Abstract
Background
The frequent or regular use of analgesics and anti-migraine drugs can make headache more frequent and induce the transformation of episodic to chronic headache. Chronic headache due to medication overuse is defined as headache that is present on = 15 days per month for at least three months in a patient who previously suffered from primary headaches, and who takes analgesics on = 15 days per month or anti-migraine drugs (triptans or ergot alkaloids), opioid drugs, or combined analgesics on = 10 days per month.
Methods
This review is based on pertinent articles published up to December 2017 that were retrieved by a selective search in PubMed employing the terms “medication overuse AND headache” and “medication overuse headache.”
Results
The prevalence of medication overuse headache in the general population in Germany is 0.7% –1%. This disorder is more common in women and in persons suffering from comorbid mental disorders or other painful conditions. The treatment of medication overuse headache consists of three steps. Patient education and counseling are given with the goal of reducing the intake of medication for acute headache treatment. The ensuing headache prophylaxis is with topiramate, amitriptyline, or onabotulinum toxin A. If these treatment strategies fail, a drug holiday is recommended. This can be in the outpatient, day clinic, or inpatient setting, depending on the severity of the condition and its comorbidities.
Conclusion
Patients who frequently take acute medication to treat headache episodes must be identified early in order to avoid headache chronification and medication overuse headache. The suggested treatment algorithm is still in need of validation by randomized trials.
Chronic headache due to the frequent or regular consumption of analgesics or anti-migraine drugs is defined, in the classification of the International Headache Society (IHS ICHD-3), as headache that is present on 15 or more days of each month and that is caused by the excessively frequent use of analgesics or anti-migraine drugs (1) (table 1). The definition requires either the overuse of simple analgesics on 15 or more days per month, or else the overuse of triptanes, ergotamines, opioids, and (caffeine or codeine-containing) combined analgesics on 10 or more days per month, for at least three consecutive months. The overuse of any kind of analgesic or anti-migraine drug can lead to medication overuse headache (2). The analgesic need not have been taken for the treatment of headache; the frequent use of analgesics for other, e.g., musculoskeletal, indications can increase the frequency of migraine headaches in patients who already have them (3).
Table 1. The definition of headache due to the overuse of analgesics and anti-migraine medications*.
| Criteria | ||
| A | Headache on ≥ 15 days per month in a patient with a pre-existing headache disorder | |
| B | Regular overuse (for ≥ 3 months) of one or more medications that can be used for the acute or symptomatic treatment of headache | |
| C | Not better explained by another ICHD-3 diagnosis | |
| Subgroups | Medication use | |
| 8.2.1 | Ergotamine overuse headache (ergot alkaloids) | ≥ 10 days/month |
| 8.2.2 | Triptan overuse headache | ≥ 10 days/month |
| 8.2.3 | Non-opioid analgesic overuse headache - Paracetamol (= acetaminophen) - Nonsteroidal anti-inflammatory drugs - Acetylsalicylic acid - Other analgesics | ≥ 15 days/month |
| 8.2.4 | Opioid overuse headache | ≥ 10 days/month |
| 8.2.5 | Combined analgesics (two or more analgesics, or an analgesic in combination with caffeine) | ≥ 10 days/month |
* Medication overuse headache (MOH) according to the diagnostic criteria of the International Headache Society ICHD-3) (e55)
The causal link between the frequent consumption of analgesics or anti-migraine drugs and the development of the clinical condition called medication overuse headache can be difficult to demonstrate in the individual case. In some patients who take analgesics and anti-migraine drugs frequently, the headaches do not become any more frequent, nor do they become chronic. Thus, medication overuse does not necessarily cause medication overuse headache.
Migraine and tension headache are primary headache syndromes, but medication overuse headache is a secondary headache syndrome that arises in combination with an underlying primary one. For this reason, both diagnoses should always be documented and given a designation according to the ICHD classification: thus, patients suffer from medication overuse headache in combination with chronic migraine. Chronic migraine is defined as headache on at least 15 days per month for at least 3 consecutive months, with headache that satisfies the criteria for migraine on at least 8 days per month (1). Patients with cluster headache can develop medication overuse headache only if they also have migraine or a positive family history of migraine (4).
Medication overuse headache is to be distinguished from medication-induced headache, the definition of which requires that the headache is induced by a drug given for other reasons than to treat pain, e.g., sildenafil or nitrates (ICHD-3) (1).
A number of studies on the epidemiology, pathophysiology, and clinical features of headache due to the overuse of analgesics and anti-migraine drugs have been published in recent years, as have up-to-date randomized clinical trials on the treatment and prevention of this condition. These new scientific data, as will be discussed in the following sections, provide a basis for recommendations for patient care.
Epidemiology
The prevalence of medication overuse headache in Germany ranges from 0.7% to 1% (5, 6). Accordingly, 25% to 50% of all patients with chronic headache (i.e., headache on more than 15 days per month) overuse medications (7). The eTable contains data on the frequency of analgesic and anti-migraine drug overuse in different countries. The figures from the United States of America are accounted for mainly by the overuse of opioids and barbiturates, which are not recommended in Germany for the acute treatment of headache. Women suffer more commonly than men from medication overuse headache, in a ratio of 4:1 (5). The peak prevalence by age is reached in the middle of the fifth decade (8, 9). The prevalence of medication overuse headache in children lies between 0.3% and 1% (10, 11).
Diagnosis
The clinical features of analgesic and anti-migraine drug overuse headache depend on the type of primary headache from which the patient suffers. Migraine patients who overuse triptans report daily headaches that generally have the features of a migraine attack, or else an increase in the frequency of migraines (12) (table 2). As the headaches become more frequent, their phenotype can change as well. In migraine patients, the accompanying vegetative phenomena—nausea, vomiting, photophobia, phonophobia—tend to become less prominent, and the headaches, therefore, can become hard to distinguish from tension headaches. In patients with chronic tension headache who overuse analgesics, the headaches become more frequent, but the clinical features of the dull, pressing holocranial pain do not change (12). Future studies are needed to provide a well-founded answer to the question whether there are really substance-specific clinical presentations of medication overuse headache. The pathophysiology of medication overuse headache is presented in eBox 1.
