Highlights
-
•
De Garengeot hernia is defined as femoral hernia containing the appendix.
-
•
De Garengeot hernia with appendicitis is a very rare surgical finding.
-
•
Diagnosis most often is made intraoperatively.
-
•
Treatment depends on complications of the hernia and the anatomical position of the appendix.
-
•
Prompt surgical treatment is essential in order to avoid severe complications.
Keywords: Femoral hernia, Appendicitis, Appendicectomy
Abstract
Background
De Garengeot hernia is defined as femoral hernia containing appendix. An acute appendicitis in a femoral hernia is a extremely unusual surgical finding and occurs in 0.08%–0.013% of all cases.
Case report
We report the case of an elderly woman, who presented with a typical clinical image of incarcerated femoral hernia and underwent open surgery. An infrainguinal incision was performed and after the dissection of hernia sac, an acute appendicitis within femoral hernia was revealed. Subsequently, appendectomy and hernioplasty were performed.
Conclusion
Acute appendicitis within femoral hernia should be included in differential diagnosis of patients presenting with clinical signs of an incarcerated femoral hernia and prompt surgical treatment is essential in order to avoid severe complications.
1. Introduction
Femoral hernia appears posterior and inferior below the inguinal ligament and occurs when abdominal content, abdominal viscera or omentum passes through the femoral ring into the femoral canal, medial to the femoral vein, artery and nerve. This type of hernia is more frequent in women, accounting for 3% of all abdominal wall hernias. De Garengeot hernia is defined as femoral hernia containing the appendix, occurring in approximately 1% of all femoral cases, while the presence of an appendicitis within a femoral hernia is even more rare, occurring in 0.08% to 0.13% of all cases [1]. De Garengeot hernia was first reported in 1731 by a French surgeon, in the name of Rene Jacques Croissant de Garengeot, and in 1785, Hevin first described an appendectomy for acute appendicitis on a patient with De Garengeot hernia [2]. De Garengeot hernia is diagnosed most times randomly during surgery and should be distinguished from Amyand hernia, which is defined as inguinal hernia containing the appendix and is a more frequent surgical finding due to higher prevalence of inguinal hernias [3]. We present a case of De Garengeot hernia with acute appendicitis, in a 90-year-old woman.
2. Case presentation
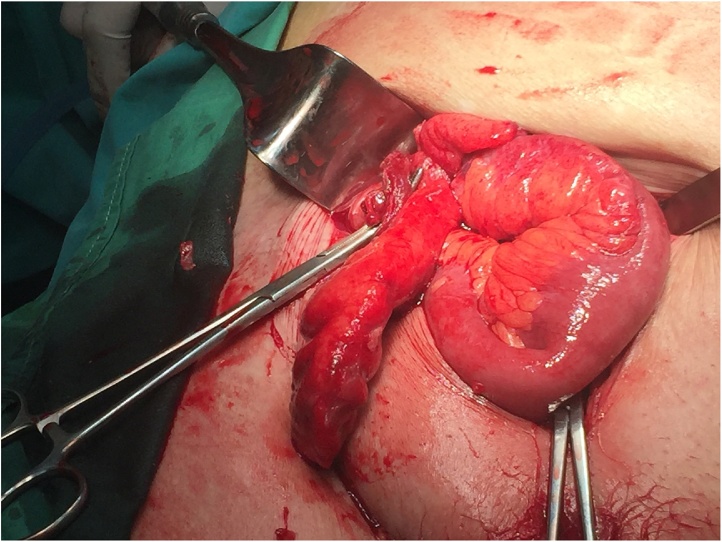
A 90-year-old woman was admitted at the emergency department complaining right lower abdominal pain and vomiting during the last 48 h. Her past medical history consists hypertension and diabetes mellitus type II. Upon physical examination, an irreducible and painful groin lump on palpation was observed below the right inguinal ligament. Laboratory findings showed leucocytosis (WBC: 13.500/mL) and an elevated CRP of 10 mg/dL. The other biochemistry tests were within normal limits. The patient was non febrile and stable hemodynamically. A femoral hernia was diagnosed and the patient underwent laparotomy under epidural anesthesia. An infrainguinal incision was performed. The femoral hernia was found out and was opened. An inflamed appendix within the sac was revealed (Fig. 1). Subsequently, appendectomy was performed and the hernia was repaired via hernioplasty, using a McVay technique. The postoperative course was uneventful and the patient was discharged after seven days. Furthermore, the patient followed up four weeks after being discharged and she had not developed any kind of wound infection and the incision was well-healed. She had no signs of recurrence.
