Abstract
Background and aim
Vanek's tumor is a rare solitary lesion that is non-neoplastic, and arises from the submucosa of the gut. The most commonly affected sites are the stomach and the ileum [1]. IFP causing intestinal obstruction is uncommon and that ileo-ileal intussusception has been reported in the literature rarely. We present a case of an ileo-ileal intessuception in a patient who presented with acute on chronic pain abdomen and anorexia. CT abdomen & pelvis revealed a 46 × 36 mm intraluminal mass in the left iliac fossa causing ileo-ileal intussusception.
Case presentation
A 60 years old gentleman was brought to the A&E with a history of intestinal obstruction. He was examined and admitted to the surgical unit. CBC revealed unique feature of reactive thrombocytosis apart from a low hemoglobin and a raised TLC. His CT scan demonstrated findings of ileo-ileal intussusception. After an informed written consent, patient underwent an exploratory laparotomy and had resection and anastomosis of the bowel. Histopathology of the specimen revealed findings compatible with IFP. Patient made an uneventful recovery post-operatively and was sent home in the next few days. On follow-up, the patient was doing well and had no complaints of abdominal pain or anorexia.
Conclusion
Vanek's tumor although a rare entity, should be considered in each case of acute abdomen and physicians and surgeons need to have a high degree of suspicion in such cases. Moreover, IFP can cause reactive thrombocytosis that gets resolved after a post-operative period of 6–8 weeks.
Keywords: Vanek's tumor, Inflammatory fibroid polyp, Ileo-ileal, Intussusception
Highlights
-
•
IFP is a rare entity.
-
•
Most commonly involves the gastric antrum and ileum.
-
•
Presents as an acute abdomen.
-
•
They can cause reactive thrombocytosis.
-
•
CT scan is helpful in the diagnosis.
-
•
The preferred treatment is operative resection.
1. Introduction
Intussusception means invagination of the proximal part of the gut into the distal part [2]. They can occur in children and in adults, the causes being different in both the cases. In adults, tumors are the main etiology for intussusception and around 80% of them are benign [3,4]. Inflammatory fibroid polyp is a rare, benign lesion of the GI tract [5]. Vanek in 1949 described the condition for the first time as an eosinophilic submucosal granuloma [6]. Later on, in 1953, the term IFP was proposed by Helwig and Ranier and is thus the generally accepted term [7]. Ileal intussusception is rarely caused by inflammatory fibroid polyp [8]. We report a case of an ileo-ileal intussusception in a 60 years old gentleman who presented with symptoms of subacute intestinal obstruction and anorexia due to an ileo-ileal intussusception caused by inflammatory fibroid polyp.
This work has been reported in line with the SCARE criteria [9].
2. Case presentation
A 60 years old patient presented to the ER with the chief complaints of pain abdomen and anorexia for the last few days. The pain was generalized in origin, more so in the left iliac fossa and was moderate in nature associated with nausea. The patient had few mild episodes of pain in the previous month but he didn't seek proper medical attention and had used various OTC medications for pain relief. He denied any episode of bleeding per rectum during the course of his illness. There was no history of weight loss. His previous history reveals a right inguinal hernia mesh repair in 2015 and a hemorrhoidectomy for grade-III hemorrhoids 2 months back. He had an unremarkable drug, family or psychosocial history including smoking status.
On examination, the patient was anemic. Abdomen was slightly distended, with tenderness in the left flank region, resonant percussion notes and sluggish bowel sounds. His lab results showed an Hb of 7.4mg/dl and a TLC of 15,180/cmm and Platelet count of 870,000/cmm. An erect radiograph of the abdomen showed air fluid levels. CT abdomen & pelvis was advised that demonstrated an eccentrically located, heterogeneously enhancing intraluminal mass in the left iliac fossa acting as a lead point for intussusception formation and resultant distended fluid filled proximal gut loops (Fig. 1).
Fig. 1.
Intraluminal mass in the left iliac fossa and resultant dilated gut loops.