Table 2. Risk factors for the development of chronic headache due to the overuse of analgesics and anti-migraine medications*.
| Risk factors | Odds ratio | 95% CI |
| Age (<50 years) | 1.8 | [1.3; 2.4] |
| Female sex | 1.9 | [1.4; 2.6] |
| Low educational attainment | 1.9 | [1.2; 3.0] |
| Chronic musculoskeletal symptoms | 1.9 | [1.4; 2.7] |
| Gastrointestinal disturbances | 1.6 | [1.1; 2.2] |
| Anxiety disorder or depression | 4.7 | [2.4; 9.0] |
| Smoking | 1.8 | [1.2; 2.5] |
| Lack of exercise | 2.7 | [1.2; 6.3] |
| Metabolic syndrome | 5.3 | [1.6; 24.6] |
| Regular use of tranquilizers | 5.2 | [3.0; 9.0] |
| Regular use of acetylsalicylic acid | 0.5 | [0.3; 0.9] |
| Frequent use of ibuprofen | 0.7 | [0.5; 1.0] |
| Frequent use of opioids | 2.3 | [1.3; 3.9] |
eBOX 1. The pathophysiology of medication overuse headache.
The pathophysiological mechanisms underlying medication overuse headache (MOH) are not precisely understood at present. The condition seems to arise only in persons with a pre-existing headache disorder, generally either tension-type headache or migraine (e42). Persons with cluster headache very rarely develop MOH. Oversensitivity to medications taken for the acute treatment of headache attacks may have a genetic basis, as it is apparently associated with a number of polymorphisms affecting, e.g., angiotensin-converting enzyme (ACE) (e43), brain-derived neurotrophic factor (BDNF) (e44), catechol-O-methyltransferase (COMT), and the sodium-dependent serotonin transporter SLC6A4 (e45).
Any type of pain-relieving drug can, in principle, cause MOH, but the effect is stronger with triptans than with simple analgesics. The reason may be that triptans induce changes in neurotransmitter metabolism, particularly in the serotoninergic (e46-e48) and endocannabinoid (e49, e50) systems, that are of central importance to the generation of MOH. These changes cause cerebral hyperexcitability, which can be demonstrated electrophysiologically as an increased response to stimulation together with a deficit of habituation (e51, e52). These changes can be seen regardless of whether the stimulus is delivered to the head or to the extremities (e51), and they can be reversed by the cessation of medication overuse (e51, e52). Imaging studies have revealed functional and structural changes in multiple brain areas (e53), affecting structures that play a role in sensory discrimination, cognition, attention, and emotionality, among others (e53). These changes, too, can be reversed by the cessation of medication overuse.
The diagnosis of analgesic or anti-migraine drug overuse headache is based on the history and on the documentation of medication use in a headache diary. If headache becomes chronified in a patient over age 60, or if focal neurologic signs or pathological mental changes are found, magnetic resonance imaging of the brain is mandatory. In markedly overweight patients of any age, the cerebrospinal fluid pressure should be measured in order to rule out idiopathic intracranial hypertension (“pseudotumor cerebri”) (13).
Course
The development of analgesic or anti-migraine drug overuse headache over time depends on the substances taken, among other factors. Chronification is faster when triptans and opioids are overused, compared to single analgesics and caffeine-containing combination analgesics (9). This conclusion can, however, be viewed critically. For each patient, the choice of medication clearly depends to some extent on the severity of the headaches; patients with more severe headaches are more likely to be treated with a combination of triptans and analgesics.
Risk factors
The main risk factors for medication overuse headache are listed in Table 2. Acetylsalicylic acid as a single substance is not a risk factor.
Treatment
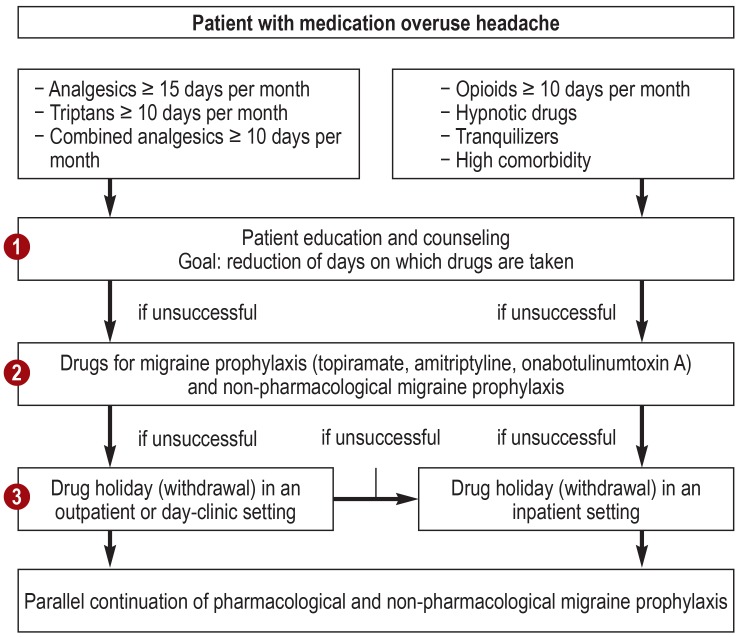
The treatment of analgesic and anti-migraine drug overuse headache consists of three steps (figure).
Figure.
The treatment of headache due to the overuse of analgesics and anti-migraine drugs
Step 1 (education and counseling): The patient is informed that the frequent use of analgesics and anti-migraine drugs can lead to the development of chronic headaches. The goal is to limit the consumption of simple analgesics to fewer than 15 days per month, and that of specific analgesics, anti-migraine drugs, and caffeine-containing combined analgesics to fewer than 10 days per month.
Step 2: Pharmacological and non-pharmacological prophylaxis of the patient’s primary headaches is initiated.
Step 3: If these approaches fail, there should be a drug holiday (drug withdrawal) in an outpatient, day-clinic, or inpatient setting, whichever is most appropriate. Primary headache prophylaxis by pharmacological and non-pharmacological means should continue in parallel.
Education and counseling
As triptans and analgesics do not cause mental or physical dependence, the term “drug holiday” is preferable to the term “withdrawal.” Some patients who overuse medications meet the criteria for addiction, including loss of control, the development of tolerance, and an increasing dose (14). A meta-analysis of 7 clinical trials involving 391 patients detected no difference between drug holidays in an inpatient setting and drug holidays in an outpatient or day-clinic setting with respect to the reduction of headache days (15). In the largest trial to date concerning the treatment of medication overuse headache, 379 patients underwent an interdisciplinary three-week outpatient program with medical, psychological, nursing, and physiotherapeutic components. They graded their own headaches on a scale from 0 to 10 before treatment, at the end of the three-week period, and one year later. The mean pain intensities were 6.1, 3.5, and 3.3, respectively (16). The patients’ anxiety and depression scores improved as well.
