Abstract
A 9-year-old boy with primary myoclonus dystonia with comorbid severe attention deficit hyperactive disorder (ADHD) also had sleep onset and maintenance insomnia. Polysomnography showed features of non-rapid eye movement parasomnia. Daily bedtime clonidine helped sleep and hyperactivity. ADHD symptoms improved with 40 mg daily lisdexamphetamine mesylate. As the myoclonus and dystonia symptoms progressed, clonazepam was initiated at a dose of 0.5 mg daily at bedtime. It was anticipated that clonazepam would also improve parasomnia. Concomitant with the initiation of clonazepam, he developed a sleep-related eating disorder (SRED) continuing almost throughout the night. The symptoms went away upon stopping clonazepam. This is the first description of clonazepam producing SRED though it is the treatment of choice for this disorder.
Citation:
Ghosh D, Petrecca AM, Khuhro AL. Sleep-related eating disorder (SRED): paradoxical effect of clonazepam. J Clin Sleep Med. 2018;14(7):1261–1263.
Keywords: sleep-related eating disorder, SRED, clonazepam
INTRODUCTION
Clonazepam is a benzodiazepine derivative used to treat some sleep disorders, seizures and anxiety.1 Primary myoclonus dystonia2 responds only to the medications clonazepam and/or trihexiphenidyl. Sleep-related eating disorder (SRED) is characterized by the partial arousals from sleep to ingest food, and occurs usually within the first 3 hours of falling asleep.3 This disorder is a form of non-rapid eye movement (NREM) parasomnia4 similar to sleep terror. The patient does not have full memory of the events in the morning after waking. Clonazepam is used to treat parasomnias, SRED inclusive.3,4 Though total sleep duration is increased after using clonazepam, it reduces duration of slow wave sleep, and thereby improves parasomnias which happen during deeper slow wave sleep.3,4 The other mechanism behind the effect of clonazepam on parasomnia is an increase in arousal threshold as observed by Ferri et al.5 Clonazepam, commonly used to treat SRED3,4 has never been reported to produce those symptoms. In a child with primary myoclonus dystonia and associated insomnia, the addition of clonazepam to help with his myoclonus, dystonia and insomnia produced SRED persisting throughout the night. Once the clonazepam was removed, the SRED symptoms resolved with no further recurrence. This paradoxical response to clonazepam has not been reported so far.
REPORT OF CASE
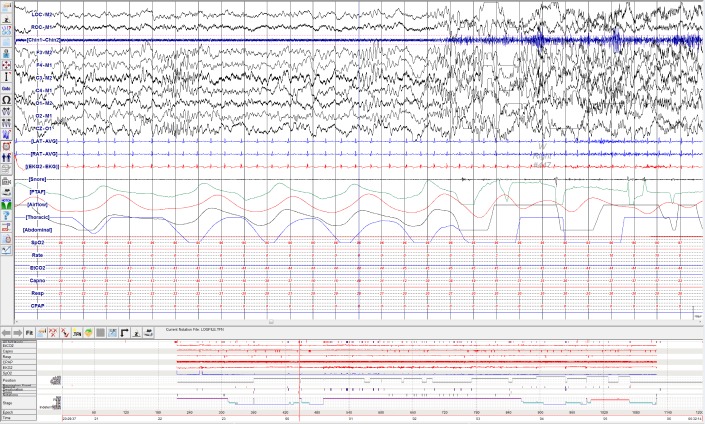
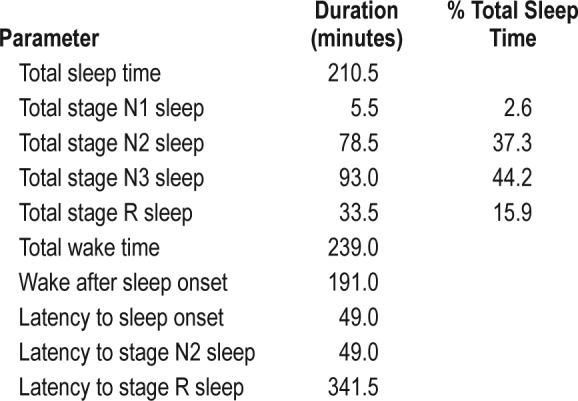
The patient was a 9-year-old boy who came in for a movement disorder neurology evaluation with tremor-like movements and muscle stiffening, more during activity. He was noted to have typical clinical features of primary myoclonus dystonia. He had significant comorbid conditions of severe attention deficit hyperactive disorder (ADHD) and insomnia. His ADHD was reasonably controlled with escalating dose of lisdexamphetamine, up to 40 mg every morning. He underwent polysomnography for insomnia; the study showed NREM parasomnia (Figure 1 and Video 1 in the supplemental material). Polysomnography showed a sleep efficiency of 47%; arousal index 4 events/h (total 15 arousals); apnea-hypopnea index 0 events/h; and periodic limb movement index 0 events/h. Additional relevant details of the study are noted in Table 1. His insomnia was reasonably controlled with clonidine at a dose of 0.1 mg before bedtime daily. The symptoms of myoclonus dystonia progressively worsened to produce difficulties in carrying on daily activities like use of spoon for eating, drinking from a cup without a straw, handwriting/drawing, buttoning/unbuttoning, and putting keys into locks. He also started falling while walking due to a combination of myoclonus and dystonia of the feet. Clinical examination was otherwise normal. His brain MRI was normal.
