Abstract
Recent studies of immigrant health have focused on an apparent paradox in which some new immigrants arrive healthier than expected but exhibit poorer health outcomes with duration of residence. Although a variety of explanations have been put forth for this epidemiological pattern, questions remain about the socio-historical generalizability of the empirical findings and accompanying theoretical explanations. By examining childhood mortality patterns of European immigrants to the United States in the early 20th century, this study tests hypotheses from current immigrant health literature in a previous era of immigration. In contrast with post-1965 immigrant groups, European arrivals did not have better outcomes than their U.S.-born white counterparts. Rather, their rates corresponded to a “middle tier” status in between U.S.-born black and white populations. Analysis of post-migration trajectories returned mixed results that similarly differ from contemporary patterns. Many new immigrant groups had higher rates of excess childhood mortality than their U.S-born counterparts, but outcomes appear to have improved with duration of residence or among the second generation. These findings suggest socio-historical variation in the context of reception may act as a “fundamental cause” of immigrant health and mortality outcomes.
Keywords: Immigrant health, Epidemiological paradox, Assimilation, European immigration
Highlights
-
•
I test hypotheses from current immigrant health literature in a previous era of immigration using childhood mortality estimates for European immigrants in 1910.
-
•
In contrast with post-1965 immigrant groups, European arrivals did not have better outcomes than their U.S.-born white counterparts.
-
•
European immigrant childhood mortality rates corresponded to a ”middle tier” status in between U.S.-born black and white populations, but outcomes improved with duration of residence.
-
•
Historical comparison of immigrant contexts of reception can advance understanding of the fundamental causes of immigrant health
1. Introduction
Recent research on the health of immigrant populations to the United States has focused extensively on two empirical patterns. First, many new immigrants exhibit better-than-expected health outcomes upon arrival (Antecol and Bedard, 2006, Dubowitz et al., 2010, Landale et al., 2000, Lariscy et al., 2015, Ruiz et al., 2013). This finding has been dubbed a “paradox,” in part because health advantages are often observed despite other determinants of poor health, such as low socioeconomic status and experiences of discrimination. Second, the health status of new immigrants often worsens—or health advantages fade—with greater duration of residence in the United States (Cho et al., 2004, Hamilton and Hummer, 2011, Rumbaut, 1997). The second and third generations are often less healthy than the first, and even within the population of first-generation immigrants, health status may deteriorate after migration.
Despite extensive research on this topic, it is still unclear how these patterns vary for different immigrant groups or across social, economic, cultural, and political destination contexts. Although this research originated in studies of Hispanic migrants, researchers have also found evidence supporting the “immigrant health advantage” for Asian and Pacific Islander immigrants (Frisbie, Cho, & Hummer, 2001), West Indian and African blacks (Hamilton and Hummer, 2011, Read and Emerson, 2005, Read et al., 2005), and other immigrant populations (Singh and Hiatt, 2006, Singh et al., 2013). However, scholars have also found considerable heterogeneity within pan-ethnic Hispanic and Asian categories (Camacho-Rivera et al., 2015, John et al., 2012, Subramanian et al., 2009), as well differing trends for immigrant populations that have received less empirical attention, such as Arab and Middle Eastern immigrants (Abdulrahim and Baker, 2009, Reynolds et al., 2016). Such variation raises questions about the generalizability of the mechanisms involved in the immigrant health paradox in relation to group-specific and context-specific social conditions.
Although scholars have begun expanding the scope of comparison to include a wider range of immigrant groups and destination contexts, the focus has remained on the post-1965 wave of immigration to the United States. This paper offers a comparison case by examining the childhood mortality outcomes of European immigrants to the United States in the early 20th century. Prior to the National Origins Act of 1924, immigrants represented nearly 15 percent of the U.S. population, yet little is known about the health and mortality patterns of immigrants during this period. Testing hypotheses from contemporary immigrant health research in a previous era of immigration can be valuable for contextualizing empirical patterns and theoretical explanations in the literature. Specifically, finding evidence of the paradox in a drastically different historical context would support the generalizability of the selection and acculturation mechanisms that dominate the research. However, health patterns that differed from the expected pattern—of healthy arrivals followed by deterioration with duration of residence—would direct attention toward alternative explanations and highlight the importance of contextualizing research and theory about the causes of immigrant health trajectories.
The findings of this study suggest early immigrants followed a very different trajectory than contemporary migrants—new immigrants had higher childhood mortality rates than the U.S.-born white population and saw improvement with duration of residence. There was also considerable heterogeneity in outcome patterns within the European immigrant population tied to region of origin, likely shaped in part by selection effects and consequences of contemporaneous ethno-racial boundary hierarchies. The paper concludes with a discussion of how historical comparison can contribute to contemporary immigrant health research by shifting causal questions further “upstream.” Many explanations for patterns of immigrant population health focus extensively on risk factors for disease, such as stress experiences, behavioral changes, and similar post-migration exposures. Historical comparison can explicitly highlight the variable upstream social conditions that shape immigrants’ ability to avoid such risks or minimize the consequences of disease after migration. For early European immigrants, childhood mortality patterns corresponded both to contemporaneous ethno-racial boundaries and a process of linear assimilation that was unique to the era. I argue that such social and political characteristics in the context of reception can be conceptualized as a fundamental cause (Link & Phelan, 1995) that shapes access to resources for new immigrants across eras of differing risk factors and diseases. This insight can be applied to contemporary research on immigrant health as well.
2. Background
2.1. Explaining immigrant health trajectories
Existing explanations for the “immigrant health paradox” include both generalizable and contextualized theories. Studies have often explained the initial better-than-expected health outcomes of new migrants as a result of selection during the migration process, selective return migration, or cultural differences that shape health behaviors (Dubowitz et al., 2010, Palloni and Arias, 2004). At least a portion of the selection effect is thought to be inherent to the migration process—i.e., it is more difficult for the critically and chronically ill to migrate long distances, thus any immigrant sub-population will under-represent the less-healthy tail of a population distribution (Jasso, Massey, Rosenzweig, & Smith, 2004). In theory, these selective barriers to migration would also be present for European immigrants undertaking long journeys by ship in the early 1900s.
Other explanations are more context-specific and might not apply across eras. Proponents of the “cultural buffering” explanation note that many immigrant groups, particularly Hispanic migrants, share cultural norms that promote better diets, stronger social ties, and lower rates of smoking and alcohol abuse, relative to the U.S.-born population (Antecol and Bedard, 2006, Blue and Fenelon, 2011, Fenelon, 2013, Singh and Siahpush, 2002). This process inherently depends on characteristics of origin-group culture, as well as the links between behaviors and major risk factors for disease. Infectious diseases were a larger cause of overall mortality in the early 1900s, which would suggest a different set of risk factors tied less to long-term patterns of diet and exercise. Similarly, although contemporary mortality data are possibly skewed by return-migration of older migrants—known as the “salmon bias” (Palloni and Arias, 2004, Turra and Elo, 2008)—such reverse selection depends on contextual factors, such as feasibility of return migration. Although transnationalism and return migration played a role in migration patterns in the early 1900s (Wyman, 1996), return trips were less feasible and less common than they are today.
