Abstract
Objectives:
The purpose of this study is to evaluate and ascertain the current knowledge, perception, level of awareness, and attitudes toward cervical cancer (CC) among women in Malaysia.
Methods:
A cross-sectional study was conducted which involved 210 women aged between 21 and 60 years old at the public in Malaysia, a subsequent statistical analysis was performed by SPSS version 22.
Results:
In comparison with other studies, there is still lacking of awareness on CC and these induced informal cluelessness and poor attitudes toward it. In terms of risk factors, there are two factors with some degree of awareness among women in Malaysia, i.e., multiple sexual partners and sexually transmitted diseases. Women in Malaysia have less awareness on the causes and clinical manifestations of the disease (P < 0.05). They are aware that regular papanicolaou (Pap) smear would screen CC and surgery could be a treatment of choice. In addition, women in Malaysia also have moderate awareness about Pap smear as prevention to detect and prevent CC at the early stage.
Conclusions:
Women in Malaysia only has a good awareness about multiple sex partner and sexually transmitted disease as a risk factor for CC, they also have good knowledge on regular Pap smear as a tool to diagnose and surgery as a treatment. Future, further effort is required to promote awareness of women’s perception and attitudes toward CC.
Keywords: Cervical cancer, knowledge and attitudes, papanicolaou smears
Introduction
Cervical cancer (CC) is one of the most common international malignancy in women and a serious public health problem. The main burden of CC actually is in the developing country, as it takes away young mothers causing considerable emotional and economic upset in the family. This disease is also called as “hidden or silent” cancer because the usually patient is asymptomatic and its diagnosis is incidental after a loop biopsy of the cervix for pre-invasive ailment. In the world, its annual incidence is approximately around 500,000 women, and nearly 274,000 of them expire from the disease.[1] It is the second most common global malignancy in women and the most common in women in under-developed countries and emergent nations which account more than 80% of the global burden of the disease.[2] More than 50% of international cases appear within the Asia-Pacific region, and India has the top predicted figure of CC cases and decreases within Asia.[3] In Malaysia, CC is the second most common malignancy in women which consists 12.9% of total female cancers.[4] There is lack of effective control measures in both under-developed and developing countries. In the developed country, CC is uncommon cancer due to early detection programs such as screening, education, good access to better medical care, and early treatment for precancerous lesions, which are the key for reducing CC morbidity and mortality.[5]
The primary underlying cause of CC is human papillomavirus (HPV), which is one of the sexually transmitted diseases (STD).[6] HPV infection leads to precancerous change in the cervical epithelium known as cervical intraepithelial neoplasia (CIN) which has the potential to turn into malignant stage if left untreated.[7] In the United States, maximum 80% of sexually active females is revealed to the virus by 50 years old.[8] There are more than 200 types of HPV, more than 40 types are easily spread via direct sexual contact. In Malaysia, HPV-16 and HPV-18 are the most common and constitute 88% of CC.[9] Population-based screening program utilizes exfoliative cervical cytology,[10] the papanicolaou (Pap) smear decreases the CC morbidity and mortality in developed countries.[11,12] Development of HPV vaccines is to prevent the primary infection with certain oncogenic HPV which is HPV 16, 18, 31, and 33. Many countries including Malaysia have introduced a national program of HPV vaccination with the aim of reducing morbidity and mortality of CC. HPV vaccine is effective, safe, and potentially protecting future female generations.[13,14]
In Malaysia, public health programs control and prevent CC including free screening of CIN using Pap smear, educational program through campaign and advertisement, and free HPV vaccination to 14-year-old school girl. The success and benefit of these programs rely greatly on the level of consciousness of the targeted group on different basic aspects of this disease. Various researchers were performed to evaluate women’s awareness and knowledge level.[13,15-17] However, currently, there is still insufficient information and research to explore the level of knowledge of CC among Malaysian women.
Hence, the purpose of this study is to evaluate current awareness, knowledge, and attitudes of women toward CC in Malaysia. The outcome of this study may provide inputs toward designing a suitable strategy to inform and educate the Malaysian women on prevention of CC, augment the public health program to control and prevent CC.
Methods
A cross-sectional study was conducted on women in Malaysia. The participants were identified by a random sampling at the age from 21 to 60. 210 participants were randomly selected. They were informed on the nature of this study with full confidentiality and informed consents were taken. The questionnaire was modified from Vaidya et al.[18] and was created based on the risk factor, causes, warning signs, diagnosis, treatment and prevention of CC to evaluate the current awareness and knowledge level of women about CC in Malaysia. The questionnaires were distributed at the public area in Malaysia; this questionnaire consisted of 34 questions with additional other questions such as age, education level, marital status, and employment for demographic recording purpose. Each item was graded in the Likert’s scale from 1 to 5 whereby 1 is strongly disagree, and 5 is strongly agree; the respondents were instructed to score each question based on their knowledge from 1 to 5. Data were analyzed by the Statistical Package for the Social Sciences Version 22 (SPSS v22) including t-test.
