Abstract
Objectives:
To present the findings of a systematic review on the use of simulation-based learning experiences (SBLEs) to teach communication skills to nursing students and clinicians who provide palliative and end-of-life care to patients and their families.
Background:
Palliative care communication skills are fundamental to providing holistic patient care. Since nurses have the greatest amount of direct exposure to patients, building such communication competencies is essential. However, exposure to patients and families receiving palliative and end-of-life care is often limited, resulting in few opportunities to learn these skills in the clinical setting. Simulation-based learning experiences can be used to supplement didactic teaching and clinical experiences to build the requisite communication skills.
Methods:
Searches of CINAHL, MEDLINE, PsychINFO, ERIC, and Web of Science electronic databases and Grey Literature returned 442 unique records. Thirty articles met the established criteria, including the SBLE must contain a nursing role.
Results:
Simulation-based learning experience are being used to teach palliative and end-of-life communication skills to nursing students and clinicians. Lack of standardization, poor evaluation methods, and limited exposure to the entire interprofessional team makes it difficult to identify and disseminate validated best practices.
Conclusion:
While the need for further research is acknowledged, we recommend this evidence be augmented by training programs that utilize SBLEs through (1) applying standards, (2) clearly specifying goals and objectives, (3) integrating externally validated scenarios, and (4) employing rigorous evaluation methods and measures that link the SBLE to the training objectives and desired clinician practice behaviors and patient outcomes.
Keywords: simulation, communication, end of life, palliative care, nursing education, interprofessional
Introduction
Effective communication among members of the interprofessional team and with the patient is essential to achieving desired patient outcomes. Curricula for members of the health-care team are replete with objectives focused on developing communication skills; however, curricula that outline specific communication skills needed in palliative and end-of-life (EOL) care remain deficient. Recent national reports have emphasized the need to improve primary palliative care, including patient-centered communication, which focuses on fostering healing relationships, exchanging information, and responding to emotions, for both students and clinicians.1–3 As a result, educators are increasingly using simulation-based learning activities to help build critical communication skills in the clinical setting.4 As frontline providers of care, nurses are key members of the interprofessional team. The purpose of this article is to report the findings of a systematic review designed to identify how simulation is being used to teach communication skills to nursing students and clinicians who care for patients and families receiving palliative and EOL care.
Palliative care communication skills are essential to providing patients with effective symptom management, psychosocial and spiritual support, and advance care planning.5 For nurses, the ability to develop skills in caring for dying patients and their families is a significant professional rite of passage—one that they remember for the remainder of their careers.6,7 As nurses develop skills in caring for dying patients, they gain more confidence in the care they provide.8 Students who participate in palliative care immersion experiences that allow them to hone their communication skills report they feel better prepared to care for dying patients in their first year of professional practice.9
Time constraints and limited availability of clinical settings in nursing education may not allow direct experience in palliative and EOL care for large cohorts of nursing students. Therefore, most new nurses must develop communication competencies in palliative and EOL care on the job, which is not ideal and can be unnecessarily anxiety-provoking.10 Furthermore, nurse clinicians—who are accustomed to advocating for their patients’ needs—cite a need for more education on palliative and EOL care.11–13 The use of simulation-based learning may enable educators to reach greater numbers of nursing students and clinicians to foster the development of these important communications skills.14
Simulation-based learning experiences (SBLEs) offer an opportunity to enhance students’ and clinicians’ communication skills. Simulation typically involves mimicking the real-world scenarios to provide learners with pertinent experiences under controlled or practice conditions.15,16 The SBLEs involve a variety of simulated learning methods, including manikin-based, standardized/simulated patients or computer-based programs, virtual reality, or hybrid simulation to achieve realistic environments representative of the learner’s professional responsibilities.17 An important concept in SBLEs is fidelity, defined as “the degree to which a simulated learning experience approaches reality.”18 Fidelity goes beyond the manikin itself and includes environmental fidelity, conceptual fidelity, and psychological fidelity. Fidelity allows the SBLE to replicate the practice environment, typically the hospital, as closely as possible and allows learners to practice their skills in a safe environment.
In the following sections, we report the methods and findings of a systemic review of the literature for SBLE exemplars focused on palliative care and EOL communication that include the nursing role. For this article, SBLE is defined as a method of accomplishing learning goals through interacting with people, simulators, computers, or task trainers that in some way mimic or represent the real-world experiences and responsibilities, adapted from Agency for Healthcare Research and Quality’s definition.17 The communication component of the SBLE is defined as the exchange of thoughts, messages, or information related to palliative care or EOL care through speech and behavior using actors or artifacts to represent patients, families, caregivers, or members of health-care teams.
Methods
Data Sources
The sponsoring institution’s nursing librarian, with the other coauthors of the article, performed a comprehensive systematic literature search on February 15, 2017, of the PubMed, CINAHL, ERIC, Web of Science, and PsycINFO databases. Searches of the grey literature resources—ProQuest Dissertations & Theses Global, Worldcat Dissertations and Theses, and NLM Gateway—were also performed. All search strategies included terms related to the concepts of simulation, palliative care, EOL, and nursing. The complete strategy is available upon request. No date, study, or subject filters were applied. Comprehensive details of the protocol for this systematic review were registered on PROSPERO at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017058046.19
Inclusion and Exclusion Criteria
Explicit inclusion and exclusion criteria were established to ensure a uniform selection of articles amongst reviewers. The inclusion criteria were articles that (1) described a simulated learning experience that (a) involved technology (b) was delivered to nursing students or practicing nurses (c) and focused on palliative care or EOL communication and (2) included an evaluative component. The exclusion criteria were letters, commentaries, news items, and articles not published in English. In addition, we excluded articles that did not provide a description of the sample, lacked evaluation results, or had insufficient details about the learning scenarios. These criteria excluded articles that did not provide sufficient details to determine whether an SBLE involving communication was performed and evaluated. A list of articles excluded during the full-text review phase and the rationale for exclusions are available upon request. Our final list of 30 articles includes all instances of SBLEs in which other health disciplines were either included in the scenarios or participated in the training. The list, however, does not include interprofessional SBLEs that took place without direct involvement from the nursing profession (an inclusion criteria).
Review Process
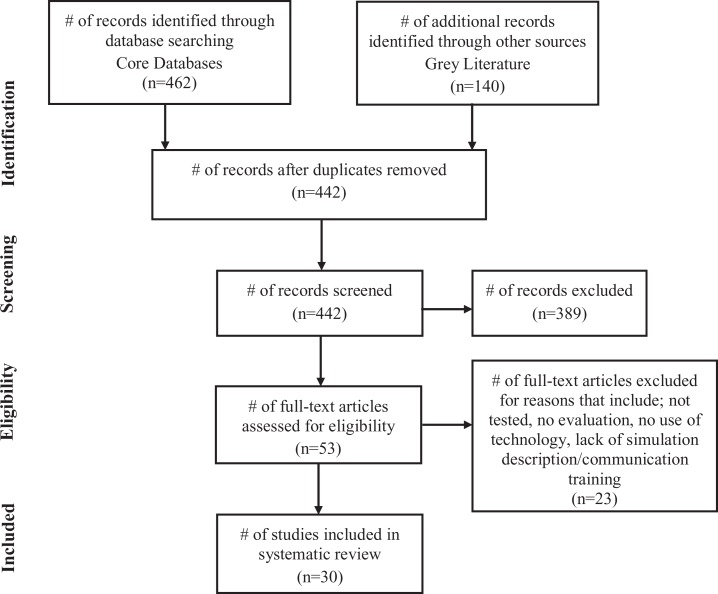
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram20 (Figure 1) lists the number of articles included during each phase of the systematic review (identification, screening, eligibility, included). The database and grey literature search identified 442 studies, excluding duplicates. During the screening phase, 2 reviewers (M.S. and T.M.) independently reviewed all abstracts for inclusion and exclusion criteria. Disagreements between reviewers were resolved through discussion and consensus (M.S., T.M., G.K.). All articles that met the inclusion criteria and none of the exclusions or had abstracts with insufficient information available to determine whether they met inclusion status were moved to the eligibility (full text) review phase. Two reviewers separately (M.S. and T.M.) evaluated 53 full-text articles during the eligibility review phase to confirm those that met all of the inclusion and none of the exclusion criteria. All discrepancies between the 2 reviewers in this phase were resolved by a third reviewer (G.K.). In total, 30 articles matched the eligibility criteria.