Figure 1. Polysomnography showing NREM parasomnia.
Polysomnography showed that the patient woke up from stage N2 sleep. It showed arousal in EEG, increased muscle activity in chin and leg which was associated with crying and body movement (noted in the audio/video component of polysomnography, Video 1). The above features are consistent with the diagnosis of NREM parasomnia. EEG = electroencephalography, NREM = non-rapid eye movement.
Table 1.
Summary of polysomnography parameters.
As the myoclonus and dystonia symptoms were producing significant disability, clonazepam was started at a dose of 0.5 mg daily before bedtime with instruction for slow upward titration. Concomitant with initiation of clonazepam, the child was noted to have multiple daily episodes of nocturnal sleep eating behavior continuing intermittently almost throughout the night starting from about an hour after falling asleep. This behavior was never noted prior to starting the medication. During a typical spell, while sleeping at his bedroom, he would come out of sleep and try to go to the refrigerator which was kept in the basement. Because sleep walking had occured in the past in this child and his sister, his mother kept the basement locked so that the children could not access the basement during sleep. Though apparently awake, he would be only partly responsive; he would walk up to his mother's room and ask for food. When his mother would bring him food, she noticed that the patient would eat very quickly, which was not his usual eating behavior when awake. No agitation was noted; however, his mother did not try to stop him from eating. She was seriously concerned about the possibility of choking as the patient would remain partly responsive during eating. He would not have any memory of the events upon awakening in the morning. Symptoms started only after starting clonazepam so this medication was stopped. The SRED symptoms completely went away with discontinuation of clonazepam and did not return over more than a year of follow up while off clonazepam. There was no change in other medication during that period.
Trihexiphenidyl was introduced for control of myoclonus and dystonia with partial benefit of the symptoms, and currently he is being considered for bilateral globus pallidus pars interna deep brain stimulation to control motor symptoms of myoclonus and dystonia.
DISCUSSION
Clonazepam is a benzodiazepine derivative that acts on gamma-aminobutyric acid (GABA) receptors in the brain. Benzodiazepines enhance the GABA neurotransmission, thus working as sedative, anti-anxiety, and muscle relaxant medication.1 Clonazepam is also used to help control seizures,1 and is one of the two effective medical treatment options for primary myoclonus dystonia.2 SRED symptoms may have significant impact in life through risk of choking, excess eating with its obvious consequences, and poor sleep efficiency with consequent excessive daytime sleepiness.3,6–13 Clonazepam is used to treat parasomnias, SRED inclusive.3,4 GABAergic effect underlies efficacy against SRED. Shorter acting benzodiazepines have rarely been known to produce phenomena akin to sleep walking/wandering, but there is no report of SRED as a complication.13 SRED has been well described as a side effect from psychotropic medications like olanzapine,6 risperidone,7 and quetiapine.8 For reasons not completely clear, SRED symptoms have also been observed as side effects to sedative medications like mirtazapine (with significant antidepressant and anti-anxiety activity),9 and zolpidem.10 Hoque and Chesson described an adult developing sleep walking, SRED, and sleep driving after starting zolpidem which improved upon its discontinuation. The authors did pre- and post-zolpidem fluorodeoxyglucose-positron emission tomography scan of brain without any specific changes.11 The authors postulated a possible cerebral pattern generator being disinhibited after using zolpidem to cause these NREM events.11 Even sodium oxybate,12 used to treat narcolepsy, has been observed to produce this side effect of SRED.
