Abstract
Aluminum (Al) is widely found in the nature. Although the relation between Al and neurodegenerative diseases is still controversial, Al is related with many brain diseases including Alzheimer's disease, Parkinson's disease, and multiple sclerosis. Al exposure occurs mainly through environment, occupational, and dietary factors for humans. Al exposure with diet can be through foods, food additives, water, and contamination of Al equipment/utensils. The aim of this review is to summarize various hypotheses, which link Al and neurodegeneration, and to determine the roles of Al exposure through different sources including diet, environment, and occupation. Future studies should be done in vulnerable subgroups of population including children, patients receiving antacid or Al-containing pharmeteucials on a daily basis, patients with reduced renal function, and patients on parenteral nutrition regimens that are likely to be affected by possible adverse health effects of Al. In addition, gender, age, and Al interactions need to be determined. One of the most important challanges in future epidemiological studies is to determine which variables should be controlled. In addition, experimental studies should be more focused and translational. In this context, exposure dose, dose–response effects, and time lapse between exposures and cognitive assessments are very important.
Keywords: Aluminum, Alzheimer's disease, multiple sclerosis, neurodegenerative diseases, Parkinson's disease
INTRODUCTION
Aluminum (Al), the third most commonly found element in the nature after oxygen and silicon, composes nearly 8% of the earth crust. Although Al is found commonly in the environment, there is no known essential role of Al in the living systems. In general, Al is not essential for the growth, reproduction, and sustainability of life in terms of humans and animals.[1] Al is widely used in the fields of medicine, pharmacy, food technology, and cosmetics. Al is also commonly used in food preparation equipment and kitchen utensils.[2] Al exposure occurs mainly through environment, occupational, and diet for humans. Al exposure with diet can be through foods, food additives, water, and contamination of Al equipment/utensils.[1] Although the total intake of Al considerably varies upon country, place of residence, and diet composition, nearly 10 mg of Al is taken to the human body on a daily basis; 9.6 mg of this amount is taken from foods, 0.1–0.4 mg of this amount is taken from kitchen utensils and packaging, and 5 μg of this amount is taken from air.[3] Al absorption is generally less than Al intake, and approximately 95% of the total Al is excreted through feces. Indeed, Al absorption may vary from 0.01% to 1% of the total Al intake.[4,5] It has been reported that citrate may increase Al absorption if it is present in enough amount in the gastrointestinal tract to compete with other binding ligands for Al.[6] Other short-chain carboxylic acids such as acetate, oxalate, lactate, malate, tartrate, gluconate, ascorbate, and carbonate have also been shown to increase Al absorption in some animal studies, although not as effective as citrate.[7,8,9,10,11] This may be due to formation of more stable complex between Al and citrate than other ligands.[12] Contrary to this, it has been reported that the increased diet intake of the compounds containing silicone decreases the absorption of Al and facilitates the excretion of Al.[12] In addition to this, flouride has also been shown to be capable of elimination of Al in urine and feces.[6] Iron affects the absorption of Al and the accumulation of Al in the brain. Therefore, it has been shown that Al absorption is generally higher at low iron levels. Adequate iron stores may help to reduce the intestinal absorption of Al since iron may compete with Al to bind to the transferrin. The calcium status, like iron, also affects the absorption and accumulation of Al. In animal studies, calcium deficiency in the diet has been shown to increase the rate and amount of Al absorption.[13,14] Vitamin D supplementation may increase Al content in the muscles and hearts. Besides, the parathyroid hormone can increase the absorption of Al by situmilating renal synthesis of 1,25-dihydroxyvitamin D3.[15] Hence, Al bioavailability is highly dependent on individual differences. The necessity of controlling these differences in both experimental and epidemiological studies as confounding variables should be considered.[16] The total body load of Al is approximately 30–50 mg. Only 1% of the total body Al accumulates in the brain.[17,18] Although brain is an important organ that accumulates Al in terms of exposure, it contains less Al than other tissues.[12,18] The gray matter of the brain contains twice as much Al as white matter.[19] In addition to this, it is also reported that Al accumulates in human brains with increasing age.[20,21] Although the mechanisms of how Al enters the brain are not fully known, it is thought that Al passes through the blood–brain barrier through transferrin and accumulates in the area of the brain cortex that is rich in transferrin receptors.[17,22]
Although there is lots of evidence implicating that Al in the progression of events leads to neurodegenerative diseases, some of the evidence remains controversial. However, it is widely accepted that Al is a recognized neurotoxin, which could cause neurodegeneration.[23] Al affects >200 important biological reactions and causes negative effects on central nervous system. Among these reactions affected by Al, there are mechanisms effective on brain development, such as axonal transport, neurotransmitter synthesis, synaptic transmission, phosphorylation or de-phosphorylation of proteins, protein degradation, gene expression, peroxidation, and inflammatory responses.[24] Al can bind to histone-DNA complex and induce conformational changes of chromatin and induce topological changes of DNA.[25,26] Al can also alter gene expression by inducing decreased expression of neurofilament and tubulin, altered expression of genes of neurofilament, amyloid precursor protein (APP), and neuron-specific enolase, decreased expression of transferrin receptor, altered expression of RNA polymerase I, altered expression of oxidative stress marker genes (SOD1, glutathione reductase, etc.), and altered expression of β-APP secretase.[27,28,29,30,31,32] In addition to these effects of Al, it has been suggested that Al can affect cellular functions such as inhibiting the activity of hexokinase, phosphofructokinase, and glucose-6-phosphate dehydrogenase and causing mitochondrial dysfunction and depletion of adenine-triphosphate (ATP).[33,34,35,36,37] The aforementioned phosphorylation or de-phosphorylation reactions that can be affected by Al are inhibiting the activity of protein phosphatase and dephosphorylation of tau, increasing the activity of protein kinase C and cytoskeleton proteins, and inducing nonenzymatic phosphorylation of tau.[38,39,40,41] Al can also cause an abnormal accumulation of proteins by causing the accumulation of tau protein in neuroblastoma cells, neurofibrillary degeneration in vivo, and the accumulation of amyloid β protein (AβP) in vivo.[42,43,44,45]
While in vivo and in vitro studies have shown that Al has negative effects on the central nervous system, the results are conflicting. Studies in Al welders found that Al may cause memory and attention task deficits, but on the other hand, there are studies which showed that occupational Al exposure does not lead to a cognitive or motor performance decline.[46,47,48,49] In addition to this occupational Al exposure studies, cognitive deficit was demonstrated in the studies that were made with dialysis patients after administration of the Al chelator.[50,51] On the contrary, Jackson et al.[52] reported no significant differences on cognitive tests in dialysis patients. These studies show that more studies have to be done for determining the relationship between Al and neurological disorders. Although the relation between Al and neurodegenerative diseases is still controversial, Al is related with many brain diseases including Alzheimer's disease (AD), Parkinson's disease (PD), and multiple sclerosis (MS) [Figure 1].[24,53,54,55,56]
Figure 1.
