Abstract
Objectives
To compare cone beam computed tomography (CBCT) and magnetic resonance tomography (MRT) in patients with temporomandibular joint (TMJ) arthralgia in respect of the evaluation of bony structures, and to correlate joint space distances measured in CBCT with the morphology and the position of the disc visualized in MRT.
Materials & methods
26 temporomandibular joints (TMJs) in 13 patients clinically diagnosed with TMJ arthralgia were examined by both CBCT and MRT. All images were evaluated by use of a form. The results were compared in regard of conformability of the diagnoses of osseous structures established by each imaging method. Anterior, superior and posterior joint space distances measured in CBCT-images were related to disc morphology and position visualized in MRT.
Results
Conformability of CBCT and MRT in the evaluation of bony TMJ structures ranged from 69.3 to 96.6 %. Osseous alterations such as erosions, osteophytes and cysts detected by CBCT could partly not be discerned by MRT. The correlation of joint space distances with disc morphology (biconcave or not biconcave) was not statistically significant. The correlation of joint space distances and disc position was statistically significant only for the superior joint distance.
Conclusion
CBCT outclasses MRT in the visualization of osseous alterations, which are diacritic in the differentiation of simple arthralgia from osteoarthritis. Therefore, CBCT imaging is appropriate in patients clinically diagnosed with TMJ arthralgia.
Superior joint space distance not being the highest joint space in sagittal CBCT indicates an anterior disc displacement.
For the visualization of structural changes or displacement of the disc frequently associated with osseous changes, MRT is the optimal tool. Thus, the combination of the two imaging methods allows a comprehensive diagnosis in TMJ arthralgia patients.
Keywords: Medical imaging, Dentistry
1. Introduction
In any field of medicine, a thorough anamnesis and a clinical exploration present the basic diagnostic measures in a patient seeking medical consultation. In dependence of the clinical findings, further tests or imaging techniques may be indicated in order to verify, specify or reject the preliminary diagnosis. In the assessment of temporomandibular joint disorders, diagnostic criteria have been established for clinical and research applications (Diagnostic Criteria for Temporomandibular Disorders, DC/TMD; Research Diagnostic Criteria for Temporomandibular Disorders, RDC/TMD) [1, 2]. (R)DC/TMD axis I relates to clinical TMD conditions such as muscle disorders (group I), disc displacements (group II) and arthralgia, arthritis and arthrosis (group III). Arthralgia has been defined as pain and tenderness in the joint capsule and/or the synovial lining of the TMJ (pain in the lateral pole and/or the posterior attachment during palpation plus one or more self-reports of pain in the region of the joint or in the joint during maximum unassisted opening or during assisted opening or during lateral excursion). For a diagnosis of simple arthralgia, coarse crepitus must be absent. Osteoarthritis has been defined as an inflammatory condition within the joint that results from a degeneration of the joint structures, and represents a combination of arthralgia plus coarse crepitus in the joint or plus one or more findings in TMJ imaging, such as erosion, sclerosis, flattening and osteophyte formation in joint surfaces. Osteoarthrosis, in contrast, has been defined as a non-painful degenerative disorder of the joint in which joint form and structure are abnormal. Coarse crepitus and/or osseous changes in imaging are indicative. Painful osteoarthritis may progress into osteoarthrosis. Uemura et al. have correlated roentgenological signs to the severity of degeneration, with erosive changes of the condyle representing an early stage and sclerosis of the articular fossa and/or eminence presenting severe destruction [3]. Thus, TMJ imaging is helpful in tracking disease progression and even necessary in the differential diagnosis of arthralgia and osteoarthritis.
Which imaging technique should be applied in which clinical diagnosis? The two modern imaging technologies CBCT and MRT, which are to be compared in this study, are based on entirely different principles.
CBCT has, for various indications, become standard equipment in dental offices. It is compact in size, easy to operate, and available for immediate imaging. In CBCT, a circular orbit of an X-ray source (forming a three dimensional (3D) cone shaped X-ray bundle) around the object creates a multitude of projection images which are acquired by a 2D detector and processed to 3D reconstructions by means of cone beam reconstruction algorithms. 3D imaging provides more detailed information on anatomic structures than conventional 2D X-ray examination, such as panoramic radiography or lateral cephalometry, albeit by delivering a considerably higher radiation dose [4]. Thereby, in CBCT imaging, a several to ten times lower radiation dose is used than in multislice CT [4, 5, 6, 7], which still represents the gold standard in the diagnosis of bony defects and fractures of the TMJ.CBCT has been proved to be precise enough to supply reliable and clinically relevant data of the TMJ [8, 9]. Ikeda and Kawamura determined the physiological position of the condyle in centric relation in the sagittal, coronal and axial plane in healthy probationers, in order to provide norms for the clinical assessment of condylar position obtained by CBCT [10, 11].
