Highlights
-
•
ACL reconstruction is a common and safe procedure; however, complications of VTE can occur.
-
•
An adult man with no risk factors developed PE after arthroscopic ACL reconstruction.
-
•
Clinical pulmonary embolism was confirmed one-week post-surgery radiologically.
-
•
No guidelines are available on prophylactic anticoagulation for arthroscopic ACL reconstruction.
-
•
This report will increase the awareness of serious complications after ACL reconstruction.
Abbreviations: ACL, anterior cruciate ligament; VTE, venous thromboembolism; DVT, deep vein thrombosis; PE, pulmonary embolism; CT, computed tomography
Keywords: Pulmonary embolism, Deep venous thrombosis, Knee arthroscopy, Anterior cruciate ligament, Complications, Case report
Abstract
Introduction
Venous thromboembolism is a serious complication in orthopedic surgery. It is very common in major surgery, such as total hip arthroplasty. However, few reports have described the incidence of pulmonary embolism and its associated risk factors following less invasive surgery, such as arthroscopic knee surgery.
Presentation of case
We describe a rare presentation of a young man with bilateral pulmonary embolism of the main pulmonary arteries following arthroscopic anterior cruciate ligament reconstruction.
Discussion
The present patient is different from other similar cases in that he was an active healthy man without any risk factors for the development of thrombosis. Despite this, he experienced a bilateral pulmonary embolism one week after knee arthroscopy.
Conclusion
Although anterior cruciate ligament reconstruction is a common and safe procedure performed on a daily basis, unexpected complications may occur. One of these is venous thromboembolism which may be fatal.
1. Introduction
Anterior cruciate ligament (ACL) reconstruction is one of the commonest orthopedic surgical procedures performed, ranking as the sixth commonest orthopedic operation. It is usually performed arthrsoscopically [[1], [2], [3]], commonly as a “day case” surgery. Moreover, it is considered a safe procedure with low complication rates.
The incidence of venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), is very low in healthy adults, but is still a significant complication which can cause serious morbidity and has the potential to be fatal. The majority of existing data regarding the incidence of VTE after arthroscopic surgeries of the lower extremity relate to the knee, with no reports of cases of VTE events associated with ankle or hip arthroscopy [[2], [3], [4], [5]].
The risk of VTE is lower in arthroscopic ACL reconstruction than that in knee arthroplasties, where the incidence can reach 70% if no prophylaxis is given. The possibility of VTE events may actually be increased in arthroscopic ACL reconstruction as compared to routine, uncomplicated arthroscopic procedures such as meniscectomy, which are considered less traumatic with no osseous drilling required [2,3,[5], [6], [7], [8]]. In a study of about 14,000 ACL reconstructions, Jameson et al. showed a symptomatic 90-day PE rate of 0.18% [3]. In addition, most studies and review articles show the same incidence of symptomatic PE in population based that ranges from 0.02% to 0.2%, with very rare reports of bilateral symptomatic PE occurring after ACL reconstruction in healthy adult patients [2,3,7,8].
Here we present a rare case of an active adult man who underwent an arthroscopic ACL reconstruction and developed bilateral pulmonary embolism thereafter. The current case report was written according to the recently published SCARE criteria [9].
2. Presentation of case
A 29-year-old man presented with left knee pain and instability after a history of a sport-related twisting injury. Physical examination showed a mild effusion with positive Lachman and anterior drawer test. He was a social smoker and was not known to have any chronic diseases. His body mass index was 22. Magnetic resonance imaging confirmed an ACL tear with a longitudinal tear of the lateral meniscus.
Two months later, under general anesthesia, he underwent arthroscopic ACL reconstruction using ipsilateral hamstring autograft, as well as partial meniscectomy of the lateral meniscus. A tourniquet was used under pressure of 300 mmHg for 50 min and total operation time was 90 min. Blood loss was minimal and no transfusion was needed. The patient tolerated the procedure well and was transferred to the recovery room in a stable condition. He did not receive any special mechanical or pharmacological thromboembolic prophylaxis. His exercise protocol for the first postoperative week was weight bearing as tolerated, range of motion exercises, and ambulation with a knee immobilizer.
