Abstract
Introduction:
Presbyopia is an important cause of avoidable visual disability.
Objective:
To estimate the prevalence of near vision impairment and spectacle coverage among middle and older-aged adults in rural Nepal.
Materials and methods:
The surveys was carried out among the people of age 35 and over in randomly-selected cluster samples in rural settings of Kaski district of western Nepal, Near visual acuity, with and without presenting near correction, was measured at 40 cm using a LogMAR near vision tumbling E chart under ambient indoor lighting. Subjects with uncorrected binocular distance vision of 20/40 or worse were refracted and those with near vision of 20/40 or worse tested with plus sphere to obtain the best-corrected binocular near visual acuity.
Results:
A total of 2,360 persons aged 35 years and over were enumerated and 2,156 (91.3 %) were examined. The age- and gender-standardized prevalence of uncorrected near visual impairment (vision of 20/40 or worse) in study population was found to be 66.1 %. Near vision could not be corrected (>20/40) even after distance and near vision correction in 6.4 %. Using the multiple logistic regression models, uncorrected visual impairment was associated with an older age (odds ratio [OR] = 1.13, P < 0.001) and a lower educational level (OR = 1.11, P = 0.01) was less associated with female gender (OR = 0.72, P = 0.038). Over 90 % of people with near visual impairment did not have spectacles.
Conclusion:
The prevalence of presbyopia appears to be higher with an earlier onset and over 90 % of people in need of near correction do not have spectacles in this setting.
Keywords: presbyopia, prevalence, near vision
Introduction
Uncorrected refractive error is increasingly recognized as an important cause of avoidable visual disability worldwide, and has been included as one of the priority diseases in Vision 2020 (Pararajasegaram, 1999; Resnikoff et al 2004). The World Health Organization (WHO) also acknowledged that presbyopia is an important disease affecting quality of life, but it has yet to be included in WHO estimates of disease burden, in part due to lack of scientifically-valid, population-based data (Resnikoff et al, 2004).
Prevalence of presbyopia has been reported in Tanzania (Burke et al, 2006), China (Lu et al 2011), India (Nirmalan et al, 2006) and Timor-Leste (Ramke et al, 2007). Widely-varying prevalence rates of presbyopia and spectacle coverage among presbyopic persons have been reported, partly due to differences in definitions, protocols, measurement conditions and age groups between studies (Holden et al, 2008).
The purpose of the current study was to evaluate the prevalence of near vision impairment among people aged 35 years and above using a standardized protocol. Survey was conducted by enrolling subjects starting at the age of 35 years, presumably prior to the onset of presbyopia, the study could assess the age-specific onset and prevalence of vision impairment caused by presbyopia.
Materials and methods
Study sites and sampling:
The study was conducted in a rural area 200 kilometers west of Kathmandu in the Kaski district. The study area in Kaski District consisted of mainly rural, valley, hills and mountain with altitude ranging from 1000 to 8000 meters. Agriculture is the subsistence occupation of the population residing in this area, which has also been partially supported by tourism in the town and villages along the trekking routes. The total population of the district is 380,527 with an average density of 189 person per square kilometer (2001 Census).
The survey was carried out in a randomly-selected sample of individuals within study site. The sampling frame was constructed using geographically-defined clusters based on census data. Cluster boundaries were defined in such a way that each cluster would have approximately 100 study participants. A sample size on the order of 2,000 was based on estimating the prevalence of near vision impairment within age subgroups, with adjustment for nonparticipation and cluster design effects.
In door-to-door household visits, eligible persons were enumerated by name, gender, age, education (highest level completed), and spectacle usage. Those 65 years and above were interviewed in all households, those 50–64 were interviewed in every other household (1/2 of households), and those 35–49 were interviewed in every fourth household (1/4 of households). The interviews covered the questions on vision functioning and work productivity and an assessment of the burden of their visual disability. This age-based sampling for interviews was used to ensure a reasonably balanced distribution of study subjects across the three age categories.
