Abstract
Background:
Major neurocognitive disorder (MCD) is an acquired progressive decline in cognitive abilities that causes a drop in specific acquired performance compared to former performances. We tried to investigate the efficacy of herbal combination of sedge, saffron, and Astragalus honey on cognitive and depression score of patients with MCD.
Materials and Methods:
It was a randomized double-blind clinical trial conducted on sixty patients with MCD, who referred to the geriatric psychiatry clinic of Isfahan University of Medical Sciences in Iran. All the study participants had been using anti-MCD medications. Participants were randomized to receive a combination of sedge, saffron, and Astragalus honey in case group (n = 30) or placebo group for 8 weeks other than anti-MCD medications. Cognitive and depression scores were assessed using Addenbrook's Cognitive Scale and Geriatric Depression Scale, respectively, before intervention and at the 1st and 2nd months after intervention. The ANCOVA repeated-measure test was used to analyze the data using SPSS 20 software.
Results:
The Addenbrook's Cognitive Test score was 32.2 ± 26.5 in intervention and 22.1 ± 15.1 in control group before intervention (P = 0.074) and 38.8 ± 27.7 in intervention group and 22.6 ± 14.1 in control group in control group 1 month after intervention (P = 0.007). In addition, Geriatric Depression Scale score was 14.6 ± 7.9 in intervention group and 14.5 ± 6.9 in control group before intervention (P = 0.945) and 12.9 ± 6.9 in intervention and 14.3 ± 7.1 in control group 1 month after intervention (P = 0.465) and 12.2 ± 6.5 in intervention group and 14.4 ± 7.1 in control group 2 month after intervention (P = 0.224).
Conclusion:
Our findings suggest that adding the herbal combination of sedge, saffron, and Astragalus honey to the current protocols of treatment of MCD patients could be useful in the improvement of cognitive and depression score of these patients.
Keywords: Astragalus plant, cognition, cognitive disorders, mental status tests
INTRODUCTION
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM 5), major neurocognitive disorder (MCD) is marked by severe impairment in memory, judgment, orientation, and cognition that is mostly acquired and not congenital. There are several subtypes of MCD, namely Alzheimer's disease (AD), vascular dementia, frontotemporal lobar degeneration, Lewy body disease, traumatic brain injury from physical trauma, HIV disease, and Prion disease. Some kinds that are caused by medical condition are Parkinson's disease, Huntington's disease, substance/medication induced, multiple etiologic, and unspecified dementia.[1] The most common type of dementia is AD.[2]
Studies had shown that severity of dementia in AD greatly depends on the increase of neurons in the nucleus basalis of Meynert in brain which is accompanied with a significant reduction to the amount of acetylcholine transfer enzyme.[3]
Due to the impairment in cognitive and global function of patients with MCD, it may cause a huge catastrophic disease burden on patients and may induce a heavy psychological distress for their relatives and hence the optimal treatment is highly critical.
The available documented treatments are by cholinesterase inhibitors such as donepezil, rivastigmine, galantine, and tacrine. These drugs reduce acetylcholine neurotransmitter inactivation and thus enhance cholinergic neurotransmission.[4] The other effective drug called memantine is a kind of neuroprotective drug and its effective mechanisms include blocking NMDA glutamate receptors from moderate-to-severe cases of the disease and FDA approved.[5,6,7,8]
Several herbal remedies have been used in the treatment of cognitive disorders with variable results.[9,10,11] Ginkgo biloba L. with antioxidant properties showed effectiveness with the mechanism of increasing the blood flow in the brain.[6] It seems that those herbal remedies that contain antioxidant properties could improve the brain blood flow and decrease the degenerative process in the brain.