Figure 1.
PRISMA flow diagram illustrating the selection process of articles.
Kirkpatrick’s Level of Evaluation
The Kirkpatrick Model21,22 was used to differentiate the level of evaluation assessment completed for the training reported in each of the articles reviewed. The model consists of 4 levels: (1) participants responses—REACTION—to training (eg, satisfaction); (2) extent of knowledge, attitude, or skills gained—LEARNING; (3) extent to which desired behaviors are being used on the job—BEHAVIOR; and (4) extent to which desired behaviors are producing the desired outcomes in practice—RESULTS— (eg, achieving desired patient outcomes). The level of evaluation for each article is reported in the last column of Table 1.
Table 1.
Summary of SBLE Facets and Communication Components of Included Articles.
| Citation | Palliative Care and End-of-Life Communication Topics and Methods | Simulation Components | Scenario Facets and Participants | Evaluation Level and Results |
|---|---|---|---|---|
| Betcher23 | Topics: end-of-life (EOL) goals; advanced care planning; grief support; family conflict related to EOL wishes Methods: patient/family conversations; debriefing using videotaped simulations in group including the actors, registered nurses (RNs), chaplain, RNs from a hospice agency | Technology: simulations were videotaped Features: role-play using actors; lectures | Scenario: hospitalized adult patient with advanced disease Externally developed: no Audience: 8 inpatient RNs; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: Caring Efficacy Scale (CES) pre–postsimulation Results: Scores increased by an average of 11% |
| Bodine and Miller24 | Topics: grief; cultural considerations; fearful patient; symptom management Methods: patient/family conversations; debriefing facilitated by emergency department (ED) resident | Technology: high-fidelity simulator; video clips Features: lectures; case studies; scripted role-play using ER resident | Scenario: terminally ill adult in distress Externally developed: no Audience: 53 ER RNs randomly assigned to SimMan or No SimMan training; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: Adapted ELNEC Knowledge Assessment test pre–postsimulation Results: improvement in EOL communication for simulation group nonsignificant |
| Carman et al25 | Topics: medicolegal considerations; interpersonal family conflicts; transition to palliative care Methods: patient/family/provider conversations; debriefing facilitated by faculty | Technology: high-fidelity simulator; video clip Features: lectures; role play using faculty members (medical role) and students | Scenario: hospitalized adult with neurocranial Hemorrhage Externally developed: no Audience: 71 first-semester accelerated BSN students; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: Frommelt Attitudes on Care of the Dying (FATCOD) Scale pre–postsimulation Results: Improvement in total FATCOD scores (P < .010) |
| Coyle et al26 | Topics: discuss death; dying and EOL goals of care; aid decision-making; respond empathetically to patient emotions Methods: patient/family conversations; debriefing including participants and actors | Technology: video clips Features: lectures; scripted role-play scenarios using actors (medicine) | Scenario: hospitalized adult Externally developed: adapted Memorial Sloan Kettering Cancer Center module for EOL care Audience: 247 inpatient oncology RNs | Kirkpatrick: levels 1 and 2 Tool: assess confidence with EOL communication and satisfaction Results: significant perceived increase in confidence pre–post (retrospective); high satisfaction |
| Dame and Hoebeke27 | Topics: symptom management; discuss EOL issues; provide comfort to family member; offer options for spiritual support Methods: patient/family conversations; debriefing with students | Technology: high-fidelity simulator Features: scripted role play using actor and students | Scenario: hospice adult with terminal lung cancer Externally developed: no Audience: 57 sophomore BSN students | Kirkpatrick: level 2 Tool: FATCOD-B pre–postsimulation Results: increase in posttest mean showing increased positive beliefs and feelings about the dying (P < .001) |
| Eaton et al28 | Topics: mediation of conflict related to cultural preference about funeral and body preparation; care needs of patient in pain Methods: patient/family conversations; debriefing using videotaped simulations | Technology: high-fidelity simulator; simulations were videotaped Features: role-play using actors and students | Scenario: hospice care adult Externally developed: adapted Scheikl and O’Neill (2009) scenario Audience: 30 senior BSN students; observed and participated as nurse or other role | Kirkpatrick: level 3 Tool: open-ended questions post simulation and postclinical practicum Results: 3 qualitative themes emerged; experiential learning, affirmative outcomes, and family as client |
| Ellman et al29 | Topics: advanced care planning; spiritual needs; cultural issues Methods: multidisciplinary team conversations; family conversations | Technology: online module; video clips Features: workshop; role-play using students | Scenario: adult patients with cancer Externally developed: no Audience: 217 interprofessional students in nursing, medicine, chaplaincy, social work; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: open-ended questions Results: perception of enhanced communication through family meeting |
| Fabro et al30 | Topics: symptom management; acknowledgement of family concerns; provide encouragement and family comfort; spiritual care Methods: patient/family conversations; debriefing using guide with questions | Technology: high-fidelity simulator Features: role-play using students (other team members/hospitalist) | Scenario: hospitalized adult patient Externally developed: no Audience: 21 senior BSN students; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: qualitative analysis of student reflection articles Results: perceived simulation enhanced learning |
| Fluharty et al31 | Topics: symptom management; promote comfort to patient; communicate compassionately with patient and family Methods: patient/family conversations; debriefing | Technology: high-fidelity simulator; audio-recorded lecture Features: scripted role-play using students | Scenario: hospice care adult Externally developed: no Audience: 370 BSN and ABSN students; observed and participated as nurse or other role | Kirkpatrick: levels 1 and 2 Tool: (1) EOL knowledge questionnaire pre–postsimulation; (2) Modified version of the Nurse Self-Concept Questionnaire; (3) End-of-Life Communication Assessment Tool post simulation; (4) Satisfaction with Instructional method questionnaire Results: (1) Improved EOL care knowledge scores (P < .000); (2) mean 6.86 (SD .61) on 1-8 scale; (3) mean 4.33 (SD .56) on 1-5 scale; (4) mean 4.07 (SD .81) on 1-5 scale |
| Forster and Donovan32 | Topics: unsuccessful resuscitation of neonate; emergency care; bereavement with family; unexpected death; grief Methods: patient/family/provider conversations; debriefing using video-recorded simulation | Technology: high-fidelity simulator; video recording of simulation Features: role-play using faculty member | Scenario: neonatal special care nursery in which babe suffers cardiac arrest Externally developed: no Audience: 10 senior dual-degree nurse midwives; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: qualitative analysis of debriefing transcripts Results: 4 qualitative themes emerged: feeling unprepared, communication changes, the value of the simulation and personal reactions to neonatal death |
| Gillan et al33 | Topics: discussion about transitioning to EOL care; discussion about organ donation; symptom management; providing support to family Methods: family/provider conversations | Technology: medium-fidelity manikin Features: role-play using actors as family | Scenario: terminally ill adult patient hospitalized due to acute respiratory arrest Externally developed: no Audience: 15 undergraduate students from nursing, social work, pharmacy, medicine; participated as nurse or other role | Kirkpatrick: level 1 Tool: quantitative and qualitative evaluation postsimulation interprofessional team experience Results: recognize the importance of interprofessional team work in palliative care setting |
| Gillan et al34 | Topics: symptom management; EOL care Methods: family/patient/provider conversations; debriefing using video recording of simulation | Technology: high-fidelity simulator; video recording of simulation Features: lectures; group tutorial sessions; role-play using students | Scenario: hospitalized adult patient Externally developed: no Audience: 120 junior BSN students; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: evaluation surveys post simulation Results: students perceived simulation as a valuable learning tool for EOL care |
