Abstract
Study Objectives:
To validate Impulse radio ultra wideband pulse-doppler radar technology against polysomnography (PSG) for sleep assessment.
Methods:
In all, 12 participants were recruited and their overnight sleep was assessed both by a Novelda XeThru radar and PSG. Two subjects had two nightly recordings, whereas 10 had one recording. Epoch by epoch (30 seconds) comparisons from bedtime to rise time were conducted. Concordance was estimated in terms of the mean difference between the radar and the PSG estimates regarding sleep onset latency, wake time after sleep onset and total sleep time. In addition, accuracy, sensitivity, specificity and Cohen kappa were calculated.
Results:
The mean difference (minutes) between the radar and the PSG registrations was −5.7 minutes (standard deviation [SD] = 22.1 minutes) for sleep onset latency, 6.4 minutes (SD = 32.5 minutes) for wake after sleep onset, and 1.5 minutes (SD = 24.6 minutes) for total sleep time. The mean values obtained for accuracy, sensitivity, specificity and Cohen kappa were 0.931, 0.961, 0.695 and 0.670, respectively.
Conclusion:
Impulse radio ultra wideband radar technology is a promising tool in terms of affordable and practical objective sleep assessment. Further technical development and more validation studies are needed in order to conclude about the utility potential of this device.
Citation:
Pallesen S, Grønli J, Myhre K, Moen F, Bjorvatn B, Hanssen I, Heglum HS. A pilot study of impulse radio ultra wideband radar technology as a new tool for sleep assessment. J Clin Sleep Med. 2018;14(7):1249–1254.
Keywords: radar, pulse doppler, validation, polysomnography, sleep assessment, methodology
INTRODUCTION
The standard technique for scientifically and clinically studying sleep is polysomnography (PSG), consisting of a comprehensive recording of multiple electrophysiological parameters during sleep.1 PSG has clear benefits for monitoring sleep quantity and quality, but also suffers from several practical limitations, related to cost, skills and time. Actigraphy prevails today as the device that over time has been established as an affordable and easy-to-operate alternative to PSG and consists of wrist-worn devices that contain, inter alia, an accelerometer, a clock, and a data storing unit.2 Validation by the use of correlations between sleep parameters harvested from actigraphic and PSG recordings are typically inflated, even when the epoch-by-epoch agreement is relatively low, since most of the data normally come from the sleep period.3 Validation in terms of sensitivity (actigraphy = sleep when PSG = sleep), accuracy (actigraphy = sleep/wake when PSG = sleep/wake), and specificity (actigraphy = wake when PSG = wake) demonstrate that the participant-specific sensitivity and accuracy are high, whereas the specificity is low.4
Radar technology has been proposed as a tool that has a great potential for monitoring and measuring subtle body movement (eg, by thorax and limbs).5 In this study, we present the results from a pilot investigation where impulse radio ultra wideband (UWB) pulse-Doppler technology was used to estimate wakefulness and sleep. UWB technology is based on radio waves with very low energy levels at short range. This technology rests on the principle that body, limb and respiratory movements of a person cause changes of the frequency (Doppler shift) of the radio waves. The results of radar data were in the present study compared to outputs from PSG recordings.
METHODS
A total of 12 persons, (6 males, 6 females) with a mean age of 34.4 years (standard deviation [SD] = 11.9, range 19–60 years) were recruited.
Polysomnography
Electrodes were montaged (including F4-M1, C4-M1, O2-M1, left and right electrooculogram, and electromyogram submentalis) and analyzed according to The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications.6 Sleep was scored according to American Academy of Sleep Medicine guidelines by trained personnel.
Impulse Radio Ultra Wideband Radar (IR-UWB Radar)
The radar device used was the Novelda XeThru model X2,7 an IR-UWB pulse-Doppler radar. The size of the radar chip itself is 5 × 5 mm, suitable for integration in portable devices. The radar has an average sampling rate of 39 giga samples per second, which is downconverted to 20 frames per second.
The term “ultra wideband” (UWB) is used to refer to the 3.1–10.6 GHz band of radio frequency waves. The UWB frequency band was released for unlicensed use by the United States Federal Communications Commission (FCC) in 2002, providing that emission levels are kept low (−41.3 dBm/MHz).8 The Novelda XeThru model X2 has been tested in an approved laboratory and submitted to FCC for approval of certification (FCC-ID: 2AD9QX4M02).