Honey contains a variety of enzymatic and nonenzymatic antioxidants such as glucose oxidase, catalase, L-ascorbic acid, flavonoids, phenolic acids, carotenoids, organic acids, amino acids, and protein.[7] Sedge rhizome is rich in natural antioxidants that can have a great important therapeutic impact on the aging process and free radicals of the diseases related, such as neural degeneration.[12,13] Studies demonstrated that methanolic extract of this herb strongly prevents the acetyl cholinesterase enzyme activity.[14] Saffron also contains crocin and safranl which can reduce the harmful effects of hyoscine on memory and enhance learning. Saffron extracts contain abundant carotenoids with strong antioxidant effects and can protect nerve cells in the central nervous system.[15,16]
There are some studies about the properties of sedge, saffron, and honey in the improvement of memory disorders.[17] Although the effect of these herbal medications has been reported in different studies, the combinatory effect has not been evaluated yet. Therefore, we tried to investigate the effect of addition of the combined extract with sedge, saffron, and Astragalus honey to common treatment to improve cognitive function score and depression score in patients with MCD. We tried to determine mean attention, memory, fluency, visuospatial function, and language scores, before and after intervention and to compare them between intervention and placebo groups.
MATERIALS AND METHODS
This study was a randomized double-blind clinical trial, which had been done on sixty previously diagnosed MCD patients that referred to the geriatric psychiatry clinic of Isfahan University of Medical Sciences (IUMS) between 2015 and 2017.
The definite diagnosis of MCD was done by an expert psychiatrist based on DSM 5 criteria. The sample size was assessed by the following formula:  , but due to the case drop possibility, we enrolled thirty patients in each group. Patients were randomly allocated through a random number table into two groups of intervention and placebo as binary random blocks.
, but due to the case drop possibility, we enrolled thirty patients in each group. Patients were randomly allocated through a random number table into two groups of intervention and placebo as binary random blocks.
This research is approved by the ethics committee of IUMS (Research project number 395043; [IRCT20161030255N1]). Written informed consent was taken from patients and their family. Inclusion criteria were as follows: age over 50 years, developing any form of mild-to-moderate MCD according to psychiatric clinical interviews and diagnostic criteria of DSM V,[1] and using routine anti-MCD drug treatment. The exclusion criteria were those with intellectual disability and major psychiatric diseases such as schizophrenia, previous history of mood disorder, and taking other herbal medicines. The intervention group received two capsules of combined sedge and saffron extract daily (each capsule containing 500 mg of sedge and 30 mg of saffron extract) plus a teaspoon of Astragalus honey (equal to 5 g in each take). The placebo group received two daily placebo capsules (containing starch) with a teaspoonful of rock candy syrup (equivalent to 5 mg); the duration of therapy was 3 months. Both the active and placebo capsules were made by pharmacology faculty of IUIMS. Both groups received usual treatment of anti-MCD medications. The usual antidementia therapy includes acetylcholine esterase inhibitors such as rivastigmine and donepezil and galantamine and memantine. Addenbrook's Cognitive Examination (ACE) for patients’ cognitive assessment and Geriatric Depression Scale (GDS) scale were assessed before intervention, 1 month after intervention, and 2 months after intervention.
Variable assessment
ACE for patients’ cognitive assessment and GDS scale for patients’ depression assessment in three phases of preintervention and 1st and 2nd months of intervention were used and the results were recorded. It should be noted that in all the three sessions, the side effects of the herbal compound (sedge, saffron, and Astragalus honey), such as gastrointestinal symptoms, diarrhea, rash, drowsiness, skin discoloration, blood in the urine, and medicinal plants’ interferences with the chemical drugs, were evaluated, reported, and recorded.
ACE, revised version (ACE-R): This test is a concise test used to diagnose and classify all forms of dementia, particularly AD and frontal temporal dementia. This test consists of five subtests in which each of the subtests evaluates one part of cognitive function. The maximum score on the test score is 100, subscores are as follows: attention/orientation (18 points), memory (26 points), fluency (14 points), language (26 points), and visuospatial function (16 points).[18] Validity and reliability of the Farsi version of this scale were reported by Pouretemad in 2007, respectively, as 0.93 and 0.91.[19]
GDS is a self-reported test of thirty questions. The GDS is a standard self-report test which can be used in patients without severe intellectual disability and major psychiatric diseases.