| Gotwals and Scholtz35 | Topics: holistic care planning; bio-psycho-spiritual aspects; family composition, socioeconomic status; therapeutic and nontherapeutic communication; coping; support; grief Methods: film in nursing education; debriefing pre, during, post simulation | Technology: cinema education Features: brief presentations by students on topics associated with the movie during its showing | Scenario: pediatric patient Externally developed: use of “A Lion in the House” (2006) for cinema education-based scenario Audience: junior nursing students; observed only (N unspecified) | Kirkpatrick: level 1 Tool: review of mock care plans and qualitative comments on experience Results: feel better prepared to provide EOL care; learning objectives achieved |
| Grossman36 | Topics: cardiac arrest experience; giving bad news to family; decision-making; working in collaboration with palliative care team Methods: patient/family conversations; debriefing postsimulation using Palliative Care of Dying Critically Ill Patients Algorithm | Technology: high-fidelity simulator Features: role-play using students | Scenario: ICU hospitalized patients Externally developed: no Audience: 50 senior nursing students; observed and participated as nurse or other role | Kirkpatrick: levels 1 and 2 Tool: ELNEC_KAT 50-items and Palliative Care with Critically Ill Survey pre–postsimulation Results: improved mean ELNEC-KAT post-test scores (P <.000); perceived comfort level working with EOL patient doubled (from 3 to 6 on 1-10 scale) |
| Hamilton et al37 | Topics: symptom management; conflict with family regarding transferring to hospice care; acceptance of a terminal diagnoses Methods: family/patient/provider conversations; debriefing postsimulations | Technology: virtual reality (second life); phone; video clips Features: lecture; training on communication skills; role-play with hospice staff educators | Scenario: hospice patients Externally developed: no Audience: 229 nurses and social workers randomly assigned to 3 groups: virtual reality, phone, or role-play; participated as nurse or other role | Kirkpatrick: levels 1 and 2 Tool: Learners were scored on 4 communication aspects using guided rubrics across 3 scenarios pre–post; satisfaction surveys Results: Phone and second life resulted in greater improvement in communication skills; 85% rated program’s effectiveness as excellent or very good |
| Hjelmfors et al38 | Topics: spiritual and existential needs; ethical views; symptom management; giving bad news Methods: patient/family conversations; debriefing | Technology: high-fidelity simulator; video recordings of simulation; audio-recording of debriefing Features: role-play using actors; tutorial group; lectures; readings about scenario | Scenario: home care adult patient Externally developed: no Audience: 60 junior nursing students; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: evaluation of recorded simulation and guided debriefing Results: satisfaction with simulation; opportunity to practice handling challenging communicative situations with patients and family members |
| Kopka et al39 | Topics: symptom management; caregiving; provide sympathy, reassurance; grief; necessary arrangements after death Methods: family/patient/provider conversations; debriefing facilitated by faculty | Technology: high-fidelity simulator; movie; social media Features: role-play using faculty members; ELNEC Core preparation | Scenario: home care adult patient Externally developed: NLN ACE.S; “Evan Mayday’s Good Death” video Audience: senior BSN students; observed and participated as nurse or other role (N unspecified) | Kirkpatrick: level 1 Tool: qualitative analysis of written questionnaire Results: improved communication with patient/family; high satisfaction |
| Kopp and Hanson40 | Topics: admission of patient to oncology unit; patient decisions regarding EOL; conversation about organ and tissue donation Methods: patient/family conversations; question and answer session with EOL expert nurses; debriefing | Technology: high-fidelity simulator Features: role-play by actual nurses and faculty members; lecture; board game (challenges and issues related to EOL) | Scenario: hospitalized adult patient Externally developed: adapted CAE Healthcare Simulated Clinical Experience (SCE) EOL Care scenario; prev. METI Audience: junior BSN students; observed and participated as nurse or other role (N unspecified) | Kirkpatrick: level 1 Tool: 2 questions with a 5-point Likert Scale Results: improved understanding of communication techniques in EOL care |
| Kunkel et al41 | Topics: EOL experiences; discussions surrounded the topics of medication administration, comfort measures, religious practices, organ donation communication between family members and members of the healthcare team Methods: simulation observation; debriefing | Technology: high-fidelity simulator; METI programmed physiologic changes Features: scripted role play by actual nurses and faculty members | Scenario: hospitalized adult oncology patient Externally developed: unclear Audience: 72 junior and senior BSN students, and recent graduate nurses; observed only | Kirkpatrick: level 1 Tool: simulation effectiveness tool (SET) to measures confidence Results: 90.3% of participants indicated increased confidence |
| Ladd et al42 | Topics: transition to hospice care, family distress, final moments of life, “Five Wishes” Methods: patient/family conversations; reflective debriefing | Technology: high-fidelity simulator; video clip Features: role-play by ELNEC trainer and students; semistructured group interview; vignettes; slides; conversational lectures | Scenario: adult oncology patient Externally developed: no Audience: 35 nursing students; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: Semistructured pre–postclass survey To assess influence of student’s past experiences with death on EOL care Results: Students with prior experience were able to articulate EOL care easily |
| Leighton and Dubas43 | Topics: patient death, notifying the family, family bereavement and comforting Methods: patient/family communication; group debriefing; group discussions | Technology: high-fidelity simulator; videos Features: lectures; case Studies; student presentations; role-play; gaming; panel discussion; debates; role play by faculty member | Scenario: acute care adult oncology patient Externally developed: CAE Healthcare Simulated Clinical Experience (SCE) EOL Care scenario; prev. METI Audience: 16 sophomore, junior, senior nursing students in elective course; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: open-ended questions Results: presence of family positively impacted learning experience; fidelity of simulation is seen as valuable and helpful; lack of confidence in providing care |
| Lippe and Becker44 | Topics: family conflict regarding EOL decisions, change in status, withdrawal of care Methods: patient/family/provider conversations; prebriefing; reflective debriefing | Technology: simulator not described; live video streamed to classroom Features: scripted role play by actors, faculty (medicine), students | Scenario: acute care adult patient Externally developed: no Audience: 128 nursing students; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: (1) Perceived Competence in Meeting ELNEC Standards (PC-ELNEC) survey (2) FATCOD applied pre–postsimulation Results: (1) increase in scores on the PC-ELNEC (P < .001); (2) increase in scores on FATCOD (P < .010) |
| Montgomery et al45 | Topics: patient actively dying; forgoing future treatment; spiritual/cultural needs of patient and family; advanced directives Methods: patient/family communication; group debriefing | Technology: high-fidelity simulator Features:role-play by faculty | Scenario: adult oncology patient in home Externally developed: adapted CAE Simulated Clinical Experience (SCE) EOL Care scenario; prev. METI Audience: senior BSN students; observed and participated as nurse or other role (N unspecified) | Kirkpatrick: level 1 Tool: simulation evaluation survey Results: simulation evaluated as effective in physical signs of EOL and advance directives (90% of students); in cultural implications (85%); comfort care (76%) |
| Pastor et al46 | Topics: delivering difficult news to patients in primary care setting Methods: patient/family/provider conversations; debriefing in group setting | Technology: simulation and debriefing were videotaped Features: role-play with actors; scripted simulation conversation; self-directed learning; interdisciplinary teams | Scenario: older adult couple receiving bad news Externally developed: no Audience: 5 graduate nursing (FNP) and 5 masters of social work students; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: Readiness for Interprofessional Learning Scale (RIPLS); Survey of Students’ Perceptions of their Ability to Deliver Difficult News applied pre–postsimulation Results: qualitative only, authors concluded that tool was appropriate for evaluating achievement of simulation learning objectives |
