Abstract
Purpose
To report a case of submacular cystic lesion that turned out to be a sclerosing capillary hemangioblastoma. The retinal capillary hemangioblastoma may arise as a part of von Hippel-Lindau syndrome 1 however, they may occur as an isolated entity 2, but submacular capillary hemangioblastoma has never been reported.
Observations
A case of a 56-year-old female who presented with a right yellow submacular lesion. The mass was excised via pars-plana vitrectomy and histopathological assessment revealed a submacular sclerosing capillary hemangioblastoma.
Conclusion
and importance: The capillary hemangioblastoma is a benign vascular tumor that may arise submacularly and is not necessarily associated with von Hippel-Lindau disease. It is difficult to be differentiated clinically from other submacular lesions but the possibility should be considered.
Keywords: Capillary hemangioblastoma, Submacular lesions, von Hippel-Lindau
1. Case report
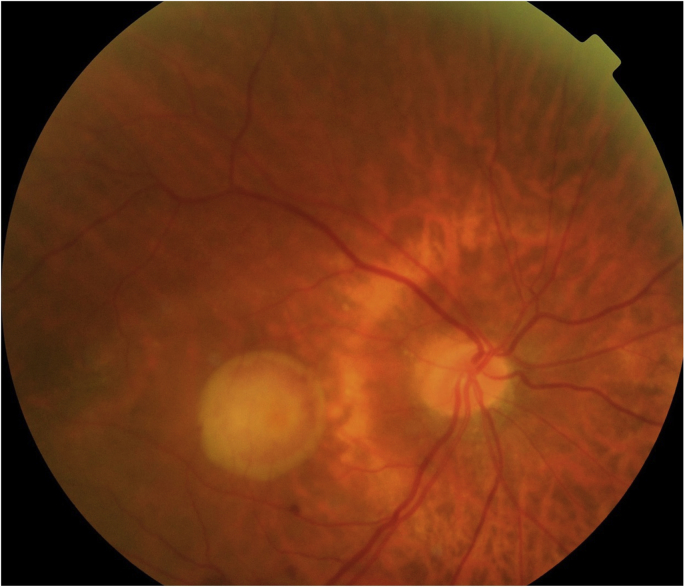
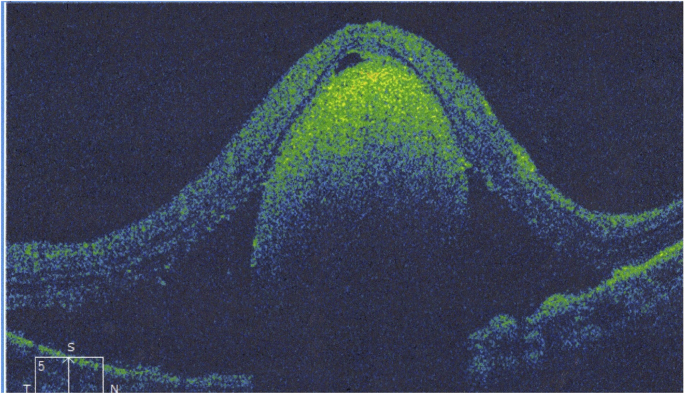
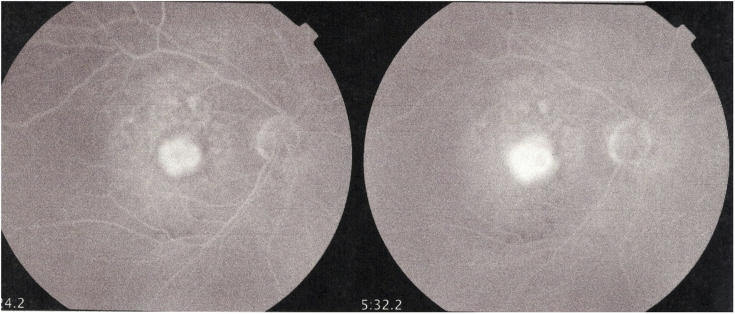
A fifty-six-year old female presented with a recent diminution of vision in the right eye of 3-months duration. The clinical evaluation revealed normal anterior segment, intact ocular motility and the visual acuity was counting fingers 27.5 inches. The fundus examination revealed a large round elevated submacular lesion with well-defined borders (Fig. 1). The Optical coherence tomography (OCT) revealed a well-defined large subfoveal lesion elevating the overlying retina (Fig. 2). The fluorescein angiography showed a hyperfluorescent lesion with a mild late leakage (Fig. 3). The examination of the left eye was unremarkable.
Fig. 1.
Fundus photography showing yellow submacular lesion. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Optical Coherence Tomography (OCT) showing submacular lesion elevating the overlying reina.
Fig. 3.
Fluorescein angiography demonstrated hyperfluorescent lesion with a mild late leakage.
An excisional biopsy was planned via a 23 gauge pars plana vitrectomy. Intraoperatively, a yellow round lesion was identified. It was well-defined with no firm adhesions to the optic nerve or the surrounding structures. It was possible to deliver the mass as one unit by enlarging the sclerotomy incision. It was a cystic soft yellowish-brown compressible lesion measuring 1 × 0.5 centimeters. The postoperative course was uneventful and the visual acuity of the patient improved to 0.1.