Yesavage et al. (1982) have designed this scale for measurement of elderly depression. Test–retest reliability and internal consistency of this scale in different researches are reported, respectively, as from 0.85 to 0.90 and from 0.89 to 0.94. Cutting point to the scale is a score of 16.5 (sensitivity 0.88 and specificity 0.87); also, in Iran, Amini et al. in a study reported the alpha coefficient of the scale to be 0.75 and the reliability coefficient of split-half scale to be 0.77.[20]
Medications were prescribed by a psychiatrist who were unaware of patients’ allocation. Therefore, the patients received the boxes including medication and placebo which had specific codes. The patients were also unaware of their allocation groups. Measurements were done by a psychologist who was unaware of the patients’ groups. In addition, the person who analyzed the data was unaware of the patients’ group and data analysis was done using codes.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics for Windows, Version 20.0. (Armonk, NY: IBM Corp), and descriptive tests (mean and standard deviation) were performed to describe the participants’ demographic characteristics. Furthermore, repeated-measures ANCOVA was performed for comparison of two groups (intervention and placebo groups) in three times (baseline and after 1 month and 2 months). Simultaneously in a model, age and education (conflict variables) were controlled. Model assumptions such as consequence normality, variance, and covariance normality of questions were investigated. P < 0.05 was considered statistically significant.
RESULTS
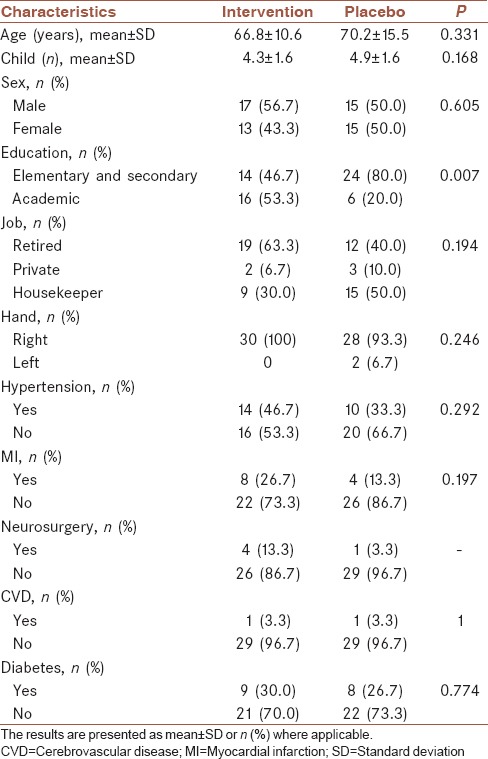
Data related to sixty patients who remained in the study were analyzed [Figure 1]. Results showed that the mean age of patients in the intervention group was 66.8 years and that of the placebo group was 70.2 years. The intervention group had a higher educational background than the placebo group which was considered in the further analysis. [Remaining details are shown in Table 1].
Figure 1.
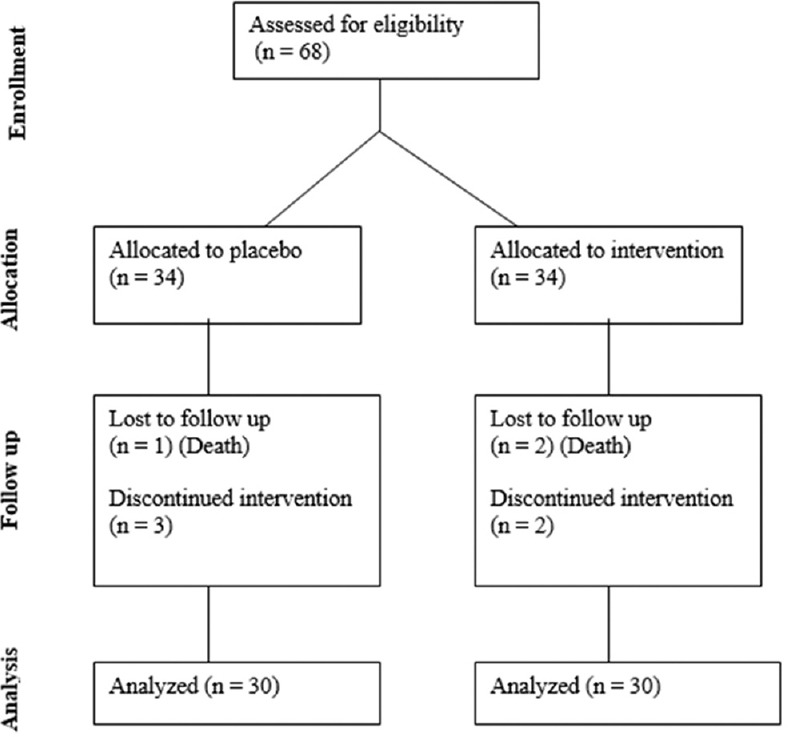
The consort flow diagram of the study
Table 1.