One week after the operation, the patient presented to the emergency department with a history of left chest pain and shortness of breath for one day, which was aggravated by inspiration. A few hours later, he developed hemoptysis with no other significant symptoms. His vital signs were as follows: Temperature 37.5 °C, heart rate 87 beats per minute, respiratory rate 23 breaths per minute, blood pressure 114/78 mmHg and oxygen saturation (SaO2) 96%. Physical examination was unremarkable with no signs of DVT. Laboratory tests showed a normal complete blood count, protein C, protein S levels, and no elevation of cardiac markers with normal electrocardiography findings. Computed tomography (CT) angiography showed bilateral pulmonary embolism with evidence of left lower lobe pulmonary infarction (Fig. 1). Doppler ultrasound of the legs showed normal blood flow, with no evidence of DVT or obstruction.
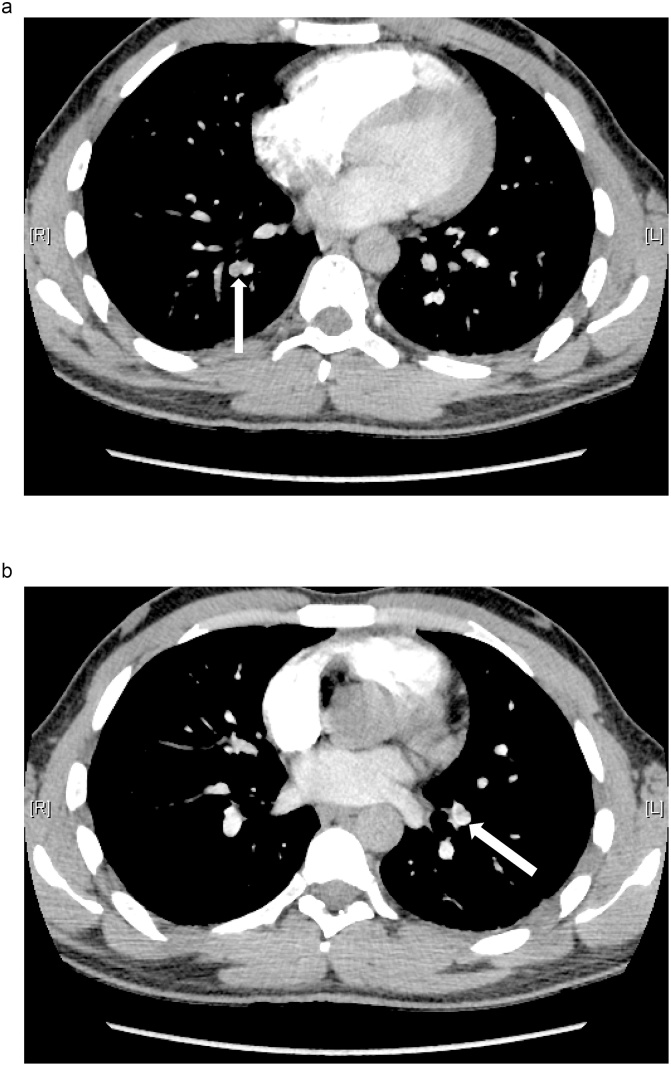
Fig. 1.
Axial (A) right and (B) left computed tomography scans reveal a pulmonary embolism.
Following the diagnosis of bilateral PE, the patient was admitted to the ward and started on low molecular weight heparin. In the next three days, he remained hemodynamically stable and showed improvement of his previous symptoms. He was discharged home on treatment with rivaroxaban for three months, followed by lifelong aspirin at the suggestion of the hematologist; he was advised to continue his physical therapy protocol as an outpatient.
The patient was followed up frequently in our clinic in the next twelve months postoperatively. He was walking, doing his physiotherapy exercises with no complaints, showed good performance in terms of knee function and had no clinical signs and symptoms of PE.