Migraine prophylaxis
Most of the patients referred to a specialized headache center because of chronic headache due to the overuse of anti-migraine drugs have already received prophylactic medication against migraine attacks, including beta-blockers, flunarizine, valproic acid, or amitriptyline, without success. It was accepted as dogma until a few years ago that prophylactic drugs against migraine cannot be effective in patients who overuse analgesics and triptans, but two prospective placebo-controlled trials with topiramate have refuted this notion (17– 19). In both studies, topiramate in doses ranging from 50 to 200 mg per day was significantly more effective than placebo in patients with chronic migraine and medication overuse. In the first trial, the mean number of migraine days in four weeks was 15.5 in the topiramate group (n = 32) and 16.4 in the placebo group (n = 27). After a mean of 90 days, the number of migraine days per month under treatment with topiramate was reduced by 3.5 ± 6.3, compared to –0.2 ± 4.7 for placebo (p < 0.05) (17). The second trial included 306 patients with chronic migraine (topiramate, n = 153; placebo, n = 153), 38% of whom met the criteria for medication overuse. The responder rate for a 25% reduction of the number of migraine days per month was 68.6% for topiramate vs. 51.6% for placebo (p = 0.005); the corresponding rates for a 50% reduction were 37.3% vs. 28.8% (p = 0.093) (18). It must be kept in mind, however, that topiramate may exacerbate mental comorbidities, which are common in patients with chronic migraine and medication overuse (20). In the two large-scale approval trials of onabotulinum toxin A for patients with chronic migraine, 65% of the patients met the criteria for medication overuse headache (21). Patients who overused barbiturates and opioids were excluded from these trials. The patients in the medication overuse headache subgroup achieved the same degree of therapeutic success (onabotulinum toxin A versus placebo) as patients without medication overuse (22). Smaller studies have addressed the putative efficacy of valproic acid, cannabinoids, pregabalin, and acupuncture against medication overuse headache, but none of them were of sufficient methodological quality to justify a recommendation for any of these pharmacological or non-pharmacological approaches. Randomized trials are now in progress to study the efficacy of antibodies against calcitonin-gene related peptide (CGRP) or the CGRP receptor in patients with chronic headache due to overuse of analgesics and anti-migraine agents.
The treatment of headache and vegetative symptoms during drug holidays
Patients with medication overuse headache who undergo a drug holiday often have more intense headaches at first. Symptoms of vegetative dysfunction, such as nausea and vomiting, agitation, anxiety, and sleep disturbances, may arise and are sometimes severe. In a systematic review of the literature, 27 studies of the treatment of such symptoms were identified (23). The recommended measures included fluid replacement, analgesics, antipsychotic drugs to suppress nausea and vomiting, and dihydroergotamine (DHE), which is not approved in Germany. The Norwegian and German placebo-controlled trials of corticosteroids in this setting revealed no therapeutic effect (24, 25), but both were methodologically inadequate. The heterogeneous patient groups that were studied in the outpatient and inpatient settings had different comorbidities and different accompanying treatments, and these factors may have masked a real effect of steroid treatment. The efficacy of steroids during drug holidays is commonly observed in routine clinical practice, notwithstanding the study findings. Acetysalicylic acid can be given intravenously to combat pain peaks during drug holidays in patients who previously overused triptans. Clinical experience supports the withholding of analgesics (as much as possible), oral or intravenous steroid administration, and at least temporary treatment with tricyclic antidepressants (administered orally or intravenously, depending on the severity of symptoms), as well as antiemetic treatment. This approach has not been validated to date by any randomized controlled clinical trial. An evaluation of observational data revealed that the severity and duration of symptoms during a drug holiday depends to a large extent on the particular substance that was overused. If triptans or analgesics alone were overused, the symptoms can usually be well controlled and subside within one week. In contrast, a drug holiday after the overuse of ergotamines, combinations of triptans and analgesics, or caffeine-containing combined analgesics usually leads to prolonged symptoms (26). In this situation, adequate treatment to suppress nausea and vomiting and sometimes the short-term use of neuroleptic drugs have proven useful in routine clinical practice. If the overused drug was an opioid (usually tilidine or tramadol), especially in a slow-release form, true withdrawal phenomena can arise, including signs of autonomic decompensation. Opioids and barbiturates should not be abruptly discontinued, but rather tapered to off. Tachycardia and hypertension as symptoms of withdrawal can be effectively treated in a monitored inpatient setting with the a2-adrenoceptor antagonist clonidine (27).
The effects of drug holidays
In a large-scale international trial in Europe and South America that included 376 patients with medication overuse headache, analgesics and acute anti-migraine drugs were discontinued and prophylaxis against migraine attacks was given. Six months into the trial, two-thirds of the patients were no longer overusing acute medication, and the chronic headache had regressed to an episodic headache in 50% (28). Over this period, depression and anxiety were also reduced, and the patients experienced less impairment as the result of their headaches. It remains unclear whether prophylactic drug treatment should be started before, during, or after the drug holiday. In Denmark, headache specialists generally wait to observe the success of the drug holiday and then begin anti-migraine prophylaxis after an interval of three to six months; in Germany, most patients are started on anti-migraine prophylactic drugs immediately before, or simultaneously with, the discontinuation of analgesics or anti-migraine drugs. This pragmatic approach is motivated by the consideration that patients with chronic headache have high relapse rates and their symptoms can be suppressed in the inpatient setting to an extent that enables them to take part in a treatment program (eBox 2).
eBOX 2. Reasons for a drug holiday in an inpatient setting.
Overuse of a medication whose withdrawal in the setting of a drug holiday would be expected to induce marked vegetative manifestations, as is the case with opioids, barbiturates, ergotamines, and caffeine-containing combined analgesics
Marked psychiatric comorbidity (depression, anxiety disturbances)
Marked somatic comorbidity
Unsuccessful outpatient drug holidays
Recurrence
In a systematic review of 22 studies with follow-up intervals ranging from 2 to 60 months and a mean follow-up interval of 12 months, the mean recurrence rate ranged from 25% to 35% (23). Predictors of recurrence of medication overuse headache included chronic tension headache as opposed to migraine, the overuse of opioids as opposed to triptans, and psychiatric comorbidities. Post-trial observations in a cohort of patients who underwent headache treatment in a day clinic at the Universitätsklinikum in Essen have shown that patient education and counseling, as part of a structured treatment program in a day clinic, can lower the recurrence rate of medication overuse headache to less than 10% (29).