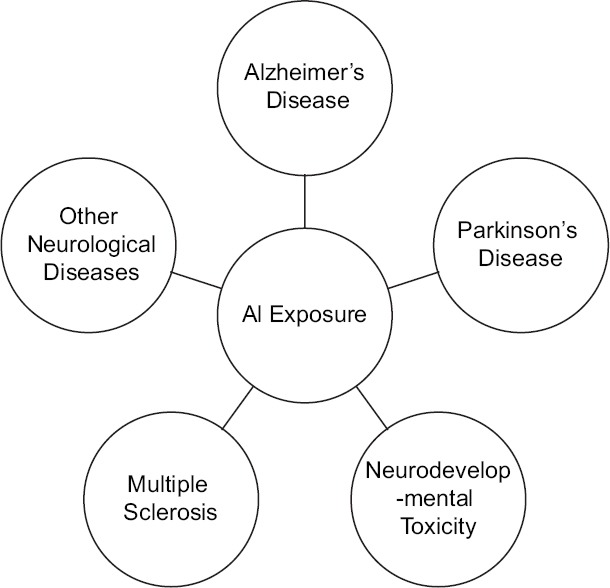
Summary of neurotoxicity of aluminum
In light of these information, the aim of this review is to summarize various hypotheses, which link Al and neurodegeneration, and to determine the roles of Al exposure through different sources including diet, environment, and occupation.
Aluminum and neurological disorders
Alzheimer's disease
AD is characterized by a neurological progressive impairment affecting several cognitive domains, behavior, and personality.[57] AD is accompanied by changes in cerebral functions as a result of biochemical incidents, each of which is related with each other. These cerebral dysfunctions result in difficulties in receiving/processing new information, difficulties in doing previously known activities/works, confusion, not participating in social activities, loss of memory, and personality changes.[58] Typical neuropathological signs of the disease are intracellular neurofibrillary tangles (hyper phosphorylation of tau protein), deposition of extracellular senile plaques (hyper phosphorylation of AβP, optimal losses of synapses and neurons in hippocampal and cerebral cortical regions, cortical and subcortical atrophy, and cerebrovascular amyloids.[54,59,60] Early-onset AD is related to familial gene mutations, which results in increased secretion of neurotoxic AβP. Apolipoprotein E susceptibility gene is a risk factor in AD. The late-onset AD, detected in 85%–95% of the cases of AD, is not related with any gene mutation.[61]
The etiological factors of AD are not exactly known. However, it is thought that genetic factors, oxidative stress, infectious factors, and environmental factors are playing role in AD.[60] As there is no sufficient genetic information about AD, it is thought that environmental factors interact with other factors and provide a basis for the formation of this disease. Al is one of these environmental factors.[62] The hypothesis, stating that Al was one of the environmental factors in the pathogenesis of AD, was named as “Al hypothesis,” based on various neuro-toxicological, analytical, and epidemiological data found in the 1960s.[63,64,65] The beginning of the hypothesis, stating that Al was included in the etiology of AD, is revealed by observing the neurofibrillary degeneration after the intracerebral injection of Al into rabbit's brain.[63] The increasing Al levels were reported in 1973 in postmortem brain samples of people with AD and they were related with AD.[64]
The role of Al in AD was related to different incidents, independent from each other. These are as follows:
High concentrations of Al increase amyloid aggregation and deposition, the main feature of the neuropathology of AD[66]
In vitro and in vivo, by means of pro-inflammatory transcription factor nuclear factor-kappa B (NF-kB), Al increases the inflammatory signalization, one of the main features of the brain with AD[20,67]
Al-induced mRNAs and microRNAs (miRNAs) show similarity with mRNAs and miRNAs[68]
In transgenic animal models with AD, dietary Al increases the formation of pathological determinants such as lipid peroxidation, oxidative stress, apoptosis, and gene expression deficiencies[44,69,70]
The disorders observed in AD such as chromatin compression, impaired energy usage, and impaired signalization including chemical messengers such as ATP were also detected in cells exposed to Al or in animal models with AD[71,72]
In the studies, the amount of Al in water was related to the incidence of AD.[20,73,74]
Although Al is not known to be neurotoxin, there is still no consensus on the relationship between Al and AD, the results from different studies are not consistent.[7] Some studies show that aluminum promotes precursor expression of the AβP, increases the levels of the B-40 and B-42 fragments in the brain, and boosts the aggregation of the AβP,[44,75,76] whereas the results previously obtained for the Aβ pathways cannot be reproduced in vivo.[77,78] Although experimental studies have produced inconsistent results on the relationship between Al and AD, epidemiological studies provide important consistent results. A recent meta-analysis by Wang et al.[57] examined 8 epidemiological studies to determine exposure to Al and association with AD. A significant correlation was found between Al exposure and AD risk according to the meta-analysis of cohort studies in which a total of 10,567 individuals were included and exposed to Al from drinking water and occupational exposure, with follow-up times ranging from 8 to 48 years. McLachlan et al.[79] found a dose–response correlation between an increasing concentration of Al in the drinking water (100 mg/L or greater Al) and a higher risk of developing AD. There are several epidemiological studies of drinking water and AD risk that have also shown dose–response effects.[73,80]
Parkinson's disease
PD, the widely observed neurodegenerative disorder after AD, is characterized with selective death of neurons in substantia nigra. By leading genetic and/or acquired disorders in ubiquitin-proteasome system, it can cause the deposition of ubiquitin-added proteins and neuronal deaths.[81] It has been suggested that several molecular mechanisms including mitochondrial dysfunction, impairment of protein quality pathways, oxidative/nitrative stress, microglia activation, and inflammation are responsible for neuronal death in PD pathogenesis.[82,83] In addition to the neuronal loss, the other neuropathological hallmark of PD is the presence of Lewy bodies in the surviving neurons. These neurons are eosinophilic cytoplasmic inclusions containing aggregates of protein such as α-synuclein (α-syn).[81]
PD is a neurodegenerative disorder, affecting speaking and motor abilities of the patient, which is characterized with tremors in the face, hands and jaw, muscle rigidity, and slow physical activities. PD occurs as a result of the decrease of stimuli by basal ganglia in motor cortex, depending on the death of neurons in globus pallidus and substantia nigra, which normally synthesizes and releases epinephrine and dopamine.[81] PD can progress with head injuries/traumas, encephalitic virus, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP, contaminant including drugs such as heroin) and exposure to some pesticides.[81] As Al+3 toxicity causes AD-type dementia in some patients with PD, it is thought that Al is playing a role in PD.[81] Moreover, catecholamine neurotransmitters and catechol parts of epinephrine and dopamine are important binding parts of Al+3. Although epinephrine and dopamine are weak Mg+2 binders in millimolar levels, they bind Al+3 in nanomolar levels. It was detected that there were high Al+3 and Fe+3 levels indicating the death of neurons in neuromelanin granules and Lewy bodies of substantia nigra and locus coeruleus (the blue part of brain stem in which there are neurons including neuro-epinephrine) parts in the brains of patients with PD.[84] As a result of iron metabolism impaired by Al+3, high levels of iron accumulate in the neurons of patients with PD, but there is no increase observed in the levels of ferritin. Consequently, oxidative damage occurs, which causes neural deaths in substantia nigra and other parts of the brain affected from PD.[84]
The relationship between PD and Al has also been demonstrated in gastric ulcer patients due to the use of Al-containing antacids.[85] Another indirect evidence between Al and PD is the ability of Al to activate the monoamine oxidase B. This enzyme increases with age and PD.[86] In addition, monoamine oxidase B may promote α-syn fibril formation.[87] It is suggested that this situation may explain the relationship between neurotoxic metals and PD.[88] Activation of the NF-kB transcription factor and triggering of inflammatory processes have been found to occur synergistically after simultaneous treatment of experimental animals with a dopaminergic neurotoxin, MPTP, and low-level Al in drinking water.[22] Yasui et al.[89] found that Al concentration in the substantia nigra, caudate nucleus, and globus pallidus was higher in PD brains and significantly higher in gray matter and the basal ganglia. In parallel, Good et al.[90] found increased Al levels in the neuromelanin granules of two of three PD cases.