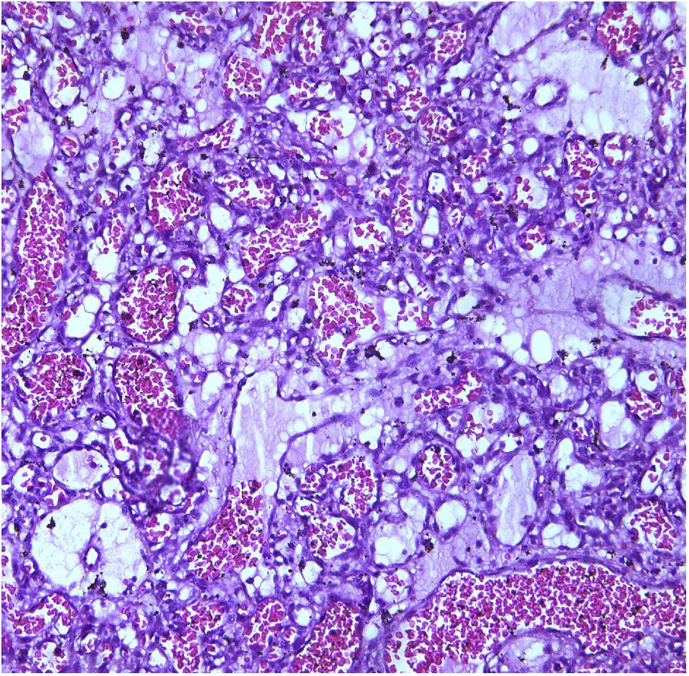
Histopathological examination demonstrated an angiomatous lesion formed of small vascular spaces lined by flat endothelial cells together with vacuolated stromal cells, however, there was no evidence of atypia, necrosis, specific infection or malignancy in all the examined sections (Fig. 4). A diagnosis of submacular sclerosing capillary hemangioblastoma was confirmed. The patient was referred to the medical oncology department for further systematic evaluation to exclude von-Hippel Lindau syndrome after pathology indicated the lesion to be a retinal capillary hemangioblastoma. Neuroimaging, urine analysis, renal ultrasonography were done and all results were normal.
Fig. 4.
Histopathologic examination showing small vascular spaces lined with flat endothelial cells.
2. Discussion
The sclerosing capillary angioma was first reported as a rare benign tumor arising from the lung, originating from pulmonary epithelium, hence the name ‘Pneumocytoma’ but it was a hemangioma rather than a hemangioblastoma.3 The retinal capillary hemangioblastoma is a rare tumor that may occur as an isolated lesion, but more commonly associated with von Hippel-Lindau syndrome.1,2 The tumor can be located anywhere in the fundus, with juxtapapilary site is common with early involvement of the macula with leakage and exudation. 4 The submacular location of sclerosing capillary hemangioblastoma has not been reported and to the best of our knowledge, this is the first case report at this abnormal location. We belive that the lesion originated from the underlying choroidal vasculature with subsequent sclerosis.
3. Conclusions
The retinal capillary hemangioblastomas are well-differentiated benign lesions that may affect vision through leakage, exudation and/or hemorrhage.4 Their presence in the submacular space is unique and has not been reported before.
The absence of these complications in our case may be related to sclerosis, however, it still affects vision due to its location with the disruption of the photoreceptors.
It represents a challenging situation to the surgeon excising this submacular lesion.
The clinical and systemic evaluation must be done to rule out associated von Hippel-Lindau disease.
Intellectual property
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Research ethics
We further confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Written consent to publish potentially identifying information, such as details or the case and photographs, was obtained from the patient(s) or their legal guardian(s).
Authorship
All listed authors meet the ICMJE criteria. We attest that all authors contributed significantly to the creation of this manuscript, each having fulfilled criteria as established by the ICMJE.
Patient consent
Written consent for publication of personal identifying information including medical record details and photographs was obtained from the patient.
Funding
No funding or grant support.
Conflicts of interest
The following authors have no financial disclosures:
Acknowledgments
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajoc.2018.05.010.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Maher E.R., Yates J.R., Harries R. Clinical features and natural history of von Hippel–Lindau disease. QJM. 1990;77:1151–1163. doi: 10.1093/qjmed/77.2.1151. [DOI] [PubMed] [Google Scholar]
- 2.Turell Mary E., Singh Arun D. Vascular tumors of the retina and choroid: diagnosis and treatment. Middle East Afr J Ophthalmol. 2010 Jul- Sep;17(3):191–200. doi: 10.4103/0974-9233.65486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baysaka Aysegul, Tolga Oz Adnan, Moğulkoç Nesrin, William Bishop Paul, Can Ceylan Kenan. A rare tumor of the lung: pulmonary sclerosing hemangioma (pneumocytoma) Respir Med. March 2013;107(Issue 3):448–450. doi: 10.1016/j.rmed.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Webster A.R., Maher E.R., Moore A.T. Clinical characteristics of ocular angiomatosis in von Hippel-Lindau disease and correlation with germline mutation. Arch Ophthalmol. 1999;117:371–378. doi: 10.1001/archopht.117.3.371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.