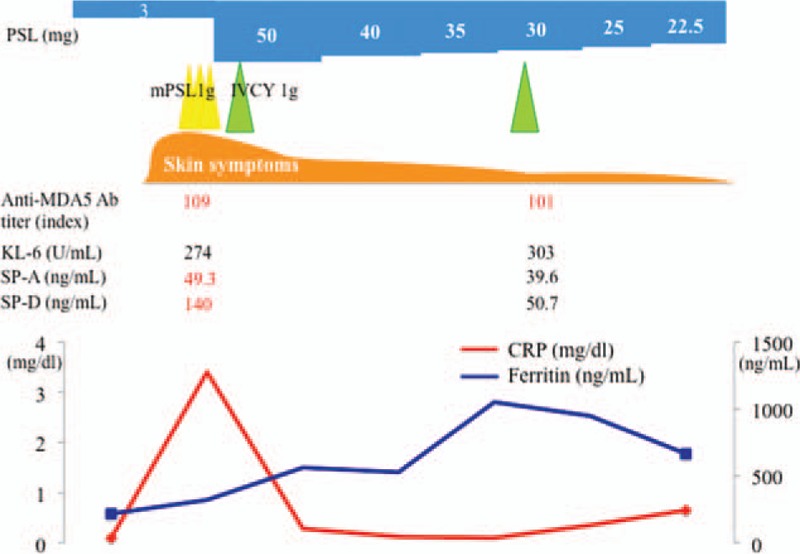
The clinical course of the patient, a 70-year-old Japanese woman. The CRP, ferritin level, and the treatment interventions during the hospital course are shown. CRP = C-reactive protein, IVCY = intravenous cyclophosphamide therapy, mPSL = methyl-prednisolone.
3. Discussion
We treated an anti-MDA-5 Ab-positive patient with recurrent CADM complicated by ILD who had maintained long-term remission for approximately 7 years after the initial diagnosis of the disease. Her case provides significant information about the mechanisms underlying the onset of ILD, the long-term prognosis, and the treatment strategies after the remission among anti-MDA-5 Ab-positive patients.
Melanoma differentiation-associated gene 5 (MDA5), which is the target autoantigen against anti-MDA5 Ab, belongs to the retinoic acid-inducible gene I (RIG-I) family and plays important roles in the innate immune system during virus infections through antiviral cytokines such as type I interferon (IFN) and tumor necrosis factor-alpha (TNF-α).[6,7] Each protein molecule in the RIG-I family recognizes a different type of virus, and MDA5 is a molecule necessary for recognizing picornaviruses including coxsackievirus,[8] suggesting that the production of anti-MDA5 Ab and the onset of CADM complicated with ILD are autoimmune phenomena induced by viral infection.[3,9]
In order to fully understand the clinical symptoms and prognosis of anti-MDA5 Ab-positive cases, it is necessary to consider differences among races and geographic regions. Japanese reports of anti-MDA5 Ab-positive DM patients demonstrated the following prevalences: CADM, approximately 80%; ILD, approximately 90%; RPILD, approximately 70%; and mortality, approximately 30%–50%,[3,9–13] indicating anti-MDA5 Ab-positive DM patients have poor prognoses. In addition, according to the reports from other East Asian countries, there was no significant difference in the prevalence of RPILD or the mortality rate between these countries and Japan. However, most of those reports showed that the prevalence of CADM is ≤40% in other East Asian countries, suggesting that this prevalence of anti-MDA5 Ab-positive CADM is much lower than that of Japan.[14–17] In North America, the prevalence of CADM is approximately 50%, whereas the prevalence of RPILD is approximately 20%, indicating that the prevalence of RPILD with anti-MDA5 Ab-positive is much lower than that of Japan.[18,19]
These racial and regional differences may be due to genetic backgrounds and environmental factors. The frequency of anti-MDA5 antibody-positive cases was reported to be higher around the Kiso River in Japan,[20] suggesting environmental involvement. There are also several reports that anti-MDA5 antibody-positivity is more frequent among individuals with HLA-DRB1 gene polymorphism,[21–23] which suggests genetic involvement. Although the mechanisms underlying the onset of ILD in anti-MDA5 Ab-positive DM patients have not been elucidated, the case of our present patient (who experienced 2 episodes of onset) suggests a genetic factor rather than an environmental factor.