Multiple sclerosis
MS is a chronic, immune-mediated, and demyelinating disease of the central nervous system, the etiology of which has not been known yet. Iron concentrations in urine were found high in secondary progressive, recurrent, and recovering patients with MS.[53] Moreover, it was detected that Al concentrations in the urine of these patients also increased. The Al excretion levels of these patients were found same as the individuals who got metal chelation therapy. Increased iron concentrations in the urine show impaired iron metabolism in patients with MS. Al excretion levels also resemble Al intoxication. This situation indicates that Al can be an environmental factor in MS etiology.[53] In addition, use of Al adjuvant-containing vaccines has also been associated with increased incidence of MS.[91,92]
Dialysis encephalopathy
For individuals with chronic kidney disease, there is a bilateral risk associated with Al. First, these patients are exposed to Al as part of the treatment process, and second, their ability to excrete Al from the body is reduced because of the disease.[93] Chronic kidney disease patients also have difficulty to excrete phosphate from the body. The high blood phosphate levels of these patients increase the risk of death from bone and heart diseases. Al hydroxide began to be used as a phosphate binder in patients with chronic kidney disease to limit phosphate absorption in the 1960s.[93] The use of Al-containing phosphate binders, especially with alkalinizing citrate solution (Shohl's solution), has been found to be more risky to form Al citrate complex which consequently increase the absorption of Al.[94,95] Dialysis encephalopathy, first described in 1972, has emerged as a complication of prolonged hemodialysis exposure.[96] Patients with dialysis encephalopathy have difficulty in speaking (dysarthria), movement planning disorder (dyspraxia), unconsciousness and psychosis following ataxia, personality changes, myoclonic movements, electroencephalographic abnormalities, convulsions, and dementia.[93]
The mechanisms of dialysis encephalopathy are not exactly known. Al passes through the blood–brain barrier through the transferrin and accumulates in the area of the brain cortex that is rich in transferrin receptors. This region where the distribution of pyramidal neurons is made requires a high degree of Fe for the synthesis of respiratory chain enzymes. The damage in this area is thought to have resulted in neuropathy.[97]
It was found that Al levels in brain, muscle, and other tissues of dialysis encephalopathy patients were high. Serum Al levels >80 μg/L have been associated with dialysis encephalopathy.[98] In addition, cerebral cortical Al concentrations of patients with dialysis encephalopathy were reported as 10–25 μg/g dry brain weight.[97] The Al content of the dialysis fluids used in many cases with encephalopathy was determined to be >200 μg/L.[99] Nowadays, the exposure of dialysis patients to Al is the minimum, as the Al level of dialysis fluid in the majority of dialysis centers is <10 μg/L.[100]
Aluminum exposure with diet
Exposure to Al in humans is mainly through diet. Al exposure to the diet can be through contamination of foods, food additives, water, and Al kitchenwares.[1] The amount of Al in foods differs according to their Al content or the interaction of nutrients with the Al kitchenwares in the process of storage, preparation, and cooking of foods.[40] Although the amount of Al in the soil is high (3%–10%), many plants contain low amounts of Al.[97] When the pH of the soil is <4.5–5.0, Al is dissolved in water and absorbed by the root of the plant.[101] The amount of Al in animal-derived foods depends on the low amount of Al in animal feed and on the limited availability of Al to animals in animal-derived products such as eggs and milk. As a result, most of the animal-derived foods contain <1 μg/g Al.[97]
Except for foods and additives including Al, Al exposure with diet can increase due to storage of foods in Al containers and Al cookware (pot, pan, tray, coffeepot, etc.) used in food preparation and cooking and contact with folios.[1] Although the amount of Al exposed as a result of the consumption of foods prepared in Al cookware was lower than the amount of Al that was taken from other sources, in case of frequent usage of Al cookware, the Al migration to food from these cookware increased significantly.[1] Moreover, factors such as cooking time and temperature, the composition of food, pH value, and the existence of other substances (organic acids, salt, and other ions) also affect Al migrations to foods. Under normal circumstances, the Al migration from substances contact with the food constitutes a small part of the total dietary exposure. In addition, the use of Al pots, plates, or folios with foods such as apple, tomato, and salted fish increases the Al migrations to these foods. Furthermore, it was reported that the use of Al plates and trays, especially with acidic foods such as tomato, pickle, and vinegar, caused the increase of Al migrations.[1,102] The provisional tolerable weekly intake level of Al was reevaluated by the Joint Expert Committee on Food Additives in 2011 in light of new toxicological studies. According to this evaluation, the provisional tolerable weekly intake level, previously published as 1 mg/kg body weight (BW), was changed as 2 mg/kg BW.[103]
Aluminum exposure from environment