Fig. 1.
Intraoperative picture showing the inflamed appendix as the content of femoral hernia.
3. Discussion
De Garengeot hernia is a very rare surgical finding and presents a higher prevalence in females, mainly in postmenopausal females, with a proportion rate of male to female 1:4 and occurs almost always in the right inguinal area. The narrow femoral ring may attribute to increased risk incarceration and strangulation of femoral hernia (5%–20%) compared to other abdominal wall hernias and the development of acute appendicitis. However, these tight anatomical structures of the femoral hernia may be a protective factor of intraperitoneal extension of infection and peritonitis development [1]. Furthermore, changes during pregnancy, increased abdominal pressure, smoking, aging, muscle and connective tissue disorders may be risk factors of De Garengeot hernia development, while the existence of appendix within a femoral hernia requires a pelvic appendix or low-positioned cecum [4]. In addition, the presence of an appendiceal diverticulum within hernia can lead to perforated appendiceal diverticulitis and necrotizing fasciitis. The perforation probably occurs after the incarceration of femoral hernia, as a result of increased intraluminal pressure [4]. De Garengeot hernia usually presents a groin lump, which is painful on palpation and irreducible. Patients can be feverish and in shock, as well as have signs of bowel obstruction, but there is usually no coexistence of peritonitis. Differential diagnosis should include other types of femoral hernia, such as Cloquet hernia and Serafini hernia, inguinal hernia, infected or necrotic lymphadenopathy, ectasia of the Vena saphena megna, lipomas or other soft tissue tumors and hypostatic abscesses in retroperitoneal processes [5]. Preoperative diagnosis of de Garengeot hernia is difficult and most often is made intraoperatively. However, it is essential for imaging examinations to be performed. Abdominal X-ray helps to exclude bowel obstruction and ultrasound is useful to reveal bowel in hernia sac, while in one case, the ultrasound diagnosed appendicitis within a femoral hernia preoperatively [6]. Additionally, Computer Tomography of the abdomen can assist in the exclusion of other disorders or establish the diagnosis, as well as in a review; CT was diagnostic in 44% of cases [1]. A typical CT image of de Garengeot hernia with appendicitis is a tubular structure with mural thickening and surrounding stranding of the fat and a low-positioned cecum [7]. However, because of the urgency of the situation, imaging tests are often not performed and diagnosis is established during the exploration of the inguinal area. If the therapy is delayed or the patient is left untreated, the inflammation may spontaneously resolve by itself or lead to life-threatening complications, which include necrosis of the hernia contents, bowel obstruction, necrotizing fasciitis and abscess formation [8]. With regard to therapy, there is no standard management of de Garengeot hernia, possibly due to the rarity of this entity, and the therapeutic strategy depends on the surgeon, complications of the hernia, the condition of the patient and the anatomical position of the appendix vermiformis (mobile cecum) [9]. Thus, the surgical tactics vary and include open hernia repair with appendectomy, initial appendectomy followed by interval hernia repair, initial hernia repair followed by interval appendectomy, diagnostic laparoscopy with appendectomy and open hernia repair, and open repair with laparotomy and appendectomy [10]. Despite the laparoscopic appendectomy which has been reported, the laparoscopic approach remains controversial [11]. The surgical choice for repair of femoral hernia with appendix or appendicitis remains also ambiguous. Prosthetic mesh can be used if there is no wound infection or abscess formation. Concerning the postoperative complications, infection of De Garengeot hernia repair occurs in up to 29% cases and wound infection is the most common complication. Risk factors include older age, delayed diagnosis and poor nutritional status [12,13]. In conclusion, femoral hernia with appendicitis occurs extremely rarely and early diagnosis and prompt surgical treatment are essential in order to avoid severe complications.
SCARE checklist
The work has been reported in line with the SCARE checklist [14].
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Sources of funding
No source of funding or sponsors.