In MRT technique, an intense signal originates from a high number of protons (such as contained in water or soft tissue or liquids in the human body). This explains why MRT has its strengths mainly in soft tissue imaging [12, 13]. Usually six to eight sagittal slices are acquired with mouth shut and open, three of which (in the medial, central and lateral part of the joint) suffice in practice. T1-weighted MRT is optimal for the evaluation of anatomy and topography, whereas T2-weighting facilitates the diagnosis of inflammatory alterations or effusion [14]. MRT examination is devoid of the adverse effects of ionizing radiation. MRT is usually performed in centers only upon referral, and requires a longer imaging time than CBCT. Metallic foreign bodies, cardiac pacemakers, cochlea implants, vascular clips, etc. present contraindications for MRT imaging [15].
A comparative evaluation of CBCT and MRT images of the same joints was conducted in order to elaborate the strengths and shortcomings of each technique in the diagnosis of TMD.
2. Materials & methods
2.1. Subjects
The study group investigated in this retrospective analysis consists of 13 consecutive patients (10 females, 3 males; aged 18–59 years, mean age 38 ± 11.626 years), who presented in an orthodontic practice in Germany for clarification and treatment of a painful condition in the TMJ region in one side or both sides. All patients were clinically diagnosed with arthralgia (diagnosis III.a according to the RDC/TMD [2]) by one clinical examiner. Patients with a severe limitation of mouth opening (RDC/TMD diagnoses I.b, II.b) were excluded, whereas the (additional) clinical diagnoses myofascial pain (RDC/TMD diagnosis I.a) or disc displacement without limited opening (RDC/TMD diagnoses II.a, II.c) or the presence of coarse crepitus (RDC/TMD diagnosis III.b) were no exclusion criteria.
2.2. CBCT data acquisition
CBCT was performed at the orthodontic practice directly after the clinical examination in order to provide an immediate diagnosis of the osseous structures, the position of the condyle and spatial relationships.
CBCT imaging was performed with mouth shut (maximal intercuspidation) by “Picasso Trio” (Vatech) in mode “high” with a field of 12 cm × 7 cm and a scanning time of 24 seconds in a natural head position [16], by which the Frankfort horizontal plane and the upper and lower margin of the reconstructed images are parallel. Slice thickness was 0.15 mm. The data were stored and processed by a flat panel detector and downloaded by EZImplant CD Viewer.
2.3. MRT data acquisition
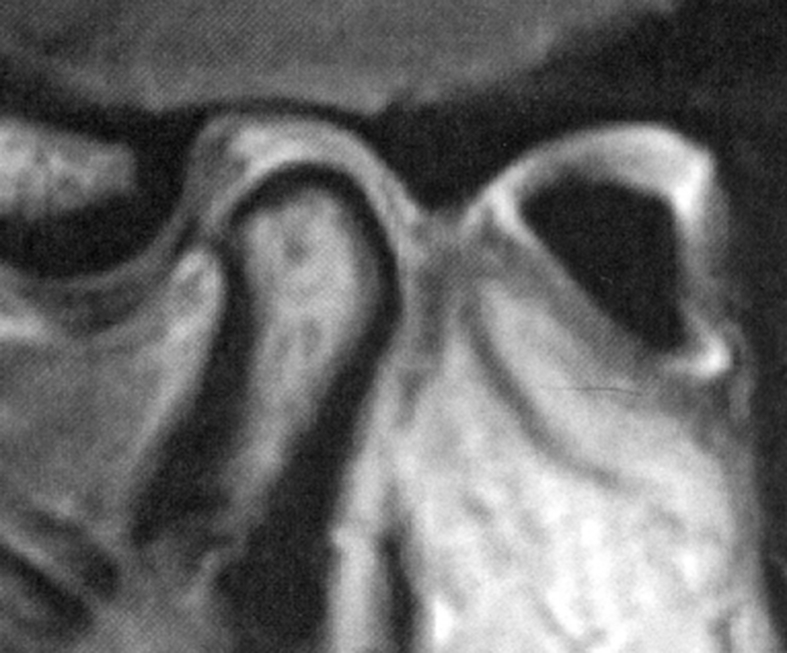
Depending on availability of appointments, MRT imaging was performed within a mean period of 19.92 ± 27.32 days (range 0–108 days) after the CBCT examination at a practice for radiology in order to visualize soft tissue structures. MRT imaging was performed in a lying position by the use of a high resolution surface coil in a magnetic field of 1.5 tesla. With mouth shut (maximum intercuspidation) (example, Fig. 1) and open, mouth-opening accomplished by means of a splint, T1-weighted sequences consisting of 10 sagittal slices of 3 mm thickness from lateral to medial were taken. The data were downloaded by Sectra CD Viewer.