Of particular interest to scholars of health inequalities is how and why the initial better-than-expected health outcomes for new migrants tend to disappear with duration of residence. The prevalence of many health conditions increases across generations for minority immigrant groups to the United States, and often morbidity and mortality risk can increase for the first generation with 10 years or less (Cho et al., 2004, Hamilton and Hummer, 2011, Rumbaut, 1997, Teitler et al., 2015). This pattern of declining health advantages has not only been observed for adult mortality and major disease categories, but it is also found for infant mortality (Hummer et al., 2007, Landale et al., 2000, Singh et al., 2013) and other indicators of maternal and infant health, such as preterm and low birthweight births (David and Collins, 1997, Osypuk et al., 2010, Teitler et al., 2012).
One of the most common explanations for these patterns of worsening health is the “acculturation hypothesis,” which attributes changes in immigrant health outcomes primarily to the adoption of unhealthy behaviors, such as smoking, a sedentary lifestyle, and unhealthy diets (Dubowitz et al., 2010, Dubowitz et al., 2007). However, researchers increasingly note the importance of understanding how “upstream” social conditions shape such acculturation patterns and processes. For instance, health effects of duration of residence vary by race and experiences racism in both sending and receiving contexts (Brown, 2018, Read and Emerson, 2005). Changes in behavioral patterns also often occur in conjunction with material hardship and processes of cumulative disadvantage (Allen et al., 2014, Riosmena et al., 2015), suggesting either segmented trajectories or multicausal mechanisms that extend beyond cultural change. Assimilation may even protect against poor health or mediate the relationship in neighborhoods of relatively low disadvantage (Akresh et al., 2016, Finch et al., 2007). Although the acculturation hypothesis is often tested as a generalizable linear process, a growing body of research finds that it is not acculturation alone, but the context of acculturation, that influences post-migration trajectories.
2.2. Fundamental causes of immigrant health
Immigrant health research to date has broadly been characterized by attention to proximate risk factors and determinants of population health, such as health behaviors, acculturative stress, stress from discrimination, and social ties. Yet scholars of immigrant health have increasingly called for greater attention to the contextual factors that shape post-migration trajectories, such as structural inequality, institutional racism, and experiences of discrimination (Acevedo-Garcia et al., 2012, Finch et al., 2004, Holmes, 2006, Yoo et al., 2009). Such work has the potential to push immigrant health research further “upstream” toward investigating the social conditions that shape migration, integration, and associated exposure to risk factors or access to resources that affect health.
Currently, one of the most influential theoretical perspectives in fields studying health and health inequalities looks at social conditions broadly as a fundamental cause of disease (Hankin & Wright, 2010). Link and Phelan, 1995, Link and Phelan, 1996 argue that social conditions can be considered a fundamental cause because they shape access to resources—both material and symbolic—that can be used to avoid risks or to minimize the consequences of disease after it occurs, even as the more proximal risk factors, linking mechanisms, and diseases change. In this sense, social conditions act as a “cause of causes” or “risk of risks” that can persist across various risk factors and disease outcomes (Link & Phelan, 2010).
Research on immigrant health has remained remarkably disconnected from the fundamental cause literature. A “Web of Science” search of the terms “immigrant” and “health” returns 11,106 articles and book chapters published between 1989 and 2017, only three of which directly reference “fundamental cause” theory. This is likely due to the “paradox” of healthy immigrant arrivals that contradicts the strong association between socioeconomic status and health seen in other populations. Link and Phelan (2010) acknowledge that this is an empirical pattern that “fundamental-cause theory as it has been formulated so far does not explain” (p. 15).
However, the fundamental cause perspective is not incompatible with immigrant health research. The challenge is identifying the unique social conditions that shape the “risk of risks” or “cause of causes” for immigrant populations, particularly after migration. Sociologists have long been interested in how aspects of the context of reception—the social, political, and economic environment into which individuals and groups migrate—play a major role in organizing the life chances of new arrivals. Characteristics of the receiving context, including state barriers to incorporation, symbolic boundaries against immigrant groups, contemporaneous ethno-racial hierarchies, and economic conditions, can shape immigrant socioeconomic trajectories as well as strategies for adaptation and integration (Portes and Böröcz, 1989, Portes and Zhou, 1993, Portes et al., 2005, Stepick and Stepick, 2010).
Shifting attention upstream to the context of reception can improve understanding of the distribution of more proximate risk factors that shape the immigrant health paradox, as well as explanations for how and why it may change with duration of residence. Selection of healthy immigrants operates, in part, through restrictive immigration policies, cultural receptivity, and other contextual factors that create barriers to immigration. Similarly, post-migration exposure to risk factors, including behavioral changes, are tied to context-dependent opportunities for mobility and integration. Scholars of race and immigration often study early 20th century migration to compare processes of assimilation, inter-group social dynamics, and ethno-racial boundary construction across historical contexts. Such comparison can similarly highlight the connections between varying social conditions and downstream patterns of health and mortality.
2.3. The context of reception in the early 20th century
Immigration to the United States has come in waves, with each wave composed of different origin groups. Before the turn of the 20th century, most immigrants arrived from Northern and Western Europe. In the 1860s, for example, immigrants from Germany, the United Kingdom, and Ireland made up 80% of all new arrivals (see Fig. 1). By the early 1900s, migrants from Central and Eastern Europe and immigrants from Southern European countries, such as Italy, constituted the majority of new arrivals. In absolute size, the number of annual immigrants in the early 1900s was comparable to the most recent wave of migration. In relative terms, migration represented a larger proportion of the population than documented migration does today.
Fig. 1.
Immigration to the United States, 1830-2013. Source: Yearbook of Immigration Statistics, Department of Homeland Security. Data represents number of individuals obtaining permanent lawful resident status per 10-year period.
Social scientists and historians have noted two key differences between the socio-historical contexts of early-wave and contemporary immigration. First, ethno-racial categories—and accompanying ethno-racial hierarchies—were different in the early 1900s. Although European immigrants were officially classified as white in Census documents, historians and sociologists have documented a different racial logic of the period that dissected the white/European population into a hierarchy based on what were considered inherent differences between Anglo-Saxon and Nordic Europeans and more recent arrivals from Southern, Central, and Eastern Europe (Brodkin, 1998, Jacobson, 1999, Roediger, 2006). It was not uncommon to see references to Irish physiology, Slav character, or other racialized trait descriptions in public discourse. The Dillingham Commission, formed in 1907 to study the “problem” of immigration, simultaneously used phrases of “race”, “stock”, or “peoples” to describe dozens of linguistic and origin-country population divisions (Dillingham, 1911). Eugenics science provided a language for reifying such differences and explaining social position as an outcome of genetic makeup and group characteristics.