3. Discussion
Arthroscopic orthopedic surgery has been perceived as low risk relative to other orthopedic surgeries, such as total joint replacement and trauma-related procedures. Although complication rates for arthroscopy are low, complications involving VTE, including DVT and PE, are the most potentially life-threatening and should be taken seriously.
In recent reports, the incidence of post-arthroscopy DVT has ranged from 3.5 to 17.9% in the absence of thromboprophylaxis, and from 0.9 to 11.9% in patients who received thromboprophylaxis with low molecular weight heparin.
ACL surgery is associated with a moderate risk of VTE because of the complexity of the procedure, which entails tourniquet use and a relatively long surgery time.
Marlovits et al. reported a statistically significant reduction (P .001) in DVT incidence with post-discharge thromboprophylaxis with enoxaparin for 20 days in patients undergoing ACL reconstruction compared with those who were limited to in-hospital thromboprophylaxis [10]. On the other hand, the 9th edition of American College of Chest Physicians guidelines [11] recommends that no thromboprophylaxis other than early mobilization is necessary for knee arthroscopy unless patients have thromboembolic risk factors.
Previous studies on PE after knee arthroscopy have been either case reports or cohort studies with few cases. A study conducted by Hetsroni et al. in 2011 where they reviewed 418,323 arthroscopic procedures, found the incidence of symptomatic PE to be 0.028% [12]. Although fatality due to PE is relatively uncommon, death from PE has been reported in one case of an athletic young woman who had two risk factors of PE [13]. Therefore, prior to surgery, patients should be informed of the risk of VTE, including fatal PE. Hetsroni et al. reported a higher risk of developing PE in patients over the age of 40 years, with an operative time longer than 90 min, female sex, and a history of cancer [12]. Moreover, Delis et al. [14] reported that only a previous history of VTE with two or more general risk factors for a hypercoagulability state is considered a statistically significant risk factor for VTE after knee arthroscopy.
We believe the present patient was unique compared to the other rare, similar cases that have been reported because he was an active healthy man without any risk factors for developing thrombosis, and was, moreover, following his physiotherapy protocol and performing the exercises. Despite this, he developed a bilateral PE one week after knee arthroscopy.
After reviewing the literature, we found that there is no informative evidence that gives clear guidelines regarding the indications for use of prophylactic anticoagulation following arthroscopic ACL reconstruction. Considering our case as well as the other case report that ended in fatal PE after arthroscopic ACL reconstruction, we believe that more studies should be conducted to clarify risk factors for developing VTE, and indications for administering thromboprophylaxis following knee arthroscopy, as complications such as VTE can occur, even if rarely.
4. Conclusion
Although ACL reconstruction is a common and safe procedure performed on a daily basis, unexpected complications may occur. One of these is venous thromboembolism, which may be fatal sometimes. Thus, clear guidelines are needed regarding VTE thromboprophylaxis following arthroscopic ACL reconstruction in patients with a low risk for developing VTE.
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
No specific grant from funding agencies in the public, commercial, or not-for-profit sectors was received for this work.
**This version had been read by all of the authors who also bear responsibility for it. The material presented is original and all of the authors agreed upon their inclusion. This manuscript has not been published by or submitted to another journal.
Ethical approval
We have reported a single case and ethical approval have been taken from our institution with valid reference number and without any conditions.
RN: 18-246-11.
IRB: H-01-R-069.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review upon request to the editor-in-chief of this journal.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
-Saeed Koaban, Orthopedic surgeon, wrote the manuscript and reviewed the final version of the manuscript.
-Raheef Alatassi, Orthopedic surgeon, performed the literature review and data collection, designed the manuscript, and contributed to writing the manuscript.
-Bandar Ahmed, Orthopedic surgeon, contributed to writing the manuscript.
-Nawaf Alogayyel, medical student, contributed to writing the manuscript.
Registration of research studies
We have reported a single case with no requirement for registry. This manuscript does not describe a clinical study.
Guarantor
Raheef Alatassi.
Contributor Information
Saeed Koaban, Email: mmhh696@gmail.com, skoaban@sfh.med.sa.
