Introduction
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a symptom complex associated with chronic pelvic pain in men after the exclusion of other confusable diseases, such as infection, malignancy, and benign prostatic hyperplasia (BPH). Prostatitis symptoms is a common reason for outpatient referral to the urologist, as up to 9% of Canadian men will experience some type of prostatitis symptoms (1/3 of these will report very bothersome symptoms to their physician) over the course of a year. These cases can constitute up to 2% of a urologist’s outpatient practice.
A proper diagnosis and evaluation in these men uses our general urologic skills and tools available to us in the outpatient clinic. The evaluation and workup need not be overly complex, but rather follow an organized approach while keeping in mind a few general principles that will aid in organizing an efficient and potentially successful management strategy.
Practice tips
Tip 1: Keep evaluation simple
Use the basic urologic principles of history (talk to the patient), physical exam (examine the patient, including the prostate and pelvic floor), and laboratory evaluation (urinalysis and urine culture) available in outpatient clinic — don’t be afraid to be a clinician! Managing these patients in a busy outpatient urologist’s office is doable and should not be more onerous than management of a BPH or overactive bladder (OAB) patient.
Tip 2: Does the patient have symptoms of CP/CPPS?
Symptoms include:
– Chronic pelvic pain in: perineum, testicles, tip of penis or below waist in pubic or bladder area
– Has it been present for at least three months?
Note: Unilateral orchalgia is not CP/CPPS; please see supplement publication on “Chronic scrotal contents pain” for further discussion of this condition.
Tip 3: Have you ruled out confusable and/or associated diseases?
These may include:
– Urinary tract infection (UTI) and bacterial prostatitis: History, urine culture
– BPH: Symptoms and size of prostate
– OAB: Storage symptoms with no pain
– Pelvic floor dysfunction: Trigger point or myofascial pain/spasm
– Malignancy: Urinalysis, cytology, +/− cystoscopy
– Determine contribution of pelvic floor dysfunctional pain: Physical exam