Examinations took place in local community facilities, according to pre-scheduled dates established at the time of enumeration. Those who did not appear at the examination site were revisited by a member of the enumeration team to encourage participation. Written informed consent using a written consent form was obtained at the time of the examination, if not already obtained during the enumeration visit.
Examination procedures:
Binocular distance and near visual acuity (VA), both with and without correction for those presenting with distance, bifocals or near vision spectacles, was measured for distance at 4 meters using a retro-illuminated log-MAR chart with tumbling-E optotypes and at 40 cm using a LogMAR near vision tumbling E chart (Precision Vision, La Salle, Illinois) under ambient lighting. VA was recorded as the smallest, line read with one or no errors. After obtaining best corrected distance visual acuity, subjects with uncorrected binocular near vision of 20/40 or worse were progressively tested with increasing plus spheres to obtain best-corrected near VA. Those presenting with binocular near vision of 20/63 or worse that could be improved by two or more lines were provided with near vision glasses free of charge.
Approval for implementation of the survey was obtained from the Institutional Research Review Board of Nepal Netra Jyoti Sangh. Human subject research approval of the protocol was also cleared by the World Health Organization (WHO) Secretariat Committee on Research Involving Human Subjects. The study adhered to the tenets of the Declaration of Helsinki.
Data management and analysis:
Computerized data entry was carried out at using standardized programs. Measurement data ranges, frequency distributions, and consistency among related measurements were checked with data cleaning programs.
Crude and standardized prevalence rates of near vision impairment 20/40 to 20/63 and <20/63 were calculated using uncorrected and best-corrected binocular VA. In adjusting for the age and gender differences the standardization procedure calculated the prevalence rates that would result if had an age- and gender-distribution similar to the aggregated sample. The association of age, gender and education with vision impairment (presenting and best-corrected binocular near vision of 20/40 or worse) was investigated with multiple logistic regression.
The proportion of participants with uncorrected, presenting and best-corrected near VA 20/40 or worse was plotted as a function of age for each site using LOWESS smoothing. The LOWESS procedure imputes smoothed values for age-specific rates using a locally-weighted regression of the prevalence of vision impairment on age.
Statistics
Statistical analyses were performed using Stata/SE Statistical Software: Release 9.0 (Stata Corporation, College Station, Texas). Confidence intervals (CI) and P values (significant at the P less than 0.05 level) were calculated with adjustment for clustering effects associated with the sampling design.
Results
A total of 2,360 persons aged >35 years was enumerated and 2,156 (91.3 %) examined, with distributions across age, gender and education as shown in Table 1.
Table 1.
Study population by gender, age, education and study site
| Enumerated | Examined | Response rate | |
|---|---|---|---|
| Gender | |||
| Male | 897 (38.0) | 814 (37.8) | 90.8 |
| Female | 1,463 (62.0) | 1,342 (62.2) | 91.7 |
| Age | |||
| 35–49 | 973 (41.2) | 861 (39.9) | 88.5 |
| 50–64 | 825 (35.0) | 764 (35.4) | 92.6 |
| ≥ 65 | 562 (23.8) | 531 (24.6) | 94.5 |
| Education | |||
| None | 1,524 (64.6) | 1,395 (64.7) | 91.5 |
| <Primary | 203 (8.6) | 179 (8.3) | 88.2 |
| Primary | 290 (12.3) | 262 (12.2) | 90.3 |
| Secondary | 85 (3.6) | 79 (3.7) | 92.9 |
| ≥ High School | 232 (9.8) | 217 (10.1) | 93.5 |
| Missing | 26 (1.1) | 24 (1.1) | 92.3 |
| All | 2,360 (100.0) | 2,156 (100.0) | 91.4 |
Data are given as number (percentage) of participants.