Ethical approval
This is a Case Report for which the patient provided written informed consent. Ethical approval has also been provided by the ethical committee of General Hospital Filiates.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Fotios Fousekis: Study design, data collection,writing.
Panagiota Christou: Data collection, writing.
Spyridon Gkogkos: Data analysis, writing.
Panagiota Aggeli: Writing.
George Pappas-Gogos: Writing, study design, Surgeon, who performed the operation
All authors have approved the final article.
Registration of research studies
N/A.
Guarantor
Fotios Fousekis
Contributor Information
Fotios S. Fousekis, Email: fotisfous@gmail.com.
Panagiota A. Christou, Email: panagiotaxrist@hotmail.com.
Spyridon Gkogkos, Email: spiro603@hotmail.com.
Panagiota Aggeli, Email: abournetas@yahoo.gr.
George Pappas-Gogos, Email: pappasg8@gmail.com.
References
- 1.Kalles V., Mekras A., Mekras D., Papapanagiotou I., AI-Harethee W., Sotiropoulos G. De Garengeot’s hernia: a comprehensive review. Hernia. 2013;17(2):177–182. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]
- 2.Gabriel A., Magdi A. De Garengeot hernia: appendicitis within a femoral hernia. Am. Surg. 2005;71(6):526–527. [PubMed] [Google Scholar]
- 3.Velimezis G., Vassos N., Kapogiannatos G., Koronakis D., Perrakis E., Perrakis A. Incarcerated recurrent inguinal hernia containing an acute appendicitis (Amyand hernia): an extremely rare surgical situation. Arch. Med. Sci. 2017;13(3):702–704. doi: 10.5114/aoms.2016.60403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Georgiou G.K., Bali C., Theodorou S.J., Zioga A., Fatouros M. Appendiceal diverticulitis in a femoral hernia causing necrotizing fasciitis of the right inguinal region: report of a unique case. Hernia. 2013;17(1):125–128. doi: 10.1007/s10029-011-0822-0. [DOI] [PubMed] [Google Scholar]
- 5.Brown N., Moesbergen T., Steinke K. The French and their hernias: prospective radiological differentiation of de Garengeot from other groin hernias. J. Radiol. Case Rep. 2013;7(4):16–21. doi: 10.3941/jrcr.v7i4.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Filatov J., Llibitzki A., Davidovitch S., Soudack M. Appendicitis within a femoral hernia: sonographic appearance. J. Ultrasound Med. 2006;25(9):1233–1235. doi: 10.7863/jum.2006.25.9.1233. [DOI] [PubMed] [Google Scholar]
- 7.Fukukura Y., Chang S.D. Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom. Imaging. 2005;30(5):620–622. doi: 10.1007/s00261-004-0283-3. [DOI] [PubMed] [Google Scholar]
- 8.Piperos T., Kalles V., Al Ahway Y., Konstantinou E., Skarpas G., Mariolis-Sapsakos T. Clinical significance of de Garengeot’s hernia: a case of acute appendicitis and review of the literature. Int. J. Surg. Case Rep. 2012;3(3):116–117. doi: 10.1016/j.ijscr.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kagan Coskun A., Kilbas Z., Yigit T., Simsek A., Harlak A. De Garengeot’s hernia: the importance of early diagnosis and its complications. Hernia. 2012;16(6):731–733. doi: 10.1007/s10029-011-0814-0. [DOI] [PubMed] [Google Scholar]
- 10.Granvall S.A. De Garengeot hernia: a unique surgical finding. JAAPA. 2014;27(5):39–41. doi: 10.1097/01.JAA.0000443968.31234.63. [DOI] [PubMed] [Google Scholar]
- 11.Talini C., Oliveira L.O., Araujo A.C., Netto F.A., Westphalen A.P. De Garengeot hernia: case report and review. Int. J. Surg. Case Rep. 2015;8C:35–37. doi: 10.1016/j.ijscr.2014.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma H., Jha P.K., Shekhawat N.S., Memon B., Memon M.A. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11(3):235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 13.Mashima H., Banshodani M., Nishihara M., Nambu J., Kawaguchi Y., Shimamoto F. De Garengeot hernia with perforated appendicitis and a groin subcutaneous abscess: a case report. Int. J. Surg. Case Rep. 2017;33:8–11. doi: 10.1016/j.ijscr.2017.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]