The patient was prepared for surgery by keeping him nil by mouth, passing a nasogastric tube, catheterizing him, starting i/v fluids, i/v antibiotics, i/v analgesics and i/v antiemetics. TED stockings were applied for VTE prophylaxis. The patient was transfused packed red blood cells and then taken to the operating room and a midline laparotomy was performed. Per-operative findings were an ileo-ileal intussusception approximately 6 feet from the ileocecal junction with proximal distended fluid filled gut loops (Fig. 2, Fig. 3).
Fig. 2.
Ileo-ileal intussusception.
Fig. 3.
The lead point for intussusception formation.
He underwent segmental resection of the lesion, an end-to-end anastomosis was fashioned. The surgery was performed by the consultant. The specimen was sent for histopathology. The lesion was polypoid in nature (Fig. 4).
Fig. 4.
Polypoid lesion along with the resected ileal segment.
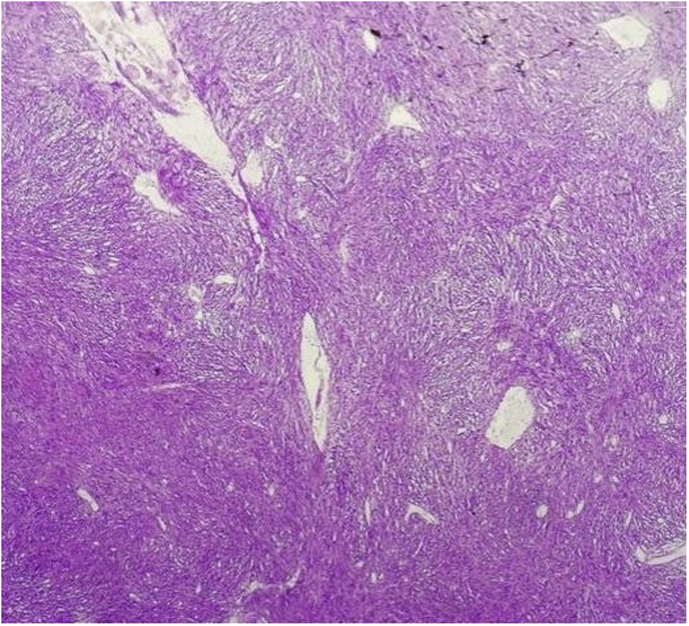
The patient was alright post-operatively, stayed in the unit for the next few days and was sent home on the 3rd post-op day. The histopathology revealed a circumscribed CD34 positive submucosal lesion showing mixture of prominent capillaries, spindle cells and inflammatory cells, predominantly eosinophils and plasma cells in a granulation tissue like stroma, findings compatible with inflammatory fibroid polyp (Fig. 5, Fig. 6).
Fig. 5.
Lobular architecture with fascicular arrangement of spindle shaped cells in submucosa.
Fig. 6.
Spindle cells are arranged concentrically around vessels giving an onion skin appearance with abundant inflammatory cells; composed of plasma cells, lymphocytes and eosinophils.
On 8 weeks follow up, the patient was doing well and had no complaints of any GI obstructive symptoms.
3. Discussion
Intussusception was first reported by Barbette of Amsterdam in 1674 [10]. It occurs as a result of difference in motility between two parts of the intestine. The proximal part is called the intussusceptum that enters the distal portion of the small intestine, called the intussusceptien [11]. In 70–90% of cases, they are usually caused by a pathologic lead point, that can be a benign or a malignant neoplasm [12,13]. Benign lesions encompass lipomas (submucosal), congenital band adhesions, Peutz Jeghers polyps, Meckel's diverticulum and inflammatory fibroid polyps [11].
