Abstract
Oxidative stress plays a central role in the pathogenesis of many human diseases. The nuclear factor erythroid 2-related factor 2 (Nrf2) is a key transcription factor regulating the intracellular antioxidant response and is an emerging target for the prevention and therapy of oxidative stress-related diseases. Salviae Miltiorrhizae Radix et Rhizoma (SMRR) is a traditional Chinese medicine (TCM) and is commonly used for the therapy of cardiac cerebral diseases. Cumulative evidences indicated that the extract of SMRR and its constituents, represented by lipophilic diterpenoid quinones and hydrophilic phenolic acids, were capable of activating Nrf2 and inhibiting oxidative stress. These bioactive constituents demonstrated a therapeutic potential against human diseases, exemplified by cardiovascular diseases, neurodegenerative diseases, diabetes, nephropathy, and inflammation, based on the induction of Nrf2-mediated antioxidant response and the inhibition of oxidative stress. In the present review, we introduced the SMRR and Nrf2 signaling pathway, summarized the constituents with an Nrf2-inducing effect isolated from SMRR, and discussed the molecular mechanism and pharmacological functions of the SMRR extract and its constituents.
1. Introduction
Oxidative stress is defined as an imbalance of the oxidants/antioxidants tilting toward an oxidative status and characterized by the overproductions of reactive oxygen species (ROS) and reactive nitrogen species (RNS) compared with the basal state [1]. Cumulative evidences have verified that oxidative stress impairs cellular components (e.g., lipids, proteins, and nucleic acids) and plays a central role in the pathogenesis of many human diseases, such as cardiovascular diseases, neurodegenerative diseases, chronic obstructive pulmonary disease (COPD), atherosclerosis, chronic kidney diseases, diabetes, and cancer [2–8]. To eliminate excess oxidants and maintain intracellular redox homeostasis, cells have developed an adaptive and dynamic antioxidant defense system, including antioxidant molecules, antioxidant enzymes, and phase II detoxifying enzymes, to protect cells and tissues against oxidative insults.
The nuclear factor erythroid 2-related factor 2 (Nrf2) is a key transcription factor regulating the intracellular antioxidant response and plays a vital role in maintaining intracellular redox homeostasis [9]. The predominant biological function of Nrf2 is to activate the transcriptions of a wide array of cytoprotective genes that are capable of counteracting the harmful effects caused by oxidative stress and toxicants. Activation of the Nrf2-mediated cellular defense system definitely intervenes the pathogenesis of oxidative stress-induced diseases, such as cancer [10], diabetes [11], respiratory diseases [12], chronic inflammation [13], cardiovascular diseases [14], and neurodegenerative diseases [15]. The protective roles of Nrf2 against oxidative insults and xenobiotic have also been verified by bioassays using Nrf2-null mice. For example, Nrf2-null mice are more susceptible to cigarette smoke-induced emphysema [16], acetaminophen-induced hepatotoxicity [17], and benzo[a]pyrene-induced carcinogenesis [18]. Therefore, the activation of the Nrf2-mediated antioxidant defense system is an efficient strategy for the prevention and therapy of these diseases.
Natural product without a doubt is an invaluable source for discovering Nrf2 activators, and nowadays, plenty of natural molecules demonstrate therapeutic potentials against oxidative stress-related disease due to their functions on the activation of Nrf2 [19]. In our systematic investigation of Nrf2 activators from traditional Chinese medicines (TCM) [1, 20–22], we found that the extract of Salviae Miltiorrhizae Radix et Rhizoma (SMRR) promoted the activity of Nrf2-mediated phase II detoxifying enzyme, NAD(P)H: quinone reductase, and thus displayed potency on the activation of the Nrf2 signaling pathway [21]. Consistent with our observations, some literatures indicated that lipophilic diterpenoid quinones and hydrophilic phenolic acids, two types of predominant bioactive ingredients of SMRR, possessed evident Nrf2-inducing properties and inhibited the pathogenesis of diseases, exemplified by Alzheimer's disease [23], cardiovascular diseases [24, 25], and hepatic injury [26].
Although some reviews concerning the chemistry and pharmacology of SMRR have been published [27, 28], chemical constituents with Nrf2-inducing effects and their pharmacological functions based on the activation of Nrf2 have not been summarized. In this review, we introduced the SMRR and Nrf2 pathway, summarized the Nrf2 activators from SMRR, and discussed their molecular mechanisms and pharmacological functions against human diseases.
2. Nrf2 Signaling Pathway
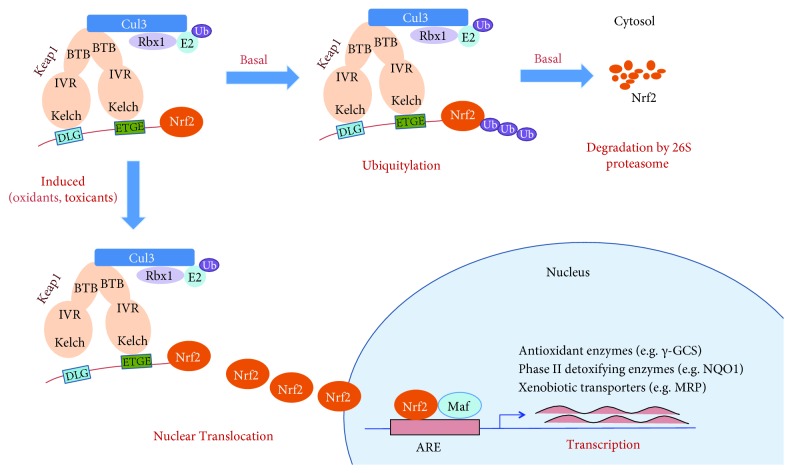
Nrf2 is a basic leucine zipper (bZIP) transcription factor bearing a Cap‘n'collar (CNC) structure [29]. It possesses seven functional domains, named as Neh1–Neh7. The Neh2 domain is the key regulatory domain with two binding sites (termed as ETGE and DLG motifs) that interact with its negative regulator, Kelch-like ECH-associated protein 1 (Keap1), a substrate adaptor protein for the cullin 3- (Cul3-) containing E3 ubiquitin ligase (Figure 1) [30, 31]. Keap1 contains three functional domains that are the broad complex/tramtrack/bric-a-brac (BTB) domain, intervening region (IVR), and Kelch domain. The N-terminal BTB domain is involved in the dimerization of Keap1 via binding with Cul3. The Kelch domain interacts with the Neh2 domain of Nrf2 and regulates its physiological functions.
Figure 1.
Schematic model of the regulation of the Nrf2 signaling pathway. Under basal conditions, Nrf2 undergoes Keap1-mediated ubiquitylation and 26S proteasome-mediated degradation. In response to oxidants, toxicants, or Nrf2 inducers, Nrf2 is released from Keap1, translocates into the nucleus, and activates the transcription of ARE-mediated protective genes.
Under a normal state, Nrf2 is primarily localized in a complex with its repressor Keap1 via direct protein-protein interactions and is maintained at a low level in cytosol through Keap1-mediated ubiquitylation and 26S proteasome-mediated degradation. Upon exposure of cells to oxidative stress, Nrf2 is released from Keap1, translocates into the nucleus, binds to the antioxidant response element (ARE) located in the promoter region of cytoprotective genes, and activates their transcription. These ARE-containing genes are mainly divided into three groups: (i) intracellular redox-balancing proteins, including γ-glutamyl cysteine synthetase (γ-GCS), thioredoxin reductase (TrxR), and heme oxygenase-1 (HO-1) that maintain the cellular redox capacity and eliminate ROS; (ii) phase II detoxifying enzymes, exemplified by NAD(P)H: quinone oxidoreductase 1 (NQO1) and glutathione S-transferase (GST), which promote excretion of toxicants; and (iii) xenobiotic transporters: multidrug resistance-associated protein (MRP) [9, 32]. The schematic model of the Nrf2 pathway is shown in Figure 1. Based on the biological functions of these genes, the activation of Nrf2-mediated defensive response efficiently counteracts oxidative insults.