For a period, new-wave European immigrant groups occupied a “middle tier” in the U.S. racial hierarchy. They were not subject to the same level of discrimination, exploitation, and racialization as the black population. However, they also were not considered full members of the Anglo-Saxon/Nordic white population at the top of the hierarchy. Irish immigrants were the first occupants of this middle tier status in the 19th century (Ignatiev, 2009), but in the early 20th century Italian and Jewish immigrants from Central and Eastern Europe were growing targets of discrimination and racialization. Many of the social conditions that characterized life for these groups—low socioeconomic status, occupational and residential segregation, and experiences of discrimination—are considered key social determinants of poor health and early mortality for contemporary minority groups. Immigrants were excluded from certain jobs—as symbolized in the iconic “Irish Need Not Apply” advertisements—or limited to low-wage work. They were often segregated in urban areas, where they were closely packed together in neighborhoods with poor sanitation and limited resources (Riis, 1901). At times, avenues to political office and other civic institutions were closed off, and racialized nativism occasionally manifested in lynchings of Italian and Jewish immigrants (Jacobson, 1999).
A second key distinction of early 20th century immigration was the assimilation pathway available to immigrants. Despite facing discrimination and racialization, European immigrants were able to assimilate into the mainstream population of U.S.-born whites over time. Early research on European immigrants viewed assimilation as a linear process, in which low-SES new immigrants arrived in urban immigrant enclaves but gradually transitioned to more ethnically-mixed suburbs in subsequent generations as they achieved a higher socioeconomic status and integrated into the mainstream white middle class (Alba, Logan, Stults, Marzan, & Zhang, 1999). This happened across generations but was also facilitated over time by policies such as post-war welfare state spending that provided opportunities for upward mobility but explicitly excluded the black population (Brodkin, 1998).
Such characteristics of the context of reception may be crucial for understanding the post-migration exposure to risk factors and disease for immigrants and their children. A model of linear assimilation allows for greater access to resources for avoiding disease and maintaining health over time. Such a pathway is not uniformly available to contemporary migrants, who may experience segmented assimilation, which can involve downward mobility or maintenance of strong ethnic community ties (Portes and Rumbaut, 2006, Portes and Zhou, 1993, Restifo et al., 2013). Differences in social context, ethno-racial boundary configurations, and structural constraints in the context of reception may represent larger barriers to integration and mobility for post-1965 migrants than for early-wave European arrivals (Portes and Rumbaut, 2006, Portes et al., 2005, Rumbaut, 1994, Stepick and Stepick, 2010). A key distinction between the two eras is the racial barriers faced by each group. Although early 20th-century European immigrants were eventually perceived as part of the U.S. white population, immigrants arriving after the 1960s from Central/South America and Asia have not made a similar transition.
3. Methods
3.1. Data
This paper examines patterns of childhood mortality using individual-level data from a 1% sample of the 1910 Census provided by the Minnesota Population Center's Integrated Public Use Microdata Series (Ruggles et al., 2010). The 1910 IPUMS dataset is a 1-in-100 sample of the United States population, including Alaskans, Hawaiians, and persons enumerated on the American Indians schedules. The 1910 sample is the only one to include data on number of marriages, total number of children born, and total number of children surviving, which are used to estimate excess childhood deaths. The final sample consists of women ages 15-49 who are not missing birth or marriage data.
3.2. Measures
Excess childhood deaths: Researchers have used indirect methods to estimate childhood mortality using available information in Census reports (Haines and Preston, 1997, United Nations, 1982). Using two key pieces of information—number of children ever born to a mother and number of surviving children—I adapt these methods to estimate excess childhood mortality at the individual level for mothers in the 1910 IPUMS dataset. Childhood mortality encompasses both infant mortality and deaths occurring after the first year of life. In this sense, it can be an indicator of both maternal health (a factor in infant mortality) and the health of the child. More than 70 percent of all deaths under the age of five in 1910 occurred within the first year of life, although infant mortality represented a smaller proportion of under-five deaths for foreign-born groups compared to the general population (see Table 5 in Harris, 1913).
Measures of excess deaths are often calculated at the group level as the number of observed deaths in the population minus an estimate of the expected deaths, based on some conditional prediction. Although general measures of excess death are not typically measured at the individual level for general mortality (i.e., every person has one observed and expected death), the possibility of multiple births per woman allows for variation in both observed and expected childhood mortality. The observed deaths per woman are calculable from the 1910 IPUMS dataset using information on the number of children born and the number of surviving children.
Estimating the number of expected deaths can be approached in multiple ways. Scholars have used information about the duration of marriage to estimate exposure to risk of death for children before a certain age, based on the assumption that marriage duration is a rough proxy for the age of the first child. Because information on marriage duration is used to estimate exposure to risk for children of the respondent, women who have been married more than once are excluded from the analysis, as are women married 25 or more years, following Haines and Preston (1997). I combine this approach with model life tables to adjust the probability to specific populations (in this case, estimates for Western and Eastern Europe provided by the United Nations). Following the examples provided by Haines and Preston (1997), I multiply these estimates by the number of children born to a given mother to provide an expected number of deaths at the time of the 1910 census, where:
EXPECTED DEATHS=[q(x)s/k(i)]*CEB
CEB=children ever born
q(x)s=probability of dying between birth and exact age (x) in a standard life table
k(i)=multiples from UN (United NationsManual X, United Nations, 1982) Manual X, chapter 3.
Gutmann, Haines, Frisbie, and Blanchard (2000) use similar data to calculate childhood mortality ratios at the individual level (i.e., observed deaths divided by expected deaths). Using a measure of excess mortality instead (observed – expected), includes zero-death respondents in relation to the number of expected.
Origin groups: This paper is interested in differences between immigrant groups of various European origins. Using information on the birthplace of the respondent and the respondent's mother and father, I divide first- and second-generation immigrants into four regions of origin: (1) Northern and Western Europe, (2) Ireland, (3) Southern Europe, and (4) Central and Eastern Europe. These distinctions correspond roughly to different waves of immigration to the United States (with Northern and Western Europeans arriving the earliest), as well as symbolic and social cleavages based on religion, culture, and ideas about racial difference.
The largest non-European group of white immigrants was from Canada and was coded as an “other” fourth group (results are not presented here). However, there was a significant group of immigrants from Canada whose parents were both born in Ireland, and these migrants were coded similar to other Irish immigrants. See Table A in the Appendix for a list of countries and frequencies for each origin group.
For analyses that include both immigrants and natives, the origin groups include both first- and second-generation immigrants. Birthplace data for each respondent's mother and father are coded into the categories listed above. Individuals are only included as members of the second generation if both their mother and father were born in the same origin region.
Individual-level controls: The key variable of interest for much of the analysis is duration of residence in the United States. Using reported information about the year of immigration, I divide migrants based on duration of 0-5 years, 6-10 years, 11-15 years, and more than 15 years.