Inflammatory fibroid polyp (IFP), is known by various names that include called Vanek's tumor, eosinophilic granuloma, polypoid myoendothelioma, haemangiopericytoma, fibroma with eosinophilic infiltration and an inflammatory pseudotumour. It is a rare lesion which was described for the first time in 1949 by Vanek as a “gastric submucosal granuloma with eosinophilia” [6]. In the gastrointestinal tract, IFPs can originate in various locations. They mostly occur in the gastric antrum (66%–75%) [1] followed by small bowel (18%–20%), with 4%–7% in the colorectal region, and 1% in the esophagus, duodenum, gallbladder and appendix each [8]. In a case series study of 76 patients by Johnstone and Morson revealed that 18% of IFPs were present in the small bowel [14]. They can also be found in the jejunum as mentioned by Bays et al. in a literature review who mentioned that until 2004 less than 20 IFPs had been reported in the jejunum [15]. Nonetheless, the most common site is ileum where they cause intussusception [16]. The average age of presentation is between 5th and 7th decade of life with an equal sex distribution [17].
Grossly, IFPs are polypoid or sessile and are 0.2–12 cm in size with an average size of 4 cm being reported in the literature [[18], [19], [20]].
On Microscopic examination, IFPs reveal spindle cells in a stroma admixed to inflammatory cells mainly eosinophils, with prominent capillaries in an edematous background. The spindle cells display “onion skinning” like pattern because they are concentrically arranged around the capillaries [18,21].
On immunohistochemistry, they are CD34 positive as was in our case as well, and this suggests that they may arise from primitive vascular or perivascular cells. IFPs show negative staining with CD117, S100 and ALK1, and that distinguishes them from gastrointestinal stromal tumor (GIST), neurogenic tumor and inflammatory myofibroblastic tumors (IMTs) respectively [16,17,[21], [22], [23]].
The clinical presentation depends upon the site of the lesion. But in literature, IFPs causing intussusception has often been described as an emergency with intestinal obstruction [20,[24], [25], [26], [27], [28], [29], [30], [31]].
In our case, the patient also presented with signs and symptoms of intestinal obstruction. But our case is unique because our patient had reactive thrombocytosis (Platelet count of 870,000/cmm), that can occur secondary to inflammation and this has been reported rarely in the literature. The thrombocytosis get resolved after the operation and on 8 weeks follow up, the platelet count was normal (284,000/cmm). Hence, it is a noteworthy finding that in a patient with a history of intestinal obstruction and a complete blood count showing thrombocytosis, suspicion of inflammatory fibroid polyp cannot be ruled out.
For the diagnosis, abdominal ultrasound has got a sensitivity of 98–100%, and a specificity of 88%–89% [32]. The most accurate diagnostic study is abdominal CT scanning as it usually defines the lead point [33], as was in our case. Capsule endoscopy and retrograde double balloon enteroscopy are the new recent techniques that can be useful in the diagnosis [34,35]. The final diagnosis is made after pathologic confirmation following surgical resection [36].
The treatment of choice in adult small bowel intussusception is operative resection, although inflammatory fibroid polyps in the upper GI tract can be dealt with endoscopically [13,15,30,31].
4. Conclusion
Inflammatory fibroid polyp is rare in adults and can present in the emergency as an intussusception causing intestinal obstruction. Hence, IFP must be considered in the differential for a patient who presents with abdominal pain. The most accurate diagnostic tool is CT scan of the abdomen and surgical resection is the treatment of choice.
Consent
A written informed consent was obtained from the patient for publication of this case report and accompanying images.
Ethical approval
Khyber Teaching Hospital Peshawar, Ethical Committee.
A written informed consent was obtained from the patient for publication of this case report and accompanying images.
Funding
There are no sources of funding.
Author contribution
ZakaUllah Jan: Wrote the paper and assisted the consultant in the procedure.
Muhammad Muslim: Performed the procedure.
KaleemUllah: Assisted the consultant in the surgery, participated in data collection.
Azam Shoaib: Prepared the patient pre-operatively and participated in data collection.
Nisar Ahmed: Data analysis and interpretation.
Zainab Mahsal Khan: Study concept and data collection.
Mahmud Aurangzeb: Supervised the whole team.
Conflicts of interest
There are no conflicts of interests to be declared.
Research registration number
None.
Guarantor
ZakaUllah Jan.