Fig. 1.
MRT-image: Anterior disc displacement.
All TMJ imaging took place in Cologne, Germany, and was indicated as standard of care, in order to confirm and specify the clinical diagnosis as a basis for treatment planning, for documentation purposes and as a baseline for monitoring. Informed consent to the anonymous analysis of the data was obtained. Data evaluation was carried out at the Department of Operative and Restorative Dentistry, Innsbruck, in the course of a thesis approved by the Medical University of Innsbruck, in accordance with the Declaration of Helsinki on medical protocol and ethics and the guidelines of the ethical committee of the Medical University of Innsbruck.
2.4. Data analysis
2.4.1. Evaluation of CBCT and MRT images
The evaluation of all images was performed by one examiner with the help of a form, which had been set up in accordance with the standardized evaluation protocol of Ottl et al. [17]. It contains analysis criteria for the shape of the condyle (convex, pointed, flattened, concave, hypoplastic, deformed, fractured), the shape of the articular tubercle (regular, pointed, flattened), the compacta quality of the condyle (regular, erosion, osteophyte formation), the spongiosa quality of the condyle (regular, degeneration, cyst formation, inflammation, tumor), the morphology of the mandibular fossa (regular, erosion, osteophyte formation) and – for MRT images only – disc morphology (no evaluation possible, biconcave, biplanar, overall or marginally thickened, overall or centrally thinned, marginally flattened, deformed, plicated, spherical, perforated, destroyed/fragmented) and the disc position in the sagittal plane (closed mouth: superior, anterior, posterior; open mouth in case of disc displacement: reduction or no reduction).
The assignment of an identical diagnosis to osseous structures by CBCT and MRT was defined as “conformability” in the evaluation of the bony structures.
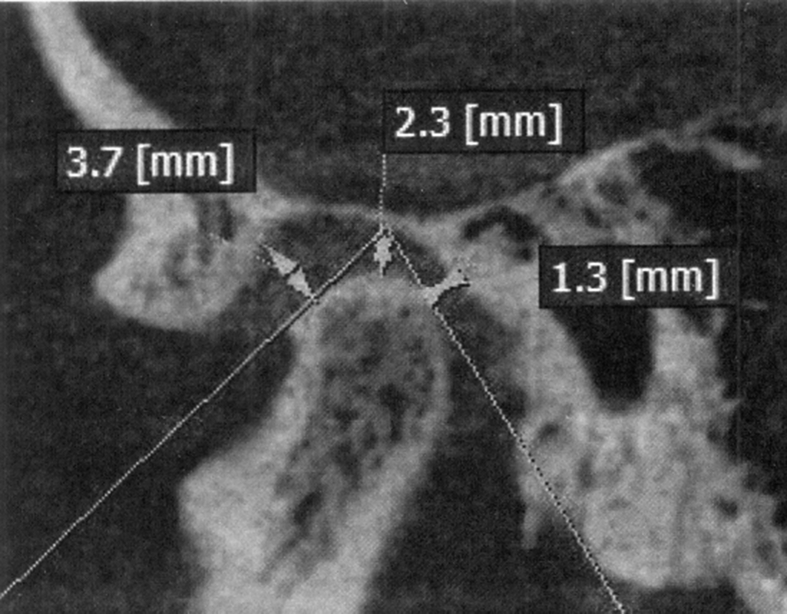
Joint space measurement in sagittal CBCT images was performed by means of the functions “ruler” and “tapeline” according to the method of Ikeda and Kawamura8: The sagittal plane dividing the longitudinal axis of the condyle in half was defined as the section which was used for measurement. The distance from the most superior point of the condyle to the most superior point of the mandibular fossa (in reference to the Frankfort horizontal plane) was determined as “superior space distance” (SS). From the most superior point of the fossa an anterior and a posterior tangent to the condyle were drawn in order to mark two points. From each of these two points an auxiliary straight line was drawn at right angle to the tangents. The distance between the point of intersection of the posterior auxiliary line and the fossa and the point of intersection of the posterior tangent and the condyle was defined as “posterior space distance” (PS), the “anterior space distance” was determined in an analogous way by the anterior tangent and the anterior auxiliary line (Fig. 2).