Other independent variables include proxies for assimilation and controls often related to health outcomes. Age and age-squared (to account for a non-linear effect on infant mortality as mothers aged) are included as continuous measures. Family size (i.e., the number of children ever born) was included to account for fertility differences. A binary variable indicating whether the individual lived in a rural (0) or urban (1) environment is included to capture differences in settlement patterns between immigrants and natives, as well as geographic differences in health outcomes. Rural areas tended to have better overall mortality and health outcomes during this period.
To assess the effect of socioeconomic status in the absence of direct income or education data, the relative occupational prestige of each individual was derived from Duncan's Socioeconomic Index (SEI) as reported in the IPUMS microdata. The SEI is a measure of occupational status based on prestige ratings from the 1947 National Opinion Research Center (NORC) survey, the income level, and educational attainment associated with each occupation, as calculated in 1950 (Duncan, 1961). The SEI is useful because it captures multiple dimensions of socioeconomic status and rating methodology does not vary across Census years. Although there is debate about the validity of such composite measures (Hauser & Warren, 1997), previous studies suggest relative stability in occupational prestige rankings, particularly in the early half of the 20th century (Hodge, Siegel, & Rossi, 1964). Because many women in the 1910 Census were not actively in the labor market, average household SEI scores were calculated.
A binary variable representing English-language ability was included (0 = does not speak English, 1 = speaks English). Language ability is commonly included as a proxy for acculturation in research on immigrant incorporation.
Finally, a measure of home-country childhood mortality rates during the year of arrival was included to account for possible sending-country influences. Data on under-five mortality per 1,000 population were downloaded from gapminder.org. These rates are based on a combination of available data and estimates from infant mortality rates. Data were available for more than 96% of country-year combinations, and countries with missing data were assigned the average value for their origin region in their arrival year. A five-year moving average was used to smooth possible year-to-year discrepancies in data reliability.
3.3. Analysis
The analysis proceeds in two steps, each focused on a slightly different question about childhood mortality patterns of immigrant and minority groups. In the first stage, I am interested in how immigrant groups from various European origins compare to native-born whites and blacks. Using OLS regression, I compare expected childhood mortality rates between first- and second-generation Northern/Western European immigrants, Irish immigrants, Southern European immigrants, Central/Eastern European immigrants, and native-born blacks, with native-born whites as the reference group. After establishing age-adjusted difference, I control for location (rural vs. urban), SEI, and English-speaking ability, to gauge the importance of assimilation factors. I include an interaction between urban location and origin group to assess different effects for each group, in addition to differences in geographic distribution.
The second question I am interested in is whether duration of residence in the United States was beneficial or harmful for the childhood mortality outcomes of various immigrant groups. For this analysis, I use a subset of the original sample that only includes first-generation immigrants for whom duration of residence information is applicable. After establishing the average effect of duration of residence in the baseline model, I include interactions between duration of residence and region of origin to investigate whether the effect differed between European-origin immigrant groups. To account for possible sending-country effects—in other words, differences in social conditions and mortality determinants that may have affected each population before migration—the second model includes sending-country childhood mortality rates in the arrival year for each immigrant. For the final model, I again incorporate controls for location, SEI, and English-language ability. I run a similar analysis including the second generation, in addition to first-generation duration categories.
4. Results
4.1. Between-group comparisons
Table 1 includes the descriptive statistics of various groups in the sample, pooling both first- and second-generation immigrants from similar origin regions. The values for excess childhood deaths represent individual-level averages. The average U.S.-born white family had .09 fewer observed deaths than expected, corresponding to an aggregate 90 fewer child deaths per 1,000 mothers. First- and second-generation immigrants from Ireland, Southern Europe, and Central/Eastern Europe had higher rates of excess childhood mortality relative to U.S.-born whites, yet experienced fewer deaths than the black population. This is consistent with their “middle tier” status in the ethno-racial hierarchy of the era. Excess child deaths for immigrants from Northern and Western Europe, however, were roughly equivalent to their U.S.-born white counterparts. While previous research has found general immigrant-native differences among those classified as white during this period, these findings highlight the importance of considering the variability within the European immigrant population.
Table 1.
Descriptive statistics by origin group, 1910.
| U.S. White | Black | N/W Europe | Irish | S. Europe | C/E Europe | |
|---|---|---|---|---|---|---|
| Children Born | 3.18 | 3.98 | 3.46 | 3.77 | 3.89 | 3.57 |
| Excess Deaths | −0.09 | 0.26 | −0.10 | 0.05 | 0.14 | 0.02 |
| Age | 31.58 | 29.72 | 34.54 | 36.26 | 30.55 | 30.59 |
| Household SEI | 25.78 | 14.10 | 27.07 | 29.44 | 20.47 | 23.58 |
| Urban | 0.32 | 0.25 | 0.59 | 0.79 | 0.79 | 0.78 |
| English Speaking | 0.99 | 0.99 | 0.95 | 1.00 | 0.42 | 0.57 |
| Observations | 46768 | 8543 | 14861 | 4007 | 2371 | 6302 |
Note: Table includes mean values for key variables. Immigrant origin groups include both first and second generation populations.
The group characteristics also reveal notable differences in exposure to potential determinants of poor health and higher childhood mortality. Immigrants from all European countries were much more likely to live in urban areas than the U.S.-born black and white populations. Urban residence in 1910 carried greater risk of infectious disease due to poor sanitation, crowded housing, and limited medical care resources. Table 1 also reveals heterogeneity in potential acculturation levels. The most recent waves of immigrants in 1910, arriving from Southern, Central, and Eastern Europe, were much less likely to speak English than earlier populations arriving from Northern and Western Europe. Family size also varied between groups and similarly corresponded to a distribution in which European immigrants had more children born than U.S.-born whites but fewer than U.S.-born blacks.
Additional comparisons and controls are introduced to Table 2. After accounting for family size and age, the relative hierarchy of between-group outcomes remains. First- and second-generation immigrants from Northern and Western Europe had a similar risk of excess childhood mortality as U.S.-born whites, whereas other immigrant groups had significantly higher risk, though substantially lower than rates for U.S.-born blacks. This general pattern persists after controlling for household SEI in Model 2. It is worth noting that the association between SEI and excess childhood mortality is moderated by family size. In a bivariate analysis, household SEI is negatively correlated with excess mortality.
Table 2.