Patient perspective
I had this problem of pain in my tummy for the last one month. The pain was episodic in nature and I had these episodes quite a few times in the previous month. I used the common pain medications for my pain relief. But then one day, I had severe pain in my tummy and I was feeling nauseated. Ultimately I had to visit the doctor. In the ER, the doctor examined me and was of the opinion that I have features of obstruction of the bowel. Later on, I was thoroughly investigated and I was told that I have intestinal obstruction due to some mass in my bowel. They planned my surgery, took out the mass and stitched back my bowel. I was in the hospital for a few days and was then sent home. I am alright now and doing my daily life activities with no episode of any pain. I am satisfied with the treatment as I was managed quite well.
Acknowledgements
The authors thank Dr Humaira Anjum (FCPS) from the Radiology Department of our institute for her descriptions of the CT images. They also thank Dr Umer Nisar Sheikh and Dr Saud Sarwar from the Shaukat Khanam Memorial Cancer Hospital & Research Centre Pathology Department for the histopathology images.
Contributor Information
Zaka Ullah Jan, Email: zuj_cck@yahoo.com.
Muhammad Muslim, Email: doctormuslim@yahoo.com.
Kaleem Ullah, Email: drkaleempk@gmail.com.
Azam Shoaib, Email: azam.kh47@gmail.com.
Nisar Ahmed, Email: drnisar@hotmail.com.
Zainab Mahsal Khan, Email: drzainab.sohail@gmail.com.
Mahmud Aurangzeb, Email: mahmud63@gmail.com.
References
- 1.Rais M., Chahdi H., Elfahssi M., Albouzidi A., Oukabli M. An unusual cause of intestinal obstruction in a young adult patient: inflammatory fibroid polyp. Case Rep. Surg. 2017;2017 doi: 10.1155/2017/3675848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waseem M., Rosenberg H.K. Intussusception. Pediatr. Emerg. Care. 2008;24:793–800. doi: 10.1097/PEC.0b013e31818c2a3e. [DOI] [PubMed] [Google Scholar]
- 3.Tekin A., Aksoy F., Vatansev C., Kücükkartallar T., Belviranli M., Toy H. A rare cause of ileus: invagination due to ectopic pancreas. Acta Chir. Belg. 2008 Jan 1;108(3):343–345. doi: 10.1080/00015458.2008.11680235. [DOI] [PubMed] [Google Scholar]
- 4.Chiang J.M., Lin Y.S. Tumor spectrum of adult intussusception. J. Surg. Oncol. 2009 Jun 1;99(7) doi: 10.1002/jso.21117. 457- [DOI] [PubMed] [Google Scholar]
- 5.Gara N., Falzarano J.S., Limm W.M., Namiki T.S., Tom L.K. Ileal inflammatory fibroid polyp causing chronic ileocolic intussusception and mimicking cecal carcinoma. World J. Gastrointest. Oncol. 2009 Oct 15;1(1):89. doi: 10.4251/wjgo.v1.i1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaněk J. Gastric submucosal granuloma with eosinophilic infiltration. Am. J. Pathol. 1949 May;25(3):397. [PMC free article] [PubMed] [Google Scholar]
- 7.Helwig E.B., Ranier A. Inflammatory fibroid polyps of the stomach. Surg. Gynecol. Obstet. 1953;96:335–367. [PubMed] [Google Scholar]