This large bandwidth enables high spatial resolution. The high frequency waves will easily penetrate soft materials such as clothes and beddings, but are less able to travel through more solid objects (eg, walls, human bodies), which instead cause reflections.9
As radio waves travel at the speed of light, the time-of-flight of the signals is very short which requires high speed demands of the system. The present radar addresses this difficulty by employing a concept known as strobed sampling. Here, several samplers are arranged in a parallel topology and employing a swift threshold sweep. For further details of the idiosyncrasies of the present radar, the reader is referred to Wisland et al.8
Pulse-Doppler Signal Processing
The waves emitted by the radar are reflected from objects (such as a breathing person beneath a blanket) in its surroundings and the reflections are detected by the receiver. If the reflecting object is moving, a frequency shift can be observed in the reflected wave. This phenomenon is commonly known as the Doppler effect, often observed with sound waves in everyday life. The effect is the same when the waves are electromagnetic, albeit on a smaller scale. Even tiny body motions, such as a thoracic activity by inhalation and exhalation as well as heart beats, produce changes in frequency of the reflected signals.10
The pulse-Doppler radar measures both the time-of-flight and the Doppler shift in the frequency of the received signals. Time-of-flight is given by the distance to the movements, measured in nanoseconds. The Doppler shift in the frequency provides information about its velocity.
A measure of total body movement, as well as information about frequency of respiration, is obtained from the received radar signals by forming range-frequency-power matrices referred to as pulse-Doppler matrices. These are generated by performing a short-time fast Fourier transform (FFT) on data from each 5-cm distance increment in the radar's range, using two different-length Hanning windows to different effect. A “fast” (3-second) window is used to estimate total body movement, and a “slow” (20-second) window is used to estimate respiration frequency. The windows are shifted and the FFT repeated every second, ie, 33% overlap for body movements and 95% overlap for respiration, giving movement and respiration information with an update rate of 1 Hz.
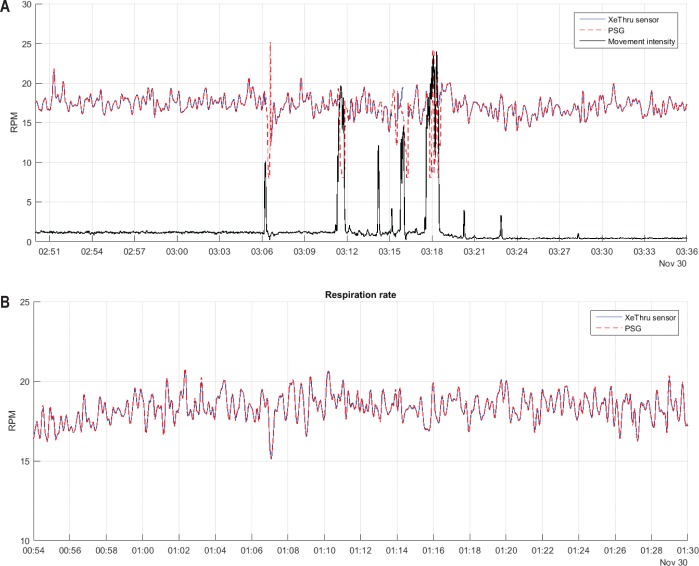
In the signal from a person who is breathing but otherwise inactive, a distinct pattern can be recognized as peaks symmetrical around the origin of the frequency axis of the pulse-Doppler matrix (Figure 1). Respiration per minute (RPM) is estimated as the absolute value of these peaks. During periods of steady respiration this estimate follows PSG signals closely (Figure 2A and Figure 2B, Wisland et al.8). An index of overall body movement is obtained by summarizing the energy of all observed movements over a range covering the whole person. This index thus encompasses movement from all body parts.
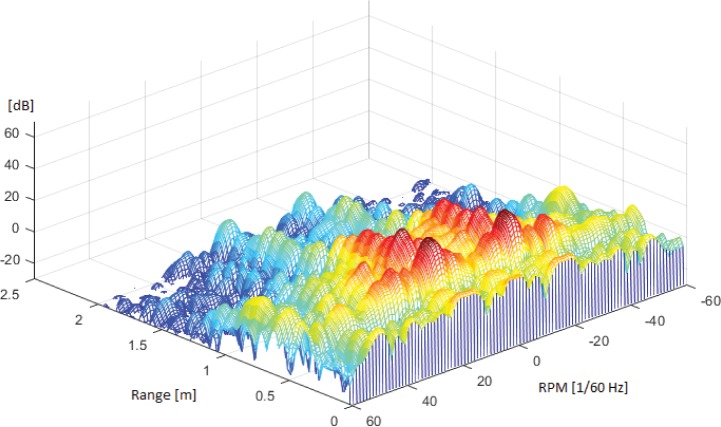
Figure 1. Breathing causes a characteristic pattern in the pulse-Doppler matrix, which is used to estimate the breathing frequency.