Prevention
The most effective way to prevent medication overuse headache is to identify patients at risk and to educate them about the use of acute medication. The risk is higher in patients with frequent headaches (10–14 headache days per month, high-frequency episodic migraine) than in those with rarer headaches (1–9 headache days per month, low-frequency episodic migraine). Likewise, patients with chronic headache, i.e., headache on at least 15 days per month, are also at high risk of developing medication overuse headache if they take acute medication on an increasing number of headache days. If opioids are taken, the risk is much higher; such patients should be identified early so that they can be treated with preventive strategies (30). A randomized trial revealed the efficacy of patient education, either with an informational brochure or with group therapy based on cognitive behavioral therapy, in preventing medication overuse headache (31). Pharmacists, too, should identify and appropriately counsel patients at risk; this is especially important in view of the fact that two different triptans, like most analgesics, can now be obtained in Germany without a prescription. Both general practitioners and specialists should implement mechanisms in their practices for the reliable detection of any increasing need for acute medication or higher demand for prescriptions in headache patients.
Critical evaluation of the concept of medication overuse headache
The concept of medication overuse headache is debated in the current literature. The valid objection has been raised that longitudinal studies of large patient cohorts are lacking and that some of the affected patients do not benefit from a drug holiday. The causal relationship between medication use and increased headache frequency has not been proven. Medication overuse is but one of the many risk factors for chronification that may be of varying importance in individual cases, yet the concept of the drug holiday takes insufficient account of this fact. New treatments need to be developed, above all, for those patients who fail to respond to the recommended treatments for medication overuse headache and whose headaches do not improve after their medications are discontinued (32).
Key Messages.
Patients with chronic headache due to the overuse of analgesics or anti-migraine drugs should be treated by a multidisciplinary team including neurologists, psychologists, physical therapists, and exercise therapists.
Thorough patient education and counseling are very important.
Patients with chronic headache due to medication overuse for whom pharmacological and non-pharmacological headache prophylaxis is ineffective should undergo a drug holiday.
In patients who overuse analgesics or triptans, a drug holiday is begun with the abrupt termination of acute therapy.
Drug holidays can usually be carried out in an outpatient or day-clinic setting. Patients who overuse opioids should be hospitalized for opioid withdrawal.
eTable. The frequency of medication overuse headache*.
| Authors | Country | Age group | Frequency of MOH |
| Castillo et al. (1999) (e2) | Spain | ≥ 14 | 1.2% |
| Wang et al. (2000) (e3) | Taiwan | ≥ 65 | 1.0% |
| Lu et al. (2001) (e4) | Taiwan | ≥ 15 | 1.1% |
| Pascual et al. (2001) – review (e5) | 1.0–1.9% | ||
| Prencipe et al. (2001) (e6) | France | ≥ 65 | 1.7% |
| Colas et al. (2004) (e7) | Spain | ≥ 14 | 1.5% |
| Zwart et al. (2004) (e8) | Norway | ≥ 20 | 0.9–1.0% |
| Dyb et al. (2006) (e9) | Norway | 13–18 | 0.2% |
| Wang et al. (2006) (e10) | Taiwan | 12–14 | 0.3% |
| Wiendels 2006 (e11) | Netherlands | 25–55 | 2.6% |
| Stovner et al.(2007) – review (7) | 0.5–1.0% | ||
| Aaseth et al. (2008. 2009) (e12, e13) | Norway | 30–44 | 1.7% |
| Rueda-Sanchez & Diaz-Martinez (2008) (e14) | Colombia | 18–65 | 4.5% |
| Katzarava et al. (2009) (e15) | Georgia | ≥ 16 | 0.9% |
| Da Silva et al. (2009) (e16) | Brazil | 10–93 | 1.6% |
| Straube et al. (2010) (e17) | Germany | 18–88 | 1.0% |
| Jonsson et al. (2011. 2012) (e18, e19) | Sweden | ≥ 15 | 1.8% |
| Linde et al. (2011) (e20) | Norway | ≥ 20 | 1.0% |
| Lipton et al. (2011) (e21) | USA | 12–17 | 1.0% |
| Ayzenberg et al. (2012) (e22) | Russia | 18–65 | 7.2% |
| Ertas et al. (2012) (e23) | Turkey | 18–65 | 2.1% |
| Hagen et al. (2012) (e24) | Norway | ≥ 20 | 0.8% |
| Shahbeigi et al. (2012) (e25) | Iran | ≥ 10 | 4.9% |
| Yu et al. (2012) (e26) | China | 18–65 | 0.9% |
| Schramm et al. (2013) (e27) | Germany | 18–65 | 0.7% |
| Park et al. (2014) (e28) | South Korea | 19–69 | 0.5% |
| Westergaard et al. (2014. 2016) (e1, e29) | Denmark | ≥ 16 | 1.6% (adj. 1.8%) |
| Kristo ffersen and Lundqvist (2014) – review (e30) | 1.0–2.0% | ||
| Steiner (2014) – editorial (e31) | 1.0–2.0% | ||
| Westergaard et al. (2015) – review (e32) | 0.5–7.2% | ||
| Bravo (2015) – review (e33) | Older patients | 1.0–7.1% | |
| Mbewe et al. (2015) (e34) | Zambia | 18–65 | 12.7% (adj. 7.1%) |
| Kulkarni et al. (2015) (e35) | India | 18–65 | 1.2% |
| Manandhar et al. (2016) (e36) | Nepal | 18–65 | 2.2% |
| Zebenigus et al. (2016) (e37) | Ethiopia | 18–65 | 0.8% (adj. 0.7%) |
| Al-Hashel et al. (2017) (e38) | Kuwait | 18–65 | 2.4% |
| Rastenytė et al. (2017) (e39) | Lithuania | 18–65 | 3.5% (adj. 3.2%) |
| Henning et al. (in press) (e40) | Germany | 18–65 | 0.7% |
| Global Burden of Disease (2015) – review (e41) | worldwide | 0.8% |
* Figures based on the review of Westergaard et al. (2014) (e1) supplemented by data from more recent studies and in part recalculated from new data.adj.: adjusted; MOH: medication overuse headache
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Prof.Hans-Christoph Diener has received honoraria for the planning or execution of clinical trials or participation in them, for serving on advisory boards, or for delivering lectures, from the following companies: Addex Pharma, Alder, Allergan, Almirall, Amgen, AstraZeneca, Autonomic Technology, Bayer Vital, Berlin Chemie, Böhringer Ingelheim, Bristol-Myers Squibb, Chordate, CoLucid, Coherex, Electrocore, EndoPharma, GlaxoSmithKline, Grünenthal, Janssen-Cilag, Johnson & Jonson, Labrys Biologicals, Lilly, La Roche, 3M Medica, MAP, Medtronic, Menarini, Minster, MSD, Neuroscore, Novartis, Novo-Nordisk, Pierre Fabre, Pfizer, Reckitt Benckiser, Sanofi, Schaper und Brümmer, Schering, St. Jude Medical, Teva, and Weber & Weber. He has received financial support for research projects from Allergan, Almirall, AstraZeneca, Bayer, Electrocore, GSK, Janssen-Cilag, MSD, and Pfizer. Headache research in the university neurology department and the West German Headache Center (Westdeutsches Kopfschmerzzentrum) in Essen are supported by the German Research Association (Deutsche Forschungsgemeinschaft, DFG), the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF), and the European Union (EU). Prof. Diener is the head of the Guidelines Committee of the German Neurological Society (Deutsche Gesellschaft für Neurologie).