| Pullen et al47 | Topics: family grief support; patient actively dying; patient suffering, interdisciplinary care roles Methods: patient/family communication; interdisciplinary group meetings; reflective debriefing | Technology: high-fidelity simulator; cinema education Features: role-play using faculty; ELNEC case studies; scripted interviews with standardized patients | Scenario: adult hospice home care patient Externally developed: no Audience: RNs and allied disciplines; observed and participated as nurse or other role; 2006-2010 (N unspecified) | Kirkpatrick: level 2 Tool: scaled EOL communication learning items with narrative comments Results: Postsimulation data showed mean 4.56 (1-5 scale) on communication items; comments sorted into themes further corroborated learning |
| Saylor et al48 | Topics: shift to palliative care treatment, patient/family education, discuss treatment options, patient/family goals Methods: patient/family/provider conversations; debriefing using recorded simulation; work within interdisciplinary teams | Technology: audio–visual recording of simulation Features: standardized patient actors | Scenario: young oncology patient in remission Externally developed: no Audience: 104 nursing and medical students, nurse interns, medical residents; observed and participated as nurse or other role | Kirkpatrick: level 2 Tool: General Self-Efficacy Scale (GES) and Jefferson Scale of Attitudes Toward Physician Nurse Collaboration (JSAPNC) applied pre–postsimulation; Evaluators (physician/nurse) used the Team Objective Structured Clinical Examination (TOSCE) tool Results: postsimulation, overall mean GES scores differed significantly (P = .001), JSAPNC scores differed significantly (P = .008), attitudes toward physician-nurse collaboration improved overall Differences in rater’s observations of nurses/students vs. physicians/students using TOSCE suggests meaning of interprofessional collaboration varies by profession |
| Shaw and Abbott10 | Topics: ethical reasoning, shift to palliative care treatment Methods: patient/family conversation; debriefing using audio–visual recording | Technology: high-fidelity simulator; audio–visual recording of simulation Features: role-play using students as clergy, family, nurse, and social worker | Scenario: adult oncology/palliative care patient Externally developed: no Audience: 17 nursing students in elective EOL course; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: Program of Nursing Curriculum Integration Simulation Effectiveness Tool included 10 items measuring perceptions of students that simulation increased critical thinking, knowledge, and confidence Results: “Do not agree” was selected for only 3 of the 170 (10 × 17) total response items |
| Sperlazza and Cangelosi49 | Topics: legal and ethical dimensions of advance directives; family dynamics related to ambivalence, stress, conflict, and grief; transition to palliative care and patient goals Methods: patient/family communication; debriefing | Technology: high-fidelity simulator Features: role-play using students; student observation; 3 separate scenes; framework guided content | Scenario: end-stage adult COPD patient Externally developed: no Audience: 30 first year associate degree nursing students; observed and participated as nurse or other role | Kirkpatrick: level 1 Tool: verbal and written feedback Results: Students indicated appreciation for and being moved by the simulation experience in debriefing sessions. Faculty identified the need to better prepare students for the simulation |
| Venkatasalu et al50 | Topics: engaging in patient conversation during difficult situation Methods: patient conversation during EOL care; debriefing | Technology: high-fidelity simulator; video telecasting Features: mentor/facilitator during simulation | Scenario: adult EOL patient Externally developed: unclear Audience: junior nursing students randomly assigned to seminar-based (n = 139) or simulation-based (n = 49) learning; observed and participated as nurse or other role | Kirkpatrick: level 3 Tool: face-to-face semistructured interviews conducted with students after training and exposure to EOL care situation in actual clinical setting Results: qualitative findings indicated that the simulation-based group members were stronger than the comparison group on emotional and clinical preparedness and converting knowledge into practice |
| Youngblood et al51 | Topics: family grief, death of a child, denial, and conflict; delivering bad news Methods: patient/family communication; simulation completed in interdisciplinary team; debriefing using the model of “Debriefing with Good Judgment” | Technology: high-fidelity simulators (SimMan, SimBaby, and PediaSIM) Features: role-play using actors | Scenario: pediatric critical care patients Externally developed: no Audience: nurses, pediatric medicine fellows, social workers and chaplains; participated as nurse or other role (N unspecified) | Kirkpatrick: level 1 Tool: narrative feedback of participants perceptions of the value of the simulations Results: overwhelmingly positive response to the experience |
Abbreviations: ACE.S, Advancing Care Excellence for Seniors; ABSN, Accelerated Bachelor of Science in Nursing; BSN, Bachelor of Science in Nursing; ELNEC, End-of-Life Nursing Education Consortium; ELNEC-KAT, ELNEC-Knowledge Assessment Tool; FNP, Family Nurse Practitioner; METI, Medical Education Technologies; NLN, National League for Nursing; PC-ELNEC, Perceived Competences in meeting ELNEC standards; SBLE, simulation-based learning experience.
Results
In the 30 articles that met the eligibility criteria, the research team focused on identifying the use of SBLEs to educate nursing students and clinicians (practicing nurses) about palliative care or EOL communication. A word cloud of the review articles was generated from summaries of each article’s synthesis to provide a visual of the themes and strengths that characterized the simulation exercises described (Figure 2). The top themes included family, care, patient, EOL, symptoms, management, grief, conflict, palliative, and support. The following paragraphs summarize information from the articles that help contextualize the communication component of the SBLEs reported in the articles (Table 1).
Figure 2.
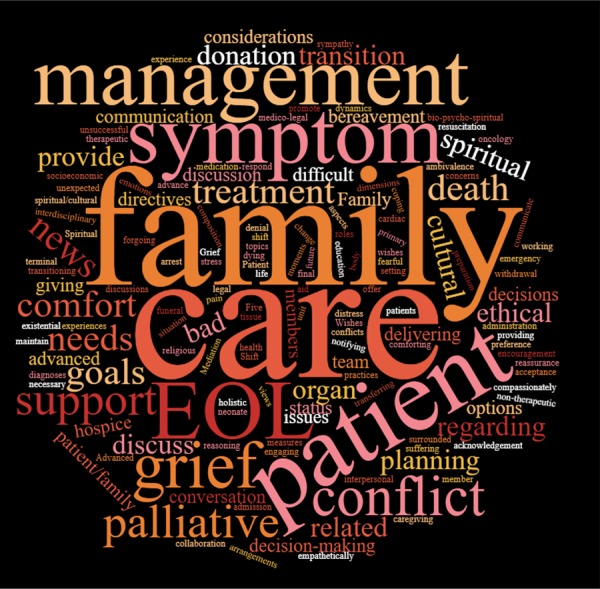
A word cloud generated using summaries of each article included in the review. Font size and boldness of the terms increase with frequency to highlight keywords and themes of the simulation-based learning experiences.
Target Learner Audience
The undergraduate nursing student was a target learner in a majority of the articles (n = 22).10,25,27–36,38–40,42–45,48–50 In the remaining 8 articles, the main target learners were the graduate nurse trainee,46 the practicing nurse,23,24,26,37,51 and both nursing students and practicing nurses together.41,47 Other members of the health team participated (were physically present) in 7 of the SBLEs. These included social workers/students,29,33,37,46,47,51 medical students/residents/physicians,29,33,48,51 chaplains/students,29 and hospice care workers.47
Simulation-Based Learning Experience Communication Focus and Interprofessional Team Members
The specific communication content varied widely across SBLE scenarios, with the majority (n = 18) focused on EOL conversations.10,23,26,27,32–34,38,40–47,50,51 The remaining 12 articles24,25,28–31,35–37,39,48,49 focused on palliative care-related communication. Over half (n = 16) of the scenario conversations involved only nurses, patients, and family members. The remaining 14 included at least one additional member of the interprofessional team (eg, physician, social worker, chaplain, hospice worker). Only half of the 14 involved direct participation by interprofessional members of the team,29,33,37,46–48,51 for the other half these roles were played by actors.10,23–26,30,44
Debriefing
Debriefing was a central element of nearly all (n = 28) simulation exercises. Debriefing methods included videotaped session review, simple question and answer sessions, guided questions, reflective sessions, and the use of published debriefing guides (eg, Debriefing with Good Judgement).52 Nursing faculty typically facilitated the debriefings but actors, registered nurses, and emergency room residents also coled these sessions.