Although Al is found in the earth crust in a large amount, the majority of natural water contain very small amounts of dissolved Al (<10 μg/L) and marine water contain 1 μg/L of Al. Al in marine water generally accumulates in unicellular algae.[97] The development of modern industrial technologies and the spreading of chemicals into the atmosphere may cause acid rains.[104] When natural water acidify due to acid rain or when natural water are treated with Al sulfate to obtain drinking water, the amount of Al in natural water increases.[97] Strong mineral acids such as sulfur and nitrogen oxalic acid in acid rain can cause mobilization of Al by dissolving it from the soil.[97] The amount of acid in lakes and rivers acidified by acid rain can reach up to 700 μg/L. This level is generally regarded as a toxic level for fish.[97] In addition, natural events such as soil erosion, fragmentation of rocks, and volcanic activity result in the removal and redistribution of Al in other environmental components, including water, air, and biota.[102] The Al concentration of air varies between 20 and 500 ng/m3 in rural areas and 1000 and 6000 ng/m3 in urban areas. Humans are exposed to environmental alumina at a concentration of 200 ng/m3 and a particle size of <5 μm. A person with a normal ventilation volume of 20 m3 is 40 μg of Al breath/day.[99]
Occupational aluminum exposure
With the increasing use of Al in everyday life and industry, Al exposure has become inevitable. Potential Al exposure is expected to be higher in people working in certain occupational groups (such as Al refining and metal industries, printing and publishing, and automotive business).[19]
Occupational exposure to Al particles during the production of Al dusts reached 100 mg/m3 in the 1950s.[105] However, the exposure levels for Al dust production in the 1990s were reported to be 5–21 mg/m3 and the exposure levels for the production of Al fuels were reported to be 1–4 mg/m3.[106] During Al welding process, 0.2–5 mg/m3 Al is produced. Powder production and welding often lead to occupational Al exposure at high levels. Cognitive deficits, attention deficits, learning and verbal or visual disorders, and “concept formation” problems have been reported in workers exposed to occupational Al exposure.[1]
CONCLUSION
It is well established that Al is a neurotoxic agent. However, the link of Al to the etiology of various serious neurological disorders such as AD remains still unclear. In spite of this uncertainty, a number of epidemiological reports concerning Al exposure and the risks of neurological disorders are available in the scientific literature. An important reason for this uncertainty is the ethical concerns of tests conducted in humans. Thus, many studies have been conducted on animals and animals have been exposed to Al throughout their lives so that the effects of Al can be fully observed in many of these studies. Al exposure should be kept to minimum since the potential effects on human health of Al are not fully understood. Future studies should be done in vulnerable subgroups of population including children, patients receiving antacids or Al-containing pharmeteucials on a daily basis, patients with reduced renal function, and patients on parenteral nutrition regimens that are likely to be affected by possible adverse health effects of Al. In addition, gender, age, and Al interactions need to be determined. One of the most important challanges in future epidemiological studies is to decide which variables should be controlled. In addition, experimental studies should be more focused and translational. In this context, exposure dose, dose–response effects, and time lapse between exposures and cognitive assessments are very important.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Domingo JL. Aluminium. In: Benjamin C, editor. Encyclopedia of Food Sciences and Nutrition. 2nd ed. Oxford: Academic Press; 2003. pp. 160–6. [Google Scholar]
- 2.Aronson JK. Meyler's Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. 15th ed. Amsterdam: Elsevier; 2006. Aluminium; pp. 97–105. [Google Scholar]
- 3.Vargel C. 1st ed. Oxford: Elseiver; 2004. Food Industry. [Google Scholar]
- 4.Moore PB, Day JP, Taylor GA, Ferrier IN, Fifield LK, Edwardson JA, et al. Absorption of aluminium-26 in Alzheimer's disease, measured using accelerator mass spectrometry. Dement Geriatr Cogn Disord. 2000;11:66–9. doi: 10.1159/000017216. [DOI] [PubMed] [Google Scholar]
- 5.Wilhelm M, Jäger DE, Ohnesorge FK. Aluminium toxicokinetics. Pharmacol Toxicol. 1990;66:4–9. doi: 10.1111/j.1600-0773.1990.tb00692.x. [DOI] [PubMed] [Google Scholar]
- 6.Glynn AW, Sparén A, Danielsson LG, Sundström B, Jorhem L. The influence of complexing agents on the solubility and absorption of aluminium in rats exposed to aluminium in water. Food Addit Contam. 2001;18:515–23. doi: 10.1080/02652030118639. [DOI] [PubMed] [Google Scholar]
- 7.Colomina MT, Gómez M, Domingo JL, Corbella J. Lack of maternal and developmental toxicity in mice given high doses of aluminium hydroxide and ascorbic acid during gestation. Pharmacol Toxicol. 1994;74:236–9. doi: 10.1111/j.1600-0773.1994.tb01104.x. [DOI] [PubMed] [Google Scholar]
- 8.Domingo JL, Gomez M, Llobet JM, Corbella J. Influence of some dietary constituents on aluminum absorption and retention in rats. Kidney Int. 1991;39:598–601. doi: 10.1038/ki.1991.70. [DOI] [PubMed] [Google Scholar]
- 9.Domingo JL, Gómez M, Sanchez DJ, Llobet JM, Corbella J. Effect of various dietary constituents on gastrointestinal absorption of Al from drinking water and diet. Res Commun Chem Pathol Pharmacol. 1993;79:377–80. [PubMed] [Google Scholar]
