Abstract
Peripatellar fat pads are intracapsular extrasynovial adipose cushions that accommodate the changing shape and volume of articular spaces during movement. Variations in bone geometry, passive and active stabilization mechanisms and/or functional demands may lead to peripatellar fat pad abnormalities. While peripatellar fat pads may be affected a variety of conditions such as synovial inflammation, tumor and fibrosis, a mechanical origin should also be considered. Commonly, the clinical term “impingement” is used synonymously in the radiological literature to refer to three distinct entities of structural peripatellar fat pad abnormalities: superolateral the infrapatellar fat pad (Hoffa fat pad) edema, suprapatellar fat pad edema, and prepatellar fat pad edema, implying a mechanical origin of these conditions. The aim of this pictorial review is to describe the normal anatomy of the extensor mechanism of the knee, and discuss the relation of patellofemoral maltracking to the above-mentioned peripatellar fat pad conditions based on current evidence.
Keywords: knee, fat pads, impingement, patellar maltracking
Introduction
Articular fat pads are intra-capsular, synovial-lined accumulations of adipose tissue that occupy potential spaces and irregularities within the joint cavity. They act as flexible, elastic, and displaceable protective cushions that accommodate the changing shape and volume of these spaces during movement. They increase the synovial surface and may promote distribution of lubricant over articular surfaces.1
Peripatellar fat pads include the suprapatellar fat pad, the prefemoral fat pad, and the infrapatellar fat pad (Hoffa fat pad) (Fig. 1). The importance of peripatellar fat pads in normal kinematics of the knee is demonstrated by the fact that resection of Hoffa fat pad alters patellar biomechanics.2 During normal flexion-extension of the knee, the suprapatellar fat pad prevents friction between the quadriceps tendon and femoral condyle, the prefemoral fat pad prevents direct contact between the patella and distal shaft of the femur, and Hoffa fat pad interposes between the trochlear articular surface and the superior tibia posteriorly and patellar ligament anteriorly (Fig. 2). Sustained friction and repetitive microtrauma can both lead to the clinical manifestation of impingement commonly reported as chronic anterior knee pain and commonly present with structural findings observed by MR imaging.
Fig. 1.
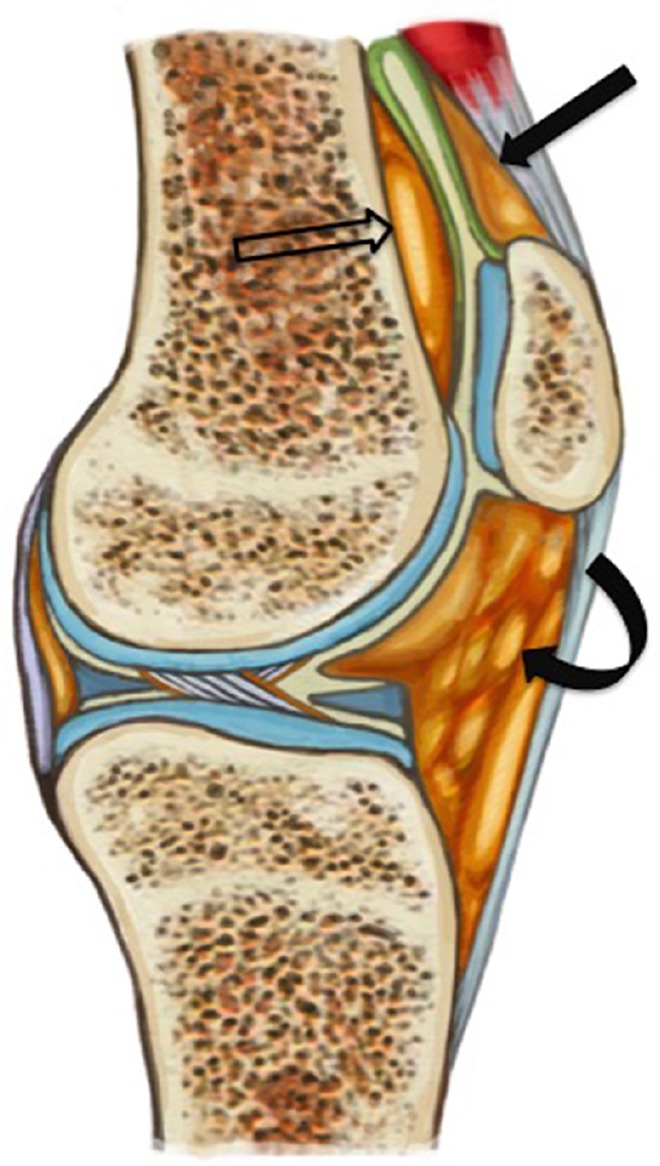
Anatomy of the peripatellar fat pads. The suprapatellar fat pad (solid straight arrow) is triangular in shape, located superior to the patella, posterior to the quadriceps tendon and anterior to the suprapatellar recess. The prefemoral fat pad (empty arrow) is anterior to the distal shaft of the femur and posterior to the suprapatellar recess. Infrapatellar fat pad (Hoffa fat pad) (curved arrow) is inferior to the patella, posterior to the patellar tendon, and anterior to the intercondylar notch.