- 8.Akbulut S., Sevinc M.M., Cakabay B., Bakir S., Senol A. Giant inflammatory fibroid polyp of ileum causing intussusception: a case report. Cases J. 2009 Aug 12;2(1):8616. doi: 10.4076/1757-1626-2-8616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. SCARE Group,The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;31(October 34):180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Yalamarthi S., Smith R.C. Adult intussusception: case reports and review of literature. Postgrad. Med. 2005 Mar 1;81(953):174–177. doi: 10.1136/pgmj.2004.022749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yakan S., Calıskan C., Makay O., Deneclı A.G., Korkut M.A. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J. Gastroenterol. WJG. 2009 Apr 28;15(16) doi: 10.3748/wjg.15.1985. 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eisen L.K., Cunningham J.D., Aufses A.H. Intussusception in adults: institutional review. J. Am. Coll. Surg. 1999 Apr 30;188(4):390–395. doi: 10.1016/s1072-7515(98)00331-7. [DOI] [PubMed] [Google Scholar]
- 13.Karamercan A., Kurukahvecioglu O., Yilmaz T.U., Aygencel G., Aytaç B., Sare M. Adult ileal intussusception: an unusual emergency condition. Adv. Ther. 2006 Jan 1;23(1):163–168. doi: 10.1007/BF02850357. [DOI] [PubMed] [Google Scholar]
- 14.Johnstone J.M., Morson B.C. Inflammatory fibroid polyp of the gastrointesthal tract. Histopathology. 1978 Sep 1;2(5):349–361. doi: 10.1111/j.1365-2559.1978.tb01727.x. [DOI] [PubMed] [Google Scholar]
- 15.Bays D., Anagnostopoulos G.K., Katsaounos E., Filis P., Missas S. CASE report: inflammatory fibroid polyp of the small intestine causing intussusception: a report of two cases. Dig. Dis. Sci. 2004 Oct 1;49(10):1677–1680. doi: 10.1023/b:ddas.0000043385.44842.c8. [DOI] [PubMed] [Google Scholar]
- 16.Nonose R., Valenciano J.S., da Silva C.M., de Souza C.A., Martinez C.A. Ileal intussusception caused by Vanek's tumor: a Case Report. Case Rep. Gastroenterol. 2011;5(1):110–116. doi: 10.1159/000326930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wysocki A.P., Taylor G., Windsor J.A. Inflammatory fibroid polyps of the duodenum: a review of the literature. Dig. Surg. 2007;24(3):162–168. doi: 10.1159/000102099. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y.I., Kim W.H. Inflammatory fibroid polyps of gastrointestinal tract: evolution of histologic patterns. Am. J. Clin. Pathol. 1988 Jun 1;89(6):721–727. doi: 10.1093/ajcp/89.6.721. [DOI] [PubMed] [Google Scholar]
- 19.Ozolek J.A., Sasatomi E., Swalsky P.A., Rao U., Krasinskas A., Finkelstein S.D. Inflammatory fibroid polyps of the gastrointestinal tract: clinical, pathologic, and molecular characteristics. Appl. Immunohistochem. Mol. Morphol. 2004 Mar 1;12(1):59–66. doi: 10.1097/00129039-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Kerr W.H., Mark J.B. Ileal intussusception in the adult due to inflammatory fibroid polyps. Surgery (St Louis) 1968 Apr;63(4):604–608. [PubMed] [Google Scholar]
- 21.Liu T.C., Lin M.T., Montgomery E.A., Singhi A.D. Inflammatory fibroid polyps of the gastrointestinal tract: spectrum of clinical, morphologic, and immunohistochemistry features. Am. J. Surg. Pathol. 2013 Apr 1;37(4):586–592. doi: 10.1097/PAS.0b013e31827ae11e. [DOI] [PubMed] [Google Scholar]
- 22.Daum O., Hatlova J., Mandys V., Grossmann P., Mukensnabl P., Benes Z., Michal M. Comparison of morphological, immunohistochemical, and molecular genetic features of inflammatory fibroid polyps (Vanek' s tumors) Virchows Arch. 2010 May 1;456(5):491–497. doi: 10.1007/s00428-010-0914-8. [DOI] [PubMed] [Google Scholar]