Dr. Holle has received honoraria for the planning or execution of clinical trials or participation in them, for serving on advisory boards, or for delivering lectures, from the following companies: Alder, Allergan, Amgen, Autonomic Technology, Bayer Vital, CoLucid, Electrocore, Grünenthal, Lilly, La Roche, Novartis, Pfizer, Sanofi, and Teva. He has received financial support for research projects from Allergan and Grünenthal.
Dr. Gaul has received honoraria for lectures, clinical trials, and for serving on advisory boards from Allergan Pharma, Ratiopharm, Boehringer Ingelheim Pharma, Lilly, Novartis Pharma, Desitin Arzneimittel, Cerbotec, Bayer vital, Hormosan Pharma, electroCore, Grünenthal, Reckitt Benckiser, and Teva. He does not own stock or shares in any pharmaceutical company.
Dr. Dresler states that he has no conflict of interest.
References
- 1.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders ICHD-3, 3rd edition. Cephalalgia. 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 2.Dichgans J, Diener HC, Gerber WD, Verspohl EJ, Kukiolka H, Kluck M. Analgetika-induzierter Dauerkopfschmerz. Dtsch med Wschr. 1984;109:369–373. doi: 10.1055/s-2008-1069197. [DOI] [PubMed] [Google Scholar]
- 3.Bahra A, Walsh M, Menon S, Goadsby PJ. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache. 2003;43:179–190. doi: 10.1046/j.1526-4610.2003.03041.x. [DOI] [PubMed] [Google Scholar]
- 4.Paemeleire K, Evers S, Goadsby PJ. Medication-overuse headache in patients with cluster headache. Curr Pain Headache Rep. 2008;12:122–127. doi: 10.1007/s11916-008-0023-4. [DOI] [PubMed] [Google Scholar]
- 5.Straube A, Pfaffenrath V, Ladwig KH, et al. Prevalence of chronic migraine and medication overuse headache in Germany—the German DMKG headache study. Cephalalgia. 2010;30:207–213. doi: 10.1111/j.1468-2982.2009.01906.x. [DOI] [PubMed] [Google Scholar]
- 6.Schramm SH, Obermann M, Katsarava Z, Diener HC, Moebus S, Yoon MS. Epidemiological profiles of patients with chronic migraine and chronic tension-type headache. J Headache Pain. 2013;14 doi: 10.1186/1129-2377-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 8.Jonsson P, Hedenrud T, Linde M. Epidemiology of medication overuse headache in the general Swedish population. Cephalalgia. 2011;31:1015–1022. doi: 10.1177/0333102411410082. [DOI] [PubMed] [Google Scholar]
- 9.Diener HC, Limmroth V. Medication-overuse headache: a worldwide problem. Lancet Neurology. 2004;3:475–483. doi: 10.1016/S1474-4422(04)00824-5. [DOI] [PubMed] [Google Scholar]
- 10.Dyb G, Holmen TL, Zwart JA. Analgesic overuse among adolescents with headache: the Head-HUNT-Youth Study. Neurology. 2006;66:198–201. doi: 10.1212/01.wnl.0000193630.03650.19. [DOI] [PubMed] [Google Scholar]
- 11.Lipton RB, Manack A, Ricci JA, Chee E, Turkel CC, Winner P. Prevalence and burden of chronic migraine in adolescents: results of the chronic daily headache in adolescents study (C-dAS) Headache. 2011;51:693–706. doi: 10.1111/j.1526-4610.2011.01885.x. [DOI] [PubMed] [Google Scholar]
- 12.Limmroth V, Katsarava Z, Fritsche G, Przywara S, Diener H. Features of medication overuse headache following overuse of different acute headache drugs. Neurology. 2002;59:1011–1014. doi: 10.1212/wnl.59.7.1011. [DOI] [PubMed] [Google Scholar]
- 13.Galvin JA, van Stavern GP. Clinical characterization of idiopathic intracranial hypertension at the Detroit Medical Center. J Neurol Sci. 2004;223:157–60. doi: 10.1016/j.jns.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Radat F, Creac‘h C, Guegan-Massardier E, et al. Behavioral dependence in patients with medication overuse headache: a cross-sectional study in consulting patients using the DSM-IV criteria. Headache. 2008;48:1026–1036. doi: 10.1111/j.1526-4610.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 15.de Goffau MJ, Klaver AR, Willemsen MG, Bindels PJ, Verhagen AP. The effectiveness of treatments for patients with medication overuse headache: a systematic review and meta-analysis. J Pain. 2017;18:615–627. doi: 10.1016/j.jpain.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Krause SJ, Stillman MJ, Tepper DE, Zajac D. A prospective cohort study of outpatient interdisciplinary rehabilitation of chronic headache patients. Headache. 2017;57:428–440. doi: 10.1111/head.13020. [DOI] [PubMed] [Google Scholar]
- 17.Diener HC, Bussone G, van Oene JC, Lahaye M, Schwalen S, Goadsby PJ. Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27:814–823. doi: 10.1111/j.1468-2982.2007.01326.x. [DOI] [PubMed] [Google Scholar]
- 18.Silberstein S, Lipton R, Dodick D, et al. Topiramate treatment of chronic migraine: a randomized, placebo-controlled trial of quality of life and other efficacy measures. Headache. 2009;49:1153–1162. doi: 10.1111/j.1526-4610.2009.01508.x. [DOI] [PubMed] [Google Scholar]
- 19.Diener HC, Dodick DW, Goadsby PJ, et al. Utility of topiramate for the treatment of patients with chronic migraine in the presence or absence of acute medication overuse. Cephalalgia. 2009;29:1021–1027. doi: 10.1111/j.1468-2982.2009.01859.x. [DOI] [PubMed] [Google Scholar]
- 20.Romigi A, Cervellino A, Marciani MG, et al. Cognitive and psychiatric effects of topiramate monotherapy in migraine treatment: an open study. Eur J Neurol. 2008;15:190–195. doi: 10.1111/j.1468-1331.2007.02033.x. [DOI] [PubMed] [Google Scholar]
- 21.Dodick DW, Turkel CC, DeGryse RE, et al. Onabotulinumtoxin A for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010;50:921–936. doi: 10.1111/j.1526-4610.2010.01678.x. [DOI] [PubMed] [Google Scholar]