Fig. 2.
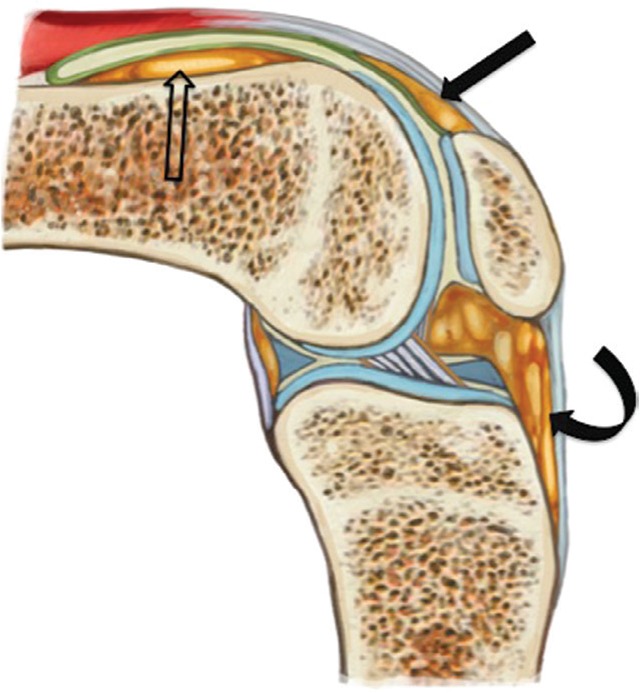
Illustration of the changes in position, shape and morphology of the peripatellar fat pads in extreme flexion of the knee. The suprapatellar fat pad (solid straight arrow) interposes between the quadriceps tendon anteriorly, and femoral condyle posteriorly; the prefemoral fat pad (empty arrow) interposes between the quadriceps tendon anteriorly, and the distal shaft of the femur posteriorly; and the infrapatellar fat pad (Hoffa fat pad) (curved arrow) interposes between the patellar ligament anteriorly, and superior tibia posteriorly.
A variety of pathologic processes can affect the peripatellar fat pads, including synovial proliferation, tumor, and fibrosis. In this manuscript we aim to focus on conditions that are often reported to have a mechanical origin: superolateral Hoffa fat pad (SHFP) edema, suprapatellar fat pad edema, and prefemoral fat pad edema. In addition, it is important to note that certain terms are being used in the context of peripatellar fat pad pathology that need to be clearly defined. In this review we will differentiate among patellofemoral alignment, patellofemoral (mal-)tracking, and peripatellar fat pad impingement. “Patellofemoral alignment” is the static articulation between the patella and the anterior femur; when pathologic it is also called mis- or malalignment. “Patellofemoral tracking” is the dynamic articulation between patella and femur often resulting in lateralization of the patella, i.e. maltracking. “Peripatellar fat pad impingement” is the clinical syndrome that may result from malalignment or maltracking. Imaging will show structural pathology that may be consistent with a clinical syndrome of impingement but the diagnosis is based on clinical presentation.
The aim of this pictorial review is to describe the normal anatomy of the extensor mechanism of the knee, and discuss the relation of patellofemoral maltracking to specific above-mentioned peripatellar fat pad conditions based on current evidence.
Extensor mechanism of the knee
The patella is the largest sesamoid bone of the body. The quadriceps tendon anchors at its upper pole, and the patellar ligament attaches at the lower pole. The patella plays a central role in the extensor mechanism, and acts as a fulcrum, by displacing the quadriceps anteriorly, therefore increasing its mechanical advantage for leg extension. As the quadriceps contracts to extend the knee, the patella sustains a valgus translational force (lateral force away from the midline) as the quadriceps components are in line with the anatomic axis of the femur rather than the anatomic axis of the leg.3 The Q angle formed by a line drawn between the anterior superior iliac spine of the pelvis to the center of the patella, and from the center of the patella to the tibial tuberosity represents an indirect measurement of valgus translational force. In normal conditions, the Q angle has been reported as 11 degrees for men and 16 degrees for women,4 and is increased in patellar maltracking.
