Highlights
-
•
This is the first case of an osteoma in the medial and lateral part of the sigmoid notch.
-
•
Sigmoid notch osteomas are rare and this is only the seventh such case reported in the English literature.
-
•
Surgical intervention was performed under general anaesthesia after nasal intubation with a transoral endoscopy assisted approach.
Keywords: Osteoma, Mandibular notch, Endoscopy, Case report
Abstract
Introduction
Osteomas are slow-growing benign tumours composed of mature compact or cancellous bone and are seen in facial bones but uncommonly in the mandible; cases that arise in the notch region are rarely reported in the literature.
Presentation of case
This article presents a 37-year-old woman with no preauricular swelling, no limitation of joint motion and pain only on the left side.
Discussion
The patient was evaluated based on preoperative clinical manifestations, orthopantomography and a computed tomography (CT) scan. The CT scan showed bone density irregularity between the coronoid process and the left mandibular condyle in the notch region arising both medially and laterally. Surgery was performed based on these images and the patient's indications and symptoms.
Conclusion
Among the cases of osteoma in the literature, only six originated in the mandibular notch, but this is the only that was both medially and laterally located.
1. Introduction
Osteomas are uncommon, slow-growing benign tumours composed of mature compact or cancellous bone [1]. They are essentially restricted to the craniofacial skeleton and are rarely, if ever, diagnosed in other bones [2,3]. In the literature, we found only six cases originating in the sigmoid notch of the mandible [4]. The literature describes three different types of osteomas depending on their location [5]: (1) osteomas may arise on the surface of bone as a polypoid or sessile mass (periosteal, peripheral or exophytic osteoma); (2) they may be located in the medullary bone (endosteal or central osteoma); and (3) extra-skeletal soft tissue lesions are typically located within muscle or the dermis of the skin (osteoma cutis).
The aim of this study is to report a case of a particularly rare osteoma that developed in the sigmoid notch region both medially and laterally with particular attention to the histopathological, radiological, clinical and surgical aspects. This is the first case of an osteoma in the medial and lateral part of the sigmoid notch.
2. Presentation of case
A 37-year-old woman was referred to our institute, with left-sided preauricular pain lasting 1 year and aggravated by palpation, but with no mouth-opening limitation.
She experiences discomfort while chewing food.
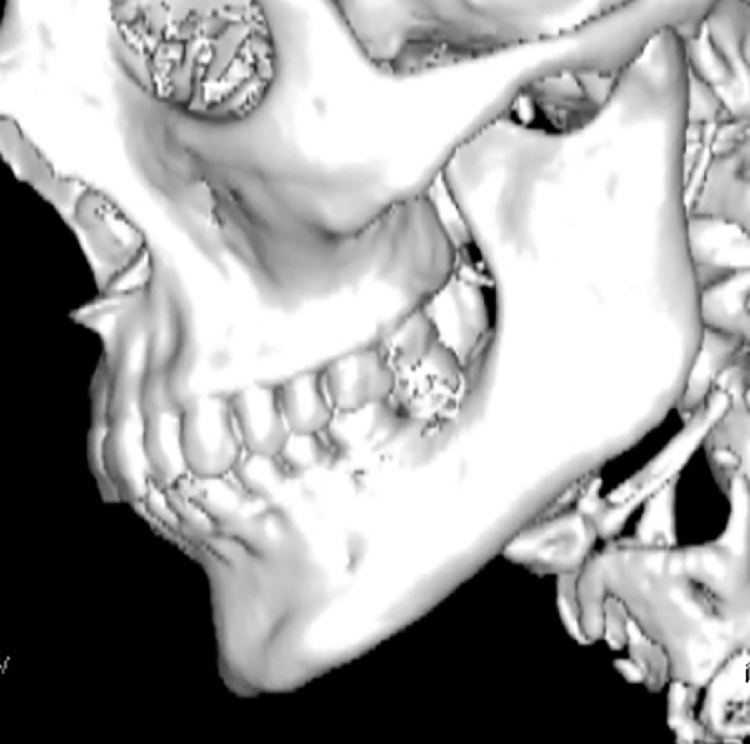
There was no history of trauma or other events contributing to onset of the symptoms. A physical examination did not detect any facial nerve paralysis, hearing or facial sensation disturbances. The results of orthopantomography were not significant. A computed tomography (CT) scan with three-dimensional reconstruction revealed bone density irregularity between the coronoid process and the left mandibular condyle with dimensions of 15 × 13 × 11 mm (Fig. 1, Fig. 2). Because the lesion didn’t have radiologic features compatible with malignant nature, no exploratory biopsy was performed.
Fig. 1.
Preoperative three-dimensional computed tomography scan.
Fig. 2.
Axial Ct scan of the Lesion.
A provisional diagnosis of osteoma was made.