- 10.Domingo JL, Gómez M, Llobet JM, del Castillo D, Corbella J. Influence of citric, ascorbic and lactic acids on the gastrointestinal absorption of Al in uremic rats. Nephron. 1994;66:108–9. doi: 10.1159/000187777. [DOI] [PubMed] [Google Scholar]
- 11.Nestel AW, Meyers AM, Paiker J, Rollin HB. Effect of calcium supplement preparation containing small amounts of citrate on the absorption of aluminium in normal subjects and in renal failure patients. Nephron. 1994;68:197–201. doi: 10.1159/000188256. [DOI] [PubMed] [Google Scholar]
- 12.Krewski D, Yokel RA, Nieboer E, Borchelt D, Cohen J, Harry J, et al. Human health risk assessment for aluminium, aluminium oxide, and aluminium hydroxide. J Toxicol Environ Health B Crit Rev. 2007;10(Suppl 1):1–269. doi: 10.1080/10937400701597766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Provan SD, Yokel RA. Reduced intestinal calcium and dietary calcium intake, increased aluminum absorption, and tissue concentration in the rat. Biol Trace Elem Res. 1989;23:119–32. doi: 10.1007/BF02917183. [DOI] [PubMed] [Google Scholar]
- 14.Taneda M. Effect of aluminum on rat brain. Enhancement by calcium deficiency. Hokkaido Igaku Zasshi. 1984;59:312–37. [PubMed] [Google Scholar]
- 15.Moon J, Davison A, Bandy B. Vitamin D and Al absorption. CMAJ. 1992;147:1308–13. [PMC free article] [PubMed] [Google Scholar]
- 16.Colomina MT, Peris-Sampedro F. Aluminum and Alzheimer's disease. Adv Neurobiol. 2017;18:183–97. doi: 10.1007/978-3-319-60189-2_9. [DOI] [PubMed] [Google Scholar]
- 17.Yokel RA, McNamara PJ. Aluminium toxicokinetics: An updated minireview. Pharmacol Toxicol. 2001;88:159–67. doi: 10.1034/j.1600-0773.2001.d01-98.x. [DOI] [PubMed] [Google Scholar]
- 18.Priest ND. The biological behaviour and bioavailability of aluminium in man, with special reference to studies employing aluminium-26 as a tracer: Review and study update. J Environ Monit. 2004;6:375–403. doi: 10.1039/b314329p. [DOI] [PubMed] [Google Scholar]
- 19.Nayak P. Aluminum: Impacts and disease. Environ Res. 2002;89:101–15. doi: 10.1006/enrs.2002.4352. [DOI] [PubMed] [Google Scholar]
- 20.Walton JR. Chronic aluminum intake causes Alzheimer's disease: Applying Sir Austin Bradford Hill's causality criteria. J Alzheimers Dis. 2014;40:765–838. doi: 10.3233/JAD-132204. [DOI] [PubMed] [Google Scholar]
- 21.Shimizu H, Mori T, Koyama M, Sekiya M, Ooami H. A correlative study of the aluminum content and aging changes of the brain in non-demented elderly subjects. Nihon Ronen Igakkai Zasshi. 1994;31:950–60. doi: 10.3143/geriatrics.31.950. [DOI] [PubMed] [Google Scholar]
- 22.Bondy SC. Low levels of aluminum can lead to behavioral and morphological changes associated with Alzheimer's disease and age-related neurodegeneration. Neurotoxicology. 2016;52:222–9. doi: 10.1016/j.neuro.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Maya S, Prakash T, Madhu KD, Goli D. Multifaceted effects of aluminium in neurodegenerative diseases: A review. Biomed Pharmacother. 2016;83:746–54. doi: 10.1016/j.biopha.2016.07.035. [DOI] [PubMed] [Google Scholar]
- 24.Kawahara M, Kato-Negishi M. Link between aluminum and the pathogenesis of Alzheimer's disease: The integration of the aluminum and amyloid cascade hypotheses. Int J Alzheimers Dis. 2011;2011:276393. doi: 10.4061/2011/276393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Latha KS, Anitha S, Rao KS, Viswamitra MA. Molecular understanding of aluminum-induced topological changes in (CCG) 12 triplet repeats: Relevance to neurological disorders. Biochim Biophys Acta. 2002;1588:56–64. doi: 10.1016/s0925-4439(02)00133-3. [DOI] [PubMed] [Google Scholar]
- 26.Bharathi KS, Jagannatha Rao KS, Stein R. First evidence on induced topological changes in supercoiled DNA by an aluminium D-aspartate complex. J Biol Inorg Chem. 2003;8:823–30. doi: 10.1007/s00775-003-0484-1. [DOI] [PubMed] [Google Scholar]
- 27.Muma NA, Singer SM. Aluminum-induced neuropathology: Transient changes in microtubule-associated proteins. Neurotoxicol Teratol. 1996;18:679–90. doi: 10.1016/s0892-0362(96)00126-2. [DOI] [PubMed] [Google Scholar]
- 28.Parhad IM, Krekoski CA, Mathew A, Tran PM. Neuronal gene expression in Al myelopathy. Cell Mol Neurobiol. 1989;9:123–38. doi: 10.1007/BF00711449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oshiro S, Kawahara M, Mika S, Muramoto K, Kobayashi K, Ishige R, et al. Aluminum taken up by transferrin-independent iron uptake affects the iron metabolism in rat cortical cells. J Biochem. 1998;123:42–6. doi: 10.1093/oxfordjournals.jbchem.a021914. [DOI] [PubMed] [Google Scholar]
- 30.Lukiw WJ, LeBlanc HJ, Carver LA, McLachlan DR, Bazan NG. Run-on gene transcription in human neocortical nuclei: Inhibition by nanomolar Al and implications for neurodegenerative disease. J Mol Neurosci. 1998;11:67–78. doi: 10.1385/JMN:11:1:67. [DOI] [PubMed] [Google Scholar]
- 31.Lin R, Chen X, Li W, Han Y, Liu P, Pi R, et al. Exposure to metal ions regulates mRNA levels of APP and BACE1 in PC12 cells: Blockage by curcumin. Neurosci Lett. 2008;440:344–7. doi: 10.1016/j.neulet.2008.05.070. [DOI] [PubMed] [Google Scholar]
- 32.Luo Y, Niu F, Sun Z, Cao W, Zhang X, Guan D, et al. Altered expression of abeta metabolism-associated molecules from D-galactose/AlCl(3) induced mouse brain. Mech Ageing Dev. 2009;130:248–52. doi: 10.1016/j.mad.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Socorro JM, Olmo R, Teijón C, Blanco MD, Teijón JM. Analysis of aluminum-yeast hexokinase interaction: Modifications on protein structure and functionality. J Protein Chem. 2000;19:199–208. doi: 10.1023/a:1007055719926. [DOI] [PubMed] [Google Scholar]