Patella alta is defined as a ratio greater than 1.2 between patellar tendon length (distance between inferior-most patella and tibial tuberosity) and patellar length (greater diagonal diameter of the patella). This is also called the Insall-Salvati index.5 A modified Insall-Salvati index—distance between the distal end of the patellar articular surface and tibial tuberosity / length of the patellar articular surface—is less affected by variations of patellar morphology and is more reproducible than the original index. Patella alta is defined by a modified Insall-Salvati index greater than 2.6 Tibial tuberosity-trochlear groove (TT-TG) distance is measured on axial images and represents lateralization of the patella in relation to the insertion of the patella tendon at the tibial tuberosity. The trochlear groove is the deepest cartilaginous point of the most superior image that depicts the complete cartilaginous trochlea. The tibial tuberosity is the center of the patellar tendon insertion onto the tibial tuberosity.7 Normal TT-TG values have been reported between 10 and 13 mm.8–10 A TT-TG distance greater than 20 mm is reportedly associated with pathologic patellar instability10 (Fig. 3). Values between 15 and 20 mm are considered borderline.11
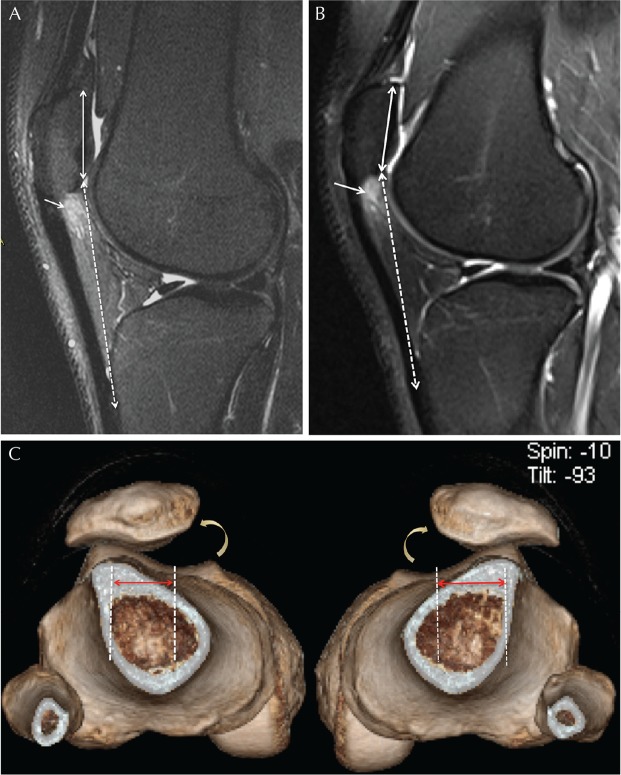
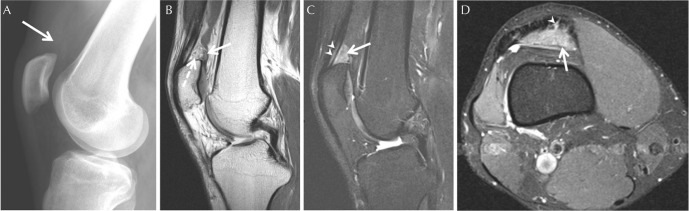
Fig. 3.
Bilateral superolateral infrapatellar fat pad (Hoffa fat pad) impingement in a 28 year-old woman with bilateral anterior knee pain due to patellar maltracking. Sagittal fat-suppressed proton-density MR images (A) of the right and (B) left knees show increased signal (arrow) in the superolateral aspect of Hoffa fat pad bilaterally. Note bilateral high-riding patella with modified Insall-Salvati index of 2.2: the distance between distal patellar articular surface and distal patellar tendon insertion (dashed double end arrow)/patellar length (solid double end arrow) is greater than 2. (C) 3D volume rendered image of both knees shows bilateral lateral patellar tilt (curved arrows), lateral patellar shift with and increased tibial tubercle –femoral trochlear distance (2 cm bilaterally) (double end arrows).
When the knee is in full extension the patella articulates with the shallowest part of the femoral sulcus and the supratrochlear region of the femur that is covered by the prefemoral fat pad and synovium. In this position the femur provides little osseous stability to the patella. As the knee flexes, the patella migrates inferiorly to engage in deeper portion of the trochlea. Therefore, the tendency of the patella to sublux is increased in full extension rather than in flexion, a position where the patella becomes more stable due to its close articulation within the trochlear groove.12 Trochlea dysplasia, commonly defined as a flattened, shallow sulcus results in patellofemoral (PF) incongruity. This results in dependence on soft tissue restraints for patellar stability in order to avoid lateral dislocation. In addition to trochlear dysplasia, abnormal patellofemoral alignment may also result in maltracking. Patellofemoral malalignment may be axial (lateral patellar displacement from excessive lateralization of the tibial tuberosity, measured as TT-TG distance) or sagittal (high riding patella). A recent study showed a positive association between Q angle and TT-TG distance.13
In summary, valgus translational force results in increased shear forces on the lateral patellofemoral joint, which is balanced by proper patellofemoral tracking. Imbalance may result from of combination of variable in bone geometry, function of active and passive soft tissue restraints, and functional demands.3 The peripatellar fat pads are thought to act as protective cushions, therefore, may undergo pathologic changes as a result of patellofemoral maltracking.