Plotted above is the strength, in decibels (dB) of frequency components (respirations per minute, RPM) received at different ranges, summarized over a period of 20 seconds. Symmetric peaks around the origin of the frequency axis indicate periodicity, as the inhalation and exhalation induces movements towards and away from the radar. The range to the first, highest, peaks gives the distance between the radar and the target. Weaker “mirror images” extend behind the first peaks as some portion of reflected waves take detours on their way back to the receiver (bouncing of walls, etc.)
Figure 2. Comparison of respiration measured by radar and PSG.
(A) Comparison showing RPM and movement during light sleep period. (B) Close-up comparison of RPM from radar (XeThru) and PSG during deep sleep period. This figure was originally published in the 2016 whitepaper “XeThru vs. Polysomnography (PSG) Comparative Study,” by Novelda AS and is reproduced here with permission of Novelda AS. PSG = polysomnography, RPM = respiration per minute.
Sleep Algorithm
The sleep algorithm summarizes the movement index and RPM values into 30-second epochs (epoch length chosen to conform with the American Academy of Sleep Medicine standards for PSG scoring). It then employs two static threshold parameters on the overall movement index to decide sleep/wake status for each epoch, using the presence of a respiration signal to determine the difference between a target laying completely still and a target being gone (eg, having left the bedroom).
As opposed to actigraphy, this sleep algorithm integrates movements from all body parts.
Procedure
The radar was placed on the bedside table or on a photo tripod placed along the head of the participant facing diagonally downwards to the feet. Two subjects had two recordings whereas the rest had one recording.
To determine the values of the static threshold parameters, the sleep algorithm was run for a large set of reasonable parameter combinations. Each result was then time-aligned to corresponding PSG sleep/wake state data using an epoch level best fit method designed to choose the best temporal alignment in a range of −40 to +40 epochs. This was done for each protocol exclusively in order to adjust for mismatch between the clock in the radar and the clock in the PSG—ensuring comparison of data collected at the same timepoints. For the final analysis standard 30-second epochs were used. Accuracy, sensitivity, and specificity of sleep/wake from the aligned radar sleep algorithm output in relation to the PSG blueprint was then calculated for each parameter combination and their product mapped in one color coded two-dimensional matrix per data set (14 in total). The best overall parameter tuning was chosen by visual inspection of these 14 maps, and used to determine the final sleep algorithm output for all data sets. The study was approved by the Institutional Review Board of the Faculty of Psychology, University of Bergen, Norway.
Statistics
We calculated the agreement between PSG and radar parameters for sleep onset latency (SOL), wake after sleep onset (WASO) and total sleep time (TST) by estimating the mean difference between them and their corresponding SD, providing a measure of bias.
Further, epoch by epoch (30 seconds) comparisons from bedtime to rise time were conducted. Accuracy, sensitivity and specificity were calculated. In addition, Cohen kappa reflecting epoch by epoch fit was calculated.