Fig. 2.
CBCT-image of the same joint as in Fig. 1: Determination of joint space distances.
Measurement of each image was performed three times at three different days by the same examiner. The mean value of the three measurements was used as the determined space distance. Intraexaminer reliability was assessed by use of the intraclass correlation coefficient (ICC), with ICCs > 0.75 being considered acceptable [18, 19].
2.4.2. Statistical evaluation
Comparison of the findings in CBCT- and MRT-images was accomplished by means of contingency tables.
For the draw up of tables and diagrams and for the statistical analysis the software SPSS 15.0 (SPSS Statistics, IBM, Chicago) was used.
The unpaired t-test was used to assess a correlation between joint space distances and disc morphology or disc position, respectively. Significance was set at p < 0.05.
3. Results
3.1. Comparison of CBCT and MRT images with respect to osseous structures
Condyle shape was conformably diagnosed in CBCT and MRT in 96.2% (n = 25): Convex in 57.7% (n = 15), deformed and flattened in 19.2 % (n = 5), pointed in 7.7% (n = 2), hypoplastic in 7.7% (n = 2), and deformed in 3.8% (n = 1).
In 3.8% (n = 1) condyle shape was diagnosed as convex in MRT, whereas it was diagnosed as flattened in CBCT.
The shape of the articular tubercle was classified conformably in 84.6% (n = 22): Regular in 69.2% (n = 18), flattened in 11.5% (n = 3), and pointed in 3.8% (n = 1).
In 15.4% (n = 4) the shape of the articular tubercle was classified as regular in MRT, whereas it was classified as pointed in CBCT.
Compacta quality of the condyle was assessed conformably in 69.3% (n = 18) (Table 1): Regular in 57.7% (n = 15), erosion and osteophyte formation in 7.7% (n = 2), osteophyte formation in 3.8% (n = 1).
Table 1.
Comparison of compacta quality of the condyle in CBCT- and MRT-images (n = 26).
| CBCT | MRT |
|||
|---|---|---|---|---|
| Regular | Osteophyte | Erosion and Ostheophyte | Total | |
| Regular | n = 15 (57.7%)∗ | n = 0 (0%) | n = 0 (0%) | n = 15 (57.7%) |
| Erosion | n = 5 (19.2%)† | n = 0 (0%) | n = 0 (0%) | n = 5 (19.2%) |
| Osteophyte | n = 2 (7.7%)† | n = 1 (3.8%)∗ | n = 0 (0%) | n = 3 (11.5%) |
| Erosion and Osteophyte | n = 0 (0%) | n = 1 (3.8%)† | n = 2 (7.7%)∗ | n = 3 (11.5%) |
| Total | n = 22 (84.6%) | n = 2 (7.7%) | n = 2 (7.7%) | n = 26 (100%) |
n, number.
(n = 18; 69.3%), conformability.
(n = 8; 30.7%), non-conformability.
In 26.9% (n = 7) compacta quality was classified as regular in MRT, whereas erosions were found in 19.2 % (n = 5) and osteophyte formation was found in 7.7% (n = 2) in CBCT. In 3.8% (n = 1) osteophyte formation only was assessed in MRT, whereas erosion and osteophyte formation was assessed in CBCT.
Spongiosa quality of the condyle was diagnosed with conformable results in 96.2% (n = 25): Regular in 80.8% (n = 21), degeneration in 11.5% (n = 3), degeneration and cyst formation in 3.8% (n = 1).
In 3.8% (n = 1) spongiosa quality was classified as regular in MRT, whereas cyst formation was detected in CBCT.
The morphology of the mandibular fossa was conformably classified as regular in 73.1% (n = 19).
In 26.9% (n = 7) the fossa was classified as regular in MRT, while CBCT visualized an erosion.
3.2. Soft tissue imaging by MRT
The morphology of the disc was classified as biconcave in 57,7% (n = 15) and as not biconcave in 42,3% (n = 11): overall thickened in 11.5% (n = 3), marginally thickened in 7.7% (n = 2), marginally flattened in 7.7% (n = 2), overall thinned in 3.8% (n = 1), destroyed in 3.8% (n = 1), biplanar in 3.8% (n = 1), deformed in 3.8% (n = 1).
The position of the disc was classified as superior in 50% (n = 13), as anterior without reduction in 30.8% (n = 8), and as anterior with reduction in 19.2% (n = 5).