Superolateral Hoffa fat pad edema
SHFP edema is a common finding in routine knee MR imaging studies, with a reported prevalence of 13% in a sample of middle-aged individuals with or at risk of osteoarthritis,14 and 50% in a small cohort of 16 asymptomatic female volleyball players.15 Numbers on the prevalence in the general population are not available. SHFP edema is thought to be the imaging correlate of patellofemoral friction syndrome,16 which is characterized by anterior knee pain and tenderness, typically at the lower pole of the patella. The pain is commonly exacerbated by hyperextension and physical examination can demonstrate focal point tenderness at the inferior pole of the patella.
SHFP edema is thought to be a sensitive indicator of subtle patellar maltracking, as several studies have reported strong associations between its presence and morphologic variations such as a high-riding patella (patella alta) and lateral patellar displacement, which is defined as an increased TT-TG distance.14,17–20 Increased TT-TG distance and high riding patella both result in exaggeration of valgus translational force during flexion and therefore result in higher risk of friction of Hoffa fat pad between the lateral femoral condyle and the lateral aspect of the patellar tendon, as seen on MRI. SHFP edema has also been linked to cartilage loss and osteoarthritis of the lateral patellofemoral compartment.21 Both of these findings are related to patellar maltracking.
On MR imaging, sagittal and axial fluid-sensitive images reveal focal increased signal intensity in the superolateral portion of Hoffa fat pad, between the lateral femoral condyle and patellar tendon, described as edema (Table 1).7,21–23 Gadolinium-chelate contrast medium injection may reveal contrast enhancement.7 In addition, Campagna et al. also reported association of SHFP edema with focal tendinopathy of the lateral aspect of the patellar ligament opposite the lateral trochlea, and with a short distance between the lateral femoral condyle and patellar ligament17 (Figs. 4 and 5).
Table 1.
Peripatellar fat pad abnormalities and relationship to anterior pain, patellar maltracking and patellofemoral degeneration
| MR findings | Mechanism – relation to patellar maltracking | Patellofemoral osteoarthritis | Association to anterior knee pain | |
|---|---|---|---|---|
| Superolateral Hoffa fat pad edema | Hyperintense edema-like signal at the superolateral corner of Hoffa fat pad (between patellar tendon and lateral femoral condyle) | Yes (both sagittal and axial malalignment) | Yes | Yes |
| Suprapatellar fat pad edema | Edema-like signal intensity +/− convex appearance toward the suprapatellar pouch | No | Yes | Controversial |
| Prefemoral fat pad edema | Edema-like signal intensity +/− swelling | Possible* | Yes | Controversial |
reported association with superolateral fat pad edema. No reported association with parameters of patellar maltracking. Hoffa fat pad, infrapatellar fat pad.
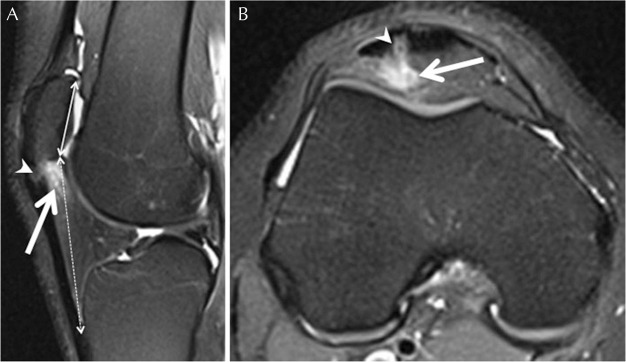
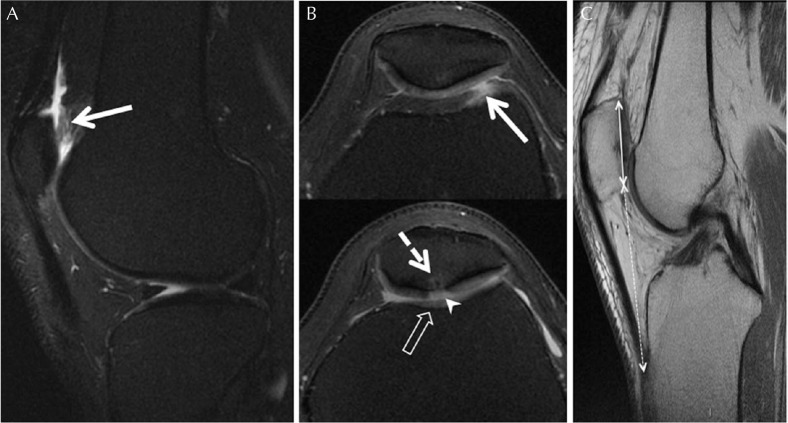
Fig. 4.