RESULTS
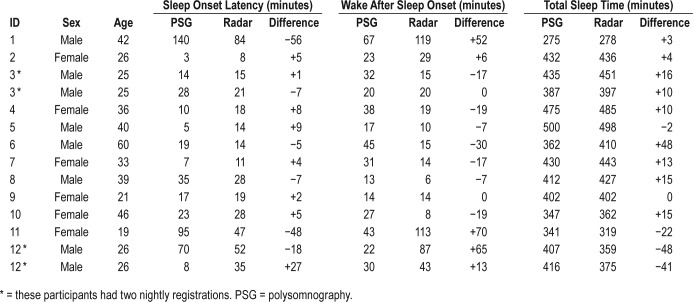
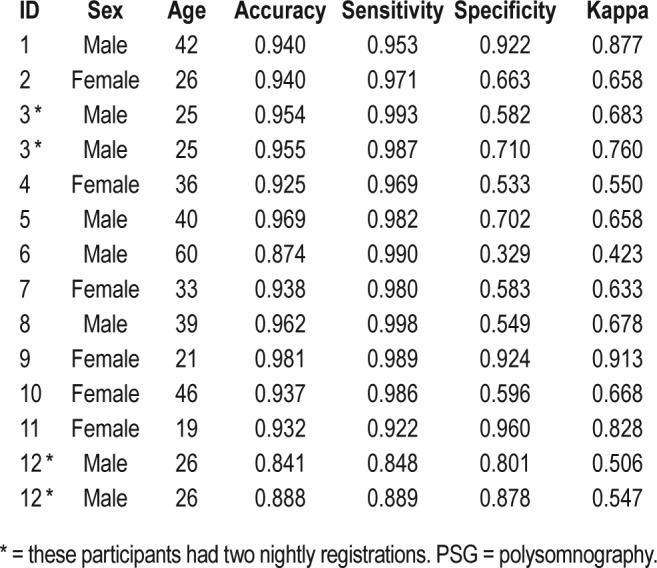
Table 1 shows the demographic and sleep data recorded by PSG and radar for the 14 nights, as well as the difference between them. The mean difference (underestimating) for SOL was −5.7 minutes (SD = 22.1). The mean difference (overestimating) for WASO was +6.4 minutes (SD = 32.5) whereas the mean difference for TST (overestimating) was +1.5 minutes (SD = 24.6). Table 2 depicts the accuracy, sensitivity, specificity and the Cohen kappa for the epoch by epoch comparisons between PSG and radar across the 14 nights. The accuracy ranged from 0.841 to 0.980 with a mean of 0.931 (SD = 0.038). The sensitivity ranged from 0.848 to 0.998 and had a mean of 0.961 (SD = 0.045). In regard of specificity the values ranged from 0.329 to 0.960 with a mean of 0.695 (SD = 0.183). The Cohen kappa values ranged from 0.423 to 0.913. The mean kappa was 0.670 (SD = 0.140).
Table 1.
Demographics and comparison of sleep measures assessed by PSG and radar.
Table 2.
Accuracy, sensitivity, specificity and Cohen kappa for epoch by epoch comparison (radar validated against PSG) for the 14 nights.
DISCUSSION
The present study is the first that have investigated this IRUWB radar technology as a tool for sleep assessment. Overall, the results showed that the discrepancy between PSG and radar estimates was relatively small also when compared to actigraphic concordance with PSG.4 Generally, the radar tended to overestimate WASO and underestimate SOL. The overall discrepancy between the PSG and radar for TST was small overall. Still, it should be noted that for some participants the discrepancy between the radar and the PSG was of a larger magnitude. The mean accuracy was 0.931 which is higher or comparable to that reported for actigraphic recordings.11 Also, the sensitivity obtained with the radar technology was higher than what has been reported in previous actigraphic studies.12 The overall specificity obtained in the present study was close to .70, which is higher than reported for actigraphy.12 Furthermore, the mean kappa value was higher than what has been reported for actigraphy.13
The results suggest that IR-UWB radar may become an alternative objective measure to actigraphy. An obvious advantage over actigraphy is that movements can be assessed from many parts of the body simultaneously, such as movement from the extremities as well as respiration movements, which both change notably during sleep.14,15 The present sleep algorithm uses only a portion of the data from the radar. Explicit use of respirations per minute (RPM) information should be considered for future iterations. The future developmental potential regarding this new technology is large and currently, a radar 10–100 times more sensitive than the one used in the present study has been developed,16 and we are currently conducting new validation studies with this device. The new radar technology may also be able to assess heart rate, which would enable development of even better sleep algorithms. Due to the large amount of data detectable with the radar it is conceivable that algorithms for detection of different sleep stages (eg, non-rapid eye movement and rapid eye movement sleep stages) can be developed. In addition, as the radar has been implemented in a standard complementary metal-oxide-semiconductor (CMOS) technology, it can be produced using standard techniques at a low cost and we expect the production costs of this device not to exceed the costs of actigraphs.
Study Limitations
This pilot study is among the first indexing sleep with IR-UWB radar technology, hence much more empirical evidence is needed before firm conclusions about its validity can be drawn. The sample was rather small and amounted to a few nights in total. Validation studies on the new radar technology in different sleep-disordered populations are warranted. Further development and refinement of the sleep-scoring algorithm is warranted in order to ensure that it provides valid results across different sleep pathologies and age groups. The new technology was validated against PSG since the latter is considered the gold standard of sleep recordings. However, since the radar utilizes movement data, future validation against actigraphy, preferably with concomitant PSG recordings, should also be prioritized. Further, future studies should investigate if the new radar technology is equally performant at all sleeping positions (e,. lateral, supine, prone) and at different distances from the radar. If two people sleep closely together it should be noted that the radar cannot distinguish between the two. However, an artificial wall with a range of 0.4 m to 10 m can be established, disregarding all movement outside the wall. Thus, if two people sleep on different sides of a bed, the technology can as such register data stemming exclusively from the person closest to the radar. In the future it is also possible that the radar technology may identify idiosyncratic movements of an individual and as such distinguish between movements arising from different individuals.