Surgical intervention was performed under general anaesthesia after nasal intubation with a transoral endoscopy assisted approach. An intraoral anterior ramal incision similar to the one used for a sagittal osteotomy of the mandible was made; the lateral and medial surface of ascending ramus was exposed up to the coronoid process, then the masseter muscle and the temporal tendon were stripped laterally to expose the mass, and the lesion was removed at the level of the sigmoid notch. We visualised the neoformation through an endoscope using 0° and 45 ° angle optics (Karl Storz, Tuttlingen, Germany) (Fig. 3). Then, we performed an ostectomy of the lesion using a drill with a curved rotary cutter working both medial and lateral to the coronoid process. Coronoidectomy wasn’t performed.
Fig. 3.
Intraoperative endoscopic view.
The lesion was completely removed and was sent for histopathological evaluation. The surrounding soft tissues were intact. The specimen was a nodular 15 × 13 × 11 mm formation with a hard outer surface.
Primary closure of the wound was achieved with 4-0 Vicryl.
Multiple fragments of mature lamellar bone with few marrow spaces were observed microscopically. These histopathological findings revealed a diagnosis of compact osteoma. The follow-up period was 12 months without recurrence (Fig. 4).
Fig. 4.
Postoperative three-dimensional computed tomography scan.
This case report was written according to the Surgical CAse REport guidelines [21].
3. Discussion
Osteoma is defined by World Health Organisation as a benign lesion consisting of well-differentiated mature bone tissue with a predominantly laminar structure and very slow growth [6]; it is clearly distinct from exostoses and tori, which are hamartomas. Their aetiology remains unknown [[7], [8], [9]].
Some authors have considered that these tumours arise either from embryological cartilaginous nests or from persistent embryological periosteum cells. According to developmental or embryological theory, osteomas would originate from the suture between bones with different embryological derivations (membranous/endochondral) [10]. Other possible aetiological factors are inflammation [11], trauma and endocrine pathologies [12]. However, none of these hypotheses related to the aetiology of these lesions has been proven [13].
We found only six cases in the literature located laterally, medially or in the middle of the sigmoid notch [4]. This case is thus novel because the osteoma was located both medially and laterally.
Osteomas appear radiographically as circumscribed sclerotic masses; periosteal osteomas may have a uniform sclerotic pattern or may demonstrate a sclerotic periphery with a central trabecular pattern [5]. CT is the best imaging modality to determine the location, attachment, extension and anatomical relationship of the lesion [14]. The actual prevalence of osteomas in unknown; however, Sondergard reported that the prevalence of osteoma in the normal population in about 4% [15].
Histological classification is used to differentiate among compact (dense, compact bone), cancellous (soft, spongy bone) and mixed-type osteomas. A compact osteoma consists of mature lamellar bone with few marrow spaces. A cancellous/trabecular osteoma is characterised by bony trabeculae and fibro-fatty marrow enclosing osteoblasts, surrounded by a cortical bone margin. The compact type is the most common type seen in the mandible, as in our case.
The differential diagnosis of osteomas includes exostoses, osteochondroma, osteoid osteoma, periosteal osteoblastoma, parosteal osteosarcoma, peripheral ossifying fibroma, Paget’s disease, fibrous dysplasia and odontoma [16,17].
Treatment includes observation with periodic clinical and radiological examinations [18] for small, non-progressing, asymptomatic solitary lesions. Surgery should be considered for large, deforming osteomas [4]. In the present case, excision was considered, as the lesion was progressive and was causing pain during jaw movement.
We adopted an endoscopy assisted transoral approach for aesthetic purposes, which allowed easy access to this unusually located osteoma. The follow-up period is currently 12 months without recurrence. Recurrence of a peripheral osteoma after surgical excision is extremely rare [4]. Malignant transformation of a peripheral osteoma has not been reported in the literature [4].
4. Conclusion
Sigmoid notch osteomas are rare and this is only the seventh such case reported in the English literature [4,12,19,20]. Among the previously reported cases, the mean age at presentation was 48.7 years. In contrast to the other reported cases, our patient’s osteoma was located both medially and laterally.
Five cases were females and two were males. The tumour was localised in the right part in four cases and the left in three. Conservative management was adopted in cases where the lesion was asymptomatic (two cases plus one not available); in the present case, pain during mandibular movement and the particular location warranted surgical excision. An osteoma in the mandibular notch region is rare: diagnosis, as well as the description of each new case, is essential for documentation, especially for this type of tumour, which has a very low incidence.
Conflicts of interest
No conflict.
Sources of funding
No found.
Ethical approval
Ethical approval has been exempted by my institution, Spedali Civili Brescia, Italy.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Gabriele Bocchialini have contributed in study concept, data collection, data analysis and interpretation and in writing the paper.
Andrea Bolzoni Villaret have contributed in study concept, data collection and data analysis.
Stefano Negrini have contributed in data collection, data analysis and interpretation.
Andrea Tironi have contributed in data analysis and interpretation.
Luana Salvagni have contributed in study concept and writing the paper.
Andrea Castellani have contributed in study concept, data collection, data analysis and interpretation.
Registration of research studies
No.
Guarantor
Gabriele Bocchialini.