3. Salviae Miltiorrhizae Radix et Rhizoma (SMRR)
Salviae Miltiorrhizae Radix et Rhizoma, named as “Danshen” in Chinese, is the roots and rhizomes of Salvia miltiorrhiza Bunge (Labiatae) (Figure 2) and has a long history for the therapy of human diseases in China. Its medical applications have been recorded in many Chinese medical documents, including “Shennong's Classic of Materia Medica” (Shennong Ben Cao Jing) and “Compendium of Materia Medica” (Ben Cao Gang Mu). According to the theory of TCM, it possesses the capabilities of promoting blood flow in menstruation, removing blood stasis, relieving pain, resolving mental uneasiness and restlessness, nourishing the blood, and tranquilizing the mind (Chinese Pharmacopoeia, 2015). Presently, it is predominantly used in multicomponent preparations (e.g., Fufang Danshen Tablets, Fufang Danshen Dripping Pills, and Guanxin Danshen Capsules) to treat cardiac cerebral diseases (e.g., ischemic heart disease, ischemic stroke, coronary heart disease, angina, and thrombosis) owing to SMRR's biological functions of inhibiting platelet aggregation, modulating endothelial cell permeability, and protecting cells from ischemia-reperfusion (I/R) injury. Besides these pharmacological effects, a growing body of data indicated that SMRR potently activated intracellular antioxidant enzymes, upregulated endogenous antioxidants, and scavenged intracellular ROS. Therefore, SMRR demonstrated potential therapeutic effects against oxidative stress-induced diseases, such as cardiovascular diseases, inflammation, and renal disease [33–35].
Figure 2.
Pictures of Salvia miltiorrhiza and Salviae Miltiorrhizae Radix et Rhizoma: (a) the whole plant of S. miltiorrhiza; (b) the roots of S. miltiorrhiza; and (c) medicinal materials of SMRR used in TCM.
4. Chemical Ingredients from SMRR and Their Potential Nrf2-Inducing Effects
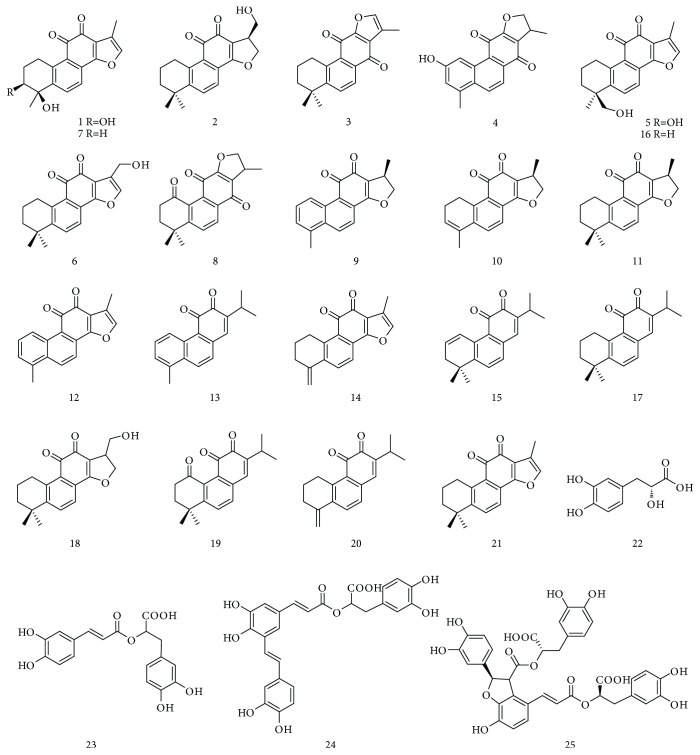
Since the long history of traditional applications and significant therapeutic effects against human diseases, a large number of phytochemical investigations of SMRR have been performed to give the isolation of diverse chemical ingredients. The structural information of the purified ingredients has been summarized by some reviews [27, 36, 37]. Based on their structural characteristics and molecular polarity, SMRR-derived chemical ingredients are classified into two groups: (i) lipophilic diterpenoid quinones, which are commonly abietane-type diterpenoid skeleton with quinone moiety, including tanshinone I (12), tanshinone IIA (16), and miltirone (17), and (ii) hydrophilic phenolic acids that are condensed caffeic acid derivatives with different linkage and degree of polymerization, such as danshensu (22) and salvianolic acids A-B (24-25). Up to now, more than fifty diterpenoid quinones and forty phenolic acids have been reported from SMRR [27]. Among them, tanshinone IIA (16) and salvianolic acid B (25) are considered to be biologically active substances of SMRR and thus are selected as the markers for the quality control of SMRR (Chinese Pharmacopoeia, 2015). In this section, we have only summarized the chemical ingredients with Nrf2-inducing activity. As depicted in Table 1 and Figure 3, diterpenoid quinones are the predominant Nrf2 inducers of SMRR. For instance, Zhang et al. identified twenty diterpenoid quinones, including constituents 1–17, using a strategy combining a HPLC-based high-resolution peak fractionation approach and an ARE luciferase assay in HEK 293 T cells [38]. Furthermore, diterpenoid quinones 1, 5, 9, 11, and 15–21 were verified to be potential Nrf2 inducers by a HPLC/MS/MS method combined with QR-inducing assay in Hepa 1c1c7 cells [39]. Of which, 15,16-dihydrotanshinone I (9), tanshinone I (12), tanshinone IIA (16), and miltirone (17) have been extensively investigated. The phenolic acids, including danshensu (22), rosmarinic acid (23), and salvianolic acids A-B (24-25), are capable of activating Nrf2-mediated cytoprotective responses.
Table 1.
Chemical constituents with Nrf2-inducing activity.
| Structural type | No | Name of compounds | Nrf2-inducing activity | Cell or animal models | Ref |
|---|---|---|---|---|---|
| Diterpenoid quinones | 1 | Tanshindiol B | 6.80-fold induction of ARE luciferase activity | HEK 293 T cells | [38] |
| 4.85 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| 2 | 17-Hydroxycryptotanshinone | 3.97-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 3 | Isotanshinone IIA | 6.45-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 4 | Trijuganone A | 4.31-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 5 | Tanshinone IIB | 5.34-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 4.85 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| 6 | Przewaquinone A | 6.01-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 7 | Przewaquinone B | 7.27-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 8 | 1-Ketoisocryptotanshinone | 5.65-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 9 | 15,16-Dihydrotanshinone I | 3.38-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 4.80 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| Induction of ARE luciferase and upregulation of Nrf2 protein level | MDA-MB-231 cells | [40] | |||
| Induction of Nrf2, NQO1, and γ-GCS protein levels | Human dermal fibroblasts. | [41] | |||
| 10 | 1,2,15,16-Tetrahydrotanshinone I | 4.37-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 11 | Cryptotanshinone | 3.61-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 5.07 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| Induction of ARE luciferase and upregulation of Nrf2 protein level | MDA-MB-231 cells | [40] | |||
| Induction of ARE-luciferase activity | Hep G2 cells | [26] | |||
| 12 | Tanshinone I | 2.60-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 5.90 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| Induction of ARE luciferase and upregulation of Nrf2 protein level | MDA-MB-231 cells | [40] | |||
| Upregulation of Nrf2, HO-1, GCLC, and GCLM | SH-SY5Y cells | [42, 43] | |||
| Induction of ARE-luciferase activity | Hep G2 cells | [26] | |||
| Induction of Nrf2, NQO1, and γ-GCS protein levels | Human dermal fibroblasts | [41] | |||
| 13 | RO-090680 | 3.06-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 14 | Methylenetanshinquinone | 2.77-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 15 | 1,2-Didehydromilitirone | 3.79-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 1.04 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| 16 | Tanshinone IIA | 2.58-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 5.10 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| Upregulation of Nrf2, HO-1, and NQO-1 protein levels | JB6 cells | [44] | |||
| Induction of ARE luciferase and upregulation of Nrf2 protein level | MDA-MB-231 cells | [40] | |||
| Upregulation of Nrf2, NOQ-1, HO-1, GCLC, and GCLM protein levels | Human aortic smooth muscle cells. | [45] | |||
| Induction of ARE-luciferase activity and upregulation of mRNA levels of GCLC, NQO1, and HO-1 | Hepa G2 cells | [26] | |||
| Induction of Nrf2 and upregulation of mRNA and protein levels of HO-1, NQO1, and GCLC | SH-SY5Y cells | [46] | |||
| 17 | Miltirone | 3.32-fold induction of ARE luciferase activity | HEK 293 T cells | [38] | |
| 0.92 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |||
| Enhancement of Nrf2 translocation and upregulation mRNA and protein levels of Nrf2, HO-1, and NQO1 | EA.hy926 cells | [47] | |||
| 18 | 17-Hydroxycryptotanshinone | 4.85 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |
| 19 | 1-Oxomiltirone | 0.40 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |
| 20 | 4-Methylenemiltirone | 0.46 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |
| 21 | 1,2-Dihydrotanshinone I | 5.40 μM for 2-fold induction of QR activity | Hepa 1c1c7 cells | [39] | |
|
| |||||
| Phenolic acids | 22 | Danshensu | Upregulation of mRNA and protein levels of Nrf2 | Rat heart | [48] |
| 23 | Rosmarinic acid | Upregulation of Nrf2 and HO-1 protein level | Rat cochlea | [49] | |
| 24 | Salvianolic acid A | Induction of mRNA and protein levels of Nrf2 and HO-1 | RPE cells | [50, 51] | |
| 25 | Salvianolic acid B | Induction of Nrf2 and HO-1 | Rat lung tissue | [52] | |
| Induction of Nrf2 protein level | Rat primary neurons | [53] | |||
| Induction of Nrf2, HO-1, and GCLC protein levels | Hepa G2 cells | [54] | |||
Figure 3.