Comparison of disc morphology right to left side (n = 13): In 53.8% (n = 7) disc morphology was biconcave in one side and not biconcave in the other side, in 30.8% (n = 4) disc morphology was bilaterally biconcave, and in 15.4% (n = 2) disc morphology was bilaterally not biconcave.
Comparison of disc position right to left side (n = 13): In 38.4% (n = 5) disc position was anterior in one side and superior in the other side, in 30.8% (n = 4) disc position was bilaterally superior, and in 30.8% (n = 4) disc position was bilaterally anterior.
3.3. Space distance measurements in CBCT images
Intraclass reliability (ICC) in the measurement of joint space distances was 0.92, and associated with a high reliability level.
Mean joint space distances measured in CBCT-images were: AS 2.58 ± 0.71 mm; SS 2.82 ± 0.78; and PS 2.25 ± 0.59 (Table 2).
Table 2.
Mean, minimum, and maximum joint space distances (mm) measured in CBCT-images.
| AS | SS | PS | |
|---|---|---|---|
| Mean + SD | 2.58 ± 0.71 | 2.82 ± 0.78 | 2.25 ± 0.59 |
| Minimum | 1.30 | 1.43 | 0.97 |
| Maximum | 3.83 | 4.37 | 3.73 |
AS, anterior space distance; SS, superior space distance; PS, posterior space distance; SD, standard deviation.
3.4. Correlation of space distances and disc morphology and position
The correlation of mean joint space distance measured in CBCT images and disc morphology (biconcave or not biconcave) assessed in MRT is depicted in Table 3.
Table 3.
Mean values of joint space distances (mm) in joints with biconcave and not biconcave discs.
| Disc morphology | n | Mean ± SD | |
|---|---|---|---|
| AS | Biconcave | 15 | 2.60 ± 0.54a |
| Not biconcave | 11 | 2.54 ± 0.92a | |
| SS | Biconcave | 15 | 3.05 ± 0.77b |
| Not biconcave | 11 | 2.50 ± 0.71b | |
| PS | Biconcave | 15 | 2.28 ± 0.50c |
| Not biconcave | 11 | 2.21 ± 0.72c |
AS, anterior space distance; SS, superior space distance; PS, posterior space distance; n, number; SD, standard deviation.
p = 0.84; unpaired t-test.
p = 0.77; unpaired t-test.
p = 0.77; unpaired t-test.
For neither joint space (AS, SS, or PS), a statistically significant correlation between mean joint space distance and disc morphology was found (unpaired t-test).
The correlation of mean joint space distance measured in CBCT-images and disc-position (superior or anterior) assessed in MRT (Table 4) was statistically significant only for SS, not for AS and PS. (Unpaired t-test).
Table 4.
Mean values of joint space distances (mm) in joints with a superior and joints with an anterior disc position.
| Disc position | n | Mean ± SD | |
|---|---|---|---|
| AS | Superior | 13 | 2.48 ± 0.47a |
| Anterior | 13 | 2.68 ± 0.90a | |
| SS | Superior | 13 | 3.23 ± 0.80b |
| Anterior | 13 | 2.41 ± 0.52b | |
| PS | Superior | 13 | 2.45 ± 0.63c |
| Anterior | 13 | 2.05 ± 0.49c |
AS, anterior space distance; SS, superior space distance; PS, posterior space distance; n number; SD, standard deviation.
p = 0.49; unpaired t-test.
p = 0.004; unpaired t-test.
p = 0.08; unpaired t-test.
4. Discussion
CBCT is - for various indications - more and more becoming standard equipment in dental offices and is thus easily available for immediate TMJ imaging. CBCT provides high geometric accuracy in the display of hard tissues and a good ratio between performance and low cost, together with a low radiation dose [20].
In case of arthralgia (RDC/TMD diagnosis III.a), a clinical condition of pain and tenderness of the joint capsule and/or the synovial lining of the TMJ, certain features in imaging (such as erosion of the normal cortical delineation, sclerosis of parts or all of the condyle and the articular eminence, flattening of joint surfaces and osteophyte formation) change the diagnosis into osteoarthrosis of the TMJ (RDC/TMD diagnosis III.b), an inflammatory condition within the joint that results from a degeneration of the joint structures [2]. In other words, the detection/presence of osseous changes impacts the clinical prognosis. Radiographic degenerative findings have been shown to induce changes in treatment strategy, which may be of benefit to the patients afflicted with osteoarthrosis [21]. CBCT monitoring may further be useful in tracking disease progression. Moreover, some authors have recommended CBCT-examination in TMD-patients with confirmed anterior disc displacement without reduction or disc deformity on MRT, who are at risk of having osseous abnormalities in the TMJ [22, 23].