– Calculi: Nature of pain, urinalysis
– Interstitial cystitis/bladder pain syndrome (IC/BPS): Pain with bladder filling, relief with emptying
– Irritable bowel syndrome (IBS): Absominal/pelvic pain associated with diarrhea +/− constipation
Tip 4: Determine the clinical picture using the UPOINT phenotype tool
CP/CPPS is a heterogeneous patient population; identifying the patient phenotype is of utmost importance and will greatly impact management plan and outcomes. The UPOINT tool allows identification of up to six clinically defined domains and will help simplify the approach for the practitioner.
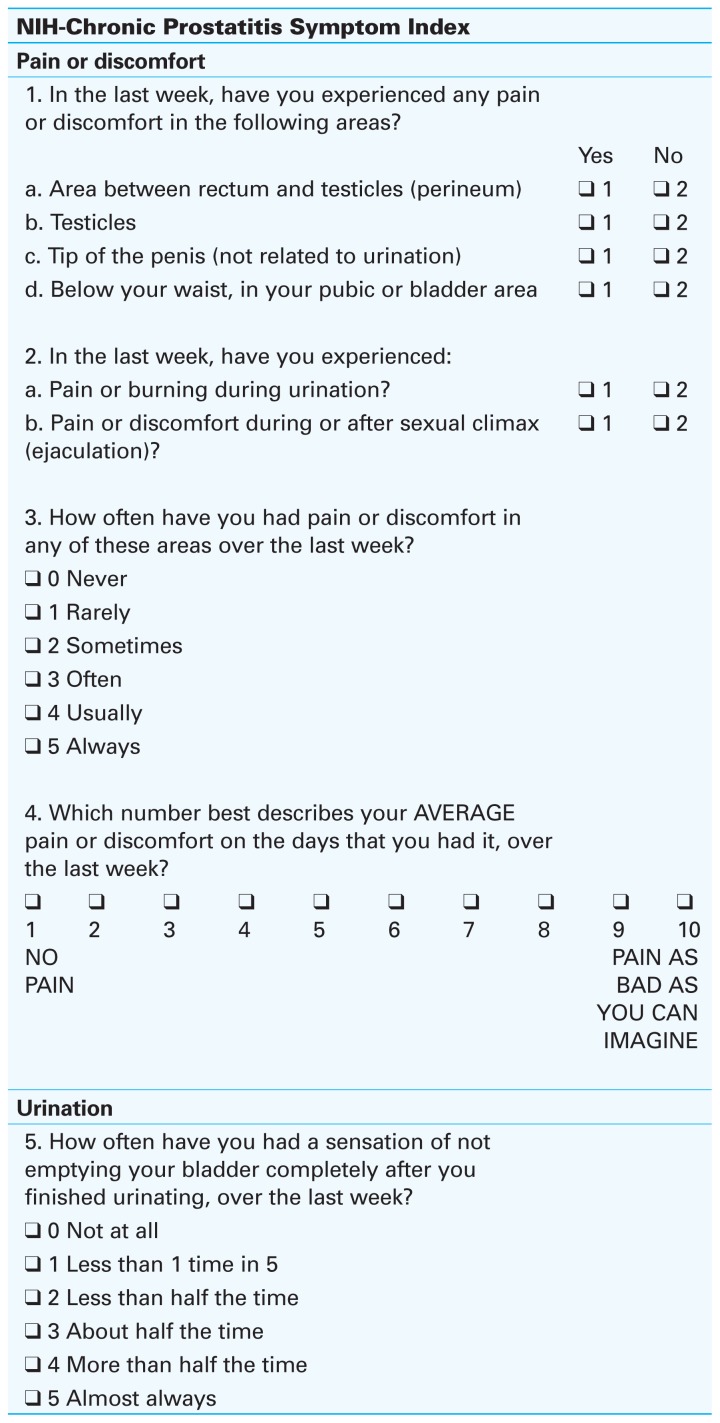
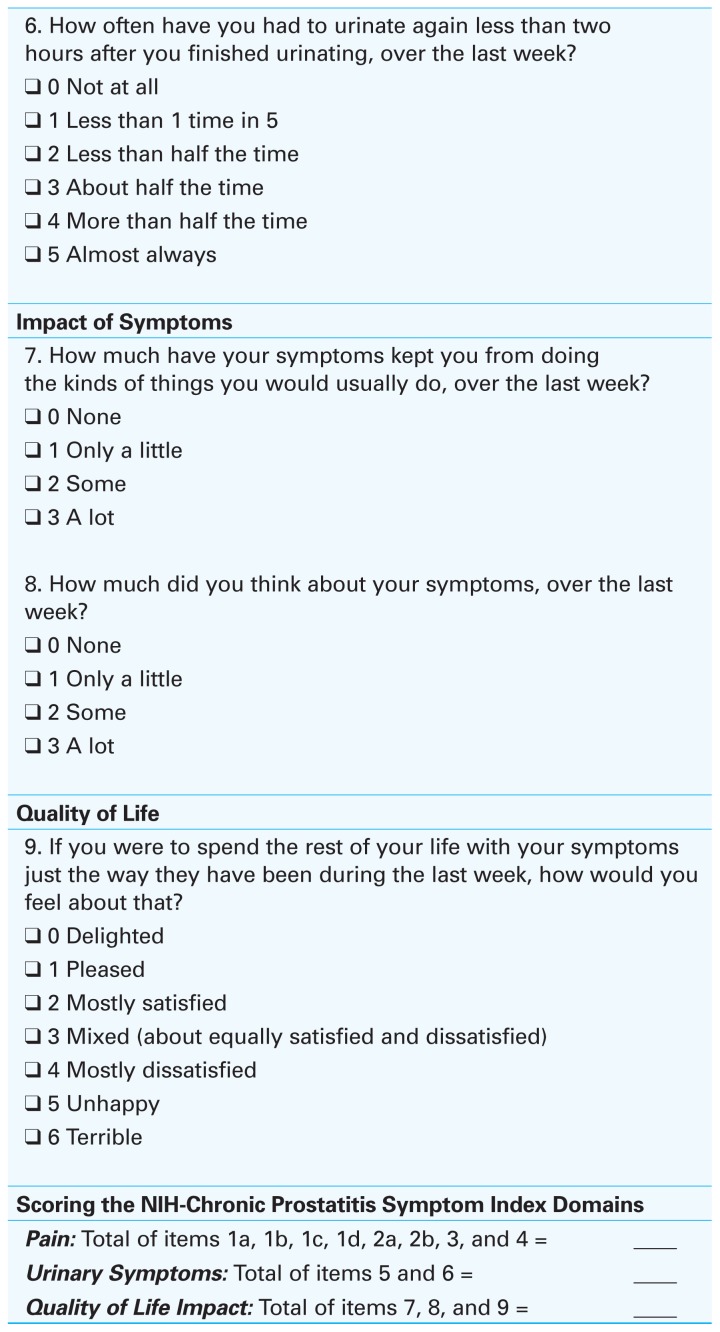
Tip 5: Quantitate symptoms using the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) tool (Fig. 1)
Fig. 1.
The NIH Chronic Prostatitis Symptom Index (CPSI) tool can be useful to first evaluate and then secondarily monitor patients’ progress and assess response to treatment (see “Recommended reading” for reference).
This simple, one-page index can be completed by patients in minutes during their outpatient visits and includes everything you need to know about their disease: location of pain, frequency, pain severity, urinary symptoms, and impact of symptoms on quality of life. This can be a useful tool to monitor progress and assess objective response to management plans.
Tip 6: Examine the patient
It is important to determine specific pain locations for your CP/CPPS patients, and also to rule out other abdominal or pelvic pathology. A careful pelvic floor examination performed prior to actual prostate palpation allows one to examine trigger points and pelvic floor spasm and tenderness more accurately.
Tip 7: Perform prostate massage
Chronic bacterial infection of the prostate (category II) must be ruled out. This is best achieved with a pre- and post-prostate massage urine test. Uropathogenic bacteria cultured in the post-prostate massage urine specimen or more colony counts in the post-prostatic massage specimen compared to the pre-prostate massage midstream urine specimen indicates that the patient may have a bacterial infection that could be managed with antimicrobial therapy.