Chemical constituents with potential Nrf2-inducing effects isolated from SMRR.
5. Nrf2-Based Therapeutic Potential of SMRR and Its Constituents against Human Diseases
Plenty of reviews have summarized the pharmacological functions and therapeutic effects of SMRR and its constituents on cardiovascular diseases [25, 55–57], neurodegenerative disease [23], cancer [58], osteoporosis [59], diabetes, and liver fibrosis [28]. In this section, we focused on their therapeutic effects related to the activation of Nrf2-mediated antioxidant response and inhibition of oxidative stress.
5.1. Cardiovascular Diseases
Oxidative stress plays an important role in the pathogenesis of cardiovascular diseases, including hypertension, I/R injury, atherosclerosis, and heart failure [7, 60–62]. Inductions of the Nrf2-regulated enzymes [e.g., superoxide dismutase (SOD), HO-1, catalase (CAT), and glutathione peroxidase (GPx)] are beneficial for the therapy of these cardiovascular diseases. The aqueous extract of SMRR prevented myocardium oxidative injury in an I/R rat model [34]. It enhanced capacities of antioxidant enzymes (e.g., SOD, CAT, and GPx) and prevented myocardium cell apoptosis. Similarly, the ethanol extract of SMRR, together with tanshinone IIA (16) and salvianolic acid B (25), dose-dependently reduced the levels of myocardium malondialdehyde (MDA) and ROS and enhanced myocardium glutathione (GSH) levels in the I/R rat model [63].
Tanshinone IIA (16) induced the Nrf2 signaling pathway via activating ERK and PKB, as well as downregulating the levels of tumor necrosis factor (TNF-α) and angiotensin II, and inhibited H2O2-induced ROS production in human aortic smooth muscle cells [45]. It reversed TNF-α-induced downregulations of intracellular GSH, NADPH, and glucose 6-phosphate dehydrogenase (G6PDH). Tanshinone IIA (16) also increased the expressions of Nrf2-mediated proteins, HO-1, ATP-binding cassette transporter A1 (ABCA1), and ATP-binding cassette transporter G1 (ABCG1) in lipid-laden macrophages, and thus suppressed accumulation of cholesterol in human macrophages [64]. Tanshinone IIA (16) increased Nrf2 and HO-1 expressions through the activation of phosphoinositide 3-kinase (PI3K)/Akt in human umbilical vein endothelial cells (HUVECs) and protected cells against H2O2-induced HUVEC oxidative injury [65–67]. It also upregulated the GPx activity and protected J774 macrophages against H2O2-induced cell death [68]. Tanshinone IIA (16) attenuated cardiac dysfunction and fibrosis and prevented cardiac remodeling via downregulating NAD(P)H oxidase-derived ROS production in 2K2C hypertensive rats [69]. In addition, tanshinone IIA (16) inhibited the productions of oxidized low-density lipoprotein (ox-LDL) and superoxide anion and reduced MDA level in the excessive vitamin D2 and high-cholesterol diet-induced rat atherosclerotic calcification model [70].
Ox-LDL induces endothelial dysfunction and changes of intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), and E-selectin, which are involved in the pathogenesis of atherosclerosis. Cryptotanshinone (11) inhibited ox-LDL-induced membrane expressions of ICAM-1, VCAM-1, and E-selectin, which was associated with its capability of inhibiting ROS production and nuclear factor-κB (NF-κB) activation [71]. Miltirone (17) enhanced the expressions of Nrf2, HO-1, and NQO1 in human EA.hy926 endothelial cells [47]. It protected EA.hy926 cells against ox-LDL-induced endothelial insults via inhibiting ROS synthesis and upregulating SOD and glutathione S-transferase (GST) in an Nrf2/HO-1 dependent manner.
Danshensu (22) was investigated for its cardioprotective activity using isolated rat hearts of the I/R model [48]. It attenuated I/R injury through scavenging ROS and inhibiting the oxidative stress. A further study indicated that danshensu (22) upregulated endogenous antioxidant enzymes (e.g., SOD, CAT, MDA, GPx, and HO-1), which was associated with the activation of the Nrf2/Akt/ERK1/2 signaling pathway. Salvianolic acid A (24) inhibited the productions of intracellular ROS and MDA and alleviated the change of mitochondrial membrane potential (MMP), in the tert-butyl hydroperoxide- (t-BHP-) induced HUVEC oxidative injury model [72].
5.2. Neurodegenerative Diseases
Oxidative stress and its impairment to the mitochondria play a dominant role in the onset and progression of multiple neurodegenerative disorders, including Alzheimer's disease, Parkinson's disease, and Huntington's disease [73]. Based on its function on inhibiting oxidative stress, Nrf2 is considered to be an emerging target for the treatment of neurodegenerative disorders [73, 74]. Tanshinone I (12) activated the expressions of Nrf2, HO-1, glutamate-cysteine ligase catalytic subunit (GCLC), and glutathione cysteine ligase modulatory subunit (GLCM) in SH-SY5Y cells [42]. Tanshinone I (12) inhibited 6-hydroxydopamine- (6-OHDA-) induced cell death and ROS production in SH-SY5Y neuroblastoma cells [42]. In an in vivo assay, tanshinone I (12) attenuated 6-OHDA-induced striatal oxidative stress and blocked dopaminergic neurotoxicity in 6-OHDA-lesion mice. It also protected the mitochondria against paraquat-induced redox impairment via upregulating Nrf2-regulated antioxidant enzymes, such as Mn-superoxide dismutase (Mn-SOD), GPx, and γ-glutamate-cysteine ligase (γ-GCL) [43]. Similarly, tanshinone IIA (16) induced the expressions of Nrf2, HO-1, GCLC, and GCLM in SH-SY5Y cells and protected cells against 6-OHDA-induced ROS production and cell death in an Nrf2-dependent manner in vitro [46]. It ameliorated neurodegeneration in a 6-OHDA-induced rat model of Parkinson's disease.
Salvianolic acid A (24) enhanced neuronal survival and stabilized MMP in SH-SY5Y cells and protected SH-SY5Y cells against H2O2-induced oxidative injury [75]. This protective effect was caused by the inhibition of the AMP-activated protein kinase (AMPK) and the Akt signaling pathway. Salvianolic acid B (25) was evaluated for the protection against cognitive decline using a high-fat diet-fed mouse model [76]. It upregulated antioxidant enzymes (e.g. SOD and GPx), attenuated hippocampal redox status, and thus counteracted cognitive decline [76]. Salvianolic acid B (25) was also investigated for its neuroprotection using lipopolysaccharide- (LPS-) and 1-methyl-4-phenylpyridinium- (MPP+-) induced neuronal injury model in vitro [53]. Salvianolic acid B (25) upregulated Nrf2 expression and decreased LPS- and MPP+-induced toxicities of dopamine neurons in the primary neuroglia of a mouse. Salvianolic acid B (25) attenuated dopaminergic neuronal loss, inhibited neuroinflammation, and improved the neurological function of neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine- (MPTP-) treated mice [53].
5.3. Diabetes
Oxidative stress triggers the mitochondrial damage which is the predominant contributing factor of excessive β-cell death [77]. Furthermore, high glucose-induced redox imbalance provokes oxidative insults of human tissues and organs (e.g., cardiovascular system, kidney, and eyes) [78]. The activation of Nrf2-regulated antioxidant response relieved the pathogenesis and progression of diabetes [79, 80]. Salvianolic acid B (25) inhibited the development of diabetes-related nephropathy and vascular complications in a type 2 diabetic animal model [81]. It also protected pancreatic β-cells against cytokines, interferon-γ (INF-γ), and interleukin- (IL-) 1β and induced INS-1 cell death through activating the expressions of Nrf2, HO-1, and Sirt1 [82]. Salvianolic acid A (24) reduced the levels of advanced glycation end products (AGEs) and MDA and improved intestinal motility in diabetic rats [83].