DISCLOSURE STATEMENT
Work for this study was performed at the University of Bergen, Norway. All authors have seen and approved the manuscript. The project was supported by a grant from Novelda. IH and HSAH are both employees of Novelda—the developer of the radar and funder of the study. The other authors report no conflicts of interest.
EDITOR'S NOTE
The Emerging Technologies section focuses on new tools and techniques of potential utility in the diagnosis and management of any and all sleep disorders. The technologies may not yet be marketed, and indeed may only exist in prototype form. Some preliminary evidence of efficacy must be available, which can consist of small pilot studies or even data from animal studies, but definitive evidence of efficacy will not be required, and the submissions will be reviewed according to this standard. The intent is to alert readers of Journal of Clinical Sleep Medicine of promising technology that is in early stages of development. With this information, the reader may wish to (1) contact the author(s) in order to offer assistance in more definitive studies of the technology; (2) use the ideas underlying the technology to develop novel approaches of their own (with due respect for any patent issues); and (3) focus on subsequent publications involving the technology in order to determine when and if it is suitable for application to their own clinical practice. The Journal of Clinical Sleep Medicine and the American Academy of Sleep Medicine expressly do not endorse or represent that any of the technology described in the Emerging Technologies section has proven efficacy or effectiveness in the treatment of human disease, nor that any required regulatory approval has been obtained.
REFERENCES
- 1.Hirshkowitz M. Monitoring and staging human sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 5th ed. St. Louis, MO: Elsevier Saunders; 2011. pp. 1602–1609. [Google Scholar]
- 2.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15(4):259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2(5):389–396. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 4.Marino M, Li Y, Rueschman MN, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36(11):1747–1755. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mostov K, Liptsen E, Boutchko R. Medical applications of shortwave FM radar: remote monitoring of cardiac and respiratory motion. Med Phys. 2010;37(3):1332–1338. doi: 10.1118/1.3267038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events. Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 7.Novelda. X2 Impulse radar transceiver. Trondheim, Norway: Novelda; 2015. [Google Scholar]
- 8.Wisland DT, Granhaug K, Pleym JR, Andersen N, Støa S, Hjortland HA. Remote monitoring of vital signs using a CMOS UWB radar transceiver. New Circuits and Systems Conference (NEWCAS), 14th IEEE International 26-29 June 2016; 2016; Vancouver, BC, Canada. [Google Scholar]
- 9.Stone WC. NIST construction automation program report no. 3. Electromagnetic signal attenuation in construction materials. Gaithersburg, MD: National Institute of Standards and Technology; 1997. [Google Scholar]
- 10.Aardal Ø, Hamran SE, Berger T, Paichard Y, Lande TS. Chest movement estimation from radar modulation caused by heartbeats 2011. IEEE Biomedical Circuits and Systems Conference; 2011; San Diego, CA. [Google Scholar]
- 11.Sivertsen B, Omvik S, Havik OE, et al. A comparison of actigraphy and polysomnography in older adults treated for chronic primary insomnia. Sleep. 2006;29(10):1353–1358. doi: 10.1093/sleep/29.10.1353. [DOI] [PubMed] [Google Scholar]
- 12.Nakazaki K, Kitamura S, Motomura Y, et al. Validity of an algorithm for determining sleep/wake states using a new actigraph. J Physiol Anthropol. 2014;33:31. doi: 10.1186/1880-6805-33-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sargent C, Lastella M, Halson SL, Roach GD. The validity of activity monitors for measuring sleep in elite athletes. J Sci Med Sport. 2016;19(10):848–853. doi: 10.1016/j.jsams.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Kripke DF, Mullaney DJ, Messin S, Wyborney VG. Wrist actigraphic measures of sleep and rhythms. Electroencephalogr Clin Neurophysiol. 1978;44(5):674–676. doi: 10.1016/0013-4694(78)90133-5. [DOI] [PubMed] [Google Scholar]
- 15.Douglas NJ, White DP, Pickett CK, Weil JV, Zwillich CW. Respiration during sleep in normal man. Thorax. 1982;37(11):840–844. doi: 10.1136/thx.37.11.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Novelda. Xethru X4. Trondheim, Norway: Novelda; 2017. [Google Scholar]