Superolateral infrapatellar fat pad (Hoffa fat pad) impingement in a 46-year-old woman with lateral infrapatellar knee pain. (A) Sagittal and (B) axial fat-suppressed proton-density MR images reveal high signal intensity (edema) in the superolateral aspect of Hoffa fat pad between the lateral aspect of the patellar tendon and the lateral femoral condyle (solid arrow). Additionally there is focal thickening and increased signal in the lateral aspect of the patellar tendon consistent with tendinosis (arrowhead). Note high riding patella with a modified Insall-Salvati: distance between distal patellar articular surface and distal patellar tendon insertion (dashed double end arrow)/patellar length (solid double end arrow) is 2.4 (greater than 2). No trochlear dysplasia or lateral patellar displacement was found in this case.
Fig. 5.
Superolateral infrapatellar fat pad (Hoffa fat pad) impingement in a 37-year-old man. (A) Sagittal and (B) axial fat-suppressed proton-density weighted MR images demonstrate high signal in the superolateral aspect of Hoffa fat pad between the lateral aspect of the patellar tendon and the lateral femoral condyle (arrow). Note short distance between the lateral aspect of the patellar tendon and the lateral femoral condyle (solid line). Modified Insall-Salvati ratio was within normal limits in this case, although the tibial tubercle - trochlear groove distance (not shown) at 20 mm was consistent with lateral patellar shift.
SHFP impingement is usually successfully managed with conservative therapy, including physical therapy targeted at restoring the biomechanics of patellar tracking and taping in an attempt to unload the inferior fat pad.24
Prefemoral fat pad edema
The literature is limited regarding this entity, which is thought to be under-recognized,7 and is sometimes referred to as impingement. Anterior knee pain is a commonly reported presenting symptom, sometimes debilitating, proximal to the superior pole of the patella, with a possible catching sensation resulting from the fat pad snapping over the femoral condyle.3,25
MR imaging shows edema and enlargement of the prefemoral fat pad characterized by high signal intensity on fluid sensitive images, and low signal intensity on T1-weighted images, better appreciated on sagittal and axial planes (Table 1) (Figs. 6 and 7).7 Two patterns of prefemoral fat pad edema have been described. One, at the superior central part of the fat pad (closer to midline on axial views), is believed to be related to a prominent superior patellar osteophyte causing impingement. The second pattern is described at the inferolateral part (away from midline on axial views) of the prefemoral fat pad, and has been found to have high association with patellofemoral friction syndrome.26 This association was also supported by another study showing prefemoral fat pad edema present in 68% of the patients with knee pain and SHFP edema21 (Fig. 6). However to the best of our knowledge, no association between prefemoral fat pad edema and measurements of patellar maltracking have been reported.
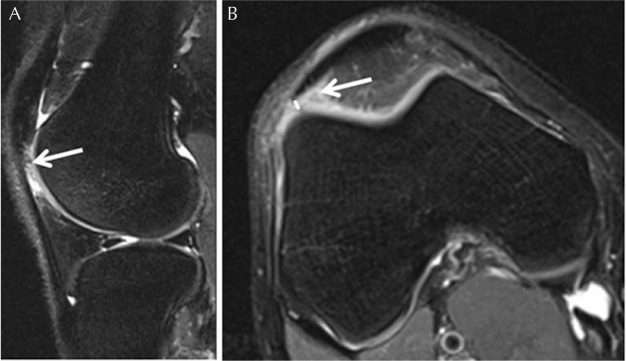
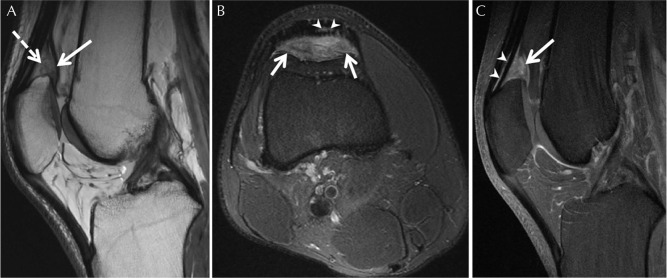
Fig. 6.
Prefemoral fat pad impingement in a 42-year-old woman with anterior pain of the right knee. (A) Sagittal proton-density MR image. (B) Sagittal fat-suppressed proton-density MR image. (C) Axial fat-suppressed proton-density MR image. Enlargement and signal change of the inferolateral aspect of the prefemoral fat pad (low signal on proton-density and high signal on fat-suppressed proton-density, as shown by solid arrows) with bulging and mass effect toward the suprapatellar pouch, and associated joint knee effusion (arrowheads). Note associated full-thickness cartilage defect and bone marrow lesion of the lower patella (asterisk), and edema of the superolateral aspect of the infrapatellar fat pad (Hoffa fat pad) (curved arrow) consistent with associated patellofemoral maltracking. Note high riding patella with modified Insall Salvati ratio: distance between distal patellar articular surface and distal patellar tendon insertion (dashed double end arrow)/patellar length (solid double end arrow) measured at 2.4 (greater than 2).
Fig. 7.