Technology
High-fidelity simulators were the most common technology used in the scenarios (n = 21) or medium-fidelity manikins33 though details were limited. Most authors indicated that their SBLEs were supported by video review, either of the actual simulation experience (n = 9)10,23,28,32,34,38,44,46,48 or review of previously recorded video scenarios (n = 9).24–26,29,35,37,39,42,43 Two simulation experiences were recorded and streamed live to separate classrooms.44,50 Other technology used included online modules,29 audio recordings,31,38 virtual and phone communication,37 social media,39 and manikins with programmable physiologic changes.40,41,43,45,51
Scenario Enactment
The authors reported a variety of “features” used to enact their scenarios. Twenty-eight of the exercises involved role play by actors or the actual participants. Roles played by others included the patient, family member, nurse, physician, social worker, chaplain, and hospice worker. In 8 of the articles, the authors reported using scripts.24,26,27,31,41,44,46,47 Other features of the SBLEs included workshops,29 lectures,24–26,35,37,38,40,43 case studies,24,43 student presentations,35,43 board games/gaming,40,43 panel discussions,43 group tutorial sessions,35,37,38 self-directed learning,46 standardized patient interviews,47 framework-guided content,49 and debates.43
Scenario Sources
The simulation exercise scenarios were most frequently developed by internal faculty and personnel (n = 20). Eight of the 30 scenarios utilized externally developed scenarios and 2 of the articles provided no scenario source information. The externally developed scenarios utilized in these SBLEs included the following: (1) the Memorial Sloan Kettering Cancer Center for EOL care53,54 adapted curriculum,26 (2) the adapted Scheikl and O’Neill55 simulation scenario,28 (3) the National League for Nursing (NLN) Advancing Care Excellence for Seniors (ACE.S)56 module,39 (4) the adapted Simulation Clinical Experience (SCE) EOL care scenarios from CAE Healthcare (previously known as Medical Education Technologies [METI]),40,43,45 (5) “A Lion in the House”57 video,35 and (6) “Evan Mayday’s Good Death”58 video.39
Simulation Frameworks and Curriculum
Some of the authors reported using existing evidence-based frameworks and curricula to guide the development or design of their SBLE. Three27,28,30 authors used the Nursing Education Simulation Framework by Jeffries,59 140 reported use of the Simulation Learning Pyramid,60 and 536,39,42,43,47 utilized aspects of the End-of-Life Nursing Education Consortium (ELNEC) curriculum.61
Patient-Related Characteristics
Most of the scenarios focused on an adult patient (n = 25); 15 in the hospital setting,10,24–26,29,30,33,34,36,40,41,43,44,49,50 7 in a hospice setting,23,27,28,31,37,42,47 and 3 in homecare settings38,39,45 with life-limiting illnesses such as cancer, chronic diseases, and cranial hemorrhage at various stages. One SBLE focused on a hospitalized young adult48 and 3 articles reported using pediatric scenarios, 2 in the hospital setting,32,51 and 1 unspecified.35
Evaluation
As noted earlier, The Kirkpatrick Model21,22 was used to differentiate the level of evaluation assessment completed for the training reported in each of the 30 articles reviewed (see Table 1). In 16 of the articles, a level 1 (REACTION) post-training assessment was conducted and typically focused on the user’s satisfaction with, perceived value of, or perceived learning from the training. Twelve articles were classified as including level 2 (LEARNING) assessments. All 12 reported conducting pre- and postevaluations to assess changes in knowledge level, attitudes, and/or self-confidence with palliative care or EOL patients and their families. A level 3 (BEHAVIOR) was reported in 2 of the articles. There were no level 4 (RESULTS) reported in the 30 articles reviewed.
Authors reported using a variety of instruments to evaluate the SBLEs, but for most, there was no evidence provided about previous testing or psychometrics. There were several authors, however, who reported using existing tools to conduct their evaluations. These tools included the followings: Frommelt Attitudes on Care of the Dying,62 (n = 3),25,27,44 the Perceived Competences in meeting ELNEC standards or ELNEC-Knowledge Assessment Tool63 (n = 3),24,36,44 and the Caring Efficacy Scale64 (n=1).23 In one study,48 the authors used 3 different tools: the General Self-Efficacy Scale,65 the Jefferson Scale of Attitudes Toward Physician/Nurse Collaboration,66 and the Team Objective Structured Clinical Examination Tool.67 While all of the articles included a communication component in the SBLE, these were almost always embedded within a larger scenario that included physical care or monitoring patient status. As a result, the evaluations typically did not specify the component to which the responses referred making it impossible to draw conclusions about the individual components.
Finally, we noted the absence of information that seems critical to assessing the quality and outcomes of the SBLEs in these articles. One is the length of the SBLE. Although the descriptions indicated the SBLEs varied in length, most did not provide sufficient information to assess the actual time involved. The length and depth of the scenario are certain to have an impact. Second, all aspects of the communication component are not clearly specified in these articles, making it difficult to duplicate or compare across SBLEs. Third, the articles contain virtually no information about the potential impact of enacting or only observing the direct nurse communicator role. In most instances, the nurses and nursing students only observed the direct nurse communicator role. We therefore wonder whether trainees who enact the direct nurse communicator role during an SBLE (active learner) achieve a higher level of communication competency than their colleagues who only observe the role.
Discussion
In this systematic review, we examined 30 articles to determine how SBLEs are being used to build the communication skills of nursing students and clinicians with palliative care and EOL patients and families. Though commonalities were reported, the wide variation in the details of these SBLEs and range of evaluation levels and tools make it difficult to draw general conclusions. These findings support what others have found as well.4,68 Below, we discuss our findings and the potential implications of them.
As was noted in the previous section, we observed a number of important differences among the SBLEs. For the scenarios, these included the learning aims, patient characteristics (eg, health issue/s, gender, age), setting simulated (eg, hospital, hospice, homecare), content and length of the scenario, timing of the communication (eg, initial diagnosis, EOL), individuals involved (eg, parents, spouses, care team members), and enactment features (eg, manikin, actors, standardized patients, scripts, roles played by the students/clinicians). The debriefing process also varied widely even though the authors reported using some form of debriefing in 28 of the SBLEs. Though the differences across scenarios signify the diversity of SBLEs, the inability to compare the impact of these on trainee outcomes is problematic.
The evaluations reported in the articles are problematic for several reasons. For a number of the SBLEs, the objectives and desired competencies were not clearly articulated. In the absence of clear objectives and competencies, it is not possible to ascertain whether they are achieved. In addition, the tools used in the evaluations were most often internally developed and not previously validated, as is typically done to evaluate SBLEs in undergraduate courses. The majority of these evaluations were posttest measures (n = 16) capturing the perceptions or reactions of the students and nurses to the exercises (Kirkpatrick level 1).21,22 Since the main purpose of palliative and EOL communication SBLEs is to prepare nursing students and practicing nurses to enhance their communication skills, a level 2 evaluation at minimum is needed to determine actual knowledge gained. While level 2 evaluation need not involve pre- and posttest, this is most desirable. Levels 3 and 4 assessments provide even greater understanding of the impact of SBLEs since they assess translation of behavior into practice (level 3) and achievement of desired patient outcomes as a result of nurse behaviors (level 4). Our results, however, concur with those of others4,68 who found that there is little attention on assessing important relationships between SBLEs and clinician behaviors in the clinical setting (level 3) and desired patient outcomes (level 4), the ultimate end goal of this training.