Comparison of demographic characteristics in patients with major neurocognitive disorder with respect to the intervention and placebo groups
Results of statistical tests [Table 2] show that attention (P = 0.006), memory (P = 0.004), language (P = 0.009), and visuospatial function (P = 0.015) are statistically significant in the intervention group, but fluency variable is not significant in the intervention group (P = 0.289). In total, Addenbrook's score in the intervention group was statistically significant (P = 0.001) [Table 3].
Table 2.
Summary results of variables of attention, memory, fluency, language, and visuospatial function in three stages
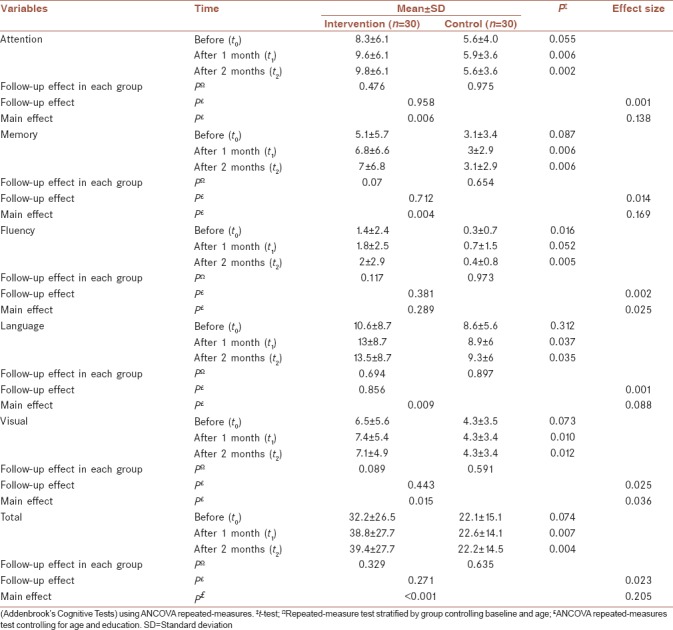
Table 3.
Analysis of variance of Mini-Mental State Examination and Geriatric Depression Scale at three stages of the test
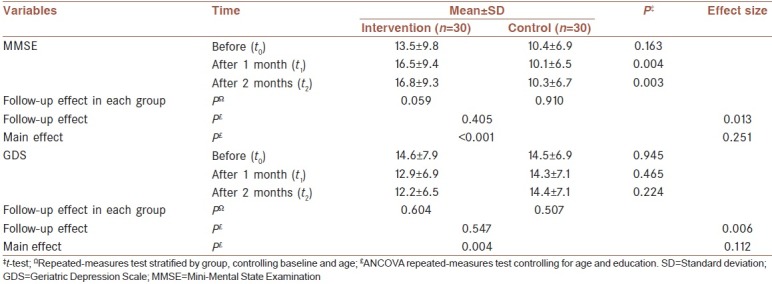
The results of Mini–Mental State Examination (MMSE) scores in intervention group were statistically significant (P = 0.001), and also GDS scores during intervention were statistically significant in the intervention group (P = 0.004).
DISCUSSION
Main study results
In this study, we evaluated the effect of adding sedge with honey and saffron to routine anti-MCD medications of patients with MCD. The effect was determined in 1 month and 2 months after starting the intervention. The effect was evaluated using Addenbrook's Cognitive Scale, MMSE, and GDS.