- 34.Lai JC, Blass JP. Inhibition of brain glycolysis by aluminum. J Neurochem. 1984;42:438–46. doi: 10.1111/j.1471-4159.1984.tb02697.x. [DOI] [PubMed] [Google Scholar]
- 35.Cho SW, Joshi JG. Inactivation of Bakers’ yeast glucose-6-phosphate dehydrogenase by aluminum. Biochemistry. 1989;28:3613–8. doi: 10.1021/bi00434a069. [DOI] [PubMed] [Google Scholar]
- 36.Kumar V, Bal A, Gill KD. Impairment of mitochondrial energy metabolism in different regions of rat brain following chronic exposure to aluminium. Brain Res. 2008;1232:94–103. doi: 10.1016/j.brainres.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 37.Lemire J, Mailloux R, Puiseux-Dao S, Appanna VD. Aluminum-induced defective mitochondrial metabolism perturbs cytoskeletal dynamics in human astrocytoma cells. J Neurosci Res. 2009;87:1474–83. doi: 10.1002/jnr.21965. [DOI] [PubMed] [Google Scholar]
- 38.Shetty KT, Veeranna, Guru SC. Phosphatase activity against neurofilament proteins from bovine spinal cord: Effect of aluminium and neuropsychoactive drugs. Neurosci Lett. 1992;137:83–6. doi: 10.1016/0304-3940(92)90304-p. [DOI] [PubMed] [Google Scholar]
- 39.Johnson GV, Cogdill KW, Jope RS. Oral aluminum alters in vitro protein phosphorylation and kinase activities in rat brain. Neurobiol Aging. 1990;11:209–16. doi: 10.1016/0197-4580(90)90547-d. [DOI] [PubMed] [Google Scholar]
- 40.Yamamoto H, Saitoh Y, Yasugawa S, Miyamoto E. Dephosphorylation of tau factor by protein phosphatase 2A in synaptosomal cytosol fractions, and inhibition by aluminum. J Neurochem. 1990;55:683–90. doi: 10.1111/j.1471-4159.1990.tb04187.x. [DOI] [PubMed] [Google Scholar]
- 41.el-Sebae AH, Abdel-Ghany ME, Shalloway D, Abou Zeid MM, Blancato J, Saleh MA, et al. Aluminum interaction with human brain tau protein phosphorylation by various kinases. J Environ Sci Health B. 1993;28:763–77. doi: 10.1080/03601239309372852. [DOI] [PubMed] [Google Scholar]
- 42.Guy SP, Jones D, Mann DM, Itzhaki RF. Human neuroblastoma cells treated with aluminium express an epitope associated with Alzheimer's disease neurofibrillary tangles. Neurosci Lett. 1991;121:166–8. doi: 10.1016/0304-3940(91)90676-k. [DOI] [PubMed] [Google Scholar]
- 43.Kawahara M, Muramoto K, Kobayashi K, Kuroda Y. Functional and morphological changes in cultured neurons of rat Cerebral cortex induced by long-term application of aluminum. Biochem Biophys Res Commun. 1992;189:1317–22. doi: 10.1016/0006-291x(92)90217-9. [DOI] [PubMed] [Google Scholar]
- 44.Praticò D, Uryu K, Sung S, Tang S, Trojanowski JQ, Lee VM, et al. Aluminum modulates brain amyloidosis through oxidative stress in APP transgenic mice. FASEB J. 2002;16:1138–40. doi: 10.1096/fj.02-0012fje. [DOI] [PubMed] [Google Scholar]
- 45.Rodella LF, Ricci F, Borsani E, Stacchiotti A, Foglio E, Favero G, et al. Aluminium exposure induces Alzheimer's disease-like histopathological alterations in mouse brain. Histol Histopathol. 2008;23:433–9. doi: 10.14670/HH-23.433. [DOI] [PubMed] [Google Scholar]
- 46.Giorgianni CM, D’Arrigo G, Brecciaroli R, Abbate A, Spatari G, Tringali MA, et al. Neurocognitive effects in welders exposed to aluminium. Toxicol Ind Health. 2014;30:347–56. doi: 10.1177/0748233712456062. [DOI] [PubMed] [Google Scholar]
- 47.Akila R, Stollery BT, Riihimäki V. Decrements in cognitive performance in metal inert gas welders exposed to aluminium. Occup Environ Med. 1999;56:632–9. doi: 10.1136/oem.56.9.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kiesswetter E, Schäper M, Buchta M, Schaller KH, Rossbach B, Scherhag H, et al. Longitudinal study on potential neurotoxic effects of aluminium: I. Assessment of exposure and neurobehavioural performance of al welders in the train and truck construction industry over 4 years. Int Arch Occup Environ Health. 2007;81:41–67. doi: 10.1007/s00420-007-0191-2. [DOI] [PubMed] [Google Scholar]
- 49.Buchta AM, Kiesswetter BE, Schäper BM, Zschiesche CW, Schaller DK, Kuhlmann AA, et al. Neurotoxicity of exposures to aluminium welding fumes in the truck trailer construction industry. Environ Toxicol Pharmacol. 2005;19:677–85. doi: 10.1016/j.etap.2004.12.036. [DOI] [PubMed] [Google Scholar]
- 50.Altmann P, Dhanesha U, Hamon C, Cunningham J, Blair J, Marsh F, et al. Disturbance of cerebral function by aluminium in haemodialysis patients without overt aluminium toxicity. Lancet. 1989;2:7–12. doi: 10.1016/s0140-6736(89)90254-7. [DOI] [PubMed] [Google Scholar]
- 51.Bolla KI, Milstien S, Briefel G, Wieler L, Kaufman S. Dihydropteridine reductase activity: Lack of association with serum aluminum levels and cognitive functioning in patients with end-stage renal disease. Neurology. 1991;41:1806–9. doi: 10.1212/wnl.41.11.1806. [DOI] [PubMed] [Google Scholar]
- 52.Jackson M, Warrington EK, Roe CJ, Baker LR. Cognitive function in hemodialysis patients. Clin Nephrol. 1987;27:26–30. [PubMed] [Google Scholar]
- 53.Exley C, Mamutse G, Korchazhkina O, Pye E, Strekopytov S, Polwart A, et al. Elevated urinary excretion of aluminium and iron in multiple sclerosis. Mult Scler. 2006;12:533–40. doi: 10.1177/1352458506071323. [DOI] [PubMed] [Google Scholar]
- 54.Kawahara M. Effects of aluminum on the nervous system and its possible link with neurodegenerative diseases. J Alzheimers Dis. 2005;8:171–82. doi: 10.3233/jad-2005-8210. [DOI] [PubMed] [Google Scholar]
- 55.Bansal VK, Bansal S. Nervous system disorders in dialysis patients. Handb Clin Neurol. 2014;119:395–404. doi: 10.1016/B978-0-7020-4086-3.00025-4. [DOI] [PubMed] [Google Scholar]