5.4. Nephropathy
Oxidative stress has been implicated in the onset and promotion of nephropathy, and the modulation of Nrf2 is an efficient strategy for the therapy of renal diseases [84]. Ethyl acetate extract of SMRR enhanced the expression of Nrf2 and inhibited ROS production in high-glucose-induced mouse mesangial cells (MMCs) [33]. It reduced albuminuria and alleviated renal damage in streptozocin-induced mice. SMRR injection inhibited N(G)-nitro-d-arginine-induced oxidative injury in a rat kidney [85]. It upregulated the activities of endogenous antioxidant enzymes (e.g., SOD and GPx) and decreased the level of MDA. Salvianolic acid B (25) activated Nrf2, reduced cellular ROS level in HK-2 cells, and protected cells against H2O2-induced cell death [86]. Furthermore, an in vivo study indicated that it activated Nrf2 expression, inhibited renal oxidative stress, and attenuated renal tubular injury in iodinated contrast media-induced acute renal injury in rats. This protection against renal damage was associated with the activation of the PI3K/Akt/Nrf2 pathway.
5.5. Inflammation
Oxidative stress activates redox-sensitive NF-κB and subsequently triggers the overproductions of proinflammatory cytokines and enzymes, such as tumor necrosis factor-α (TNF-α), ILs, cyclooxygenase-2 (COX-2), and inducible NO synthesis (iNOS) [87]. Nrf2 negatively regulated these proinflammatory cytokines and enzymes and thus inhibited inflammatory response. SMRR upregulated the GSH level and inhibited MDA level in the synovium and articular cartilage of the rabbits and prevented articular cartilage degeneration in rabbits with osteoarthritis [35]. Extract of SMRR induced the expressions of HO-1 and Nrf2 and inhibited H2O2-stimulated production of ROS in RAW 264.7 macrophages [88]. The activation of Nrf2 was attributed to the PI3K/Akt and MEK1 signaling pathway. Tanshinone IIA (16) induced HO-1 expression in RAW 264.7 macrophages and inhibited LPS-stimulated upregulation of COX-2 and iNOS [89]. A high-fat diet gave rise to the decrease of Nrf2 expression, accumulation of oxidative stress, and inflammation in C57BL/6 mouse. Salvianolic acid B (25) upregulated the expressions of Nrf2, HO-1, and NQO1 and thus inhibited the expressions of NF-κB, COX-2, and iNOS in mice fed a high-fat diet [90].
5.6. Liver Diseases
As the major metabolism organ of xenobiotics, the liver is apt to be kept in a sustained oxidative state, which causes a variety of liver diseases, covering fibrosis, cirrhosis, and carcinoma [91, 92]. The extract of SMRR inhibited aflatoxin B1- (AFB1-) induced cytotoxicity in cultured primary rat hepatocytes since its capability of inhibiting oxidative stress [93]. AFB1-induced ROS formation and GSH depletion could be reverted by SMRR extract treatment. Tanshinone IIA (16) upregulated the protein level of Nrf2 and enhanced the mRNA levels of GCLC, NQO1, and HO-1 in HepG2 cells and in a C57BL/6J mouse liver [26]. Tanshinone IIA (16) alleviated acetaminophen- (APAP-) induced upregulations of serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), and lactate dehydrogenase (LDH). It reverted the APAP-induced decreases of GSH, GST, GPx, SOD, and CAT in a mouse liver and thus prevented APAP-induced hepatotoxicity. Similarly, tanshinone IIA (16) upregulated the levels of Nrf2-mediated antioxidant enzymes (e.g., HO-1, SOD, CAT, and GPx) and inhibited fibrosis in a rat model of cirrhosis.
Salvianolic acid A (24) evidently reduced oxidative stress, evidenced by decreasing the levels of ROS and MDA and increasing the levels of hepatic superoxide dismutase and GSH, in rat liver tissue [94]. Furthermore, salvianolic acid A (24) significantly inhibited carbon tetrachloride- (CCl4-) induced hepatotoxicity. Decreased levels of serum ALT and AST in response to CCl4 exposure were recovered after treatment with 24. Salvianolic acid A (24) demonstrated radioprotective effects against γ-radiation-induced damage in human embryo liver L-02 cells, which was associated with inhibitions of ROS generation and mitochondrial cytochrome C release [95]. Salvianolic acid B (25) demonstrated APAP-induced liver injury in mice [54]. It upregulated the expressions of Nrf2, GCLC, and HO-1 via the activation of the PI3K and protein kinase C (PKC) pathway in HepG2 cells.
5.7. Lung Diseases
The lung is directly and continuously exposed to the external oxidants and toxicants, and thus excessive ROS are produced in the lung tissue. These endogenous and exogenous oxidants contribute to the pathophysiology of lung diseases, exemplified by chronic obstructive pulmonary disease and pulmonary fibrosis [96, 97]. Tanshinone I (12) enhanced Nrf2-mediated expressions of NQO1 and γ-GCS through hindering Nrf2 ubiquitination and specifically reacting with cysteine residue at amino acid 151 in Keap1 protein [40]. It protected human bronchial epithelial HBE cells against As(III)-induced oxidative damage in an Nrf2-dependent manner. An in vivo study using Nrf2+/+ and Nrf2−/− mice indicated that tanshinone I (12) attenuated As(III)-induced inflammatory lung damage in Nrf2+/+ mice, and this protective effect vanished in Nrf2−/− mice.
Salvianolic acid B (25) upregulated the expressions of Nrf2 and HO-1, enhanced GSH production, and inhibited cigarette smoke-induced lung pathological changes and inflammatory responses [52]. Salvianolic acid B (25) reduced the expression of ROS-generating enzyme NADPH oxidase-4 (Nox4) in lung tissue of mice [98]. It inhibited paraquat-induced structure distortion, collagen overproduction, proinflammatory cytokine release, and oxidative insults. Salvianolic acid B (25) inhibited PQ-induced activation of the transforming growth factor-β (TGF-β1)/Smad3 pathway, which was a key regulator of pulmonary fibrosis [99]. The capability of 25 in activating Nrf2 and inhibiting pulmonary fibrosis was further confirmed by a MRC-5 human lung fibroblast cell model and a bleomycin-induced rat pulmonary fibrosis model [100].
5.8. Ocular Diseases
Oxidative stress is involved in the pathogenesis of age-related macular degeneration [101]. Salvianolic acid A (24) inhibited H2O2-induced ROS production and prevented H2O2-induced primary and transformed retinal pigment epithelial cell death and apoptosis [51]. Activations of Nrf2 and HO-1 by salvianolic acid A (24) are essential for this protective effect. The Nrf2-inducing effect of 24 is associated with the activations of PI3K and the mammalian target of rapamycin (mTOR) signaling pathway [50]. It attenuated ox-LDL-induced lipidosis and apoptosis in the retinal pigment epithelium layer and inhibited ox-LDL-induced elevated ROS level and RPE inflammation in a rat model. These data suggested that salvianolic acid A (24) was a potential therapeutic agent against age-related macular degeneration.
5.9. Others
Because of wide distribution in the human tissues and organs, the activation of Nrf2 is an effective method for the therapy of many human diseases [102, 103]. Noise-induced hearing loss is associated with oxidative stress and lipoperoxidative damage. Rosmarinic acid (23) enhanced Nrf2/HO-1-mediated endogenous antioxidant defense system, attenuated hearing loss, and promoted hair cell survival in a noise-induced rat model [49]. Tanshinone I (12) and 15,16-dihydrotanshinone (9) induced the expressions of Nrf2, GCLC, and NQO1 through inhibiting Nrf2 ubiquitination in human Hs27 dermal fibroblasts and HaCaT keratinocytes [41]. These two constituents significantly suppressed solar-simulated UV and riboflavin-sensitized ultraviolet-induced skin cell death. A solar-simulated UV-induced human skin reconstruct model was established for evaluating the photoprotective effect of 15,16-dihydrotanshinone (9). Treatment with 15,16-dihydrotanshinone (9) definitely attenuated epidermal solar insult.