The results of our intervention showed significant increase in all items of Addenbrook's Cognitive Scale in the intervention group in comparison to the control group except fluency, which was also significantly higher in the intervention group after 2 months of follow-up. The items of these test include attention, memory, fluency, language, and visuospatial function. The fluency score was not significantly different in two groups at 1-month follow-up. Furthermore, we reported significant increase in MMSE in 1- and 2-month follow-ups. The GDS was not significantly different in two groups.
In summary, we observed the benefits of adding sedge with honey and saffron to routine anti-MCD medication of patients with MCD.
Role of honey in neurocognitive disorders
Some researchers have assessed the mechanism of action of honey in brain tissue. Oyefuga et al. in 2012 showed that usage of 250 mg honey causes a reduction of lipid peroxidation in the brain tissue and simultaneous reinforcement of superoxide dismutase and activities of glutathione reductase;[10] also Cia in his research in 2011 concluded that honey reduces the number of degenerating nerve cells in the CA1 region of the hippocampus, an area that is too much prone to oxidative stress.[21] Al-Rhbi in a study in 2014 showed that honey has a significant impact on short- and long-term memory.[22] In another study of Akhondzadeh et al., on 55 patients with dementia, the authors concluded that 30 g of honey in a day can be as effective as donepezil for patients with mild dementia.[23] In 2009, in one of the British universities, British researchers studied the cognitive function improvement on 212 patients with dementia who were treated by honey and saffron supplement; within 8 weeks, significant improvement in sleep and memory of patients was observed that was statistically significant. It was also shown that with longer treatment time, even up to 2 years, the recovery rate will also increase.[24]
Role of sedge in neurocognitive disorders
Since this study is a new research with innovation, unfortunately, clinical trials related to sedge are very low and have been done on animals. Among these trials, these studies can be mentioned; Rabie et al. found that sedge rhizome extract in rats, by preserving the changes in brain acetylcholine levels, significantly improved motor coordination.[20] Golghermezi and Nasri in 2015 found that sedge rhizome has no significant effect in improving learning ability of treated mice group. Intraperitoneal injection of sedge rhizome extract increases the recall rate. However, its positive impact on long-term memory is more than the short-term memory.[11]
Role of saffron in neurocognitive disorders
For studies in line with saffron, the following studies can be mentioned. A study by Geromichalos in 2012 showed that saffron can improve physical activity by 30% and acetylcholine in patients with dementia.[17] Akhondzadeh et al. showed that 3-week treatment with saffron improved cognitive performance of rats.[23] In another study of Hosseinzadeh et al. in 2004, the authors found that saffron can be as effective as fluoxetine in mice, and Noorbala et al. conducted a similar study in 2005 and achieved the same effect. In the meantime, Akhondzadeh et al. stated that saffron can be effective in mild depressed patients.[23,24,25] Moosavi also in 2014 stated in his research that 30 mg fluoxetine per day with 80 mg of saffron, during 6 weeks on depressed patients, can have a relatively better effect than saffron alone. In another study in 2015, Moosavi et al. showed that 15 mg saffron per day and 15 g crocin per day can cause good tolerance without complications for patients.[26] Hosseinali et al. also stated in their study in 2013 that 50–250 mg saffron per day causes increased dopamine, but without effect on serotonin and norepinephrine.[27]
Study limitations
Our study had several limitations. As mentioned before in the results’ section, the percentage of patients in intervention group who had higher educational levels was higher in comparison to that of the control group. However, we had randomly assigned patients to intervention and control groups, but the difference in educational level was significant. To address this issue, we have used analysis of covariances. However, it should be considered that this effect may influence our study results.
Another limitation of our study was sample size. Due to a few number of study participants, the study was done in few number of patients. This may cause the difference in educational level between two groups. Also, the study had a new topic and only a few randomized controlled trials were available.