- 56.Laabdar W, Elgot A, Gamrani H. The protective effect of curcumin on dopaminergic system after chronic aluminium intoxication: Possible link with Parkinson's disease. Parkinsonism Relat Disord. 2016;22:e188. [Google Scholar]
- 57.Wang Z, Wei X, Yang J, Suo J, Chen J, Liu X, et al. Chronic exposure to aluminum and risk of Alzheimer's disease: A meta-analysis. Neurosci Lett. 2016;610:200–6. doi: 10.1016/j.neulet.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 58.Pedersen NL. Reaching the limits of genome-wide significance in Alzheimer disease: Back to the environment. JAMA. 2010;303:1864–5. doi: 10.1001/jama.2010.609. [DOI] [PubMed] [Google Scholar]
- 59.Sjögren B, Iregren A, Montelius J, Yokel RA. Aluminum. In: Fowler BA, Nordberg M, editors. Handbook on the Toxicology of Metals. 4th ed. San Diego: Academic Press; 2015. pp. 549–64. [Google Scholar]
- 60.Gupta VB, Anitha S, Hegde ML, Zecca L, Garruto RM, Ravid R, et al. Aluminium in Alzheimer's disease: Are we still at a crossroad? Cell Mol Life Sci. 2005;62:143–58. doi: 10.1007/s00018-004-4317-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferreira PC, Piai Kde A, Takayanagui AM, Segura-Muñoz SI. Aluminum as a risk factor for Alzheimer's disease. Rev Lat Am Enfermagem. 2008;16:151–7. doi: 10.1590/s0104-11692008000100023. [DOI] [PubMed] [Google Scholar]
- 62.Yokel RA. Aluminum. In: Benjamin C, editor. Encyclopedia of Human Nutrition. 3rd ed. Waltham: Academic Press; 2013. pp. 57–63. [Google Scholar]
- 63.Klatzo I, Wisniewski H, Streicher E. Experimental production of neurofibrillary degeneration. I. Light microscopic observations. J Neuropathol Exp Neurol. 1965;24:187–99. doi: 10.1097/00005072-196504000-00002. [DOI] [PubMed] [Google Scholar]
- 64.Crapper DR, Krishnan SS, Dalton AJ. Brain aluminum distribution in Alzheimer's disease and experimental neurofibrillary degeneration. Science. 1973;180:511–3. doi: 10.1126/science.180.4085.511. [DOI] [PubMed] [Google Scholar]
- 65.Martyn CN, Barker DJ, Osmond C, Harris EC, Edwardson JA, Lacey RF, et al. Geographical relation between Alzheimer's disease and aluminum in drinking water. Lancet. 1989;1:59–62. [PubMed] [Google Scholar]
- 66.Exley C. The aluminium-amyloid cascade hypothesis and Alzheimer's disease. Subcell Biochem. 2005;38:225–34. doi: 10.1007/0-387-23226-5_11. [DOI] [PubMed] [Google Scholar]
- 67.Bondy SC. Prolonged exposure to low levels of aluminum leads to changes associated with brain aging and neurodegeneration. Toxicology. 2014;315:1–7. doi: 10.1016/j.tox.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 68.Bhattacharjee S, Zhao Y, Hill JM, Percy ME, Lukiw WJ. Aluminum and its potential contribution to Alzheimer's disease (AD) Front Aging Neurosci. 2014;6:62. doi: 10.3389/fnagi.2014.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bharathi V, Vasudevaraju P, Govindaraju M, Palanisamy AP, Sambamurti K, Rao KS, et al. Molecular toxicity of aluminium in relation to neurodegeneration. Indian J Med Res. 2008;128:545–56. [PubMed] [Google Scholar]
- 70.Zhang QL, Jia L, Jiao X, Guo WL, Ji JW, Yang HL, et al. APP/PS1 transgenic mice treated with aluminum: An update of Alzheimer's disease model. Int J Immunopathol Pharmacol. 2012;25:49–58. doi: 10.1177/039463201202500107. [DOI] [PubMed] [Google Scholar]
- 71.Alexandrov PN, Zhao Y, Jones BM, Bhattacharjee S, Lukiw WJ. Expression of the phagocytosis-essential protein TREM2 is down-regulated by an Al-induced miRNA-34a in a murine microglial cell line. J Inorg Biochem. 2013;128:267–9. doi: 10.1016/j.jinorgbio.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lukiw WJ, Pogue AI. Induction of specific micro RNA (miRNA) species by ROS-generating metal sulfates in primary human brain cells. J Inorg Biochem. 2007;101:1265–9. doi: 10.1016/j.jinorgbio.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Flaten TP. Aluminium as a risk factor in Alzheimer's disease, with emphasis on drinking water. Brain Res Bull. 2001;55:187–96. doi: 10.1016/s0361-9230(01)00459-2. [DOI] [PubMed] [Google Scholar]
- 74.Frisardi V, Solfrizzi V, Capurso C, Kehoe PG, Imbimbo BP, Santamato A, et al. Aluminum in the diet and Alzheimer's disease: From current epidemiology to possible disease-modifying treatment. J Alzheimers Dis. 2010;20:17–30. doi: 10.3233/JAD-2009-1340. [DOI] [PubMed] [Google Scholar]
- 75.Zatta P, Drago D, Bolognin S, Sensi SL. Alzheimer's disease, metal ions and metal homeostatic therapy. Trends Pharmacol Sci. 2009;30:346–55. doi: 10.1016/j.tips.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 76.Bolognin S, Messori L, Drago D, Gabbiani C, Cendron L, Zatta P, et al. Aluminum, copper, iron and zinc differentially alter amyloid-aβ(1-42) aggregation and toxicity. Int J Biochem Cell Biol. 2011;43:877–85. doi: 10.1016/j.biocel.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 77.Akiyama H, Hosokawa M, Kametani F, Kondo H, Chiba M, Fukushima M, et al. Long-term oral intake of aluminium or zinc does not accelerate Alzheimer pathology in aβPP and aβPP/tau transgenic mice. Neuropathology. 2012;32:390–7. doi: 10.1111/j.1440-1789.2011.01274.x. [DOI] [PubMed] [Google Scholar]
- 78.Ribes D, Colomina MT, Vicens P, Domingo JL. Impaired spatial learning and unaltered neurogenesis in a transgenic model of Alzheimer's disease after oral aluminum exposure. Curr Alzheimer Res. 2010;7:401–8. doi: 10.2174/156720510791383840. [DOI] [PubMed] [Google Scholar]
- 79.McLachlan DR, Bergeron C, Smith JE, Boomer D, Rifat SL. Risk for neuropathologically confirmed Alzheimer's disease and residual aluminum in municipal drinking water employing weighted residential histories. Neurology. 1996;46:401–5. doi: 10.1212/wnl.46.2.401. [DOI] [PubMed] [Google Scholar]