In multiple logistic regression modeling, examination response was associated with older age, female gender, and higher educational level (Table 1). The examined population consisted of 37.5 % male and 62.5 % female. The mean age of the examined population was 54.7 +/− 13.4 years. Nearly two-third or 64.7 % of those overall examined were without formal education. Education at the high school level or higher was reported in only 10.1 % of the examined population.
Gender and age specific prevalence of uncorrected and best-corrected binocular, near visual acuity >20/40, 20/40 to 20/63, and <20/63 and Standardized age- and gender-adjusted prevalence are also shown in Table 2.
Table 2.
Prevalence of uncorrected and best-corrected near visual acuity > 20/40, 20/40 to 20/63, and < 20/63
| Visual Acuity | >20/40 | 20/40--20/63 | < 20/63 |
|---|---|---|---|
| Gender | |||
| Male | 25.1; 90.3 | 42.4; 6.9 | 32.6; 2.8 |
| Female | 37.6; 93.1 | 36.9; 3.7 | 25.6; 3.2 |
| Age (Years) | |||
| 35–39 | 94.4; 100 | 5.3; 0.0 | 0.33; 0.0 |
| 40 −49 | 50.2; 98.6 | 35.3; 0.54 | 14.6; 0.90 |
| 50–59 | 11.4; 98.2 | 49.7; 0.99 | 38.9; 0.79 |
| 60–69 | 8.2; 91.7 | 50.1; 5.6 | 41.7; 2.7 |
| 70+ | 13.1; 68.0 | 45.1; 19.7 | 41.9; 12.3 |
| All* | 33.9 (32.3, 35.4); 93.6 (92.7, 94.4) |
39.1 (37.1, 41.1); 3.7 (3.0, 4.3) |
26.8 (25.1, 28.6); 2.5 (1.9, 3.1) |
Data given as % uncorrected visual acuity; best corrected visual acuity.
*Standardized age- and gender-adjusted prevalence (95 % confidence interval): uncorrected visual acuity; best-corrected visual acuity.
In multiple logistic regression modeling, uncorrected near vision of20/40 or worse was associated with older age OR 1.13 95 % CI 1.10 to 1.16, P=<0.001 and lower educational level OR 1.11 95 % CI 1.05 to 1.18 P=0.001 (Table 3). The female gender was significantly less associated with near vision impairment (OR 0.72, 95 % CI 0.53 to 0.98 P=0.001).
Table 3.
Multiple logistic regression odds ratios for uncorrected visual acuity 20/40 or worse
| Uncorrected Visual Acuity ≤ 20/40 | ||
|---|---|---|
| Older Age | Female Gender | Lower Education |
| Level | ||
| 1.13 (1.10–1.16) | 0.72 (0.53–0.98) | 1.11 (1.05–1.18) |
| P=<0.001 | P=0.038 | P=0.001 |
Data are given as odds ratio (95 % confidence interval).
LOWESS smoothed curves of uncorrected, presenting and best-corrected visual acuity 20/40 or worse across the age group are shown in Figure 1. The area between the uncorrected and best-corrected VA curves represents the magnitude of the need for refractive correction and the area between uncorrected and presenting shows the unmet need of presbyopic correction. Table 4 shows the utilization of near vision correction for participants with vision impairment 20/40 to 20/63 and < 20/63. The use of spectacles for near vision correction was uncommon.
Figure 1:
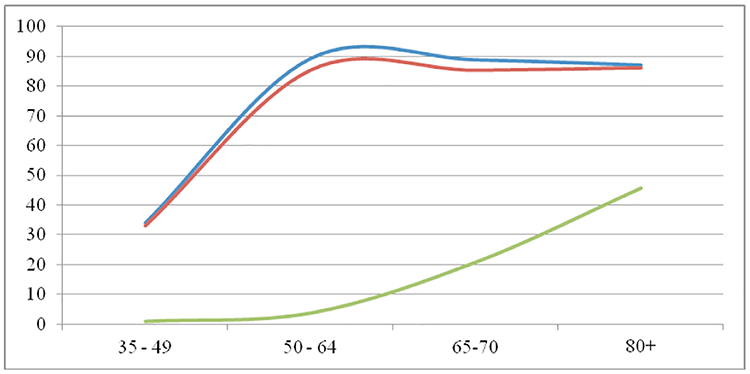
LOWESS smoothed age group -specific distributions of near visual acuity 20/40 or worse: uncorrected (top curve), presenting (middle curve), and best-corrected (bottom curve).