This study provides evidence that CBCT outclasses MRT in the evaluation of bony structures. MRT and CBCT were conformable in the assessment of the shape of the condyle in 96.2%, of the shape of the articular tubercle in 84.6%. It seems that in the assessment of shape, in which only major structural changes are differentiated, the higher resolution of CBCT has little impact on the diagnosis.
In the diagnosis of compacta quality of the condyle, conformability of CBCT and MRT was found only in 69.3%. Erosions in particular could frequently not be visualized in MRT. This may be due to a better accuracy in detail in CBCT because of lower slice thickness (0.15 mm) as compared to MRT (3 mm). These findings correspond to investigations by Alkhader et al., who also stated a relatively low sensitivity of MRT for detecting osseous TMJ abnormalities such as surface irregularities [22].
Conformability of both imaging methods in the examination of spongiosa quality of the condyle was relatively high (96.2%), probably due to the fact that the majority of TMJs (80.8%) showed no damage in the spongiosa in CBCT.
While the mandibular fossa was classified as regular in all MRT images, erosions were visualized in 26.9 % in CBCT, conformability amounting to 73.1%.
Condylar erosions represent the early stage of degenerative changes, indicating that an active degenerative disease process associated with an inflammatory component may be occurring [3, 24]. Even though some authors have found no association between pain and an increased risk of degenerative findings in TMJ tomograms [25], others have assessed an association of (chronic) TMJ arthralgia and condylar erosion [26, 27, 28]. The presence of erosions may thus serve as a prognostic factor for disease progress or for treatment success or failure.
The second aim of this investigation was the correlation of the anterior, superior and posterior joint space distances with the morphology and the position of the disc. In the patients of this study, diagnosed with arthralgia, disc morphology was regularly biconcave in 57.7%, and the disc was in a physiological superior position in 50%, which confirms an association between soft tissue damage and osseous changes as described by other authors [22, 23]. Ikeda and Kawamura assessed the “optimal physiological” position of the condyle, with SS being the highest joint space distance in sagittal CBCT images in healthy male and female probationers at a mean age of 18 years (range 12–26 years).8 Lelis et al. also found SS to be the highest space distance in CBCT-based joint measurements in asymptomatic probationers (males and females, aged 18–25 years) in maximum intercuspidation and in centric relation by use of a different measuring method [29]. Kinniburgh et al. compared joint space distances in CBCT images of adolescent patients (males and females, mean age 13 years, range 7–20 years) with a normal disc position (highest joint space distance SS) and with anterior disc displacement without reduction verified by MRT (highest joint space distance AS), also measured by a different method [30]. Also in the present investigation, in joints with a superior disc position, SS was the highest joint space distance, whereas in joints with anterior disc displacement (with or without reduction) AS presented the highest joint space distance. These findings confirm that SS is the highest space distance in joints with a physiological position of the disc. This is due to the location of the thick posterior part of the disc in 12 o’ clock position. The thin biconcave intermediate part is physiologically located in the anterior, the bilaminar zone in the posterior joint space. In case of an anterior dislocation of the disc, the thick posterior part is located in the anterior joint space, and AS increases, the thin bilaminar zone is located in the superior joint space, thus SS decreases. With further (over-)extension of the posterior band and further anterior movement of the disc, the strained inferior part of the bilaminar zone is located in the anterior joint space, AS and PS decrease [31]. In brief, anterior disc displacement results in a decrease of SS and an increase or - in the natural course of further deterioration (the turn of anterior disc displacement with reduction into anterior disc displacement without reduction [32]) – a decrease of AS.
5. Conclusion
CBCT outclasses MRT in the visualization of osseous alterations in the TMJ. The detection of bony irregularities, such as erosions, flattening, deformity, sclerosis, and osteophyte formation, differentiates “simple” arthralgia (RDC/TMD diagnosis III.a) from osteoarthritis (RDC/TMD diagnosis III.b), and impacts the prognosis and patient management. Therefore, CBCT is suitable and diacritic in patients clinically diagnosed with TMJ arthralgia.
Superior joint space distance not being the highest joint space in sagittal CBCT indicates an anterior disc displacement.
For the visualization of the position and morphology of the disc, which are of particular interest in clinical RDC/TMD diagnoses II.b to c frequently associated with osseous alterations of the TMJ, MRT is the method of choice.
Thus, the combination of the two imaging methods is optimal for a comprehensive diagnosis in TMJ arthralgia patients.