6. Conclusion and Future Perspectives
Oxidative stress plays a vital role in the pathogenesis of many human diseases. The activation of the Nrf2-mediated antioxidant defense system inhibits oxidative stress and thus effectively blocks the onset and progression of oxidative stress-induced human diseases. SMRR is a traditional Chinese medicine that has been long used for the treatment of cardiac cerebral diseases. Lipophilic diterpenoid quinones and hydrophilic phenolic acids are predominant constituents and contribute to the pharmacological functions of SMRR. These two types of constituents demonstrate potent Nrf2-inducing effects and hence are potential agents for the treatment of oxidative stress-related diseases. The SMRR extract, as well as the purified constituents, tanshinone I (12), tanshinone IIA (16), salvianolic acids A (24), and B (25), has been extensively investigated, and their inductions on the Nrf2 pathway and therapeutic effects on cardiovascular diseases, neurodegenerative diseases, diabetes, nephropathy, inflammation, liver diseases, and lung diseases have been verified by multiple models in vitro and in vivo.
Although there has been great progress on SMRR and its constituents, important areas on their phytochemistry, pharmacology, and medical applications related to the activation of Nrf2 remain to be explored. (i) Plenty of diterpenoid quinones have been isolated from SMRR; however, extensive researches still focused on several active constituents, including 15,16-dihydrotanshinone I (9), tanshinone I (12), tanshinone IIA (16), and miltirone (17). Miscellaneous diterpenoid quinones should be extensively investigated, such as their structure-activity relationship and mechanisms of action on the activation of Nrf2. (ii) Besides these verified medical applications, SMRR and its constituents possess potential pharmacological functions (e.g., chemoprevention on cancer and therapeutic effect on diabetic nephropathy) because of their activation of Nrf2. Thus, these unconfirmed pharmacological activities should be noted. (iii) Based on the traditional uses, chemical constituents, and pharmacological functions of SMRR, future works on discovering new lead compounds and developing SMRR and its constituents into new drugs for the therapy of oxidative stress-related diseases are significant.
Acknowledgments
This work was financially supported by NSF of Shandong Province (ZR2014HM019), NNSFs of China (31470419 and 81673558), and Young Scholars Program of Shandong University (2015WLJH50).
Abbreviations
- ABCA1:
ATP-binding cassette transporter A1
- AFB1:
Aflatoxin B1
- AGEs:
Advanced glycation end products
- ALT:
Alanine aminotransferase
- APAP:
Acetaminophen
- AST:
Aspartate aminotransferase
- ARE:
Antioxidant response element
- BTB:
Broad complex/tramtrack/bric-a-brac
- CAT:
Catalase
- COX-2:
Cyclooxygenase-2
- γ-GCL:
γ-Glutamate cysteine ligase
- GCLC:
Glutamate cysteine ligase catalytic subunit
- GCLM:
Glutathione cysteine ligase modulatory subunit
- γ-GCS:
γ-Glutamyl cysteine synthetase
- GPx:
Glutathione peroxidase
- GSH:
Glutathione
- GST:
Glutathione S-transferase
- HO-1:
Heme oxygenase-1
- ICAM-1:
Intercellular adhesion molecule-1
- HUVECs:
Human umbilical vein endothelial cells
- IL:
Interleukin
- INF-γ:
Interferon-γ
- iNOS:
Inducible NO synthesis
- I/R:
Ischemia-reperfusion
- IVR:
Intervening region
- Keap1:
Kelch-like ECH-associated protein 1
- LDH:
Lactate dehydrogenase
- LPS:
Lipopolysaccharide
- MDA:
Malondialdehyde
- MMP:
Mitochondrial membrane potential
- Mn-SOD:
Mn-superoxide dismutase
- MPP+:
1-Methyl-4-phenylpyridinium
- MPTP:
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- mTOR:
Mammalian target of rapamycin
- NF-κB:
Nuclear factor-κB
- NQO1:
NAD(P)H: quinone oxidoreductase 1
- Nrf2:
Nuclear factor erythroid 2-related factor 2
- 6-OHDA:
6-Hydroxydopamine
- ox-LDL:
Oxidized low-density lipoprotein
- PKC:
Protein kinase C
- PI3K:
Phosphoinositide 3-kinase
- RNS:
Reactive nitrogen species
- ROS:
Reactive oxygen species
- SMRR:
Salviae Miltiorrhizae Radix et Rhizoma
- SOD:
Superoxide dismutase
- t-BHP:
tert-Butyl hydroperoxide
- TCM:
Traditional Chinese medicines
- TGF-β1:
Transforming growth factor-β
- TNF-α:
Tumor necrosis factor-α
- TrxR:
Thioredoxin reductase
- VCAM-1:
Vascular cell adhesion molecule-1.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- 1.Zhou M.-X., Li G.-H., Sun B., et al. Identification of novel Nrf2 activators from Cinnamomum chartophyllum H.W. Li and their potential application of preventing oxidative insults in human lung epithelial cells. Redox Biology. 2018;14:154–163. doi: 10.1016/j.redox.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bargagli E., Olivieri C., Bennett D., Prasse A., Muller-Quernheim J., Rottoli P. Oxidative stress in the pathogenesis of diffuse lung diseases: a review. Respiratory Medicine. 2009;103(9):1245–1256. doi: 10.1016/j.rmed.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Chen X., Guo C., Kong J. Oxidative stress in neurodegenerative diseases. Neural Regeneration Research. 2012;7(5):376–385. doi: 10.3969/j.issn.1673-5374.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jay D., Hitomi H., Griendling K. K. Oxidative stress and diabetic cardiovascular complications. Free Radical Biology & Medicine. 2006;40(2):183–192. doi: 10.1016/j.freeradbiomed.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Klaunig J. E., Kamendulis L. M., Hocevar B. A. Oxidative stress and oxidative damage in carcinogenesis. Toxicologic Pathology. 2010;38(1):96–109. doi: 10.1177/0192623309356453. [DOI] [PubMed] [Google Scholar]
- 6.Maritim A. C., Sanders R. A., Watkins J. B. Diabetes, oxidative stress, and antioxidants: a review. Journal of Biochemical and Molecular Toxicology. 2003;17(1):24–38. doi: 10.1002/jbt.10058. [DOI] [PubMed] [Google Scholar]
- 7.Harrison D., Griendling K. K., Landmesser U., Hornig B., Drexler H. Role of oxidative stress in atherosclerosis. The American Journal of Cardiology. 2003;91(3):7–11. doi: 10.1016/S0002-9149(02)03144-2. [DOI] [PubMed] [Google Scholar]
- 8.Vaziri N. D. Roles of oxidative stress and antioxidant therapy in chronic kidney disease and hypertension. Current Opinion in Nephrology and Hypertension. 2004;13(1):93–99. doi: 10.1097/00041552-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Jaramillo M. C., Zhang D. D. The emerging role of the Nrf2–Keap1 signaling pathway in cancer. Genes & Development. 2013;27(20):2179–2191. doi: 10.1101/gad.225680.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khor T. O., Huang M.-T., Prawan A., et al. Increased susceptibility of Nrf2 knockout mice to colitis-associated colorectal cancer. Cancer Prevention Research. 2008;1(3):187–191. doi: 10.1158/1940-6207.CAPR-08-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li B., Liu S., Miao L., Cai L. Prevention of diabetic complications by activation of Nrf2: diabetic cardiomyopathy and nephropathy. Experimental Diabetes Research. 2012;2012:7. doi: 10.1155/2012/216512.216512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sussan T. E., Biswal S. Ganguly N., Jindal S., Biswal S., Barnes P., Pawankar R. Studies on Respiratory Disorders. New York, NY, USA: Humana Press; 2014. Oxidative stress and respiratory diseases: the critical role of Nrf2; pp. 335–348. (Oxidative Stress in Applied Basic Research and Clinical Practice). [DOI] [Google Scholar]
- 13.Khor T. O., Huang M.-T., Kwon K. H., Chan J. Y., Reddy B. S., Kong A.-N. Nrf2-deficient mice have an increased susceptibility to dextran sulfate sodium–induced colitis. Cancer Research. 2006;66(24):11580–11584. doi: 10.1158/0008-5472.CAN-06-3562. [DOI] [PubMed] [Google Scholar]
- 14.Li J., Ichikawa T., Janicki J. S., Cui T. Targeting the Nrf2 pathway against cardiovascular disease. Expert Opinion on Therapeutic Targets. 2009;13(7):785–794. doi: 10.1517/14728220903025762. [DOI] [PubMed] [Google Scholar]