Table 4.
Percentage of participants with uncorrected visual acuity 20/40 to 20/63 and <20/63 wearing refractive spectacles
| Glass Wearing status | TOTAL | |||
|---|---|---|---|---|
| None | Distance Only | Distance & Near | Near Only | |
| 780 (92.3) | 20 (2.38) | 20 (2.38) | 20 (2.38) | 840 (100.0) |
| 542 (89.1) | 28 (4.61) | 24 (3.95) | 14 (2.30) | 608 (100.0) |
Data are presented as number (percentage) of participants. The top entry pertains to uncorrected visual acuity 20/40 to 20/63 and the bottom entry to visual acuity <20/63.
Table 5 shows the “already met” and “unmet” need for refractive correction among those with uncorrected visual acuity 20/40 or worse. In the study sites, generally less than 5 % of the need for refractive correction was met. As shown, most of the unmet need for refractive correction was fully correctable to >20/40 with best correction. Subjects correctable to >20/40 generally experienced an improvement of at least three lines in near vision. Those not experiencing any improvement with best correction (zero lines) accounted for 3.66 % of the vision impaired participants.
Table 5.
Correction of visual impairment in participants with uncorrected visual acuity 20/40 or worse Met Need (Already Corrected to >20/40)
| Met Need (Already Corrected to >20/40) | Lines improvemen | Correctable to > 20/40 | Not Correctable to > 20/40 (in lines) | Total |
| 0 | 0 | 53 (3.66) | ||
| 1 | 16 (1.10) | 24 (1.66) | ||
| 2 | 80 (5.52) | 25 (1.73) | ||
| 3 | 429 (29.6) | 26 (1.80) | ||
| 4 | 163 (11.3) | 22 (1.52) | ||
| ≥5 | 533 (36.8) | 21 (1.45) | ||
| 56 (3.87) | All | 1,221 (84.3) | 171 (11.8) | 1448 (100) |
Data expressed as number (percentage) of participants.
Discussion
The current study is the first population-based study of presbyopia in Nepal. The study used standardized methods for near visual acuity measurement, which should improve the validity of the data collected.
Definitions adopted for presbyopia in available reports are not uniform: some utilize the near visual acuity (one line or greater improvement when near vision < N8 print) with near optical correction (Burke et al, 2006; Ramke et al, 2007), while others depend on the power of added near optical correction over that used to correct distance vision (Lu et al, 2011; Nirmalan et al, 2006). Both of these definitions are based on the fact that presbyopia is characterized by accommodation loss. In the current study, which is focused principally on ascertaining the prevalence of visual disability, we attempt to define “near vision impairment” rather than “presbyopia”, based a cutoff of near visual acuity (20/40 or worse).
Our study was carried out predominantly in rural settings and which is fairly the representative to the hilly population of Nepal. The demographic characteristics showed predominantly women (62.0 %), whereas the proportion of women was closer to that of men in the national census. The study populations in Kaski (64.6 %) were predominately illiterate. This educational profile is important in understanding the demand and unmet need for correction of near vision impairment given educated people tend to be myopic and have better access to eye care (Rosner et al, 1987; Wong et al, 2002).
Response rates were generally lower among men and younger persons because of temporary migration, which would be expected to lead to higher observed prevalence, given the age and gender as-sociations with near vision impairment. Prevalence rates would also be biased upwards if those experiencing vision problems were disproportionately more likely to participate.