Recommendations
Based on the findings of our study, we recommend studies with higher sample sizes which is needed to minimize the difference in baseline characteristics between the two groups. For achieving the higher sample sizes, we recommend larger multicentric studies. Also, we recommend more studies in this topic to achieve more valuable evidences about the role of herbal medications in the treatment of MCDs.
CONCLUSIONS
Our study has shown the beneficial effects of sedge with honey and saffron in the treatment of MCDs. However, more studies are needed to confirm these results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
At the end, it is essential to give my thanks and gratitude to IUMS, all professors who helped me in this matter, as well as patients and their families for their sincere cooperation in this study.
REFERENCES
- 1.Sadock BJ, Sadock MA, Pedro R. 11th ed. Vol. 270. USA: Lippincott Williams & Wilkins (LWW); 2015. Kaplan and Sadock's Comprehensive Text Book of Psychiatry. [Google Scholar]
- 2.Parihar MS, Hemnani T. Alzheimer's disease pathogenesis and therapeutic interventions. J Clin Neurosci. 2004;11:456–67. doi: 10.1016/j.jocn.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Giacobini E. Do cholinesterase inhibitors have disease-modifying effects in Alzheimer's disease? CNS Drugs. 2001;15:85–91. doi: 10.2165/00023210-200115020-00001. [DOI] [PubMed] [Google Scholar]
- 4.Sadock BJ, Sadock MA, Pedro R. 9th ed. Vol. 23. Lippincott Williams & Wilkins (LWW); 2009. Kaplan and Sadock's Comprehensive Text Book of Psychiatry; pp. 1867–2014. [Google Scholar]
- 5.Dixon M, Webb EC. 3rd ed. USA: Academic Press Inc; 1979. Enzymes; p. 2008. [Google Scholar]
- 6.Seidian M, Bathai F, Akhondzadeh S. Herbal medicine and natural products in the managemeat of dementia. Herbal Med J. 2004;2:1–8. [Google Scholar]
- 7.Dos Santos-Neto LL, de Vilhena Toledo MA, Medeiros-Souza P, de Souza GA. The use of herbal medicine in Alzheimer's disease – A systematic review. Evid Based Complement Alternat Med. 2006;3:441–5. doi: 10.1093/ecam/nel071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadock BJ, Sadock MA, Pedro R. 9th ed. Vol. 23. USA: Lippincott Williams & Wilkins (LWW); 2009. Kaplan and Sadock's Comprehensive Text Book of Psychiatry; pp. 1867–2000. [Google Scholar]
- 9.Mijanur Rahman M, Gan SH, Khalil MI. Neurological effects of honey: Current and future prospects. Evid Based Complement Alternat Med 2014. 2014:958721. doi: 10.1155/2014/958721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oyefuga OH, Ajani EO, Salau BA, Agboola F, Adebawo OO. Honey consumption and its anti-ageing potency in white Wister albino rats. Sch J Biol Sci. 2012;1:15–9. [Google Scholar]
- 11.Germezgoli S, Nasri S, Naseri M. Evaluating the Root Extract of Cyperus rotundus L. on Learning and Memory in Male Rats. sjimu. 2015;22:34–43. [Google Scholar]
- 12.Kilani-Jaziri S, Neffati A, Limem I, Boubaker J, Skandrani I, Sghair MB, et al. Relationship correlation of antioxidant and antiproliferative capacity of cyperus rotundus products towards K562 erythroleukemia cells. Chem Biol Interact. 2009;181:85–94. doi: 10.1016/j.cbi.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Nagulendran KR, Velavan S, Mahesh R. In vitro antioxidant activity and total polyphenolic content of cyperusrotundus rhizomes. J Chem. 2007;4:440–9. [Google Scholar]