Our patient's case showed that serum anti-SFPQ Ab turned to be positive at the recurrence. Anti-SFPQ Ab is a new DM-specific autoantibody, which is particularly specific for anti-MDA5 Ab-positive DM.[24] SFPQ is a multifunctional nuclear protein associated with the human gene expression pathway, RNA production and processing, and viral infection.[24,25] Because both SFPQ and MDA5 have important roles in viral infection, the recurrent disease in our patient's case may suggest an association with viral infection. A previous report showed that there was no significant difference in the frequency of the recurrent between anti-SFPQ Ab-positive (n = 27) and -negative (n = 24) patients with anti-MDA5 Ab-positive DM, but all 5 anti-MDA5 Ab-positive patients who showed the recurrence were anti-SFPQ Ab-positive.[24] Our patient's case may suggest an association between the recurrent and the appearance of anti-SFPQ Ab.
Measuring the anti-MDA5 Ab level is a novel tool for monitoring disease activity in RPILD with DM,[26] and hyperferritinemia predicts poor prognosis, especially if the ferritin level is >1600 ng/mL.[27] The anti-MDA5 Ab, ferritin, and IL-18 levels in the serum are also useful for the evaluation of response to treatment in ILD patients with anti-MDA5 Ab-positive DM.[12] In other words, the anti-MDA5 Ab level is a novel parameter for monitoring and a good predictor of RPILD relapse in patients with DM.[28] It was reported that 4 of 12 patients with RPILD relapsed with anti-MDA5 antibody-positive DM in both an anti-MDA5 antibody sustained-positive group and the negative conversion group; the same study showed that RPILD relapses are associated with a re-increase in anti-MDA5 Ab level in all patients (4/4), and also showed that patients with a sustained high titer of anti-MDA5 Ab tend to relapse earlier than those with who are negative for anti-MDA5 Ab.[28] In our patient's case, the ferritin level during the remission after the initial treatment was sustained at a mildly high level at 200 ng/mL, but we did not monitor her anti-MDA5 antibody titer during the remission; we feel that from now on it is necessary to monitor the anti-MDA5 antibody titer as well as the ferritin level.
Although the recurrence of ILD among anti-MDA5 Ab positive-patients had been believed to be less until now, it is important in actual clinical practice to predict the recurrence at an early stage from clinical signs. Our patient presented no respiratory symptoms at the recurrence, but we suspected the onset of a recurrence because of the characteristics of her skin symptoms, leading to the early detection of ILD exacerbation. Accordingly, the careful examination on her skin symptoms was extremely important not only at the initial diagnosis but also at the evaluation of the recurrence.
As the initial treatment of RPILD with anti-MDA5 Ab-positive DM patients, the combination of corticosteroids, cyclophosphamide, and calcineurin inhibitor is recommended.[29] However, there are no established treatment guidelines for the prevention of recurrence during remission. Our patient had been treated with oral administration of PSL 3 mg/day and CyA 100 mg/day during the remission, but her ILD eventually was recurred, accompanied by skin lesions. Anti-MDA5 Ab-positive DM patients had a lower relapse rate during the 2 years after the initial treatment compared to other DM patients.[4,5] However, it has been only about 10 years since DM patients with anti-MDA5 antibody-positive were well recognized. Although our patient's case indicates the possibility that ILD can be recurred after long-term remission, further investigation is needed to clarify the long-term prognosis among anti-MDA5 Ab-positive DM patients.
In conclusion, we successfully treated an anti-MDA5 Ab-positive CADM patient with a recurrence of ILD after she achieved long-term remission (approximately 7 years). It is commonly recognized that anti-MDA5 Ab-positive DM patients have significantly poor short-term mortality, whereas the long-term prognosis of these patients is relatively good. However, we would like to emphasize the necessity of careful monitoring for the recurrence of ILD, even after a patient achieves long-term remission. Our patient's case suggests that careful physical examinations of skin symptoms as well as the serum markers including the titer of MDA5 Ab during the remission of ILD provide a chance to make an early diagnosis of the recurrence and early intensive treatment.
Author contributions
Investigation: Yuji Hosono, Tsuneyo Mimori.
Supervision: Tomohiro Koga, Midori Ishida, Yuya Fujita, Sosuke Tsuji, Ayuko Takatani, Toshimasa Shimizu, Remi Sumiyoshi, Takashi Igawa, Masataka Umeda, Shoichi Fukui, Ayako Nishino, Shin-ya Kawashiri, Naoki Iwamoto, Kunihiro Ichinose, Mami Tamai, Hideki Nakamura, Tomoki Origuchi, Masataka Kuwana, Atsushi Kawakami.
Writing – original draft: Yushiro Endo.