Of the 2 level 3 evaluations reported in this review, one was particularly creative in assessing the relationship between an SBLE and the use of the knowledge in practice. Venkatasalu and colleagues50 evaluated the impact of the SBLE on behaviors in practice through interviews with students who had taken care of EOL patients in the clinical setting, following the completion of either a seminar-based session or SBLE. The authors found that those in the SBLE group were stronger in emotional and clinical preparedness and in converting knowledge into practice compared to those who completed the seminar training.
On another front, we were surprised to find that only 14 SBLEs included other members of the interprofessional team. Seven of the 14 involved actual participation by a member of another discipline, while in the remaining 7, the interprofessional roles were acted out by nursing students, practicing nurses, faculty, or other actors. This is concerning evidence that nurses and other interprofessional team members are not consistently trained together. Since palliative and EOL care are typically provided by interprofessional teams, training nurses and other members of the team together are particularly important to prepare teams for managing the real-time situations. Further interprofessional communication is a core competency endorsed by numerous nursing and interprofessional standards bodies including, American Association of Colleges of Nursing69–71 and the Interprofessional Education Collaborative.72 Communication with the patient and family about their palliative and EOL care nearly always has a direct or indirect impact on the overall quality of care the team provides. It is crucial therefore to include appropriate disciplines in the training plan when developing and implementing communication scenarios for palliative and EOL care.
In summary, our findings suggest that SBLEs are being used to support the development of communication competencies for nursing students and clinicians when providing palliative and EOL care, but the true impact is elusive. Given the costs involved in the training, it is crucial to not only understand the impact of SBLEs but also to be able to identify best practices and the minimum content needed to achieve desired trainee outcomes. Since our review captured both the research studies and nonstudies published in this area, we are able to see that the state of the science is very limited. Furthermore, the lack of evidence and the absence of sufficient opportunities to develop the desired communication competencies under the “real-time” conditions appear to be driving the development and use of SBLEs that are not fully validated. Though we strongly support further research in this area, effective alternative strategies for implementing SBLEs that build important palliative and EOL communication competencies in nursing students and clinicians are needed now. In conclusion, we offer the following recommendations to enhance the quality and validity of SBLEs designed to build communication competencies in palliative and EOL care. Ultimately, this strategy will augment research by simultaneously generating practice-based evidence that can also validate and be used to improve SBLEs.
Utilize existing standards to structure SBLEs: In this review, 9 articles reported using an existing framework or curriculum in the design of their SBLEs. We support the NLN’s endorsement of the use of standards in simulation projects.73 As we observed, these standards provide a context for systematically developing and integrating an SBLE into a curriculum. Of note is the ELNEC framework that contains specific content pertinent to palliative care and EOL training to the entire interprofessional team. In addition, we also endorse the use of the International Nursing Association for Clinical Simulation and Learning standards.16 These standards were first published in 2011. While none of the articles reviewed referenced these standards, they have gained solid recognition as the most comprehensive set of guidelines for simulation in the field. They comprise 7 evidence-based best practice guidelines that inform the design,16 facilitation,74 evaluation,75 integrity,76 collaboration of interprofessional team members,77 debriefing practices,78 and objective and outcomes.79 The Sim-IPE (Simulation Enhanced Interprofessional Education) provides guidance for integrating interprofessional team members into SBLEs that support patient and family goals and ultimately high-quality patient outcomes.77
Clearly specify the goals and objectives to be achieved with the SBLE. The foundation for evaluating the impact of any SBLE starts with identifying the objectives and competencies you wish to achieve through this mechanism. In the absence of these objectives, it is not possible to measure and demonstrate the impact of the SBLEs and competencies to be achieved by the learners. In this review, it was difficult to ascertain the specific communication competencies the SBLEs were expected to achieve. As we observed, it certainly makes sense to integrate communication with patients and family into learning opportunities that include other aspects of care that naturally occur simultaneously (eg, physical). In such instances, however, it is crucial to clearly articulate the specific communication objectives to be accomplished by the SBLE (eg, learners will demonstrate the use of effective communication skills while assisting a hospitalized adult patient receiving palliative care to create an advanced directive under simulated conditions). Clear articulation of a communication objective provides the foundation for determining the degree to which the objective has been met.
Utilize externally validated scenarios where appropriate to meet specified objectives. Though the use of simulation in education is still relatively young, it is growing rapidly. As a result, there are numerous sources of validated cases or scenarios that can be integrated into SBLEs, avoiding the need to develop a scenario from scratch. Eight of the articles reviewed included externally developed patient scenarios in their SBLEs. The NLN was one of the scenario sources utilized and provides access to a large library of scenarios that have been previously validated.56 We recommend consulting current sources of validated scenarios before building a scenario from scratch. It is critical, however, to ensure that any scenario selected from a bank or built from scratch provides the content needed to meet the clearly articulated objectives of the SBLE. When building communication competencies in palliative and EOL care, the scenarios must include content that allows assessment of relevant objectives.
Apply feasible, rigorous, and appropriate evaluation methods: Given the importance of health team communication to outcomes of patients receiving palliative and EOL care, it is critical to ensure our teaching strategies build the requisite competencies. Since the nurse members of the health-care team have the most frequent and direct exposure to such patients, it is particularly crucial for nurses to possess strong communication skills with patients, families, and teams. While we have assumed that the impact of SBLEs on communication competencies in palliative and EOL care is not being validated, this may be because authors did not report such information. Regardless, it is essential to understand the impact of communication training on expected outcomes when using SBLEs in order to make decisions about their ongoing use and value in training. Thus, we want to underscore the importance of utilizing strong evaluation methods and tools that can assess both the achievement of the clearly articulated training objectives and the level of learning achieved (eg, as articulated by the Kirkpatrick model). By so doing, the knowledge gained from using SBLEs in training programs (focused on building communication competencies in palliative and EOL care) can augment the research being done and speed our capability to identify and disseminate best practices.