References
- 1.Kaplan I., Calderon S., Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J. Oral Maxillofac. Surg. 1994;52(5):467–470. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 2.Clauser L., Meneghini F., Curri D. Osteoma of the frontoethmoidal sinuses: craniofacial resection and reconstructive strategy. J. Craniofac. Surg. 1991;2(2):75–81. [PubMed] [Google Scholar]
- 3.Gray J., Snip R. Giant, mushroom-shaped osteoma of the orbit originating from the maxillary sinus. Am. J. Ophthalmol. 1977;83(4):587–591. doi: 10.1016/0002-9394(77)90572-4. [DOI] [PubMed] [Google Scholar]
- 4.Sasidharan A., Gohil A., Koshy S., Gupta A.K. Bony tumour in an unusual location on the mandible. Indian J. Plast. Surg. 2015;48(May–August (2)):200–203. doi: 10.4103/0970-0358.163062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neville I. 3rd ed. Elsevier; 2009. Oral and Maxillo-Facial Pathology; pp. 650–651. [Google Scholar]
- 6.Aghabeigi B., Evans A.W., Crean S.J., Hopper C. Simultaneous repair of an orbital floor fracture and removal of an ethmoid osteoma: case report and review of the literature. Int. J. Oral Maxillofac. Surg. 2003;32(1):94–96. doi: 10.1054/ijom.2002.0275. [DOI] [PubMed] [Google Scholar]
- 7.Iatrou I.A., Leventis M.D., Dais P.E., Tosios K.I. Peripheral osteoma of the maxillary alveolar process. J. Craniofac. Surg. 2007;18(5):1169–1173. doi: 10.1097/SCS.0b013e31812f76d8. [DOI] [PubMed] [Google Scholar]
- 8.Kashima K., Rahman O.I.F., Sakoda S., Shiba R. Unusual peripheral osteoma of the mandible: report of 2 cases. J. Oral Maxillofac. Surg. 2000;58(8):911–913. doi: 10.1053/joms.2000.8223. [DOI] [PubMed] [Google Scholar]
- 9.Firat D., Sirin Y., Bilgic B., Ozyuvaci H. Large central osteoma of the maxillary antrum. Dentomaxillofac. Radiol. 2005;34(5):322–325. doi: 10.1259/dmfr/15263929. [DOI] [PubMed] [Google Scholar]
- 10.Varboncoeur A.P., Vanbelois H.J., Bowen L.L. Osteoma of the maxillary sinus. J. Oral Maxillofac. Surg. 1990;48(8):882–883. doi: 10.1016/0278-2391(90)90351-2. [DOI] [PubMed] [Google Scholar]
- 11.Sugiyama M., Suei Y., Takata T., Simos C. Radiopaque mass at the mandibular ramus. J. Oral Maxillofac. Surg. 2001;59(10):1211–1214. doi: 10.1053/joms.2001.26727. [DOI] [PubMed] [Google Scholar]
- 12.Bessho K., Murakami K.-I., Iizuka T., Ono T. Osteoma in mandibular condyle. Int. J. Oral Maxillofac. Surg. 1987;16(3):372–375. doi: 10.1016/s0901-5027(87)80162-5. [DOI] [PubMed] [Google Scholar]
- 13.Regezi J., Sciubba J. Guanabara Koogan; Rio de Janeiro, Brazil: 1993. Patologia Bucal. Correlações Clinicopatológicas. [Google Scholar]
- 14.Rao S., Rao S., Pramod D.S. Transoral removal of peripheral osteoma at sigmoid notch of the mandible. J. Maxillofac. Oral Surg. 2015;14(March (Suppl. 1)):255–257. doi: 10.1007/s12663-013-0472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sondergaard J.O., Svendsen L.B., Hegnhoj J.O., Witt N. Mandibular osteomas in ulcerative colitis. Scand. J. Gastroenterol. 1986;21:1089–1090. doi: 10.3109/00365528608996426. [DOI] [PubMed] [Google Scholar]
- 16.Greenspan A., Remagen W. Bone-forming tumors. In: Greenspan A., Remagen W., editors. Differential Diagnosis of Tumors and Tumor-Like Lesions of Bone and Joints. Lippincott-Raven Publishers; Philadelphia, Pa, USA: 1998. pp. 25–122. [Google Scholar]
- 17.Cerase A., Priolo F. Skeletal benign bone-forming lesions. Eur. J. Radiol. 1998;27(1):S91–S97. doi: 10.1016/s0720-048x(98)00049-7. [DOI] [PubMed] [Google Scholar]
- 18.Sekerci A.E., Sahman H., Ertas E.T., Sisman Y. An unusual peripheral osteoma of the mandibular notch: a case report with computed tomography evaluation. Oral Radiol. 2011;27:78–82. [Google Scholar]
- 19.Shulze D. Radiographic diagnostic: osteoma of the left mandibular notch. Quintessence Int. 2008;39:702–703. [PubMed] [Google Scholar]
- 20.Iwai T., Izumi T., Baba J., Maegawa J., Mitsuda K., Tohnai I. Peripheral osteoma of the mandibular notch: report of a case. Iran. J. Radiol. 2013;10:74–76. doi: 10.5812/iranjradiol.3734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]