Prefemoral fat pad impingement in a 44-year-old woman with chronic, anterior pain of the left knee. (A) Sagittal and (B) axial fat-suppressed T2-weighted images show enlargement and high signal intensity of the inferolateral aspect of the prefemoral fat pad (solid arrow) associated with full-thickness cartilage loss (arrowhead) and a bone marrow lesion (dashed arrow) of the patellar apex. Note shallow trochlear groove (empty arrow) consistent with patellofemoral maltracking. (C) Sagittal proton density MR image shows high riding patella with modified Insall Salvati ratio: distance between distal patellar articular surface and distal patellar tendon insertion (dashed double end arrow) / patellar length (solid double end arrow) measured at 2.1 (greater than 2) also consistent with patellar maltracking.
Management is initially conservative with analgesia, anti-inflammatory medications, and physiotherapy, consisting of stretching the quadriceps and flexor muscles to decrease the downward pressure of the patella on the fat pad.7 Kim et al. reported about a case of arthroscopic removal of a partially fibrosed prefemoral fat pad with complete resolution of symptoms and no recurrence at 1-year follow-up.25
Suprapatellar fat pad edema
The suprapatellar fat pad is the smallest of the fat pads in the anterior knee with a triangular shape and measuring on average less than 7–8 mm.27 It fills the gap between the posterior part of the quadriceps tendon insertion and the posterior superior aspect. It is separated posteriorly from the prefemoral fat pad by the joint recess. The quadriceps tendon is continuous with the fat pad and contains the most adipose tissue between its fibers at its entheses, also called endotenon fat.28 Endotenon is the connective tissue that separates adjacent tendon fascicles. This term has been used to refer to what should, strictly speaking, be called “endoligament”. In the distal attachment of the quadriceps tendon, the endotenon fat is prominent, which is thought to increase the surface area of the tendinous attachment to bone where load is transferred, thus dissipating stress.28 The endotenon fat may also act as a mechanosensory organ. Biomechanically, the suprapatellar fat pad improves the patellofemoral engagement of the extensor mechanism. Edema of the suprapatellar fat pad is found in 12 to 14% of patients undergoing knee MR imaging,29,30 but its relationship to anterior knee pain is subject to controversy.29,30 Suprapatellar fat pad edema may be similar to Hoffa disease, as suggested by similar histologic changes.31 However, it has also been suggested that suprapatellar fat pad edema may result from repetitive friction against the trochlea during high angle knee flexion (Fig. 2).7,30,32
The term “impingement” has been increasingly used for suprapatellar fat pad edema,7,33,34 although there is no evidence to support a mechanical origin of this condition. In fact, prior retrospective studies showed no association between suprapatellar fat pad edema and measurement of patellar maltracking.29,30 However a recent study reported an association between suprapatellar fat pad edema and degeneration of the patellofemoral joint over a 48 months.35
On MR imaging, the suprapatellar fat pad exhibits an increase in size with mass effect (convex appearance toward the suprapatellar joint recess), with high signal on fluid sensitive images, and low signal on T1-weighted images (lower than subcutaneous fat).30,31 The mass effect was reported to be more likely present as the fat pad signal approaches fluid (Table 1).30 In addition, edema may extend to the endotenon fat within the adjacent quadriceps tendon. (Figs. 8 and 9).28
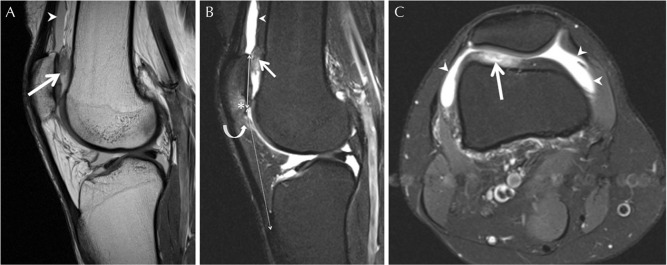
Fig. 8.
Suprapatellar fat pad impingement in a 35-year-old man with intermittent, progressively increasing anterior knee pain. (A) Lateral radiograph shows obliteration of the suprapatellar fat (arrow). (B) Sagittal proton-density MR image reveals enlargement and convex contour of the suprapatellar fat pad toward the suprapatellar pouch (solid arrow). Internal areas of thickening and signal change (dashed arrows) in comparison with the infrapatellar fat pad (Hoffa fat pad) indicate inflammation. (C) Sagittal fat-suppressed T2-weighted and (D) axial fat-suppressed proton-density images reveal high signal intensity, enlargement, and mass effect of the suprapatellar fat pad (solid arrow). Note extension of the signal change within the endotenon fat in the quadriceps enthesis (arrowheads).
Fig. 9.
Suprapatellar fat impingement in a 29-year-old woman with chronic anterior knee pain. (A) Sagittal proton-density MR image shows enlargement and mass effect of the suprapatellar fat pad (solid arrow). Note low signal intensity within the fat pad in comparison with other adipose structures in the knee joint that are indicative of inflammation (dashed arrows). (B) Axial fat-suppressed proton-density image reveals high signal intensity and enlargement of the fat pad extending into the endotenon fat of the distal quadriceps entheses (arrowheads). (C) Sagittal fat-suppressed gadolinium-chelate contrast medium-enhanced T1-weighted image shows diffuse homogenous contrast enhancement within the suprapatellar fat pad extending into the endotenon fat within the distal quadriceps enthesis (arrowheads).