- 80.Neri LC, Hewitt D. Aluminium, Alzheimer's disease, and drinking water. Lancet. 1991;338:390. doi: 10.1016/0140-6736(91)90531-s. [DOI] [PubMed] [Google Scholar]
- 81.Chin-Chan M, Navarro-Yepes J, Quintanilla-Vega B. Environmental pollutants as risk factors for neurodegenerative disorders: Alzheimer and Parkinson diseases. Front Cell Neurosci. 2015;9:124. doi: 10.3389/fncel.2015.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Goldman SM. Environmental toxins and Parkinson's disease. Annu Rev Pharmacol Toxicol. 2014;54:141–64. doi: 10.1146/annurev-pharmtox-011613-135937. [DOI] [PubMed] [Google Scholar]
- 83.Wirdefeldt K, Adami HO, Cole P, Trichopoulos D, Mandel J. Epidemiology and etiology of Parkinson's disease: A review of the evidence. Eur J Epidemiol. 2011;26(Suppl 1):S1–58. doi: 10.1007/s10654-011-9581-6. [DOI] [PubMed] [Google Scholar]
- 84.Hirsch EC, Brandel JP, Galle P, Javoy-Agid F, Agid Y. Iron and aluminum increase in the substantia nigra of patients with Parkinson's disease: An X-ray microanalysis. J Neurochem. 1991;56:446–51. doi: 10.1111/j.1471-4159.1991.tb08170.x. [DOI] [PubMed] [Google Scholar]
- 85.Altschuler E. Al-containing antacids as a cause of idiopathic Parkin-son's disease. Med Hypotheses. 1999;53:22–3. doi: 10.1054/mehy.1997.0701. [DOI] [PubMed] [Google Scholar]
- 86.Zatta P, Zambenedetti P, Milanese M. Activation of monoamine oxidase type-B by aluminum in rat brain homogenate. Neuroreport. 1999;10:3645–8. doi: 10.1097/00001756-199911260-00033. [DOI] [PubMed] [Google Scholar]
- 87.Burke WJ, Kumar VB, Pandey N, Panneton WM, Gan Q, Franko MW, et al. Aggregation of alpha-synuclein by DOPAL, the monoamine oxidase metabolite of dopamine. Acta Neuropathol. 2008;115:193–203. doi: 10.1007/s00401-007-0303-9. [DOI] [PubMed] [Google Scholar]
- 88.Uversky VN, Li J, Fink AL. Metal-triggered structural transformations, aggregation, and fibrillation of human alpha-synuclein. A possible molecular NK between Parkinson's disease and heavy metal exposure. J Biol Chem. 2001;276:44284–96. doi: 10.1074/jbc.M105343200. [DOI] [PubMed] [Google Scholar]
- 89.Yasui M, Kihira T, Ota K. Calcium, magnesium and Al concentrations in Parkinson's disease. Neurotoxicology. 1991;13:593–600. [PubMed] [Google Scholar]
- 90.Good PF, Olanow CW, Perl DP. Neuromelanin-containing neurons of the substantia nigra accumulate iron and aluminum in Parkinson's disease: A LAMMA study. Brain Res. 1992;593:343–6. doi: 10.1016/0006-8993(92)91334-b. [DOI] [PubMed] [Google Scholar]
- 91.Shoenfeld Y, Agmon-Levin N. ‘ASIA’-autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36:4–8. doi: 10.1016/j.jaut.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 92.Álvarez-Soria MJ, Hernández-González A, Carrasco-García de León S, del Real-Francia MÁ, Gallardo-Alcañiz MJ, López-Gómez JL, et al. Demyelinating disease and vaccination of the human papillomavirus. Rev Neurol. 2011;52:472–6. [PubMed] [Google Scholar]
- 93.Murphy CP, Cox RL, Harden EA, Stevens DA, Heye MM, Herzig RH, et al. Encephalopathy and seizures induced by intravesical alum irrigations. Bone Marrow Transplant. 1992;10:383–5. [PubMed] [Google Scholar]
- 94.Bakir AA, Hryhorczuk DO, Ahmed S, Hessl SM, Levy PS, Spengler R, et al. Hyperaluminemia in renal failure: The influence of age and citrate intake. Clin Nephrol. 1989;31:40–4. [PubMed] [Google Scholar]
- 95.Hewitt CD, Poole CL, Westervelt FB, Jr, Savory J, Wills MR. Risks of simultaneous therapy with oral aluminium and citrate compounds. Lancet. 1988;2:849. doi: 10.1016/s0140-6736(88)92809-7. [DOI] [PubMed] [Google Scholar]
- 96.Alfrey AC, LeGendre GR, Kaehny WD. The dialysis encephalopathy syndrome. Possible aluminum intoxication. N Engl J Med. 1976;294:184–8. doi: 10.1056/NEJM197601222940402. [DOI] [PubMed] [Google Scholar]
- 97.Priest ND. 2nd ed. Oxford: Elsevier; 2005. Encyclopedia of Human Nutrition; pp. 69–76. [Google Scholar]
- 98.Nieboer E, Gibson BL, Oxman AD, Kramer JR. Health effects of Al: A critical review with emphasis on Al in drinking water. Environ Rev. 1995;3:29–81. [Google Scholar]
- 99.WHO/IPCS. Geneva: WHO/IPCS; 1997. Environmental Health Criteria 194, Aluminium. [Google Scholar]
- 100.Elevated Serum Al Levels in Hemodialysis Patients Associated with Use of Electric Pumps. Wyoming: 2007. Centers for Disease Control and Prevention. [Google Scholar]
- 101.Matsumoto H. Cell biology of aluminum toxicity and tolerance in higher plants. Int Rev Cytol. 2000;200:1–46. doi: 10.1016/s0074-7696(00)00001-2. [DOI] [PubMed] [Google Scholar]
- 102.Aguilar F, Autrup H, Barlow S, Castle L, Crebelli R, Dekant W, et al. Safety of aluminium from dietary intake scientific opinion of the panel on food additives, flavourings, processing aids and food contact materials (AFC) EFSA J. 2008;754:1–34. doi: 10.2903/j.efsa.2008.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.World Health Organization Technical Report Series 960. Geneva: 2011. Joint FAO/WHO Expert Committee on Food Additives. Evaluation of Certain Food Additives and Contaminants. [PubMed] [Google Scholar]
- 104.Bondy SC. Oxford: Academic Press; 2009. Encyclopedia of Neuroscience; pp. 253–7. [Google Scholar]
- 105.Mıtchell J, Mannıng GB, Molyneux M, Lane RE. Pulmonary fibrosis in workers exposed to finely powdered aluminium. Br J Ind Med. 1961;18:10–23. doi: 10.1136/oem.18.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Letzel S, Schaller K, Angerer J, Drexler H, Weber A, Schmid K, et al. Biological monitoring of occupational aluminium powder exposure. Occup Hyg. 1996;3:271–80. [Google Scholar]