We did not come across any prior report of SRED as a side effect of clonazepam. The association is strongly proven in our case. He did not have any such symptom prior to use of clonazepam. Then he developed classic symptoms of SRED following introduction of clonazepam, and the symptoms disappeared upon its discontinuation. This phenomenon is completely different from sleep-related hyperphagia, which is characterized by clear recollection of the event upon awakening. At baseline, the child had other NREM parasomnias as noted in his polysomnography (Figure 1 and Video 1). On follow-up over more than a year, he did not have any recurrence of SRED symptoms while off clonazepam and with no change in his clonidine and lisdexamphetamine dose. The paradoxical phenomenon observed in our case is similar to many other neurological or psychiatric conditions where the specific treatment of a particular disorder may also produce the same manifestation of the disorder. Steroid and idiopathic intracranial hypertension, some anti-seizure medications and seizure recurrence, some antidepressants and worsening depression are some of the examples. The mechanism behind this paradoxical response to clonazepam is subject to conjectures. We think it is very pertinent to share this knowledge among neurologists and sleep medicine specialists to increase the awareness about this occurrence to help manage future patients who may experience similar side effects from clonazepam.
CONCLUSIONS
In summary, although clonazepam is widely used to treat sleep disorders, including SRED, our patient's SRED symptoms started only after clonazepam was introduced and disappeared upon its discontinuation. This paradoxical phenomenon has not been described earlier in literature.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The authors report no conflicts of interest.
REFERENCES
- 1.Cohen LS, Rosenbaum JF. Clonazepam: new uses and potential problems. J Clin Psychiatry. 1987;48(Suppl):50–56. [PubMed] [Google Scholar]
- 2.Ghosh D, Indulkar S. Primary myoclonus-dystonia: a diagnosis often missed in children. J Child Neurol. 2013;28:1418–1422. doi: 10.1177/0883073813488677. [DOI] [PubMed] [Google Scholar]
- 3.Chiaro G, Caletti MT, Provini F. Treatment of sleep-related eating disorder. Curr Treat Options Neurol. 2015;17(8):33. doi: 10.1007/s11940-015-0361-6. [DOI] [PubMed] [Google Scholar]
- 4.Horváth A, Papp A, Szűcs A. Progress in elucidating the pathophysiological basis of nonrapid eye movement parasomnias: not yet informing therapeutic strategies. Nat Sci Sleep. 2016;8:73–79. doi: 10.2147/NSS.S71513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferri R, Zucconi M, Marelli S, Plazzi G, Schenck CH, Ferini-Strambi L. Effects of long-term use of clonazepam on nonrapid eye movement sleep patterns in rapid eye movement sleep behavior disorder. Sleep Med. 2013;14(5):399–406. doi: 10.1016/j.sleep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Paquet V, Strul J, Servais L, Pelc I, Fossion P. Sleep-related eating disorder induced by olanzapine. J Clin Psychiatry. 2002;63(7):597. doi: 10.4088/jcp.v63n0710d. [DOI] [PubMed] [Google Scholar]
- 7.Lu ML, Shen WW. Sleep-related eating disorder induced by risperidone. J Clin Psychiatry. 2004;65(2):273–274. doi: 10.4088/jcp.v65n0220a. [DOI] [PubMed] [Google Scholar]
- 8.Heathman JC, Neal DW, Thomas CR. Sleep-related eating disorder associated with quetiapine. J Clin Psychopharmacol. 2014;34(5):658–660. doi: 10.1097/JCP.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 9.Jeong JH, Bahk WM. Sleep-related eating disorder associated with mirtazapine. J Clin Psychopharmacol. 2014;34(6):752–753. doi: 10.1097/JCP.0000000000000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morgenthaler TI, Silber MH. Amnestic sleep-related eating disorder associated with zolpidem. Sleep Med. 2002;3(4):323–327. doi: 10.1016/s1389-9457(02)00007-2. [DOI] [PubMed] [Google Scholar]
- 11.Hoque R, Chesson AL. Zolpidem-induced sleepwalking, sleep related eating disorder, and sleep-driving: fluorine-18-flourodeoxyglucose positron emission tomography analysis, and a literature review of other unexpected clinical effects of zolpidem. J Clin Sleep Med. 2009;5(5):471–476. [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace DM, Maze T, Shafazand S. Sodium oxybate-induced sleep driving and sleep-related eating disorder. J Clin Sleep Med. 2011;7(3):310–311. doi: 10.5664/JCSM.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lauerma H. Nocturnal wandering caused by restless legs and short-acting benzodiazepines. Acta Psychiatr Scand. 1991;83:492–493. doi: 10.1111/j.1600-0447.1991.tb05581.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.