There are sparse reports on therapeutic management of suprapatellar fat pad edema, although steroid injection was reported in one patient, yielding an excellent response and no adverse effects over a course of 4 months.36
Conclusion
In this article, we reviewed the pathophysiology and imaging presentations of peripatellar fat pad impingement syndromes. There has been a recent surge of interest in SHFP edema in the radiologic literature, suggesting an association with not only patellar maltracking but also patellofemoral osteoarthritis. Such association is less clear for prefemoral fat pad edema, and absent for suprapatellar fat pad edema.
Footnotes
Conflicts of Interest
Dr. Guermazi is consultant to Sanofi-Aventis, Merck Serono, orthotrophix, AstraZeneca and TissueGene and is shareholder of Boston Imaging Core Lab (BICL), LLC. Dr. Roemer is shareholder of BICL, LLC. None of the other authors declare any conflict of interest.
References
- 1.Soames RW, et al. Skeletal system, In: Williams PL, Bannister LH, Berry MM, et al. eds. Gray’s anatomy: the anatomical basis of medicine and surgery. 38th edition New York: Churchill Livingstone, 1995; 497–736. [Google Scholar]
- 2.Bohnsack M, Wilharm A, Hurschler C, Rühmann O, Stukenborg-Colsman C, Wirth CJ. Biomechanical and kinematic influences of a total infrapatellar fat pad resection on the knee. Am J Sports Med 2004; 32:1873–1880. [DOI] [PubMed] [Google Scholar]
- 3.Elias DA, White LM. Imaging of patellofemoral disorders. Clin Radiol 2004; 59:543–557. [DOI] [PubMed] [Google Scholar]
- 4.Horton MG, Hall TL. Quadriceps femoris muscle angle: normal values and relationships with gender and selected skeletal measures. Phys Ther 1989; 69:897–901. [DOI] [PubMed] [Google Scholar]
- 5.Insall J, Salvati E. Patella position in the normal knee joint. Radiology 1971; 101:101–104. [DOI] [PubMed] [Google Scholar]
- 6.Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res 1992; (282):170–176. [PubMed] [Google Scholar]
- 7.Grando H, Chang EY, Chen KC, Chung CB. MR imaging of extrasynovial inflammation and impingement about the knee. Magn Reson Imaging Clin N Am 2014; 22:725–741. [DOI] [PubMed] [Google Scholar]
- 8.Song EK, Seon JK, Kim MC, Seol YJ, Lee SH. Radiologic measurement of tibial tuberosity-trochlear groove (TT-TG) distance by lower extremity rotational profile computed tomography in Koreans. Clin Orthop Surg 2016; 8:45–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop 2011; 35:1799–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994; 2:19–26. [DOI] [PubMed] [Google Scholar]
- 11.Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics 2010; 30:961–981. [DOI] [PubMed] [Google Scholar]
- 12.Tria AJ, Alicea JA. Embryology and anatomy of the patella, In: Scuderi GR, ed. The patella. New York: Springer-Verlag,1995; 11–23. [Google Scholar]
- 13.Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W. Correlation of the tibial tuberosity-trochlear groove distance with the Q-angle. Knee Surg Sports Traumatol Arthrosc 2016; 24:915–920. [DOI] [PubMed] [Google Scholar]
- 14.Widjajahakim R, Guermazi A, Jarraya M, et al. The relation of patellofemoral joint alignment and trochlear morphology to superolateral Hoffa’s fat pad edema: the most study. Osteoarthritis Cartilage 2016; 24:S423. [Google Scholar]
- 15.Mehta K, Wissman R, England E, D’heurle A, Newton K, Kenter K. Superolateral Hoffa’s fat pad edema in collegiate volleyball players. J Comput Assist Tomogr 2015; 39:945–950. [DOI] [PubMed] [Google Scholar]
- 16.Chung CB, Skaf A, Roger B, Campos J, Stump X, Resnick D. Patellar tendon-lateral femoral condyle friction syndrome: MR imaging in 42 patients. Skeletal Radiol 2001; 30:694–697. [DOI] [PubMed] [Google Scholar]
- 17.Campagna R, Pessis E, Biau DJ, et al. Is superolateral Hoffa fat pad edema a consequence of impingement between lateral femoral condyle and patellar ligament? Radiology 2012; 263:469–474. [DOI] [PubMed] [Google Scholar]
- 18.De Smet AA, Davis KW, Dahab KS, Blankenbaker DG, del Rio AM, Bernhardt DT. Is there an association between superolateral Hoffa fat pad edema on MRI and clinical evidence of fat pad impingement? AJR Am J Roentgenol 2012; 199:1099–1104. [DOI] [PubMed] [Google Scholar]