Excess childhood mortality by nativity, race, and region of origin.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | 0.59*** | 0.60*** | 0.62*** | 0.81*** |
| (0.05) | (0.05) | (0.05) | (0.06) | |
| Age | −0.05*** | −0.05*** | −0.05*** | −0.05*** |
| (0.00) | (0.00) | (0.00) | (0.00) | |
| Age-squared | 0.00*** | 0.00*** | 0.00*** | 0.00*** |
| (0.00) | (0.00) | (0.00) | (0.00) | |
| Origin (Native white ref.) | ||||
| Northern/Western European | −0.00 | −0.00 | −0.09*** | −0.10*** |
| (0.01) | (0.01) | (0.01) | (0.01) | |
| Irish | 0.14*** | 0.14*** | 0.08* | 0.08** |
| (0.01) | (0.01) | (0.03) | (0.03) | |
| Southern European | 0.18*** | 0.18*** | 0.02 | −0.09* |
| (0.02) | (0.02) | (0.04) | (0.04) | |
| Central/Eastern European | 0.09*** | 0.09*** | 0.10*** | 0.01 |
| (0.01) | (0.01) | (0.02) | (0.02) | |
| Black | 0.29*** | 0.30*** | 0.25*** | 0.26*** |
| (0.01) | (0.01) | (0.01) | (0.01) | |
| No. of births | 0.06*** | 0.07*** | 0.07*** | 0.07*** |
| (0.00) | (0.00) | (0.00) | (0.00) | |
| SEI | 0.01*** | −0.00 | 0.00 | |
| (0.00) | (0.00) | (0.00) | ||
| Urban | 0.12*** | 0.11*** | ||
| (0.01) | (0.01) | |||
| Interactions | ||||
| Irish*Urban | 0.11*** | 0.11*** | ||
| (0.02) | (0.02) | |||
| N/W European*Urban | 0.01 | 0.01 | ||
| (0.03) | (0.03) | |||
| S European*Urban | 0.12** | 0.13** | ||
| (0.04) | (0.04) | |||
| C/E European*Urban | −0.09*** | −0.08** | ||
| (0.03) | (0.03) | |||
| Black*Urban | 0.14*** | 0.14*** | ||
| (0.02) | (0.02) | |||
| English speaking | −0.20*** | |||
| (0.02) | ||||
| Num. obs. | 82,707 | 82,707 | 82,707 | 82,707 |
Table reports OLS coefficients with standard errors in parentheses. The SEI coefficient represents a 10-point change in household SEI score.
p 0.05.
p 0.01.
p 0.001.
A larger portion of the between-group variation appears to be related to the geographic distribution of immigrants. This is further illustrated when an interaction is introduced to highlight the relative urban vs. rural effects for each group in Model 3. All groups except Northern/Western and Central/Eastern Europeans experienced higher childhood mortality in urban environments than in rural areas. Urban residence in general was associated with higher risk of excess childhood mortality, and most recent immigrants in 1910 tended to cluster in urban areas. However, there were also differential effects of urban residence by group. Central and Eastern European immigrants appear to be an outlier among the groups, in that urban residence was much less detrimental to childhood mortality outcomes relative to other recent immigrants.
Another major factor was English speaking ability. This is a commonly-used measure of “acculturation” in contemporary research on immigration and may serve as a proxy for acculturation/assimilation of white European migrants during this period. However, speaking English was associated with lower rates of childhood mortality in Model 4, whereas research on contemporary immigrant health typically finds a determintal effect of language-based acculturation measures. Although both first- and second-generation immigrants are included in these analyses, the English-speaking variable primarily applies to the first generation. By the second-generation, at least 95% of all groups reported speaking English. In the first generation, roughly half of Central and Eastern European immigrants did not speak English, which accounts for a substantial portion of their higher rates of excess childhood mortality.
4.2. Duration effects
One of the primary objectives of this paper is to compare the effects of duration of residence on immigrant childhood mortality outcomes. Table 3 includes marginal effects estimates for duration of residence based on regression models that only include the first-generation immigrant population for which duration of residence is relevant. Childhood mortality outcomes tended to improve with greater duration of residence in the United States for the pooled group of immigrants. This finding is noteworthy in itself because it differs from the association with duration of residence seen for contemporary immigrant groups.
Table 3.
Marginal effects of duration of residence by origin group, 1910.
| Duration of Residence | No Controls | Sending Country | Full Controls |
|---|---|---|---|
| Northern/Western European | |||
| 0–5 yrs | ref. | ref. | ref. |
| 6–10 yrs | −0.042 | −0.045 | −0.033 |
| 11–15 yrs | −0.004 | −0.054 | −0.027 |
| More than 15 | −0.052 | −0.201*** | −0.164*** |
| Irish | |||
| 0–5 yrs | ref. | ref. | ref. |
| 6–10 yrs | −0.137 | −0.089 | −0.086 |
| 11–15 yrs | −0.239* | −0.228* | −0.218. |
| More than 15 | 0.002 | −0.136 | −0.126 |
| Southern European | |||
| 0–5 yrs | ref. | ref. | ref. |
| 6–10 yrs | 0.011 | −0.082 | −0.062 |
| 11–15 yrs | 0.046 | −0.132* | −0.087 |
| More than 15 | 0.123* | −0.121* | −0.055 |
| Central/Eastern European | |||
| 0–5 yrs | ref. | ref. | ref. |
| 6–10 yrs | −0.022 | −0.066* | −0.034 |
| 11–15 yrs | −0.053 | −0.17*** | −0.106* |
| More than 15 | −0.127*** | −0.31*** | −0.222*** |
As suggested in the previous section, each European immigrant group had unique integration experiences and different relative mortality outcomes during this period. Although duration of residence is generally associated with fewer excess childhood deaths, the degree of difference was not as great for Southern European or Irish immigrants after adding the full set of controls. The second model of Table 3 controls for origin-country childhood mortality rates, and suggests a portion of the variation is related to differences in mortality rates among sending country contexts and over time. For Irish immigrants, greater duration of residence also correlates with higher mortality in the origin country at the time of migration. Specifically, excess mortality for Irish immigrants with more than 15 years of residence may be due, in part, to residual effects of the Irish potato famine.
The final model in Table 3 includes all controls for SEI, urban residence, and English-speaking ability. In regression models with full controls, the relative differences in predicted probability of excess death between origin groups is almost negligible, and all groups exhibit lower excess death with greater duration of residence. This association is strongest for Central and Eastern European migrants, for whom duration of residence had the largest effect.
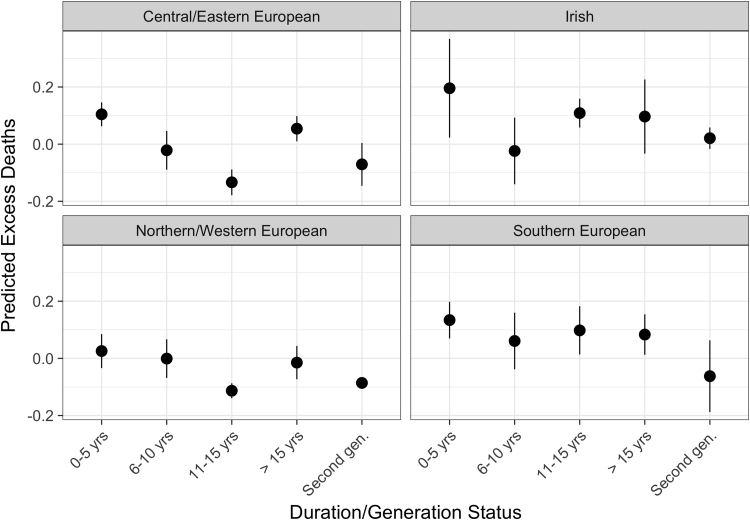
Fig. 2 plots the predicted rates of excess childhood mortality for each duration category and also includes estimates for second-generation immigrants. The model controls only for age variables and number of children born, in order to descriptively portray the trajectories. Each group appears to show improvement in childhood mortality outcomes with duration of residence in the United States, though to varying degrees and not linearly. For each group, the second generation had lower rates of childhood mortality than first generation immigrants. Looking at unadjusted individual-level rates, second-generation immigrants from Northern and Western Europe (-.13) and Central and Eastern Europe (-.10) had lower rates of excess childhood mortality than the U.S.-born white population (-.09). Only second-generation Irish immigrants failed to converge to the rates of the U.S.-born white population, but the 0 predicted excess deaths was significantly better than the rate of the U.S.-born black population.