Raheef Alatassi, Email: raheef332@hotmail.com, ralatassi@sfh.med.sa.
Bandar Ahmed, Email: dr.bandar@yahoo.com.
Nawaf Alogayyel, Email: W.6F@hotmail.com.
References
- 1.Nordenvall R., Bahmanyar S., Adami J., Stenros C., Wredmark T., Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am. J. Sports Med. 2012;40(8):1808–1813. doi: 10.1177/0363546512449306. [DOI] [PubMed] [Google Scholar]
- 2.Janssen R.P.A., Reijman M., Janssen D.M., van Mourik J.B.A. Arterial complications, venous thromboembolism and deep venous thrombosis prophylaxis after anterior cruciate ligament reconstruction: a systematic review. World J. Orthop. 2016;7(9):604–617. doi: 10.5312/wjo.v7.i9.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jameson S.S., Dowen D., James P., Serrano-Pedraza I., Reed M.R., Deehan D. Complications following anterior cruciate ligament reconstruction in the English NHS. Knee. 2012;19(1):14–19. doi: 10.1016/j.knee.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Bushnell B.D., Anz A.W., Bert J.M. Venous thromboembolism in lower extremity arthroscopy. Asrthroscopy. 2008;24(5):604–611. doi: 10.1016/j.arthro.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Schippinger G., Wirnsberger G.H., Obernosterer A., Babinski K. Thromboembolic complications after arthroscopic knee surgery: incidence and risk factors in 101 patients. Acta Orthop. Scand. 1998;69(2):144–146. doi: 10.3109/17453679809117615. [DOI] [PubMed] [Google Scholar]
- 6.Takigami J., Hashimoto Y., Yamasaki S., Terai S., Nakamura H. A case of asymptomatic bilateral massive pulmonary embolism after arthroscopic multiple knee ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017;25(1):260–262. doi: 10.1007/s00167-014-3466-7. [DOI] [PubMed] [Google Scholar]
- 7.Gaskill T., Pullen M., Bryant B., Sicignano N., Evans A.M., DeMaio M. The prevalence of symptomatic deep venous thrombosis and pulmonary embolism after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2015;43(11):2714–2719. doi: 10.1177/0363546515601970. [DOI] [PubMed] [Google Scholar]
- 8.Struijk-Mulder M.C., Ettema H.B., Verheyen C.C., Büller H.R. Deep vein thrombosis after arthroscopic anterior cruciate ligament reconstruction: a prospective cohort study of 100 patients. Arthroscopy. 2013;29(7):1211–1216. doi: 10.1016/j.arthro.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill DP, for the SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Marlovits S., Striessnig G., Schuster R., Stocker R., Luxl M., Trattnig S. Extended-duration thromboprophylaxis with enoxaparin after arthroscopic surgery of the anterior cruciate ligament: a prospective, randomized, placebo-controlled study. Arthroscopy. 2007;23(7):696–702. doi: 10.1016/j.arthro.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Falck-Ytter Y., Francis C.W., Johanson N.A., Curley C., Dahl O.E., Schulman S. American College of Chest Physicians: prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(Suppl. 2):e278S–e325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hetsroni I., Lyman S., Do H., Mann G., Marx R.G. Symptomatic pulmonary embolism after outpatient arthroscopic procedures of the knee: the incidence and risk factors in 418 323 arthroscopies. Bone Jt. J. 2011;93(1):47–51. doi: 10.1302/0301-620X.93B1.25498. [DOI] [PubMed] [Google Scholar]
- 13.Janssen R.P., Sala H.A. Fatal pulmonary embolism after anterior cruciate reconstruction. Am. J. Sports Med. 2007;35:1000–1002. doi: 10.1177/0363546506298581. [DOI] [PubMed] [Google Scholar]
- 14.Delis K.T., Hunt N., Strachan R.K., Nicolaides A.N. Incidence, natural history, and risk factors of deep vein thrombosis in elective knee arthroscopy. Thromb. Haemost. 2001;86:817–821. [PubMed] [Google Scholar]