- 23.Forasté-Enríquez C.F., Mata-Hernández R., Hernández-Villaseñor A., Alderete-Vázquez G., Grube-Pagola P. Intestinal obstruction in adults due to ileal intussusception secondary to inflammatory fibroid polyp: a case report. Rev. Gastroenterol. México. 2017;82(3):263–265. doi: 10.1016/j.rgmx.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 24.Rubinstein R., Mogle P., Merguerian P., Rosenmann E. Inflammatory fibroid polyp of the small intestine: report of two cases and review of the literature. Isr. J. Med. Sci. 1983 Sep;19(9):828–833. [PubMed] [Google Scholar]
- 25.Costamagna D., Erra S., Zullo A., Servente G., Durando R. Small bowel intussusception secondary to inflammatory fibroid polyp of the ileum. Chir. Ital. 2008;60(2):323–327. [PubMed] [Google Scholar]
- 26.Dome F., Taziaux P., Boniver J., Fridman V., Delbecque K. Ileum intussusception in an adult: a case report. Rev. Med. Liege. 2007;62(7–8):498–500. [PubMed] [Google Scholar]
- 27.Saïji E., Ayadi-Kaddour A., Ben S.S., Ghariani B., Chelly-Ennaiffer I., Lahmar-Boufaroua A., Goutallier-Ben F.C., Khalfallah M.T., Mzabi-Regaya S. Inflammatory fibroid polyp of the ileum presenting as intussusception: a case report in an adolescent. La Tunisie Med. 2006 Jul;84(7):454–457. [PubMed] [Google Scholar]
- 28.Karamercan A., Kurukahvecioglu O., Yilmaz T.U., Aygencel G., Aytaç B., Sare M. Adult ileal intussusception: an unusual emergency condition. Adv. Ther. 2006 Jan 1;23(1):163–168. doi: 10.1007/BF02850357. [DOI] [PubMed] [Google Scholar]
- 29.Malik K.A., Pande G.K., Aftab Z., Nirmala V. Inflammatory fibroid polyp of the ileum causing intussusception. Saudi Med. J. 2005;26(6):995–998. [PubMed] [Google Scholar]
- 30.Savargaonkar P., Morgenstern N., Bhuiya T. Inflammatory fibroid polyp of the ileum causing intussusception: report of two cases with emphasis on cytologic diagnosis. Diagn. Cytopathol. 2003 Apr 1;28(4):217–221. doi: 10.1002/dc.10258. [DOI] [PubMed] [Google Scholar]
- 31.Gonul I.I., Erdem O., Ataoglu O. Inflammatory fibroid polyp of the ileum causing intussusception: a case report. Turk. J. Gastroenterol. 2004 Mar;15(1):59–62. [PubMed] [Google Scholar]
- 32.Nemoto Y., Kaneko M., Fujisaki J., Saida Y., Takahashi K., Maetani I. A case of an ileal inflammatory fibroid polyp causing intestinal intussusception. J. Gastroenterol. Hepatol. Res. 2015 Jan 21;4(1):1451–1454. [Google Scholar]
- 33.Lvoff N., Breiman R.S., Coakley F.V., Lu Y., Warren R.S. Distinguishing features of self-limiting adult small-bowel intussusception identified at CT. Radiology. 2003 Apr;227(1):68–72. doi: 10.1148/radiol.2272020455. [DOI] [PubMed] [Google Scholar]
- 34.Kim S.G., Choi K.D., Kim J.S., Jung H.C., Song I.S. Ileal inflammatory fibroid polyp: a rare cause of obscure gastrointestinal bleeding diagnosed by wireless capsule endoscopy. Dig. Dis. Sci. 2006 May 1;51(5):906–908. doi: 10.1007/s10620-006-9338-3. [DOI] [PubMed] [Google Scholar]
- 35.Miyata T., Yamamoto H., Kita H., Yano T., Sunada K., Sekine Y., Iwamoto M., Kuno A., Onishi N., Ido K., Nokubi M. A case of inflammatory fibroid polyp causing small-bowel intussusception in which retrograde double-balloon enteroscopy was useful for the preoperative diagnosis. Endoscopy. 2004 Apr;36(04):344–347. doi: 10.1055/s-2004-814305. [DOI] [PubMed] [Google Scholar]
- 36.O'Kane A.M., O'Donnell M.E., McCavert M., Taylor K., Lee J., Wilkinson A.J. Inflammatory fibroid polyp of the ileum causing recurrent intussusception and chronic ischaemia: a case report. Cases J. 2008 Oct 16;1(1):244. doi: 10.1186/1757-1626-1-244. [DOI] [PMC free article] [PubMed] [Google Scholar]