Footnotes
Abbreviations: anti-MDA5 Ab = antimelanoma differentiation-associated gene 5 antibody, anti-SFPQ Ab = anti-splicing factor proline/glutamine-rich protein antibody, CADM = clinically amyopathic dermatomyositis, CyA = cyclosporine., DM = dermatomyositis, ILD = interstitial lung disease, IVCY = intravenous cyclophosphamide therapy, mPSL = methyl-prednisolone, PSL = prednisolone, RPILD = rapidly progressive interstitial lung disease.
Patient Consent: Written informed consent was obtained from the patient by the corresponding author.
Conflicts of Interest: KM holds a patent on anti-MDA5 antibody-measuring kits and the other authors have no conflicts of interest to disclose.
References
- [1].Sontheimer RD. Would a new name hasten the acceptance of amyopathic dermatomyositis (dermatomyositis sine myositis) as a distinctive subset within the idiopathic inflammatory dermatomyopathies spectrum of clinical illness? J Am Acad Dermatol 2002;46:626–36. [DOI] [PubMed] [Google Scholar]
- [2].Sato S, Hirakata M, Kuwana M, et al. Autoantibodies to a 140-kd polypeptide, CADM-140, in Japanese patients with clinically amyopathic dermatomyositis. Arthritis Rheum 2005;52:1571–6. [DOI] [PubMed] [Google Scholar]
- [3].Sato S, Hoshino K, Satoh T, et al. RNA helicase encoded by melanoma differentiation-associated gene 5 is a major autoantigen in patients with clinically amyopathic dermatomyositis: association with rapidly progressive interstitial lung disease. Arthritis Rheum 2009;60:2193–200. [DOI] [PubMed] [Google Scholar]
- [4].Koga T, Fujikawa K, Horai Y, et al. The diagnostic utility of anti-melanoma differentiation-associated gene 5 antibody testing for predicting the prognosis of Japanese patients with DM. Rheumatology (Oxford) 2012;51:1278–84. [DOI] [PubMed] [Google Scholar]
- [5].Isoda K, Kotani T, Takeuchi T, et al. Comparison of long-term prognosis and relapse of dermatomyositis complicated with interstitial pneumonia according to autoantibodies: anti-aminoacyl tRNA synthetase antibodies versus anti-melanoma differentiation-associated gene 5 antibody. Rheumatol Int 2017;37:1335–40. [DOI] [PubMed] [Google Scholar]
- [6].Yoneyama M, Kikuchi M, Matsumoto K, et al. Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity. J Immunol 2005;175:2851–8. [DOI] [PubMed] [Google Scholar]
- [7].Takeuchi O, Akira S. MDA5/RIG-I and virus recognition. Curr Opin Immunol 2008;20:17–22. [DOI] [PubMed] [Google Scholar]
- [8].Kato H, Takeuchi O, Sato S, et al. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature 2006;441:101–5. [DOI] [PubMed] [Google Scholar]
- [9].Nakashima R, Imura Y, Kobayashi S, et al. The RIG-I-like receptor IFIH1/MDA5 is a dermatomyositis-specific autoantigen identified by the anti-CADM-140 antibody. Rheumatology (Oxford) 2010;49:433–40. [DOI] [PubMed] [Google Scholar]
- [10].Hamaguchi Y, Kuwana M, Hoshino K, et al. Clinical correlations with dermatomyositis-specific autoantibodies in adult Japanese patients with dermatomyositis: a multicenter cross-sectional study. Arch Dermatol 2011;147:391–8. [DOI] [PubMed] [Google Scholar]
- [11].Fujikawa K, Kawakami A, Kaji K, et al. Association of distinct clinical subsets with myositis-specific autoantibodies towards anti-155/140-kDa polypeptides, anti-140-kDa polypeptides, and anti-aminoacyl tRNA synthetases in Japanese patients with dermatomyositis: a single-centre, cross-sectional study. Scand J Rheumatol 2009;38:263–7. [DOI] [PubMed] [Google Scholar]
- [12].Gono T, Sato S, Kawaguchi Y, et al. Anti-MDA5 antibody, ferritin and IL-18 are useful for the evaluation of response to treatment in interstitial lung disease with anti-MDA5 antibody-positive dermatomyositis. Rheumatology (Oxford) 2012;51:1563–70. [DOI] [PubMed] [Google Scholar]
- [13].Hoshino K, Muro Y, Sugiura K, et al. Anti-MDA5 and anti-TIF1-gamma antibodies have clinical significance for patients with dermatomyositis. Rheumatology (Oxford) 2010;49:1726–33. [DOI] [PubMed] [Google Scholar]