Fig. 2.
Excess childhood mortality by duration of residence and generation. Graphed point represents predicted value and lines represent 95% confidence intervals. Includes controls for age, age-squared, and number of children born.
5. Discussion
This analysis contributes two unique empirical findings to research on immigration, race, and health in the early 20th century. First, it finds inequalities in childhood mortality between immigrants from different European regions, relative to U.S.-born whites. Some of these differences appear related to sending-country mortality differences, human capital, and ability to assimilate. However, the patterns of mortality match up relatively well with the documented boundaries between “whites” and other groups during this period. Immigrants from Ireland and Southern, Central, and Eastern Europe—who had the highest rates of childhood mortality among immigrant groups included in this study—were often marginalized as they arrived to the United States in greater numbers. In contrast, older immigrant cohorts from Northern/Western Europe often had easier paths to assimilation, in part because of a racial discourse that placed them firmly at the top of the ethno-racial hierarchy.
Second, this analysis finds variation in how childhood mortality patterns changed with duration of residence in the United States. Whereas contemporary immigrants often arrive healthier than the U.S.-born population and experience worsening outcomes with duration of residence, the opposite was true for European immigrants as measured by childhood mortality rates. Many new immigrant groups had higher rates of excess childhood mortality than their U.S-born counterparts—with Northern/Western Europeans as the exception—but outcomes generally improved with duration of residence or among the second generation. The “duration effect” was strongest for Central and Eastern Europeans, who came from origin countries with relatively high mortality and also saw smaller negative effects of urban residence.
At first glance, differences in context make the two eras difficult to compare. Immigrants in the early 1900s died primarily from infectious diseases, in contrast with the chronic conditions of today. The corresponding risk factors also differed in ways that made changing health behaviors associated with acculturation less salient to overall health and mortality outcomes. However, there are a number of theoretical implications in the above findings. First, they suggest the selection-acculturation framework used to explain contemporary immigrant health patterns is, at minimum, not generalizable to all contexts.
Beyond that, I argue the two eras can be compared by drawing on sociological insights about immigration and race that direct attention further “upstream” to the social conditions that shape post-migration life in different sociohistorical contexts. If researchers are interested in why today's new immigrants arrive relatively healthy, or why health seems to deteriorate after migration, there are multiple levels of causal questions that can be addressed. Health scholars have increasingly become interested in how social conditions—such as socioeconomic status and systemic racism—can act as a “cause of causes” or “risks of risks” for disease and mortality, even as the more proximal risk factors and linking mechanisms change (Link and Phelan, 1995, Link and Phelan, 1996, Lutfey and Freese, 2005, Phelan and Link, 2015, Phelan et al., 2010). Examining the health and mortality outcomes of European immigrant groups in 1910 provides a case for looking beyond the immediate mechanisms often associated with immigrant health trajectories—behavioral change, experiences of discrimination, access to care, etc.—to the upstream context of reception that shapes and institutionalizes group boundaries and distributes exposure to proximate mechanisms.
The empirical patterns of childhood mortality for European immigrants in 1910 are relatively unsurprising when considered in sociohistorical context. Between-group outcomes differentials for new immigrants correspond with the social hierarchy that has been described in a broad sociological and historical literature (Brodkin, 1998, Jacobson, 1999, Lieberson, 1980, Roediger, 2006). This hierarchy likely shaped exposure to risks—such as unsanitary urban environments, discrimination experiences, and barriers to economic opportunity—that affected a variety of health outcomes. The apparent improvement in health associated with duration of residence—and into the second generation—also corresponds with pathways of assimilation and upward mobility that were available to European immigrants during this period. Although there is debate about the brightness of boundaries between native-born whites and European immigrants (Fox & Guglielmo, 2012), the literature is clear that boundaries blurred into the middle of the 20th century.
Similarly, if the post-1965 wave of immigrants experience “health deterioration” in certain contexts, their outcome patterns are relatively unsurprising in light of literature about the contemporary context of reception. For instance, contemporary migrants no longer uniformly have access to the same linear pathway to socioeconomic and ethno-racial incorporation as early European immigrants. Rather, intersections of race, settlement location, and socioeconomic circumstances result in segmented trajectories, in which outcomes, including health, may not improve or may deteriorate after migration.
There are of course limitations to this historical comparison. First, the measure of childhood mortality used was only calculable from the 1910 Census sample, and the conclusions drawn are limited by the cross-sectional analysis. Although duration of residence was used as a proxy for post-migration changes, disentangling cohort, period, and duration effects is important when inferring trajectories of health patterns (Teitler, Martinson, & Reichman, 2015). Longitudinal linked data or multi-year comparisons in future research would allow for a more valid operationalization of post-migration health trajectories. Second, this study's ability to account for socioeconomic differences was limited. Duncan's Socioeconomic Index (SEI) was the best-available measure, but disaggregated indicators of educational attainment and earnings could provide a more complex picture. Finally, the dependent variable is an approximate estimate of childhood mortality that lacks detail about the age or cause of death. Although childhood mortality rates were interpreted as an outcome of the parent's generation, in part because many childhood deaths occured within the first year of life, additional research using other disease and mortality indicators could confirm or contradict the results presented here.
Despite limitations, comparison across contexts of reception is important for moving analyses of immigrant health upstream. Scholars of health have increasingly argued that risk factors for disease are themselves distributed by social conditions and institutional configurations. Further analysis of the institutional and structural context of reception may answer lingering questions about selection, acculturation, and the “paradox.” This broad perspective does not omit questions about health behaviors, social ties, and other proximate determinants of immigrant health. Rather, it shifts attention to social conditions of the context of reception in which exposure to risk factors and disease occurs.
Appendix
Table A.1.