Acknowledgment
The authors would like to thank Debra McDonald for her expert editorial assistance.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Madison B. Smith, RN, BSN,  http://orcid.org/0000-0003-1061-018X
http://orcid.org/0000-0003-1061-018X
Margaret Ansell  http://orcid.org/0000-0003-1653-3816
http://orcid.org/0000-0003-1653-3816
References
- 1. American Nurses Association. Call for Action: Nurses Lead and Transform Palliative Care. Silver Spring, MD: 2017. Available at: http://nursingworld.org/callforaction-nursesleadtransformpalliativecare. Accessed February 19, 2018. [Google Scholar]
- 2. Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences near the End of Life. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 3. Epstein RM, Street JR. Patient-centered communication in cancer care: promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute; 2007. [Google Scholar]
- 4. Kirkpatrick AJ, Cantrell MA, Smeltzer SC. Palliative care simulations in undergraduate nursing education: an integrative review. Clin Sim Nurs. 2017;13(9):414–431. [Google Scholar]
- 5. Dahlin C, National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines For Quality Palliative Care: Pittsburgh, Pennsylvania: National Consensus Project; 2013. [Google Scholar]
- 6. Anderson NE, Kent B, Owens RG. Experiencing patient death in clinical practice: nurses’ recollections of their earliest memorable patient death. Intl J Nurs Studies. 2015;52(3):695–704. [DOI] [PubMed] [Google Scholar]
- 7. Kent B, Anderson NE, Owens RG. Nurses’ early experiences with patient death: the results of an on-line survey of registered nurses in New Zealand. Intl J Nurs Stud. 2012;49(10):1255–1265. [DOI] [PubMed] [Google Scholar]
- 8. Dunn KS, Otten C, Stephens E. Nursing experience and the care of dying patients. Oncol Nurs Forum. 2005;32(1):97–104. [DOI] [PubMed] [Google Scholar]
- 9. Glover TL, Horgas AL, Castleman J, Turpening P, Kittelson S. An experiential learning approach to primary palliative care nursing education: the comfort shawl project. JHPN. 2017;19(6):534–538. [Google Scholar]
- 10. Shaw PA, Abbott MA. High-fidelity simulation: teaching end-of-life care. Nurse Educ Today. 2017;49:8–11. [DOI] [PubMed] [Google Scholar]
- 11. O’Shea MF. Staff nurses’ perceptions regarding palliative care for hospitalized older adults. Am J Nurs. 2014;114(11):26–34; quiz 35, 44. [DOI] [PubMed] [Google Scholar]
- 12. White KR, Coyne PJ. Nurses’ perceptions of educational gaps in delivering end-of-life care. Oncol Nurs Forum. 2011;38(6):711–717. [DOI] [PubMed] [Google Scholar]
- 13. Anderson WG, Puntillo K, Boyle D, et al. ICU bedside nurses’ involvement in palliative care communication: a multicenter survey. J Pain Symp Manag. 2016;51(3):589–596.e582. [DOI] [PubMed] [Google Scholar]
- 14. Cantrell MA, Franklin A, Leighton K, Carlson A. The evidence in simulation-based learning experiences in nursing education and practice: an umbrella review. Clin Simul Nurs. 2017;13:634–667. [Google Scholar]
- 15. Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(suppl 1):i2–i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. INACSL. INACSL standards of best practice: simulationsm design. Clin Simul Nurs. 2016;12:S5–S12. [Google Scholar]
- 17. Lopreiato J, Downing D, Gammon W, et al. Healthcare Simulation Dictionary. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [Google Scholar]
- 18. INACSL. INASCL standards of best practice: simulationsm glossary. Clin Simul Nurs. 2016;12:S39–S47. [Google Scholar]
- 19. Smith MB, Macieira T, Bumbach MD, et al. The use of simulation to teach nursing students and clinicians palliative care and end-of-life communication: a systematic review. 2017; PROSPERO 2017 CRD42017058046 http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017058046. Accessed February 19, 2018. [DOI] [PMC free article] [PubMed]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, w264. [DOI] [PubMed] [Google Scholar]
- 21. Kirkpatrick D. Techniques for evaluating training programs. Train Dev J. 1979;33:78. [Google Scholar]
- 22. Kirkpatrick Partners. The Kirkpatrick Model. 2017. https://www.kirkpatrickpartners.com/Our-Philosophy/The-Kirkpatrick-Model. Updated February 19, 2018. Accessed November 14, 2017.
- 23. Betcher DK. Elephant in the room project: improving caring efficacy through effective and compassionate communication with palliative care patients. Medsurg Nurs. 2010;19(2):101–105. [PubMed] [Google Scholar]
- 24. Bodine JL, Miller S. A comparison of lecture versus lecture plus simulation educational approaches for the end-of-life nursing education consortium course. J Hosp Palliat Nurs. 2017;19(1):34–40. [Google Scholar]
- 25. Carman MJ, Sloane R, Molloy M, Flint E, Phillips B. Implementation of a learning bundle to promote end-of-life education for prelicensure nursing students. J Hosp Palliat Nurs. 2016;18(4):356–363. [Google Scholar]
- 26. Coyle N, Manna R, Shen MJ, et al. Discussing death, dying, and end-of-life goals of care: a communication skills training module for oncology nurses. Clin J Onc Nurs. 2015;19(6):697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dame L, Hoebeke R. Effects of a simulation exercise on nursing students’ end-of-life care attitudes. J Nurs Ed. 2016;55(12):701–705. [DOI] [PubMed] [Google Scholar]
- 28. Eaton MK, Floyd K, Brooks S. Student perceptions of simulation’s influence on home health and hospice practicum learning. Clin Sim Nurs. 2012;8(6):e239–e247. [Google Scholar]
- 29. Ellman MS, Schulman-Green D, Blatt L, et al. Using online learning and interactive simulation to teach spiritual and cultural aspects of palliative care to interprofessional students. J Palliat Med. 2012;15(11):1240–1247. [DOI] [PubMed] [Google Scholar]
- 30. Fabro K, Schaffer M, Scharton J. The development, implementation, and evaluation of an end-of-life simulation experience for baccalaureate nursing students. Nurs Edu Persp. 2014;35(1):19–25. [DOI] [PubMed] [Google Scholar]
- 31. Fluharty L, Hayes AS, Milgrom L, et al. A multisite, multi–academic track evaluation of end-of-life simulation for nursing education. Clin Sim Nurs. 2012;8(4):e135–e143. [Google Scholar]
- 32. Forster E, Donovan H. Enhancing bereavement support skills using simulated neonatal resuscitation. Intl J Palliat Nurs. 2016;22(10):500–507. [DOI] [PubMed] [Google Scholar]
- 33. Gillan PC, Arora S, Sanderson H, Turner L. Palliative Care Simulation: Nurturing Interprofessional Collegiality. vol 2 USA: Pacific University; 2013:9. [Google Scholar]
- 34. Gillan PC, Parmenter G, van der Riet PJ, Jeong S. The experience of end of life care simulation at a rural Australian university. Nurse Educ Today. 2013;33(11):1435–1439. [DOI] [PubMed] [Google Scholar]
- 35. Gotwals BA, Scholtz S. Video-enhanced simulation in pediatric end-of-life care. Nurs Educ Perspect. 2016;37(6):360–362. [Google Scholar]
- 36. Grossman S. Development of the palliative care of dying critically ill patients algorithm: implications for critical care nurses. J Hosp Palliat Nurs. 2013;15(6):355–359. [Google Scholar]
- 37. Hamilton G, Ortega R, Hochstetler V, Pierson K, Lin P, Lowes S. Teaching communication skills to hospice teams: comparing the effectiveness of a communication skills laboratory with in-person, second life, and phone role-playing. Am J Hosp Palliat Med. 2014;31(6):611–618. [DOI] [PubMed] [Google Scholar]
- 38. Hjelmfors L, Strömberg A, Karlsson K, Olsson L, Jaarsma T. Simulation to teach nursing students about end-of-life care. J Hosp Palliat Nurs. 2016;18(6):512–518. [Google Scholar]
- 39. Kopka JA, Aschenbrenner AP, Reynolds MB. Helping students process a simulated death experience: integration of an NLN ACE.S evolving case study and the ELNEC curriculum. Nurs Educ Perspect. 2016;37(3):180–182. [PubMed] [Google Scholar]