- 15.Barone M. C., Sykiotis G. P., Bohmann D. Genetic activation of Nrf2 signaling is sufficient to ameliorate neurodegenerative phenotypes in a Drosophila model of Parkinson’s disease. Disease Models & Mechanisms. 2011;4(5):701–707. doi: 10.1242/dmm.007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rangasamy T., Cho C. Y., Thimmulappa R. K., et al. Genetic ablation of Nrf2 enhances susceptibility to cigarette smoke–induced emphysema in mice. The Journal of Clinical Investigation. 2004;114(9):1248–1259. doi: 10.1172/JCI200421146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Enomoto A., Itoh K., Nagayoshi E., et al. High sensitivity of Nrf2 knockout mice to acetaminophen hepatotoxicity associated with decreased expression of ARE-regulated drug metabolizing enzymes and antioxidant genes. Toxicological Sciences. 2001;59(1):169–177. doi: 10.1093/toxsci/59.1.169. [DOI] [PubMed] [Google Scholar]
- 18.Ramos-Gomez M., Dolan P. M., Itoh K., Yamamoto M., Kensler T. W. Interactive effects of nrf2 genotype and oltipraz on benzo[a]pyrene–DNA adducts and tumor yield in mice. Carcinogenesis. 2003;24(3):461–467. doi: 10.1093/carcin/24.3.461. [DOI] [PubMed] [Google Scholar]
- 19.Kumar H., Kim I. S., More S. V., Kim B. W., Choi D. K. Natural product-derived pharmacological modulators of Nrf2/ARE pathway for chronic diseases. Natural Product Reports. 2014;31(1):109–139. doi: 10.1039/C3NP70065H. [DOI] [PubMed] [Google Scholar]
- 20.Shen T., Jiang T., Long M., et al. A curcumin derivative that inhibits vinyl carbamate-induced lung carcinogenesis via activation of the Nrf2 protective response. Antioxidants & Redox Signaling. 2015;23(8):651–664. doi: 10.1089/ars.2014.6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou M.-X., Wei X., Li A.-L., et al. Screening of traditional Chinese medicines with therapeutic potential on chronic obstructive pulmonary disease through inhibiting oxidative stress and inflammatory response. BMC Complementary and Alternative Medicine. 2016;16(1):p. 360. doi: 10.1186/s12906-016-1347-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen T., Chen X.-M., Harder B., et al. Plant extracts of the family Lauraceae: a potential resource for chemopreventive agents that activate the nuclear factor-erythroid 2-related factor 2/antioxidant response element pathway. Planta Medica. 2014;80(5):426–434. doi: 10.1055/s-0034-1368197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang X.-Z., Qian S.-S., Zhang Y.-J., Wang R.-Q. Salvia miltiorrhiza: a source for anti-Alzheimer’s disease drugs. Pharmaceutical Biology. 2016;54(1):18–24. doi: 10.3109/13880209.2015.1027408. [DOI] [PubMed] [Google Scholar]
- 24.Cui G., Shan L., Hung M., et al. A novel danshensu derivative confers cardioprotection via PI3K/Akt and Nrf2 pathways. International Journal of Cardiology. 2013;168(2):1349–1359. doi: 10.1016/j.ijcard.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Gao S., Liu Z., Li H., Little P. J., Liu P., Xu S. Cardiovascular actions and therapeutic potential of tanshinone IIA. Atherosclerosis. 2012;220(1):3–10. doi: 10.1016/j.atherosclerosis.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 26.Wang W., Guan C., Sun X., et al. Tanshinone IIA protects against acetaminophen-induced hepatotoxicity via activating the Nrf2 pathway. Phytomedicine. 2016;23(6):589–596. doi: 10.1016/j.phymed.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Su C.-Y., Ming Q.-L., Rahman K., HAN T., Qin L.-P. Salvia miltiorrhiza: traditional medicinal uses, chemistry, and pharmacology. Chinese Journal of Natural Medicines. 2015;13(3):163–182. doi: 10.1016/s1875-5364(15)30002-9. [DOI] [PubMed] [Google Scholar]
- 28.Wu W.-y., Wang Y.-p. Pharmacological actions and therapeutic applications of Salvia miltiorrhiza depside salt and its active components. Acta Pharmacologica Sinica. 2012;33(9):1119–1130. doi: 10.1038/aps.2012.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moi P., Chan K., Asunis I., Cao A., Kan Y. W. Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the beta-globin locus control region. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(21):9926–9930. doi: 10.1073/pnas.91.21.9926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitsuishi Y., Motohashi H., Yamamoto M. The Keap1–Nrf2 system in cancers: stress response and anabolic metabolism. Frontiers in Oncology. 2012;2 doi: 10.3389/fonc.2012.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li W., Kong A. N. Molecular mechanisms of Nrf2-mediated antioxidant response. Molecular Carcinogenesis. 2009;48(2):91–104. doi: 10.1002/mc.20465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lau A., Villeneuve N. F., Sun Z., Wong P. K., Zhang D. D. Dual roles of Nrf2 in cancer. Pharmacological Research. 2008;58(5-6):262–270. doi: 10.1016/j.phrs.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.An L., Zhou M., Marikar F. M. M. T., et al. Salvia miltiorrhiza lipophilic fraction attenuates oxidative stress in diabetic nephropathy through activation of nuclear factor erythroid 2-related factor 2. The American Journal of Chinese Medicine. 2017;45(7):1441–1457. doi: 10.1142/S0192415X17500781. [DOI] [PubMed] [Google Scholar]
- 34.Ge G., Zhang Q., Ma J., et al. Protective effect of Salvia miltiorrhiza aqueous extract on myocardium oxidative injury in ischemic–reperfusion rats. Gene. 2014;546(1):97–103. doi: 10.1016/j.gene.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 35.Bai B., Li Y. Danshen prevents articular cartilage degeneration via antioxidation in rabbits with osteoarthritis. Osteoarthritis and Cartilage. 2016;24(3):514–520. doi: 10.1016/j.joca.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Liu H.-Y., Jiang C.-T., Feng J., Wang X. Research progress of Tanshinones. Chinese Pharmacological Bulletin. 2016;32:1643–1647. [Google Scholar]
- 37.Jassbi A. R., Zare S., Firuzi O., Xiao J. Bioactive phytochemicals from shoots and roots of Salvia species. Phytochemistry Reviews. 2016;15(5):829–867. doi: 10.1007/s11101-015-9427-z. [DOI] [Google Scholar]
- 38.Zhang H., Luo L.-P., Song H.-P., et al. A high-resolution peak fractionation approach for streamlined screening of nuclear-factor-E2-related factor-2 activators in Salvia miltiorrhiza. Journal of Chromatography A. 2014;1326:47–55. doi: 10.1016/j.chroma.2013.12.042. [DOI] [PubMed] [Google Scholar]
- 39.Ma Z., Zhang M., Song Z. Characterization of tanshinones with quinone reductase induction activity from Radix Salvia miltiorrhiza by liquid chromatography/tandem mass spectrometry. Rapid Communications in Mass Spectrometry. 2009;23(18):2857–2866. doi: 10.1002/rcm.4195. [DOI] [PubMed] [Google Scholar]
- 40.Tao S., Zheng Y., Lau A., et al. Tanshinone I activates the Nrf2-dependent antioxidant response and protects against As(III)-induced lung inflammation in vitro and in vivo. Antioxidants & Redox Signaling. 2013;19(14):1647–1661. doi: 10.1089/ars.2012.5117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tao S., Justiniano R., Zhang D. D., Wondrak G. T. The Nrf2-inducers tanshinone I and dihydrotanshinone protect human skin cells and reconstructed human skin against solar simulated UV. Redox Biology. 2013;1(1):532–541. doi: 10.1016/j.redox.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jing X., Wei X., Ren M., Wang L., Zhang X., Lou H. Neuroprotective effects of tanshinone I against 6-OHDA-induced oxidative stress in cellular and mouse model of Parkinson’s disease through upregulating Nrf2. Neurochemical Research. 2016;41(4):779–786. doi: 10.1007/s11064-015-1751-6. [DOI] [PubMed] [Google Scholar]
- 43.de Oliveira M. R., Schuck P. F., Bosco S. M. D. Tanshinone I induces mitochondrial protection through an Nrf2-dependent mechanism in paraquat-treatedhuman neuroblastoma SH-SY5Y cells. Molecular Neurobiology. 2017;54(6):4597–4608. doi: 10.1007/s12035-016-0009-x. [DOI] [PubMed] [Google Scholar]