- 22.Silberstein SD, Blumenfeld AM, Cady RK, et al. Onabotulinumtoxin A for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci. 2013;331:48–56. doi: 10.1016/j.jns.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Chiang CC, Schwedt TJ, Wang SJ, Dodick DW. Treatment of medication-overuse headache: a systematic review. Cephalalgia. 2015 doi: 10.1177/0333102415593088. [DOI] [PubMed] [Google Scholar]
- 24.Rabe K, Pageler L, Gaul C, et al. Prednisone for the treatment of withdrawal headache in patients with medication overuse headache: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2013;33:202–207. doi: 10.1177/0333102412462638. [DOI] [PubMed] [Google Scholar]
- 25.Boe MG, Mygland A, Salvesen R. Prednisolone does not reduce withdrawal headache: a randomized, double-blind study. Neurology. 2007;69:26–31. doi: 10.1212/01.wnl.0000263652.46222.e8. [DOI] [PubMed] [Google Scholar]
- 26.Katsarava Z, Fritsche G, Muessig M, Diener HC, Limmroth V. Clinical features of withdrawal headache following overuse of triptans and other headache drugs. Neurology. 2001;57:1694–1698. doi: 10.1212/wnl.57.9.1694. [DOI] [PubMed] [Google Scholar]
- 27.Gowing L, Farrell M, Ali R, White JM. Alpha(2)-adrenergic agonists for the management of opioid withdrawal. Cochrane Database Syst Rev. 2016 CD002024. [Google Scholar]
- 28.Tassorelli C, Jensen R, Allena M, et al. A consensus protocol for the management of medication-overuse headache: evaluation in a multicentric, multinational study. Cephalalgia. 2014;34:645–655. doi: 10.1177/0333102414521508. [DOI] [PubMed] [Google Scholar]
- 29.Gaul C, van Doorn C, Webering N, et al. Clinical outcome of a headache-specific multidisciplinary treatment program and adherence to treatment recommendations in a tertiary headache center: an observational study. J Headache Pain. 2011;12:475–483. doi: 10.1007/s10194-011-0348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westergaard ML, Hansen EH, Glumer C, Jensen RH. Prescription pain medications and chronic headache in Denmark: implications for preventing medication overuse. Eur J Clin Pharmacol. 2015;71:851–860. doi: 10.1007/s00228-015-1858-3. [DOI] [PubMed] [Google Scholar]
- 31.Fritsche G, Frettloh J, Huppe M, et al. Prevention of medication overuse in patients with migraine. Pain. 2010;151:404–413. doi: 10.1016/j.pain.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 32.Scher AI, Rizzoli PB, Loder EW. Medication overuse headache: an entrenched idea in need of scrutiny. Neurology. 2017;89:1296–1304. doi: 10.1212/WNL.0000000000004371. [DOI] [PubMed] [Google Scholar]
- 33.Hagen K, Linde M, Steiner TJ, Stovner LJ, Zwart JA. Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trøndelag Health Studies. Pain. 2012;153:56–61. doi: 10.1016/j.pain.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 34.Scher AI, Lipton RB, Stewart WF, Bigal M. Patterns of medication use by chronic and episodic headache sufferers in the general population: results from the frequent headache epidemiology study. Cephalalgia. 2010;30:321–328. doi: 10.1111/j.1468-2982.2009.01913.x. [DOI] [PubMed] [Google Scholar]
- 35.He Z, Dong L, Zhang Y, Kong Q, Tan G, Zhou J. Metabolic syndrome in female migraine patients is associated with medication overuse headache: a clinic-based study in China. Euro J Neurol. 2015;22:1228–1234. doi: 10.1111/ene.12732. [DOI] [PubMed] [Google Scholar]
- 36.Diener HC, Holle D, Solbach K, Gaul C. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12:575–583. doi: 10.1038/nrneurol.2016.124. [DOI] [PubMed] [Google Scholar]
- E1.Westergaard ML, Glumer C, Hansen EH, Jensen RH. Prevalence of chronic headache with and without medication overuse: associations with socioeconomic position and physical and mental health status. Pain. 2014;155:2005–2013. doi: 10.1016/j.pain.2014.07.002. [DOI] [PubMed] [Google Scholar]
- E2.Castillo J, Munoz P, Guitera V, Pascual J. Epidemiology of chronic daily headache in the general population. Headache. 1999;39:190–196. doi: 10.1046/j.1526-4610.1999.3903190.x. [DOI] [PubMed] [Google Scholar]
- E3.Wang SJ, Fuh JL, Lu SR, et al. Chronic daily headache in chinese elderly—prevalence, risk factors, and biannual follow-up. Neurology. 2000;54:314–319. doi: 10.1212/wnl.54.2.314. [DOI] [PubMed] [Google Scholar]
- E4.Lu SR, Fuh JL, Chen WT, Juang KD, Wang SJ. Chronic daily headache in Taipei, Taiwan: prevalence, follow-up and outcome predictors. Cephalalgia. 2001;21:980–986. doi: 10.1046/j.1468-2982.2001.00294.x. [DOI] [PubMed] [Google Scholar]
- E5.Pascual J, Colas R, Castillo J. Epidemiology of chronic daily headache. Curr Pain Headache Rep. 2001;5:529–536. doi: 10.1007/s11916-001-0070-6. [DOI] [PubMed] [Google Scholar]
- E6.Prencipe M, Casini AR, Ferretti C, et al. Prevalence of headache in an elderly population: attack frequency, disability, and use of medication. J Neurol Neurosurg Psychiatry. 2001;70:377–381. doi: 10.1136/jnnp.70.3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Colas R, Munoz P, Temprano R, Gomez C, Pascual J. Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life. Neurology. 2004;62:1338–1342. doi: 10.1212/01.wnl.0000120545.45443.93. [DOI] [PubMed] [Google Scholar]
- E8.Zwart J, Dyb G, Hagen K, Svebak S, Stovner L, Holmen J. Analgesic overuse among subjects with headache, neck, and low back pain. Neurology. 2004;62:1540–1544. doi: 10.1212/01.wnl.0000123262.96132.fc. [DOI] [PubMed] [Google Scholar]