Declarations
Author contribution statement
Dagmar Schnabl: Analyzed and interpreted the data; Wrote the paper.
Anna-Kathrin Rottler: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data.
Werner Schupp: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data.
Wolfgang Boisserée: Contributed reagents, materials, analysis tools or data.
Ingrid Grunert: Conceived and designed the experiments; Analyzed and interpreted the data.
Funding statement
The work was supported by the University Hospital for Dental Prosthetics and Restorative Dentistry of the Medical University of Innsbruck, Austria.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Schiffman E., Ohrbach R., Truelove E., Look J., Anderson G., Goulet J.P., List T., Svensson P., Gonzalez Y., Lobbezoo F., Michelotti A., Brooks S.L., Ceusters W., Drangsholt M., Ettlin D., Gaul C., Goldberg L.J., Haythornthwaite J.A., Hollender L., Jensen R., John M.T., De Laat A., de Leeuw R., Maixner W., van der Meulen M., Murray G.M., Nixdorf D.R., Palla S., Petersson A., Pionchon P., Smith B., Visscher C.M., Zakrzewska J., Dworkin S.F., International RDC/TMD Consortium Network, International Association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Fac. Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dworkin S., LeResche L. Research diagnostic criteria for temporomandibular disorders. J. Craniomandib. Disord.: Fac. Oral Pain. 1992;6:327–330. [PubMed] [Google Scholar]
- 3.Uemura S., Nakamura M., Iwasaki H., Fuchihata H. A roentgenological study on temporomandibular joint disorders. Morphological changes of TMJ in arthrosis. Dent. Radiol. 1979;19:224–237. [Google Scholar]
- 4.Qu X.M., Li G., Ludlow J.B., Zhang Z.Y., Ma X.C. Effective radiation dose of ProMax 3D cone-beam computerized tomography scanner with different dental protocols. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010;110:770–776. doi: 10.1016/j.tripleo.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Li G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci. Dent. 2013;43:63–69. doi: 10.5624/isd.2013.43.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loubele M., Bogaerts R., Van Dijck E., Pauwels R., Vanheuden S., Suetens P., Marchal G., Sanderink G., Jacobs R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur. J. Radiol. 2009;71:461–468. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Ludlow J.B., Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008;106:930–938. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 8.Zain-Alabdeen E.H., Alsadhan R.I. A comparative study of accuracy of detection of surface osseous changes in the temporomandibular joint using multidetector CT and cone beam CT. Dentomaxillofac. Radiol. 2012;41:185–191. doi: 10.1259/dmfr/24985971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Z.L., Cheng J.G., Li G., Zhang J.Z., Zhang Z.Y., Ma X.C. Measurement accuracy of temporomandibular joint space in Promax 3-dimensional cone-beam computerized tomography images. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012;114:112–117. doi: 10.1016/j.oooo.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda K., Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2009;135:495–501. doi: 10.1016/j.ajodo.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda K., Kawamura A., Ikeda R. Assessment of optimal condylar position in the coronal and axial planes with limited cone-beam computed tomography. J. Prosthodont. 2011;20:432–438. doi: 10.1111/j.1532-849X.2011.00730.x. [DOI] [PubMed] [Google Scholar]
- 12.Senna B.R., Dos Santos S.V.K., Franca J.P., Marques L.S., Pereira L.J. Imaging diagnosis of the temporomandibular joint: critical review of indications and new perspectives. Oral Radiol. 2009;25(2):86–98. [Google Scholar]
- 13.Petersson A. What you can and cannot see in TMJ imaging – an overview related to the RDC/TMD diagnostic system. J. Oral Rehabil. 2010;37:771–778. doi: 10.1111/j.1365-2842.2010.02108.x. [DOI] [PubMed] [Google Scholar]
- 14.Larheim T.A. Current trends in temporomandibular joint imaging. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995;80:555–576. doi: 10.1016/s1079-2104(05)80154-4. [DOI] [PubMed] [Google Scholar]
- 15.Ibrahim M.A., Dublin A.B. Contraindications. In: StatPearls, editor. Magnetic Resonance Imaging (MRI), Gadolinium. StatPearls Publishing; 2018. https://www.ncbi.nlm.nih.gov/Books/NBK482487/ [PubMed] [Google Scholar]