- 44.Wang L., Zhang C., Guo Y., et al. Blocking of JB6 cell transformation by tanshinone IIA: epigenetic reactivation of Nrf2 antioxidative stress pathway. The AAPS Journal. 2014;16(6):1214–1225. doi: 10.1208/s12248-014-9666-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang H.-S., Wang S.-Q. Nrf2 is involved in the effect of tanshinone IIA on intracellular redox status in human aortic smooth muscle cells. Biochemical Pharmacology. 2007;73(9):1358–1366. doi: 10.1016/j.bcp.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 46.Zhang X. S., Ha S., Wang X. L., Shi Y. L., Duan S. S., Li Z. A. Tanshinone IIA protects dopaminergic neurons against 6-hydroxydopamine-induced neurotoxicity through miR-153/NF-E2-related factor 2/antioxidant response element signaling pathway. Neuroscience. 2015;303:489–502. doi: 10.1016/j.neuroscience.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 47.Zhang L., Zhang H., Li X., et al. Miltirone protects human EA.hy926 endothelial cells from oxidized low-density lipoprotein-derived oxidative stress via a heme oxygenase-1 and MAPK/Nrf2 dependent pathway. Phytomedicine. 2016;23(14):1806–1813. doi: 10.1016/j.phymed.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 48.Yu J., Wang L., Akinyi M., et al. Danshensu protects isolated heart against ischemia reperfusion injury through activation of Akt/ERK1/2/Nrf2 signaling. International Journal of Clinical and Experimental Medicine. 2015;8(9):14793–14804. [PMC free article] [PubMed] [Google Scholar]
- 49.Fetoni A. R., Paciello F., Rolesi R., et al. Rosmarinic acid up-regulates the noise-activated Nrf2/HO-1 pathway and protects against noise-induced injury in rat cochlea. Free Radical Biology & Medicine. 2015;85:269–281. doi: 10.1016/j.freeradbiomed.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 50.Mao K., Shu W., Qiu Q., Gu Q., Wu X. Salvianolic acid a protects retinal pigment epithelium from OX-LDL-induced inflammation in an age-related macular degeneration model. Discovery Medicine. 2017;23:129–148. [PubMed] [Google Scholar]
- 51.Zhang H., Liu Y. Y., Jiang Q., et al. Salvianolic acid A protects RPE cells against oxidative stress through activation of Nrf2/HO-1 signaling. Free Radical Biology & Medicine. 2014;69:219–228. doi: 10.1016/j.freeradbiomed.2014.01.025. [DOI] [PubMed] [Google Scholar]
- 52.Zhang D.-F., Zhang J., Li R. Salvianolic acid B attenuates lung inflammation induced by cigarette smoke in mice. European Journal of Pharmacology. 2015;761:174–179. doi: 10.1016/j.ejphar.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 53.Zhou J., Qu X. D., Li Z. Y., et al. Salvianolic acid B attenuates toxin-induced neuronal damage via Nrf2-dependent glial cells-mediated protective activity in Parkinson’s disease models. PLoS One. 2014;9(7, article e101668) doi: 10.1371/journal.pone.0101668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin M., Zhai X., Wang G., et al. Salvianolic acid B protects against acetaminophen hepatotoxicity by inducing Nrf2 and phase II detoxification gene expression via activation of the PI3K and PKC signaling pathways. Journal of Pharmacological Sciences. 2015;127(2):203–210. doi: 10.1016/j.jphs.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 55.Chang C.-C., Chang Y.-C., Hu W.-L., Hung Y.-C. Oxidative stress and salvia miltiorrhiza in aging-associated cardiovascular diseases. Oxidative Medicine and Cellular Longevity. 2016;2016:11. doi: 10.1155/2016/4797102.4797102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen W., Chen G. Danshen (Salvia miltiorrhiza Bunge): a prospective healing sage for cardiovascular diseases. Current Pharmaceutical Design. 2017;23(34):5125–5135. doi: 10.2174/1381612823666170822101112. [DOI] [PubMed] [Google Scholar]
- 57.An Z., Yang G., Liu G., Zheng H., Li C., Zhang W. Novel insights on the vascular protective effects of tanshinone. International Journal of Clinical and Experimental Medicine. 2016;9:20711–20718. [Google Scholar]
- 58.Zhang Y., Jiang P., Ye M., Kim S. H., Jiang C., Lü J. Tanshinones: sources, pharmacokinetics and anti-cancer activities. International Journal of Molecular Sciences. 2012;13(12):13621–13666. doi: 10.3390/ijms131013621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guo Y., Li Y., Xue L., et al. Salvia miltiorrhiza: an ancient Chinese herbal medicine as a source for anti-osteoporotic drugs. Journal of Ethnopharmacology. 2014;155(3):1401–1416. doi: 10.1016/j.jep.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 60.Howden R. Nrf2 and cardiovascular defense. Oxidative Medicine and Cellular Longevity. 2013;2013:10. doi: 10.1155/2013/104308.104308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harrison D. G., Gongora M. C. Oxidative stress and hypertension. Medical Clinics of North America. 2009;93(3):621–635. doi: 10.1016/j.mcna.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 62.Zweier J. L. Measurement of superoxide-derived free radicals in the reperfused heart. Evidence for a free radical mechanism of reperfusion injury. Journal of Biological Chemistry. 1988;263(3):1353–1357. [PubMed] [Google Scholar]
- 63.Qiao Z., Ma J., Liu H. Evaluation of the antioxidant potential of Salvia miltiorrhiza ethanol extract in a rat model of ischemia-reperfusion injury. Molecules. 2011;16(12):10002–10012. doi: 10.3390/molecules161210002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu Z., Wang J., Huang E., et al. Tanshinone IIA suppresses cholesterol accumulation in human macrophages: role of heme oxygenase-1. Journal of Lipid Research. 2014;55(2):201–213. doi: 10.1194/jlr.M040394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhuang S., Cheng T.-H., Shih N.-L., et al. Tanshinone IIA induces heme oxygenase 1 expression and inhibits cyclic strain-induced interleukin 8 expression in vascular endothelial cells. The American Journal of Chinese Medicine. 2016;44(2):377–388. doi: 10.1142/S0192415X1650021X. [DOI] [PubMed] [Google Scholar]
- 66.Chan P., Chen Y.-C., Lin L.-J., et al. Tanshinone IIA attenuates H2O2-induced injury in human umbilical vein endothelial cells. The American Journal of Chinese Medicine. 2012;40(6):1307–1319. doi: 10.1142/S0192415X12500966. [DOI] [PubMed] [Google Scholar]
- 67.Zhu H., Chen Z., Ma Z., et al. Tanshinone IIA protects endothelial cells from H2O2-induced injuries via PXR activation. Biomolecules & Therapeutics. 2017;25(6):599–608. doi: 10.4062/biomolther.2016.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li Y.-I., Elmer G., LeBoeuf R. C. Tanshinone IIA reduces macrophage death induced by hydrogen peroxide by upregulating glutathione peroxidase. Life Sciences. 2008;83(15-16):557–562. doi: 10.1016/j.lfs.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang P., Wu X., Bao Y., et al. Tanshinone IIA prevents cardiac remodeling through attenuating NAD (P)H oxidase-derived reactive oxygen species production in hypertensive rats. Pharmazie. 2011;66(7):517–524. [PubMed] [Google Scholar]
- 70.Tang F., Wu X., Wang T., et al. Tanshinone II A attenuates atherosclerotic calcification in rat model by inhibition of oxidative stress. Vascular Pharmacology. 2007;46(6):427–438. doi: 10.1016/j.vph.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 71.Zhao W., Wu C., Chen X. Cryptotanshinone inhibits oxidized LDL-induced adhesion molecule expression via ROS dependent NF-κB pathways. Cell Adhesion & Migration. 2016;10(3):248–258. doi: 10.1080/19336918.2015.1119361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jia D., Li T., Chen X., et al. Salvianic acid A sodium protects HUVEC cells against tert-butyl hydroperoxide induced oxidative injury via mitochondria-dependent pathway. Chemico-Biological Interactions. 2018;279:234–242. doi: 10.1016/j.cbi.2017.10.025. [DOI] [PubMed] [Google Scholar]