- [14].Kang EH, Nakashima R, Mimori T, et al. Myositis autoantibodies in Korean patients with inflammatory myositis: anti-140-kDa polypeptide antibody is primarily associated with rapidly progressive interstitial lung disease independent of clinically amyopathic dermatomyositis. BMC Musculoskelet Disord 2010;11:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chen F, Wang D, Shu X, et al. Anti-MDA5 antibody is associated with A/SIP and decreased T cells in peripheral blood and predicts poor prognosis of ILD in Chinese patients with dermatomyositis. Rheumatol Int 2012;32:3909–15. [DOI] [PubMed] [Google Scholar]
- [16].Cao H, Pan M, Kang Y, et al. Clinical manifestations of dermatomyositis and clinically amyopathic dermatomyositis patients with positive expression of anti-melanoma differentiation-associated gene 5 antibody. Arthritis Care Res (Hoboken) 2012;64:1602–10. [DOI] [PubMed] [Google Scholar]
- [17].Chen Z, Cao M, Plana MN, et al. Utility of anti-melanoma differentiation-associated gene 5 antibody measurement in identifying patients with dermatomyositis and a high risk for developing rapidly progressive interstitial lung disease: a review of the literature and a meta-analysis. Arthritis Care Res (Hoboken) 2013;65:1316–24. [DOI] [PubMed] [Google Scholar]
- [18].Fiorentino D, Chung L, Zwerner J, et al. The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol 2011;65:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hall JC, Casciola-Rosen L, Samedy LA, et al. Anti-melanoma differentiation-associated protein 5-associated dermatomyositis: expanding the clinical spectrum. Arthritis Care Res (Hoboken) 2013;65:1307–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Muro Y, Sugiura K, Hoshino K, et al. Epidemiologic study of clinically amyopathic dermatomyositis and anti-melanoma differentiation-associated gene 5 antibodies in central Japan. Arthritis Res Ther 2011;13:R214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gono T, Kawaguchi Y, Kuwana M, et al. Brief report: Association of HLA-DRB1∗0101/∗0405 with susceptibility to anti-melanoma differentiation-associated gene 5 antibody-positive dermatomyositis in the Japanese population. Arthritis Rheum 2012;64:3736–40. [DOI] [PubMed] [Google Scholar]
- [22].Lin JM, Zhang YB, Peng QL, et al. Genetic association of HLA-DRB1 multiple polymorphisms with dermatomyositis in Chinese population. HLA 2017;90:354–9. [DOI] [PubMed] [Google Scholar]
- [23].Chen Z, Wang Y, Kuwana M, et al. HLA-DRB1 alleles as genetic risk factors for the development of anti-MDA5 antibodies in patients with dermatomyositis. J Rheumatol 2017;44:1389–93. [DOI] [PubMed] [Google Scholar]
- [24].Hosono Y, Nakashima R, Serada S, et al. Splicing factor proline/glutamine-rich is a novel autoantigen of dermatomyositis and associated with anti-melanoma differentiation-associated gene 5 antibody. J Autoimmun 2017;77:116–22. [DOI] [PubMed] [Google Scholar]
- [25].Patton JG, Porro EB, Galceran J, et al. Cloning and characterization of PSF, a novel pre-mRNA splicing factor. Genes Dev 1993;7:393–406. [DOI] [PubMed] [Google Scholar]
- [26].Sato S, Kuwana M, Fujita T, et al. Anti-CADM-140/MDA5 autoantibody titer correlates with disease activity and predicts disease outcome in patients with dermatomyositis and rapidly progressive interstitial lung disease. Mod Rheumatol 2013;23:496–502. [DOI] [PubMed] [Google Scholar]
- [27].Gono T, Kawaguchi Y, Satoh T, et al. Clinical manifestation and prognostic factor in anti-melanoma differentiation-associated gene 5 antibody-associated interstitial lung disease as a complication of dermatomyositis. Rheumatology (Oxford) 2010;49:1713–9. [DOI] [PubMed] [Google Scholar]
- [28].Matsushita T, Mizumaki K, Kano M, et al. Antimelanoma differentiation-associated protein 5 antibody level is a novel tool for monitoring disease activity in rapidly progressive interstitial lung disease with dermatomyositis. Br J Dermatol 2017;176:395–402. [DOI] [PubMed] [Google Scholar]
- [29].Kameda H, Nagasawa H, Ogawa H, et al. Combination therapy with corticosteroids, cyclosporin A, and intravenous pulse cyclophosphamide for acute/subacute interstitial pneumonia in patients with dermatomyositis. J Rheumatol 2005;32:1719–26. [PubMed] [Google Scholar]