- 16.Lundström A., Lundström F., Lebret L.M., Moorrees C.F. Natural head position and natural head orientation: basic considerations in cephalometric analysis and research. Eur. J. Orthod. 1995;17:111–120. doi: 10.1093/ejo/17.2.111. [DOI] [PubMed] [Google Scholar]
- 17.Ottl P., Hohmann A., Piwowarczyk A., Hardenacke F., Lauer H.C., Zanella F. Retrospective study on the evaluation of the TMJ by MRI using a newly developed standardized evaluation form. J. Craniomandib. Pract. 2008;26:33–43. doi: 10.1179/crn.2008.005. [DOI] [PubMed] [Google Scholar]
- 18.Lin L.I. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:225–268. [PubMed] [Google Scholar]
- 19.Müller R., Büttner P. A critical discussion of intraclass correlation coefficients. Stat. Med. 1994;13:2465–2476. doi: 10.1002/sim.4780132310. [DOI] [PubMed] [Google Scholar]
- 20.Hashimoto K., Arai Y., Iwai K., Araki M., Kawashima S., Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003;95:371–377. doi: 10.1067/moe.2003.120. [DOI] [PubMed] [Google Scholar]
- 21.Wiese M., Wenzel A., Hintze H., Petersson A., Knutsson K., Bakke M., List T., Svensson P. Influence of cross-sectional temporomandibular joint tomography on diagnosis and management decisions of patients with temporomandibular joint disorders. J. Orofac. Pain. 2011;25:223–231. [PubMed] [Google Scholar]
- 22.Alkhader M., Kuribayashi A., Ohbayashi N., Nakamura S., Kurabayashi T. Usefulness of cone beam computed tomography in temporomandibular joints with soft tissue pathology. Dentomaxillofac. Radiol. 2010;39:343–348. doi: 10.1259/dmfr/76385066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moncada G., Cortes D., Millas R., Marholz C. Relationship between disk position and degenerative bone changes in temporomandibular joints of young subjects with TMD. An MRI study. J. Clin. Pediatr. Dent. 2014;38:269–276. doi: 10.17796/jcpd.38.3.w43m8474433n7ur2. [DOI] [PubMed] [Google Scholar]
- 24.Emshoff R. Pathophysiology of intracapsular inflammation and degeneration. In: Greene C.S., Laskin D.M., editors. Treatment of Temporomandibular Disorders: Bridging the Gap between Advance in Research and Clinical Patient Management. Quintessence Publishing; 2013. pp. 33–46.http://www.worldcat.org/title/treatment-of-tmds-bridging-the-gap-between-advances-in-research-and-clinical-patient-management/oclc/814440868 [Google Scholar]
- 25.Wiese M., Svensson P., Bakke M., List T., Hintze H., Petersson A. Associations between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J. Orofac. Pain. 2008;22:239–251. [PubMed] [Google Scholar]
- 26.Cevidanes L.H., Hajati A.K., Paniagua B., Lim P.F., Walker D.G., Palconet G. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010;110:110–117. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nah K.S. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci. Dent. 2012;42:249–253. doi: 10.5624/isd.2012.42.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emshoff R., Bertram F., Schnabl D., Stigler R., Steinmaßl O., Rudisch A. Condylar erosion in patients with chronic temporomandibular joint arthralgia: a cone beam computed tomography study. J. Oral Maxillofac. Surg. 2016;74 doi: 10.1016/j.joms.2016.01.029. 1343.e1-8. [DOI] [PubMed] [Google Scholar]
- 29.Lelis E.R., Guimaraes Henriques J.C., Tavares M., de Mendonca M.R., Fernandes Neto A.J., Almeida Gde A. Cone-beam tomography assessment of the condylar position in asymptomatic and symptomatic young individuals. J. Prosthet. Dent. 2015;114:420–425. doi: 10.1016/j.prosdent.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 30.Kinniburgh R.D., Major P.W., Nebbe B., West K., Glover K.E. Osseous morphology and spatial relationships of the temporomandibular joint: comparisons of normal and anterior disc positions. Angle Orthod. 2000;70:70–80. doi: 10.1043/0003-3219(2000)070<0070:OMASRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Rammelsberg P., Jäger L., Pho Duc J.M. Magnetic resonance imaging-based joint space measurements in temporomandibular joints with disk displacements and in controls. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000;90:240–248. doi: 10.1067/moe.2000.107361. [DOI] [PubMed] [Google Scholar]
- 32.Cai X.Y., Jin J.M., Yang C. Changes in disc position, disc length, and condylar height in the temporomandibular joint with anterior disc displacement: a longitudinal retrospective magnetic resonance imaging study. J. Oral Maxillofac. Surg. 2011;69:e340–e346. doi: 10.1016/j.joms.2011.02.038. [DOI] [PubMed] [Google Scholar]