- E9.Dyb G, Holmen TL, Zwart JA. Analgesic overuse among adolescents with headache: the Head-HUNT-Youth Study. Neurology. 2006;66:198–201. doi: 10.1212/01.wnl.0000193630.03650.19. [DOI] [PubMed] [Google Scholar]
- E10.Wang SJ, Fuh JL, Lu SR, Juang KD. Chronic daily headache in adolescents: prevalence, impact, and medication overuse. Neurology. 2006;66:193–197. doi: 10.1212/01.wnl.0000183555.54305.fd. [DOI] [PubMed] [Google Scholar]
- E11.Wiendels NJ, Knuistingh NA, Rosendaal FR, et al. Chronic frequent headache in the general population: prevalence and associated factors. Cephalalgia. 2006;26:1434–1442. doi: 10.1111/j.1468-2982.2006.01210.x. [DOI] [PubMed] [Google Scholar]
- E12.Aaseth K, Grande RB, Kvaerner KJ, Gulbrandsen P, Lundqvist C, Russell MB. Prevalence of secondary chronic headaches in a population-based sample of 30-44-year-old persons The Akershus study of chronic headache. Cephalalgia. 2008;28:705–713. doi: 10.1111/j.1468-2982.2008.01577.x. [DOI] [PubMed] [Google Scholar]
- E13.Aaseth K, Grande RB, Lundqvist C, Russell MB. What is chronic headache in the general population? The Akershus study of chronic headache. Acta Neurol Scand Suppl. 2009:30–32. doi: 10.1111/j.1600-0404.2009.01209.x. [DOI] [PubMed] [Google Scholar]
- E14.Rueda-Sanchez M, Diaz-Martinez LA. Prevalence and associated factors for episodic and chronic daily headache in the Colombian population. Cephalalgia. 2008;28:216–225. doi: 10.1111/j.1468-2982.2007.01499.x. [DOI] [PubMed] [Google Scholar]
- E15.Katsarava Z, Dzagnidze A, Kukava M, et al. Primary headache disorders in the Republic of Georgia: prevalence and risk factors. Neurology. 2009;73:1796–1803. doi: 10.1212/WNL.0b013e3181c34abb. [DOI] [PubMed] [Google Scholar]
- E16.da Silva Jr A, Costa EC, Gomes JB, et al. Chronic headache and comorbibities: a two-phase, population-based, cross-sectional study. Headache. 2010;50:1306–1312. doi: 10.1111/j.1526-4610.2010.01620.x. [DOI] [PubMed] [Google Scholar]
- E17.Straube A, Pfaffenrath V, Ladwig KH, et al. Prevalence of chronic migraine and medication overuse headache in Germany—the German DMKG headache study. Cephalalgia. 2010;30:207–213. doi: 10.1111/j.1468-2982.2009.01906.x. [DOI] [PubMed] [Google Scholar]
- E18.Jonsson P, Hedenrud T, Linde M. Epidemiology of medication overuse headache in the general Swedish population. Cephalalgia. 2011;31:1015–1022. doi: 10.1177/0333102411410082. [DOI] [PubMed] [Google Scholar]
- E19.Jonsson P, Linde M, Hensing G, Hedenrud T. Sociodemographic differences in medication use, health-care contacts and sickness absence among individuals with medication-overuse headache. J Headache Pain. 2012;13:281–290. doi: 10.1007/s10194-012-0432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E20.Linde M, Stovner LJ, Zwart JA, Hagen K. Time trends in the prevalence of headache disorders The Nord-Trøndelag Health Studies (HUNT 2 and HUNT 3) Cephalalgia. 2011;31:585–596. doi: 10.1177/0333102410391488. [DOI] [PubMed] [Google Scholar]
- E21.Lipton RB, Manack A, Ricci JA, Chee E, Turkel CC, Winner P. Prevalence and burden of chronic migraine in adolescents: results of the chronic daily headache in adolescents study (C-dAS) Headache. 2011;51:693–706. doi: 10.1111/j.1526-4610.2011.01885.x. [DOI] [PubMed] [Google Scholar]
- E22.Ayzenberg I, Katsarava Z, Sborowski A, et al. The prevalence of primary headache disorders in Russia: a countrywide survey. Cephalalgia. 2012;32:373–381. doi: 10.1177/0333102412438977. [DOI] [PubMed] [Google Scholar]
- E23.Ertas M, Baykan B, Orhan EK, et al. One-year prevalence and the impact of migraine and tension-type headache in Turkey: a nationwide home-based study in adults. J Headache Pain. 2012;13:147–157. doi: 10.1007/s10194-011-0414-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E24.Hagen K, Linde M, Steiner TJ, Stovner LJ, Zwart JA. Risk factors for medication-overuse headache: an 11-year follow-up study The Nord-Trøndelag Health Studies. Pain. 2012;153:56–61. doi: 10.1016/j.pain.2011.08.018. [DOI] [PubMed] [Google Scholar]
- E25.Shahbeigi S, Fereshtehnejad SM, Mohammadi N, et al. Epidemiology of headaches in Tehran urban area: a population-based cross-sectional study in district 8, year 2010. Neurol Sci. 2013;34:1157–1166. doi: 10.1007/s10072-012-1200-0. [DOI] [PubMed] [Google Scholar]
- E26.Yu S, Liu R, Zhao G, et al. The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache. 2012;52:582–591. doi: 10.1111/j.1526-4610.2011.02061.x. [DOI] [PubMed] [Google Scholar]
- E27.Schramm SH, Obermann M, Katsarava Z, Diener HC, Moebus S, Yoon MS. Epidemiological profiles of patients with chronic migraine and chronic tension-type headache. J Headache Pain. 2013;14 doi: 10.1186/1129-2377-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E28.Park JW, Moon HS, Kim JM, Lee KS, Chu MK. Chronic daily headache in Korea: prevalence, clinical characteristics, medical consultation and management. J Clin Neurol. 2014;10:236–243. doi: 10.3988/jcn.2014.10.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E29.Westergaard ML, Glumer C, Hansen EH, Jensen RH. Medication overuse, healthy lifestyle behaviour and stress in chronic headache: results from a population-based representative survey. Cephalalgia. 2016;36:15–28. doi: 10.1177/0333102415578430. [DOI] [PubMed] [Google Scholar]
- E30.Kristoffersen ES, Lundqvist C. Medication-overuse headache: epidemiology, diagnosis and treatment. Ther Adv Drug Saf. 2014;5:87–99. doi: 10.1177/2042098614522683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E31.Steiner TJ, Stovner LJ, Katsarava Z, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15 doi: 10.1186/1129-2377-15-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E32.Westergaard ML, Hansen EH, Glumer C, Jensen RH. Prescription pain medications and chronic headache in Denmark: implications for preventing medication overuse. Eur J Clin Pharmacol. 2015;71:851–860. doi: 10.1007/s00228-015-1858-3. [DOI] [PubMed] [Google Scholar]