- 19.Jibri Z, Martin D, Mansour R, Kamath S. The association of infrapatellar fat pad oedema with patellar maltracking: a case-control study. Skeletal Radiol 2012; 41:925–931. [DOI] [PubMed] [Google Scholar]
- 20.Matcuk GR, Cen SY, Keyfes V, Patel DB, Gottsegen CJ, White EA. Superolateral Hoffa fat-pad edema and patellofemoral maltracking: predictive modeling. AJR Am J Roentgenol 2014; 203:W207–W212. [DOI] [PubMed] [Google Scholar]
- 21.Subhawong TK, Eng J, Carrino JA, Chhabra A. Superolateral Hoffa’s fat pad edema: association with patellofemoral maltracking and impingement. AJR Am J Roentgenol 2010; 195:1367–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saddik D, McNally EG, Richardson M. MRI of Hoffa’s fat pad. Skeletal Radiol 2004; 33:433–444. [DOI] [PubMed] [Google Scholar]
- 23.Roemer FW, Jarraya M, Felson DT, et al. Magnetic resonance imaging of Hoffa’s fat pad and relevance for osteoarthritis research: a narrative review. Osteoarthr Cartil 2016; 24:383–397. [DOI] [PubMed] [Google Scholar]
- 24.Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med 2012; 42:51–67. [DOI] [PubMed] [Google Scholar]
- 25.Kim YM, Shin HD, Yang JY, Kim KC, Kwon ST, Kim JM. Prefemoral fat pad: impingement and a mass-like protrusion on the lateral femoral condyle causing mechanical symptoms. A case report. Knee Surg Sports Traumatol Arthrosc 2007; 15:786–789. [DOI] [PubMed] [Google Scholar]
- 26.Zakhary M, Slattery TR, Thein R, Shabshin N, Schweitzer ME. Prefemoral fat pad edema in the knee. MRI findings in 44 patients along with clinical correlation and assessment of prevalence. Radiological Society of North America 2012 Scientific Assembly and Annual Meeting; November 27, 2012; Chicago IL. [Google Scholar]
- 27.Staeubli HU, Bollmann C, Kreutz R, Becker W, Rauschning W. Quantification of intact quadriceps tendon, quadriceps tendon insertion, and suprapatellar fat pad: MR arthrography, anatomy, and cryosections in the sagittal plane. AJR Am J Roentgenol 1999; 173:691–698. [DOI] [PubMed] [Google Scholar]
- 28.Benjamin M, Redman S, Milz S, et al. Adipose tissue at entheses: the rheumatological implications of its distribution. A potential site of pain and stress dissipation? Ann Rheum Dis 2004; 63:1549–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsavalas N, Karantanas AH. Suprapatellar fat-pad mass effect: MRI findings and correlation with anterior knee pain. AJR Am J Roentgenol 2013; 200:W291–W296. [DOI] [PubMed] [Google Scholar]
- 30.Roth C, Jacobson J, Jamadar D, Caoili E, Morag Y, Housner J. Quadriceps fat pad signal intensity and enlargement on MRI: prevalence and associated findings. AJR Am J Roentgenol 2004; 182:1383–1387. [DOI] [PubMed] [Google Scholar]
- 31.Shabshin N, Schweitzer ME, Morrison WB. Quadriceps fat pad edema: significance on magnetic resonance images of the knee. Skeletal Radiol 2006; 35:269–274. [DOI] [PubMed] [Google Scholar]
- 32.Huberti HH, Hayes WC, Stone JL, Shybut GT. Force ratios in the quadriceps tendon and ligamentum patellae. J Orthop Res 1984; 2:49–54. [DOI] [PubMed] [Google Scholar]
- 33.Gutierrez LB, Morgan TA, Link T, Feeley B, Motamedi D. Utility of musculoskeletal ultrasound in the diagnosis and treatment of suprapatellar fat pad impingement: a case report. J Clin Case Rep 2016; 6:837. doi: 10.4172/2165-7920.1000837 [DOI] [Google Scholar]
- 34.Bas A, Tutar O, Yanik I, Samanci C. Quadriceps fat-pad impingement syndrome: MRI findings. BMJ Case Rep 2012; doi: 10.1136/bcr-2012-007643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwaiger BJ, Wamba JM, Gersing AS, Nevitt MC, McCulloch CE, Link TM. Signal intensity alteration in the suprapatellar fat pad is associated with degeneration of the patellofemoral joint over 48 months – Data from the osteoarthritis initiative. Osteoarthritis Cartilage 2016; 24:S267–S268. [Google Scholar]
- 36.Van Le B, Harish S. Quadriceps fat pad edema: sonographic depiction and sonographically guided steroid injection. J Ultrasound Med 2009; 28:959–962. [DOI] [PubMed] [Google Scholar]