Those with impaired best-corrected near vision presumably suffered from media opacity (cataract, corneal diseases), fundus disease and other non-refractive ocular abnormalities. The age and sex-standardized prevalence of “best-corrected” near vision impairment were considerably higher in this study area due to limited access to eye care services.
Uncorrected near vision depends on the loss of accommodation (presbyopia), refraction status (hyperopia and myopia) and the presence of ocular disease such as un-operated cataract. The prevalence of near vision impairment based on uncorrected vision reached 60 % or higher in at a cutoff of 20/40 or worse, or 20–30 % when a more stringent cutoff (<20/63) was used. Our findings of higher prevalence of near vision impairment among older persons and women are consistent with studies carried out in Tanzania (Burke), India (Nirmalan et al 2006) and northern China (Lu et al 2011).
Among those with near vision impairment (vision of 20/40 or worse), more than 90 % of them were correctable and potentially in demand for optical correction. Among those needing near correction, more than 90 % did not have spectacles.
The current investigation is among the first population-based studies demonstrating this tremendous unmet need for presbyopic correction in rural areas. Although, one may argue that near vision tasks are less demanding in rural areas, adverse impact of near vision impairment on visual functioning has been well demonstrated in the current study. (The results will be presented in a separate paper.)
Barriers to accessing presbyopic correction include cost (Nirmalan et al, 2006; Ramke et al, 2007), knowledge (Lu et al, 2011), and difficulty in accessing high-quality refractive services (Nirmalan et al 2006). The success of a business model based on selling presbyopic spectacles in the community highlights the fact that demand exists even in rural areas (Vision Spring, 2011)
Conclusion
More than 60 % of people aged 35 years and over have near vision impairment, and that these rates increase with age. Over 90 % of people in need of near optical correction do not have spectacles in rural areas.
Acknowledgement
Financial Support: Supported by the World Health Organization, Geneva, Switzerland (under National Institutes of Health [Bethesda, Maryland]. Contract no.: N01-EY-2103).
Source of support: acknowledged.
Footnotes
Conflict of interest: none
References
- Burke AG, Patel I, Munoz B, Kayongoya A, McHiwa W, Schwarzwalder AW, et al. (2006). Population-based study of presbyopia in rural Tanzania. Ophthalmology; 113(5): 723–7. [DOI] [PubMed] [Google Scholar]
- Holden BA, Fricke TR, Ho SM, Wong R, Schlenther G, Cronje S, et al. (2008). Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol; 126(12): 1731–9. [DOI] [PubMed] [Google Scholar]
- Lu Q, He W, Murthy GV, He X, Congdon N, Zhang L, et al. (2011). Presbyopia and near vision impairment in rural Northern China. Invest Ophthalmol Vis Sci. 2011. [DOI] [PubMed] [Google Scholar]
- Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R (2006). A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci; 47(6): 2324–8. [DOI] [PubMed] [Google Scholar]
- Pararajasegaram R (1999). VISION 2020-the right to sight: from strategies to action. Am J Ophthalmol; 128(3): 359–60. [DOI] [PubMed] [Google Scholar]
- Ramke J, du Toit R, Palagyi A, Brian G, Naduvilath T (2007). Correction of refractive error and presbyopia in Timor-Leste. Br J Ophthalmol; 91(7): 860–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP (2008). Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ; 86(1): 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner M, Belkin M (1987). Intelligence, education, and myopia in males. Arch Ophthalmol; 105(11): 1508–11. [DOI] [PubMed] [Google Scholar]
- Vision Spring delivers high quality, affordable eyeglasses to individuals. http://www.visionspring.org/what-we-do/model.php [cited 2011 17 April].
- Wong TY, Foster PJ, Johnson GJ, Seah SK (2002). Education, socioeconomic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br J Ophthalmol; 86(9): 963–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