- E33.Bravo TP. Headaches of the elderly. Curr Neurol Neurosci Rep. 2015;15 doi: 10.1007/s11910-015-0552-2. [DOI] [PubMed] [Google Scholar]
- E34.Mbewe E, Zairemthiama P, Yeh HH, Paul R, Birbeck GL, Steiner TJ. The epidemiology of primary headache disorders in Zambia: a population-based door-to-door survey. J Headache Pain. 2015;16 doi: 10.1186/s10194-015-0515-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E35.Kulkarni GB, Rao GN, Gururaj G, Stovner LJ, Steiner TJ. Headache disorders and public ill-health in India: prevalence estimates in Karnataka State. J Headache Pain. 2015;16 doi: 10.1186/s10194-015-0549-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E36.Manandhar K, Risal A, Linde M, Steiner TJ. The burden of headache disorders in Nepal: estimates from a population-based survey. J Headache Pain. 2015;17 doi: 10.1186/s10194-016-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E37.Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ. The prevalence of primary headache disorders in Ethiopia. J Headache Pain. 2016;17 doi: 10.1186/s10194-016-0704-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E38.Al-Hashel JY, Ahmed SF, Alroughani R. Prevalence of primary headache disorders in Kuwait. Neuroepidemiology. 2017;48:138–146. doi: 10.1159/000478892. [DOI] [PubMed] [Google Scholar]
- E39.Rastenyte D, Mickeviciene D, Stovner LJ, Thomas H, Andree C, Steiner TJ. Prevalence and burden of headache disorders in Lithuania and their public-health and policy implications: a population-based study within the Eurolight project. J Headache Pain. 2017;18 doi: 10.1186/s10194-017-0759-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E40.Henning V, Katsarava Z, Obermann M, Moebus S, Schramm S. Remission of chronic headache: rates, potential predictors and the role of medication, follow-up results of the German Headache Consortium (GHC) Study. Cephalalgia. 2017 doi: 10.1177/0333102417699180. 333102417699180. [DOI] [PubMed] [Google Scholar]
- E41.Global Burden of Disease Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E42.Lance F, Parkes C, Wilkinson M. Does analgesic abuse cause headaches de novo? Headache. 1988;28:61–62. doi: 10.1111/j.1526-4610.1988.hed2801060_2.x. [DOI] [PubMed] [Google Scholar]
- E43.Di Lorenzo C, Coppola G, Curra A, et al. Cortical response to somatosensory stimulation in medication overuse headache patients is influenced by angiotensin converting enzyme (ACE) I/D genetic polymorphism. Cephalalgia. 2012;32:1189–1197. doi: 10.1177/0333102412461890. [DOI] [PubMed] [Google Scholar]
- E44.di Lorenzo C, di Lorenzo G, Sances G, et al. Drug consumption in medication overuse headache is influenced by brain-derived neurotrophic factor Val66Met polymorphism. J Headache Pain. 2009;10:349–355. doi: 10.1007/s10194-009-0136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E45.Cargnin S, Viana M, Ghiotto N, et al. Functional polymorphisms in COMT and SLC6A4 genes influence the prognosis of patients with medication overuse headache after withdrawal therapy. Eur J Neurol. 2014;21:989–995. doi: 10.1111/ene.12424. [DOI] [PubMed] [Google Scholar]
- E46.Srikiatkhachorn A, Anthony M. Serotonin receptor adaptation in patients with analgesic-induced headache. Cephalalgia. 1996;16:419–422. doi: 10.1046/j.1468-2982.1996.1606419.x. [DOI] [PubMed] [Google Scholar]
- E47.Srikiatkhachorn A, Anthony M. Platelet serotonin in patients with analgesic-induced headache. Cephalalgia. 1996;16:423–426. doi: 10.1046/j.1468-2982.1996.1606423.x. [DOI] [PubMed] [Google Scholar]
- E48.Srikiatkhachorn A, Puangniyom S, Govitrapong P. Plasticity of 5-HT serotonin receptor in patients with analgesic-induced transformed migraine. Headache. 1998;38 doi: 10.1046/j.1526-4610.1998.3807534.x. [DOI] [PubMed] [Google Scholar]
- E49.Rossi C, Pini LA, Cupini ML, Calabresi P, Sarchielli P. Endocannabinoids in platelets of chronic migraine patients and medication-overuse headache patients: relation with serotonin levels. Eur J Clin Pharmacol. 2008;64:1–8. doi: 10.1007/s00228-007-0391-4. [DOI] [PubMed] [Google Scholar]
- E50.Cupini LM, Costa C, Sarchielli P, et al. Degradation of endocannabinoids in chronic migraine and medication overuse headache. Neurobiol Dis. 2008;30:186–189. doi: 10.1016/j.nbd.2008.01.003. [DOI] [PubMed] [Google Scholar]
- E51.Ayzenberg I, Obermann M, Nyhuis P, et al. Central sensitization of the trigeminal and somatic nociceptive systems in medication overuse headache mainly involves cerebral supraspinal structures. Cephalalgia. 2006;26:1106–1114. doi: 10.1111/j.1468-2982.2006.01183.x. [DOI] [PubMed] [Google Scholar]
- E52.Ferraro D, Vollono C, Miliucci R, et al. Habituation to pain in „medication overuse headache“: a CO2 laser-evoked potential study. Headache. 2012;52:792–807. doi: 10.1111/j.1526-4610.2012.02151.x. [DOI] [PubMed] [Google Scholar]
- E53.Schwedt TJ, Chong CD. Medication overuse headache: pathophysiological insights from structural and functional brain MRI research. Headache. 2017;57:1173–1178. doi: 10.1111/head.13037. [DOI] [PubMed] [Google Scholar]
- E54.IHS Classification ICHD-3. www.ichd-3.org/8-headache-attributed-to-a-substance-or-its-withdrawal/ (last accessed on 9 April 2018) [Google Scholar]