- 40. Kopp W, Hanson MA. High-fidelity and gaming simulations enhance nursing education in end-of-life care. Clin Sim Nurs. 2012;8(3):e97–e102. [Google Scholar]
- 41. Kunkel C, Kopp W, Hanson M. A matter of life and death: end-of-life simulation to develop confidence in nursing students. Nurs Educ Perspect. 2016;37(5):285–286. [DOI] [PubMed] [Google Scholar]
- 42. Ladd C, Grimley K, Hickman C, Touhy TA. Teaching end-of-life nursing using simulation. J Hosp Palliat Nurs. 2013;15(1):41–51. [Google Scholar]
- 43. Leighton K, Dubas J. Simulated death: an innovative approach to teaching end-of-life care. Clin Sim Nurs. 2009;5(6):e223–e230. [Google Scholar]
- 44. Lippe MP, Becker H. Improving attitudes and perceived competence in caring for dying patients: an end-of-life simulation. Nurs Educ Perspect. 2015;36(6):372–378. [DOI] [PubMed] [Google Scholar]
- 45. Montgomery M, Cheshire M, Johnson P, Beasley A. Incorporating end-of-life content into the community health nursing curriculum using high-fidelity simulation. J Hosp Palliat Nurs. 2016;18(1):60–65. [Google Scholar]
- 46. Pastor DK, Cunningham RP, White PH, Kolomer S. We have to talk: results of an interprofessional clinical simulation for delivering bad health news in palliative care. Clin Sim Nurse. 2016;12(8):320–327. [Google Scholar]
- 47. Pullen RL, McKelvy K, Reyher L, et al. An end-of-life care interdisciplinary team clinical simulation model. Nurse Educ. 2012;37(2):75–79. [DOI] [PubMed] [Google Scholar]
- 48. Saylor J, Vernoony S, Selekman J, Cowperthwait A. Interprofessional education using a palliative care simulation. Nurse Educ. 2016;41(3):125–129. [DOI] [PubMed] [Google Scholar]
- 49. Sperlazza E, Cangelosi PR. The power of pretend: using simulation to teach end-of-life care. Nurse Educ. 2009;34(6):276–280. [DOI] [PubMed] [Google Scholar]
- 50. Venkatasalu MR, Kelleher M, Shao CH. Reported clinical outcomes of high-fidelity simulation versus classroom-based end-of-life care education. Int J Palliat Nurs. 2015;21(4):179–186. [DOI] [PubMed] [Google Scholar]
- 51. Youngblood AQ, Zinkan JL, Tofil NM, White ML. Academic education multidisciplinary simulation in pediatric critical care: the death of a child. Crit Care Nurse. 2012;32(3):55–61. [DOI] [PubMed] [Google Scholar]
- 52. Rudolph JW, Simon R, Dufresne RL, Raemer DB. There’s no such thing as “nonjudgmental” debriefing: a theory and method for debriefing with good judgement. Simul Healthc. 2006;1(1):49–55. [DOI] [PubMed] [Google Scholar]
- 53. Bialer PA, Kissane D, Brown R, Levin T, Bylund C. Responding to patient anger: development and evaluation of an oncology communication skills training module. Palliat Support Care. 2011;9(4):359–365. [DOI] [PubMed] [Google Scholar]
- 54. Brown R, Bylund CL, Eddington J, Gueguen JA, Kissane DW. Discussing prognosis in an oncology setting: initial evaluation of a communication skills training module. Psychooncology. 2010;19(4):408–414. [DOI] [PubMed] [Google Scholar]
- 55. Scheikl M, O’Neill C. Clinical Simulation: A Unique Platform for End-Of-Life Education. Harrisonburg, VA: Authors, unpublished; 2009.] [Google Scholar]
- 56. Cato M. Julia Morales, Lucy Grey. ACE.S Unfolding Cases. 2012; http://www.nln.org/professional-development-programs/teaching-resources/aging/unfolding-cases/julia-morales-and-lucy-grey. Accessed February 19, 2018.
- 57. Bognar S, Reichert J. A Lion in the House. 2006. http://www.pbs.org/independentlens/lioninthehouse/index.htm. Accessed February 19, 2018.
- 58. Strodtman L, Giacomazza M. Evan Mayday’s good death. 2006. https://www.med.umich.edu/NURSING/EndOfLife/mayday.htm. Accessed February 19, 2018.
- 59. Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educat Perspect. 2005;26(2):96–103. [PubMed] [Google Scholar]
- 60. Doerr H, Murray WB. How to build a successful simulation strategy: the simulation learning pyramid In: Murray R, ed. Clin Sim: Oper, Engineer, Manage. New York, NY: Elsevier; 2008:771–784. [Google Scholar]
- 61. AACN. End-of-Life Nursing Education Consortium (ELNEC) fact sheet. End-of-Life Nursing Education Consortium: Advancing Palliative Care. Harrisonburg, VA: Unpublished clinical simulation scenario; 2017. http://www.aacnnursing.org/Portals/42/ELNEC/PDF/FactSheet.pdf. Accessed February 19, 2018. [Google Scholar]
- 62. Frommelt KH. The effects of death education on nurses’ attitudes toward caring for terminally ill persons and their families. Am J Hosp Palliat Care. 1991;8(5):37–43. [DOI] [PubMed] [Google Scholar]
- 63. Lange JW, Shea J, Grossman SC, Wallace M, Ferrell BR. Validation of the end-of-life nursing education consortium knowledge assessment test: an abbreviated version. J Hosp Palliat Nurs. 2009;11(5):284–290. [Google Scholar]
- 64. Coates CJ. The caring efficacy scale: nurses’ self-reports of caring in practice settings. Adv Pract Nurs Q. 1997;3(1):53–59. [PubMed] [Google Scholar]
- 65. Chen G, Gully SM, Eden D. Validation of a new general self-efficacy scale. Org Res Methods. 2001;4(1):62–83. [Google Scholar]
- 66. Hojat M, Herman MW. Developing an instrument to measure attitudes toward nurses: preliminary psychometric findings. Psych Reports. 1985;56(2):571–579. [DOI] [PubMed] [Google Scholar]
- 67. Singleton A, Smith F, Harris T, Ross-Harper R, Hilton S. An evaluation of the team objective structured clinical examination. Med Educ. 1999;33(1):34–41. [DOI] [PubMed] [Google Scholar]
- 68. Brighton LJ, Koffman J, Hawkins A, et al. A systematic review of end-of-life care communication skills training for generalist palliative care providers: research quality and reporting guidance. J Pain Symp Manag. 2017;54(3):417–425. [DOI] [PubMed] [Google Scholar]
- 69. American Association of Colleges of Nursing. The essentials of baccalaureate education for professional nursing practice. http://www.aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf. 2008. Updated February 19, 2018. Accessed February 2, 2018. [DOI] [PubMed]
- 70. American Association of Colleges of Nursing. The essentials of master’s education in nursing. http://www.aacnnursing.org/Portals/42/Publications/MastersEssentials11.pdf. 2011. Updated February 19, 2018. Accessed February 2, 2018.
- 71. American Association of Colleges of Nursing. The essentials of doctoral education for advanced nursing practice. http://www.aacnnursing.org/Portals/42/Publications/DNPEssentials.pdf. 2006. Updated February 19, 2018. Accessed February 2, 2018.
- 72. Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011. https://nexusipe-resource-exchange.s3.amazonaws.com/IPEC_CoreCompetencies_2011.pdf. Updated February 19, 2018. Accessed January 20, 2018. [Google Scholar]
- 73. Tagliareni E, Forneris S. Curriculum and Simulation: Are they related? 2016; http://www.nln.org/docs/default-source/professional-development-programs/curriculum-and-simulation-(pdf).pdf?sfvrsn=0. Updated February 19, 2018. Accessed November 15, 2016.
- 74. INACSL. INACSL standards of best practice: simulationsm facilitation. Clin Sim Nurs. 2016;12:S16–S20. [Google Scholar]
- 75. INACSL. INACSL standards of best practice: simulationsm participant evaluation. Clin Sim Nurs. 2016;12:S26–S29. [Google Scholar]
- 76. INACSL. INACSL standards of best practice: simulationsm professional integrity. Clin Sim Nurs. 2016;12:S30–S33. [Google Scholar]
- 77. INACSL. INACSL standards of best practice: simulationsm simulation-enhanced interprofessional education (sim-ipe). Clin Sim Nurs. 2016;12:S34–S38. [Google Scholar]
- 78. INACSL. INACSL standards of best practice: simulationsm debriefing. Clin Sim Nurs. 2016;12:S21–S25. [Google Scholar]
- 79. INACSL. INACSL standards of best practice: simulationsm outcomes and objectives. Clin Sim Nurs. 2016;12:S13–S15. [Google Scholar]