- 14.Sharma R, Gupta R. Cyperus rotundus extract inhibits acetylcholinesterase activity from animal and plants as well as inhibits germination and seedling growth in wheat and tomato. Life Sci. 2007;80:2389–92. doi: 10.1016/j.lfs.2007.01.060. [DOI] [PubMed] [Google Scholar]
- 15.Ochiai T, Soeda S, Ohno S, Tanaka H, Shoyama Y, Shimeno H, et al. Crocin prevents the death of PC-12 cells through sphingomyelinase-ceramide signaling by increasing glutathione synthesis. Neurochem Int. 2004;44:321–30. doi: 10.1016/s0197-0186(03)00174-8. [DOI] [PubMed] [Google Scholar]
- 16.Purushothuman S, Nandasena C, Peoples CL, El Massri N, Johnstone DM, Mitrofanis J, et al. Saffron pre-treatment offers neuroprotection to nigral and retinal dopaminergic cells of MPTP-treated mice. J Parkinsons Dis. 2013;3:77–83. doi: 10.3233/JPD-130173. [DOI] [PubMed] [Google Scholar]
- 17.Abdolah SA. Mashhad: Entesharat e Astan e Ghods e Razavi; 1375. Tebolaemeh; p. 389. [Google Scholar]
- 18.Galton CJ, Erzinçlioglu S, Sahakian BJ, Antoun N, Hodges JR. A comparison of the Addenbrooke's cognitive examination (ACE), conventional neuropsychological assessment, and simple MRI-based medial temporal lobe evaluation in the early diagnosis of Alzheimer's disease. Cogn Behav Neurol. 2005;18:144–50. doi: 10.1097/01.wnn.0000182831.47073.e9. [DOI] [PubMed] [Google Scholar]
- 19.Pouretemad HR, Khatibi A, Ganjavi A, Shams J, Zarei M. Validation of Addenbrooke's cognitive examination (ACE) in a Persian-speaking population. Dement Geriatr Cogn Disord. 2009;28:343–7. doi: 10.1159/000252772. [DOI] [PubMed] [Google Scholar]
- 20.Amini Rastabi Z, Sharifi A A, Refahi J. Psychometric Properties of Geriatric Depression Scale in an Iranian Sample. sija. 2013;8:54–59. [Google Scholar]
- 21.Cai M, Shin BY, Kim DH, Kim JM, Park SJ, Park CS, et al. Neuroprotective effects of a traditional herbal prescription on transient cerebral global ischemia in gerbils. J Ethnopharmacol. 2011;138:723–30. doi: 10.1016/j.jep.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Al-Rahbi B, Zakaria R, Othman Z, Hassan A, Ahmad AH. Protective effects of tualang honey against oxidative stress and anxiety-like behaviour in stressed ovariectomized rats. Int Sch Res Notices. 2014;2014:521065. doi: 10.1155/2014/521065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akhondzadeh S, Sabet MS, Harirchian MH, Togha M, Cheraghmakani H, Razeghi S, et al. Saffron in the treatment of patients with mild to moderate Alzheimer's disease: A 16-week, randomized and placebo-controlled trial. J Clin Pharm Ther. 2010;35:581–8. doi: 10.1111/j.1365-2710.2009.01133.x. [DOI] [PubMed] [Google Scholar]
- 24.Hosseinzadeh H, Karimi G, Niapoor M. Antidepressant effect of Crocus sativus L stigma extracts and their constituents, crocin and safranal, in mice. Acta Hort. 2004;650:435–45. [Google Scholar]
- 25.Noorbala AA, Akhondzadeh S, Tahmacebi-Pour N, Jamshidi AH. Hydro-alcoholic extract of Crocus sativus L. versus fluoxetine in the treatment of mild to moderate depression: A double-blind, randomized pilot trial. J Ethnopharmacol. 2005;97:281–4. doi: 10.1016/j.jep.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Moosavi SM, Ahmadi M, Amini M, Vazirzadeh B, Sari I. The effects of 40 and 80 mg hydro-alcoholic extract of Crocus sativus in the treatment of mild to moderate depression. J Mazandaran Univ Med Sci. 2014;24:48–53. [Google Scholar]
- 27.Hosseinali E, Mojabi SN, Ranjbaran M, Shams J, Sahraei H, Hedayati M, et al. Aqueous extract of saffron (Crocus sativus) increases brain dopamine and glutamate concentrations in rats. J Behav Brain Sci. 2013;3:315–9. [Google Scholar]