Origin Groupings by Birthplace, First-Generation Immigrants.
| Northern/Western European | Central/Eastern European | Southern European | Irish | ||||
|---|---|---|---|---|---|---|---|
| Belgium | 72 | Austria | 1964 | Greece | 25 | Canada | 59 |
| Denmark | 228 | Bulgaria | 1 | Italy | 2010 | Ireland | 1708 |
| England | 1020 | Czechoslovakia | 29 | Malta | 1 | ||
| Finland | 204 | Eastern Europe, ns | 2 | Portugal | 115 | ||
| France | 131 | Hungary | 796 | Spain | 20 | ||
| Germany | 3348 | Lithuania | 4 | ||||
| Iceland | 2 | Other USSR/Russia | 2735 | ||||
| Lapland, n.s. | 1 | Poland | 129 | ||||
| Luxembourg | 4 | Romania | 72 | ||||
| Netherlands | 164 | Yugoslavia | 8 | ||||
| Norway | 512 | ||||||
| Scotland | 340 | ||||||
| Sweden | 1034 | ||||||
| Switzerland | 149 | ||||||
| Wales | 89 | ||||||
References
- Abdulrahim S., Baker W. Differences in self-rated health by immigrant status and language preference among Arab Americans in the Detroit Metropolitan Area. Social Science & Medicine. 2009;68(12):2097–2103. doi: 10.1016/j.socscimed.2009.04.017. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D., Sanchez-Vaznaugh E.V., Viruell-Fuentes E.A., Almeida J. Integrating social epidemiology into immigrant health research: A cross-national framework. Social Science & Medicine. 2012;75(12):2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- Akresh I.R., Do D.P., Frank R. Segmented assimilation, neighborhood disadvantage, and Hispanic immigrant health. SocialScience & Medicine. 2016;149:114–121. doi: 10.1016/j.socscimed.2015.12.013. [DOI] [PubMed] [Google Scholar]
- Alba R.D., Logan J.R., Stults B.J., Marzan G., Zhang W. Immigrant groups in the suburbs: A reexamination of suburbanization and spatial assimilation. American Sociological Review. 1999;64(3):446–460. [Google Scholar]
- Allen J.D., Caspi C., Yang M., Leyva B., Stoddard A.M., Tamers S.…Sorensen G.C. Pathways between acculturation and health behaviors among residents of low-income housing: the mediating role of social and contextual factors. Social Science & Medicine. 2014;123:26–36. doi: 10.1016/j.socscimed.2014.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antecol H., Bedard K. Unhealthy assimilation: Why do immigrants converge to american health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Blue L., Fenelon A. Explaining low mortality among usimmigrants relative to native-born Americans: The role of smoking. International Journal of Epidemiology. 2011;40(3):786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodkin K. Rutgers University Press; 1998. How jews became white folks and what that says about race in America. [Google Scholar]
- Brown T.H. Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces. 2018 [Google Scholar]
- Camacho-Rivera M., Kawachi I., Bennett G.G., Subramanian S. Revisiting the hispanic health paradox: The relative contributions of nativity, country of origin, and race/ethnicity to childhood asthma. Journal of Immigrant and Minority Health /Center for Minority Public Health. 2015;17(3):826–833. doi: 10.1007/s10903-013-9974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho Y., Frisbie W.P., Hummer R.A., Rogers R.G. Nativity, duration of residence, and the health of hispanic adults inthe United States. International Migration Review. 2004;38(1):184–211. [Google Scholar]
- David R.J., Collins J.W. Differing birth weight among infants of U.S.-Born blacks, African-Born blacks, and U.S.-born whites. New England Journal of Medicine. 1997;337(17):1209–1214. doi: 10.1056/NEJM199710233371706. [DOI] [PubMed] [Google Scholar]
- Dillingham W.P. U.S.Government Printing Office; 1911. Dictionary of Races or Peoples. [Google Scholar]
- Dubowitz T., Bates L.M., Acevedo-Garcia D. The Latino health paradox: Looking at the intersection of sociology and health. In: Bird C., Conrad P., Fremont A., Timmermans S., editors. Handbook of medical sociology. Sixth. Vanderbilt University Press; Nashville: 2010. pp. 106–123. [Google Scholar]
- Dubowitz T., Smith-Warner S.A., Acevedo-Garcia D., Subramanian S., Peterson K.E. Nativity and duration of time in the United States: Differences in fruit and vegetable intake among low-income postpartum women. American Journal of Public Health. 2007;97(10):1787–1790. doi: 10.2105/AJPH.2005.074856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan O.D. A socioeconomic index for all occupations. In: Reiss J. Jr, editor. Occupations and social status. Free Press of Glencoe; New York: 1961. pp. 109–138. [Google Scholar]
- Fenelon A. Revisiting the hispanic paradox in the United States: The role of smoking. Social Science & Medicine (1982) 2013;82:1–9. doi: 10.1016/j.socscimed.2012.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch B.K., Frank R., Vega W.A. Acculturation and acculturation stress: A social-epidemiological approach to mexican migrant farmworkers' health. International Migration Review. 2004;38(1):236–262. [Google Scholar]
- Finch B.K., Lim N., Perez W., Do D.P. Toward a population health model of segmented assimilation: The case of low birth weight in Los Angeles. Sociological Perspectives. 2007;50(3):445–468. [Google Scholar]
- Fox C., Guglielmo T.A. Defining America's racial boundaries: Blacks, Mexicans, and European Immigrants, 1890-1945. American Journal of Sociology. 2012;118(2):327–379. [Google Scholar]
- Frisbie W.P., Cho Y., Hummer R.A. Immigration and the health of asian and pacific islander adults in the United States. American Journal of Epidemiology. 2001;153(4):372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Gutmann M.P., Haines M.R., Frisbie W.P., Blanchard K.S. Intra-ethnic diversity in hispanic child mortality, 1890-1910. Demography. 2000;37(4):467–475. doi: 10.1353/dem.2000.0006. [DOI] [PubMed] [Google Scholar]
- Haines M.R., Preston S.H. The use of the census to estimate childhood mortality. Historical Methods. 1997;30(2):77. [Google Scholar]
- Hamilton T.G., Hummer R.A. Immigration and the health of U.S: Black adults: Does country of origin matter? Social Science & Medicine. 2011;73(10):1551–1560. doi: 10.1016/j.socscimed.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Hankin J.R., Wright E.R. Reflections on fifty years of medical sociology. Journal of Health and Social Behavior. 2010;51:S10–S14. doi: 10.1177/0022146510383840. (1 suppl) [DOI] [PubMed] [Google Scholar]
- Harris, W., (1913). Mortality Statistics 1910 (No. 11). U.S.Centers for Disease Control and Prevention.