- 73.Johnson D. A., Johnson J. A. Nrf2—a therapeutic target for the treatment of neurodegenerative diseases. Free Radical Biology & Medicine. 2015;88(Part B):253–267. doi: 10.1016/j.freeradbiomed.2015.07.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Buendia I., Michalska P., Navarro E., Gameiro I., Egea J., Leon R. Nrf2–ARE pathway: an emerging target against oxidative stress and neuroinflammation in neurodegenerative diseases. Pharmacology & Therapeutics. 2016;157:84–104. doi: 10.1016/j.pharmthera.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 75.Zhang H.-a., Gao M., Zhang L., et al. Salvianolic acid A protects human SH-SY5Y neuroblastoma cells against H2O2-induced injury by increasing stress tolerance ability. Biochemical and Biophysical Research Communications. 2012;421(3):479–483. doi: 10.1016/j.bbrc.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 76.Xia S.-F., Xie Z.-X., Qiao Y., et al. Salvianolic acid B counteracts cognitive decline triggered by oxidative stress in mice fed with high-fat diets. Journal of Functional Foods. 2014;11:278–292. doi: 10.1016/j.jff.2014.10.010. [DOI] [Google Scholar]
- 77.Bhakkiyalakshmi E., Sireesh D., Rajaguru P., Paulmurugan R., Ramkumar K. M. The emerging role of redox-sensitive Nrf2-Keap1 pathway in diabetes. Pharmacological Research. 2015;91:104–114. doi: 10.1016/j.phrs.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 78.Giacco F., Brownlee M. Oxidative stress and diabetic complications. Circulation Research. 2010;107(9):1058–1070. doi: 10.1161/CIRCRESAHA.110.223545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Uruno A., Furusawa Y., Yagishita Y., et al. The Keap1-Nrf2 system prevents onset of diabetes mellitus. Molecular and Cellular Biology. 2013;33(15):2996–3010. doi: 10.1128/MCB.00225-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Uruno A., Yagishita Y., Yamamoto M. The Keap1–Nrf2 system and diabetes mellitus. Archives of Biochemistry and Biophysics. 2015;566:76–84. doi: 10.1016/j.abb.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 81.Kang E. S., Lee G. T., Kim B. S., et al. Lithospermic acid B ameliorates the development of diabetic nephropathy in OLETF rats. European Journal of Pharmacology. 2008;579(1-3):418–425. doi: 10.1016/j.ejphar.2007.10.070. [DOI] [PubMed] [Google Scholar]
- 82.Lee B.-W., Chun S. W., Kim S. H., et al. Lithospermic acid B protects beta-cells from cytokine-induced apoptosis by alleviating apoptotic pathways and activating anti-apoptotic pathways of Nrf2–HO-1 and Sirt1. Toxicology and Applied Pharmacology. 2011;252(1):47–54. doi: 10.1016/j.taap.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 83.Yu X. Y., Zhang L., Yang X. Y., Li X. T., Du G. H. Salvianolic acid A improves intestinal motility in diabetic rats through antioxidant capacity and upregulation of nNOS. Journal of Digestive Diseases. 2016;17(7):441–447. doi: 10.1111/1751-2980.12363. [DOI] [PubMed] [Google Scholar]
- 84.Zoja C., Benigni A., Remuzzi G. The Nrf2 pathway in the progression of renal disease. Nephrology Dialysis Transplantation. 2014;29(Supplement 1):I19–I24. doi: 10.1093/ndt/gft224. [DOI] [PubMed] [Google Scholar]
- 85.You Z., Xin Y., Liu Y., et al. Protective effect of Salvia Miltiorrhizae injection on N(G)-nitro-D-arginine induced nitric oxide deficient and oxidative damage in rat kidney. Experimental and Toxicologic Pathology. 2012;64(5):453–458. doi: 10.1016/j.etp.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 86.Tongqiang L., Shaopeng L., Xiaofang Y., et al. Salvianolic acid B prevents iodinated contrast media-induced acute renal injury in rats via the PI3K/Akt/Nrf2 pathway. Oxidative Medicine and Cellular Longevity. 2016;2016:11. doi: 10.1155/2016/7079487.7079487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kim J., Cha Y.-N., Surh Y.-J. A protective role of nuclear factor-erythroid 2-related factor-2 (Nrf2) in inflammatory disorders. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 2010;690(1-2):12–23. doi: 10.1016/j.mrfmmm.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 88.Lee S. E., Jeong S. I., Yang H., et al. Extract of Salvia miltiorrhiza (Danshen) induces Nrf2-mediated heme oxygenase-1 expression as a cytoprotective action in RAW 264.7 macrophages. Journal of Ethnopharmacology. 2012;139(2):541–548. doi: 10.1016/j.jep.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 89.Chen T.-H., Hsu Y.-T., Chen C.-H., Kao S.-H., Lee H.-M. Tanshinone IIA from Salvia miltiorrhiza induces heme oxygenase-1 expression and inhibits lipopolysaccharide-induced nitric oxide expression in RAW 264.7 cells. Mitochondrion. 2007;7(1-2):101–105. doi: 10.1016/j.mito.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 90.Wang B., Sun J., Shi Y., Le G. Salvianolic acid B inhibits high-fat diet-induced inflammation by activating the Nrf2 pathway. Journal of Food Science. 2017;82(8):1953–1960. doi: 10.1111/1750-3841.13808. [DOI] [PubMed] [Google Scholar]
- 91.Shin S. M., Yang J. H., Ki S. H. Role of the Nrf2-ARE pathway in liver diseases. Oxidative Medicine and Cellular Longevity. 2013;2013:9. doi: 10.1155/2013/763257.763257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aleksunes L. M., Manautou J. E. Emerging role of Nrf2 in protecting against hepatic and gastrointestinal disease. Toxicologic Pathology. 2007;35(4):459–473. doi: 10.1080/01926230701311344. [DOI] [PubMed] [Google Scholar]
- 93.Liu J., Yang C. F., Lee B. L., Shen H. M., Ang S. G., Ong C. N. Effect of Salvia miltiorrhiza on aflatoxin B1-induced oxidative stress in cultured rat hepatocytes. Free Radical Research. 1999;31(6):559–568. doi: 10.1080/10715769900301131. [DOI] [PubMed] [Google Scholar]
- 94.Wu Z.-m., Wen T., Tan Y.-f., Liu Y., Ren F., Wu H. Effects of salvianolic acid A on oxidative stress and liver injury induced by carbon tetrachloride in rats. Basic & Clinical Pharmacology & Toxicology. 2007;100(2):115–120. doi: 10.1111/j.1742-7835.2007.00020.x. [DOI] [PubMed] [Google Scholar]
- 95.Guo J., Zhang Y., Zeng L., Liu J., Liang J., Guo G. Salvianic acid A protects L-02 cells against γ-irradiation-induced apoptosis via the scavenging of reactive oxygen species. Environmental Toxicology and Pharmacology. 2013;35(1):117–130. doi: 10.1016/j.etap.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 96.Ciencewicki J., Trivedi S., Kleeberger S. R. Oxidants and the pathogenesis of lung diseases. The Journal of Allergy and Clinical Immunology. 2008;122(3):456–468. doi: 10.1016/j.jaci.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Boutten A., Goven D., Artaud-Macari E., Boczkowski J., Bonay M. NRF2 targeting: a promising therapeutic strategy in chronic obstructive pulmonary disease. Trends in Molecular Medicine. 2011;17(7):363–371. doi: 10.1016/j.molmed.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 98.Liu B., Cao B., Zhang D., et al. Salvianolic acid B protects against paraquat-induced pulmonary injury by mediating Nrf2/Nox4 redox balance and TGF-β1/Smad3 signaling. Toxicology and Applied Pharmacology. 2016;309:111–120. doi: 10.1016/j.taap.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 99.Della Latta V., Cecchettini A., Del Ry S., Morales M. A. Bleomycin in the setting of lung fibrosis induction: from biological mechanisms to counteractions. Pharmacological Research. 2015;97:122–130. doi: 10.1016/j.phrs.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 100.Liu M., Xu H., Zhang L., et al. Salvianolic acid B inhibits myofibroblast transdifferentiation in experimental pulmonary fibrosis via the up-regulation of Nrf2. Biochemical and Biophysical Research Communications. 2018;495(1):325–331. doi: 10.1016/j.bbrc.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 101.Zhao Z., Chen Y., Wang J., et al. Age-related retinopathy in NRF2-deficient mice. PLoS One. 2011;6(4, article e19456) doi: 10.1371/journal.pone.0019456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hybertson B. M., Gao B., Bose S. K., McCord J. M. Oxidative stress in health and disease: the therapeutic potential of Nrf2 activation. Molecular Aspects of Medicine. 2011;32(4-6):234–246. doi: 10.1016/j.mam.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 103.Trouba K. J., Hamadeh H. K., Amin R. P., Germolec D. R. Oxidative stress and its role in skin disease. Antioxidants & Redox Signaling. 2002;4(4):665–673. doi: 10.1089/15230860260220175. [DOI] [PubMed] [Google Scholar]