Tip 8: Ancillary tests
Further ancillary tests, such as cystoscopy, urodynamics, and/or ultrasound (pelvic or transrectal) are indicated in selected patients:
– Failure to respond to treatment
– Complex cases
– Significant obstructive voiding symptoms
– Hematuria and/or suspicious urine cytology
– Pain referable to bladder (rule out IC/BPS, Hunner’s lesion)
– Severe pain on ejaculation (ejaculatory or prostate cysts, seminal vesicle pathology can sometimes only be identified by ultrasound)
– Urodynamics can be useful primarily to evaluate possibility of obstruction, e.g., bladder neck or detrusor sphincter dyssynergia
Summary
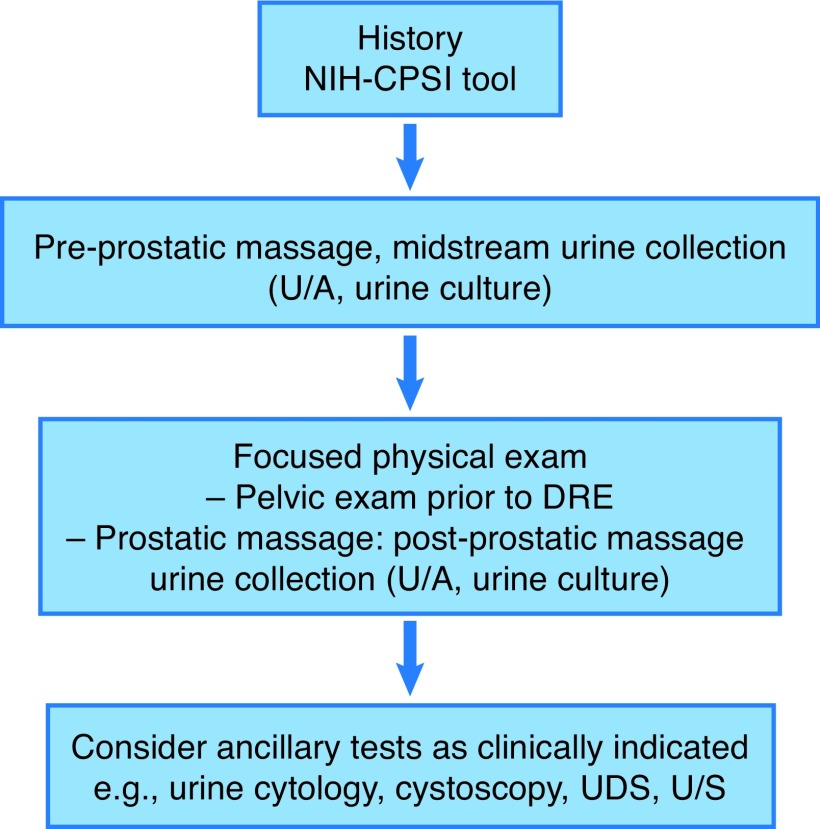
An accurate diagnosis and assessment (Fig. 2) of the clinical picture of each patient will allow successful, individualized phenotype-directed therapy.
Fig. 2.
A suggested evaluation algorithm for a patient presenting with chronic prostatitis/chronic pelvic pain syndrome. DRE: digital rectal exam; NIH-CPSI: National Institutes of Health Chronic Prostatitis Symptom Index; U/A: urinalysis; UDS: urodynamic studies; U/S: ultrasound.
Footnotes
Competing interests: Dr. Nickel has been a consultant for Astellas, Auxillium, Eli Lilly, Farr Labs, Ferring, GSK, Pfizer, Redleaf Pharma, Taris Biomedical, Tribute, and Trillium Therapeutics; a lecturer for Astellas and Eli Lilly; and has participated in clinical trials supported by Eli Lilly, GSK, J&J, Pfizer, and Taris Biomedical. Dr. Doiron reports no competing personal or financial conflicts related to this work.
This paper has been peer reviewed.
Recommended reading
- 1.Shoskes DA, Nickel JC, Dolinga R, et al. Clinical phenotyping of patients with chronic prostatitis/ chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009;73:538–42. doi: 10.1016/j.urology.2008.09.074. [DOI] [PubMed] [Google Scholar]
- 2.Litwin MS, McNaughton Collins M, Fowler MJ, et al. The NIH Chronic Prostatitis Symptom Index (NIH-CPSI): Development and validation of a new outcome measure. J Urol. 1999;162:369–75. doi: 10.1016/S0022-5347(05)68562-X. [DOI] [PubMed] [Google Scholar]
- 3.Nickel JC, Shoskes D, Wang Y, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006;176:119–24. doi: 10.1016/S0022-5347(06)00498-8. [DOI] [PubMed] [Google Scholar]
- 4.Nickel JC. Prostatitis. Can Urol Assoc J. 2011;5:306–15. doi: 10.5489/cuaj.686. [DOI] [PMC free article] [PubMed] [Google Scholar]