- Hauser R.M., Warren J.R. Socioeconomic Indexes for occupations: A review, update, and critique. Sociological Methodology. 1997;27:177–298. [Google Scholar]
- Hodge R.W., Siegel P.M., Rossi P.H. Occupational prestige in the United States, 1925-63. American Journal ofSociology. 1964;70(3):286–302. [Google Scholar]
- Holmes S.M. An ethnographic study of the social context of migrant health in the United States. PLoS Med. 2006;3(10):e448. doi: 10.1371/journal.pmed.0030448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer R.A., Powers D.A., Pullum S.G., Gossman G.L., Frisbie W.P. Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignatiev N. Routledge; 2009. How the Irish became white. [Google Scholar]
- Jacobson M.F. Harvard University Press; 1999. Whiteness of a different color. [Google Scholar]
- Jasso, Massey D., Rosenzweig M., Smith J. Immigrant health: Selectivity and acculturation. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. 2004:227–266. [Google Scholar]
- John D.A., de Castro A., Martin D.P., Duran B., Takeuchi D.T. Does an immigrant health paradox exist among Asian Americans? Associations of nativity and occupational class with self-rated healthand mental disorders. Social Science & Medicine. 2012;75(12):2085–2098. doi: 10.1016/j.socscimed.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landale N.S., Oropesa R.S., Gorman B.K. Migration and infant death: Assimilation or selective migration among Puerto Ricans? American Sociological Review. 2000;65(6):888–909. [Google Scholar]
- Lariscy J.T., Hummer R.A., Hayward M.D. Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the hispanic paradox. Demography. 2015;52(1):1–14. doi: 10.1007/s13524-014-0357-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberson S. Univ of California Press; 1980. A piece of the pie: Blacks and White immigrants since 1880. [Google Scholar]
- Link B.G., Phelan J.C. Social conditions as fundamentalcauses of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Link B.G., Phelan J.C. Understanding sociodemographic differences in healththe role of fundamental social causes. American Journal of Public Health. 1996;86(4):471–473. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link, B.G., & Phelan, J.C. (2010). Social conditions as fundamental causes of health inequalities. In Handbook of Medical Sociology (pp. 3–17). Nashville.
- Lutfey K., Freese J. Toward some fundamentals of fundamental causality: Socioeconomic status and health in the routine clinic visit for diabetes. American Journal of Sociology. 2005;110(5):1326–1372. [Google Scholar]
- Osypuk T.L., Bates L.M., Acevedo-Garcia D. Another Mexican birthweight paradox? The role of residential enclaves and neighborhood poverty in the birthweight of Mexican-origin infants. Social Science & Medicine. 2010;70(4):550–560. doi: 10.1016/j.socscimed.2009.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A., Arias E. Paradox lost: Explaining the hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41(1):311–330. [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditionsas fundamental causes of health inequalities theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51:S28–S40. doi: 10.1177/0022146510383498. (1 suppl) [DOI] [PubMed] [Google Scholar]
- Portes A., Böröcz J. Contemporary immigration: Theoretical perspectives on its determinants and modes of incorporation. International Migration Review. 1989;23(3):606–630. [PubMed] [Google Scholar]
- Portes A., Rumbaut R.G. University of California Press; 2006. Immigrant America: A portrait. [Google Scholar]
- Portes A., Zhou M. The new second generation: Segmented assimilation and its variants. The Annals of the American Academy of Political and Social Science. 1993;530(1):74–96. [Google Scholar]
- Portes A., Fernandez-Kelly P., Haller W. Segmented assimilation on the ground: The new second generation in early adulthood. Ethnic and Racial Studies. 2005;28(6):1000–1040. [Google Scholar]
- Read J.G., Emerson M.O. Racial context, black immigration and the U.S. black/white health disparity. Social Forces. 2005;84(1):181–199. [Google Scholar]
- Read J.G., Emerson M.O., Tarlov A. Implications of black immigrant health for U.S. racial disparities in health. Journal of Immigrant Health. 2005;7(3):205–212. doi: 10.1007/s10903-005-3677-6. [DOI] [PubMed] [Google Scholar]
- Restifo S.J., Roscigno V.J., Qian Z. Segmented assimilation, split labor markets, and racial/ethnic inequality the case of early-twentieth-century New York. American Sociological Review. 2013;78(5):897–924. [Google Scholar]
- Reynolds M.M., Chernenko A., Read J.G. Region of origin diversity in immigrant health: Moving beyond the Mexican case. Social Science & Medicine. 2016;166:102–109. doi: 10.1016/j.socscimed.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riis J.A. Penguin; 1901. How the other half lives: Studies among the tenements of New York. [Google Scholar]
- Riosmena F., Everett B.G., Rogers R.G., Dennis J.A. Negative acculturation and nothing more? Cumulative disadvantage and mortality during the immigrant adaptation process among latinos in the United States. International Migration Review. 2015;49(2):443–478. doi: 10.1111/imre.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roediger D.R. Basic Books; 2006. Working toward whiteness: How America's immigrants became white: The strange journey from Ellis Island to the Suburbs. [Google Scholar]
- Ruggles, S., Alexander, T., Genadek, K., Goeken, R., Schroeder, M., & Sobek, M. (2010). Integrated Public Use Microdata Series: Version 5.0 [Machine-readable database]. Minneapolis: University of Minnesota.
- Ruiz J.M., Steffen P., Smith T.B. Hispanic mortality paradox: A systematic review and meta-analysis of the longitudinal literature. American Journal of Public Health. 2013;103(3):e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumbaut R.G. The crucible within: Ethnic identity,self-esteem, and segmented assimilation among children of immigrants. International Migration Review. 1994;28(4):748. [Google Scholar]
- Rumbaut R.G. Assimilation and its discontents: Between rhetoric and reality. International Migration Review. 1997;31(4):923–960. [PubMed] [Google Scholar]
- Singh G.K., Hiatt R.A. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, andcause-specific mortality of native-born and foreign-born populations inthe United States, 19792003. International Journal of Epidemiology. 2006;35(4):903–919. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- Singh G.K., Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Singh G.K., Rodriguez-Lainz A., Kogan M.D., Singh G.K., Rodriguez-Lainz A., Kogan M.D. Immigrant health inequalities in the United States: use of eight major National Data Systems. The Scientific World Journal. 2013:e512313. doi: 10.1155/2013/512313,/%002010.1155/2013/512313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepick A., Stepick C.D. The complexities and confusionsof segmented assimilation. Ethnic and Racial Studies. 2010;33(7):1149–1167. doi: 10.1080/01419871003624076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Jun H.-J., Kawachi I., Wright R.J. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: Evidence for a nativity advantage. American Journal of Public Health. 2009;99(4):690–697. doi: 10.2105/AJPH.2007.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitler J.O., Hutto N., Reichman N.E. Birthweight of children of immigrants by maternal duration of residence in the United States. Social Science & Medicine. 2012;75(3):459–468. doi: 10.1016/j.socscimed.2012.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitler J., Martinson M., Reichman N.E. Does life in the united states take a toll on health? Duration of residence and birthweight among six decades of immigrants. International Migration Review. 2015:1–30. doi: 10.1111/imre.12207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turra C.M., Elo I.T. The impact of salmon bias on the hispanic mortality advantage: New evidence from social security data. Population Research and Policy Review. 2008;27(5):515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Manual X: Indirect Techniques for Demographic Estimation. (1982). (No. Sales No. E.83.XIII.2). New York.
- Wyman M. Cornell University Press; 1996. Round-trip to America: The immigrants return to Europe; pp. 1880–1930. [Google Scholar]
- Yoo H.C., Gee G.C., Takeuchi D. Discrimination and health among Asian American immigrants: Disentangling racial from language discrimination. Social Science & Medicine. 2009;68(4):726–732. doi: 10.1016/j.socscimed.2008.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]