Results
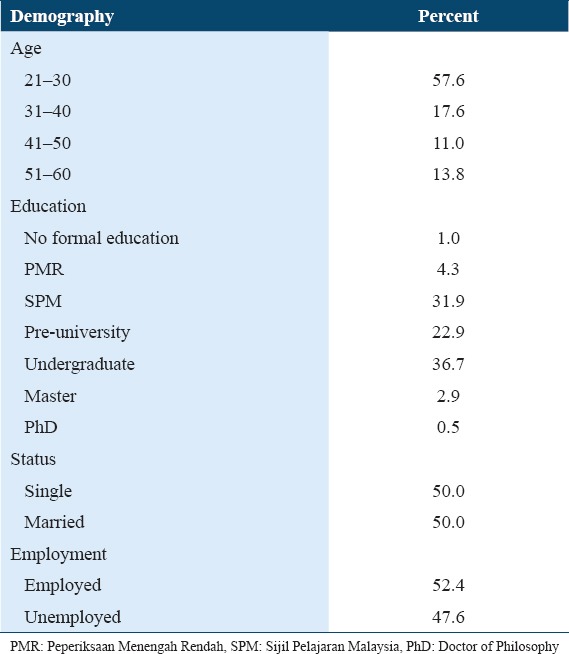
Based on Table 1, 57.6% respondents were consisting of women in the aged range from 21 to 30 years old, 17.6% were aged from 31 to 40 years old, 11% were from 41 to 50 years old, and only 13.8% were 50 years old and above. In term of education, 36.7% were undergraduates, 31.9% achieved Sijil Pelajaran Malaysia level, 22.9% accomplished pre-university study, 4.3% reached the level of Penilaian Menengah Rendah, those with masters degree account for 2.9%, and 1% has no formal education and those with Doctor of Philosophy was 0.5%. Half of the respondents were married, and 52.4% were employed.
Table 1.
The demographic profile of the respondents
This section of our research was to test the knowledge of the risk factor of CC among women. A mean score of 4 and above indicated a good awareness of that particular component. In Table 2, people were less aware of multiparity as one of the risk factors for CC with a mean score of 2.8, it did not achieve 4 (P < 0.05), it was statistically significant. As regarding to multiple sexual partners, it showed that there was awareness with a mean score of 4.2 (P < 0.05), this component was also statistically significant. As regarding to other factors, it implied less awarenesson smoking (a mean score of 3.7), immune-suppression (a mean score of 3.3), obesity (a mean score of 2.9), high calories intake (a mean score of 3.1), early sexual intercourse (a mean score of 3.1), oral contraceptive pill (a mean score of 3.1), intrauterine devices (IUDs) (a mean score of 2.9), and genetic factor (a mean score of 3.7), they were all statistically significant (P < 0.05). Thus, these means failed to achieve 4; these indicated less awareness of those particular elements. However, STD had a mean score of 3.8 (P > 0.05), it rejected the null hypothesis, and this indicated that the public might have some degree of good awareness on this factor. In short, the risk factors such as high calories intake, early sexual intercourse, oral contraceptive pills, intrauterine devices, and family history have proven a less awareness on this section with statistically significant (P < 0.05) except risk factor like STD.
Table 2.
Risk factors, causes and clinical manifestation of CC
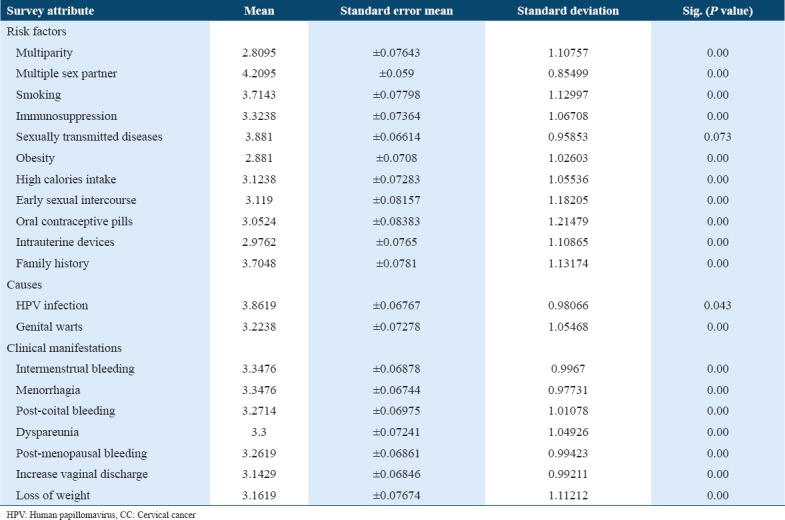
CC has two main causes, i.e., HPV infection and genital warts. In Table 2, the mean scores for HPV infection and genital warts were below 4 (P < 0.05), this indicated that public had less awareness on these two issues with theirs.
Current awareness and the knowledge level of clinical manifestation of CC such as intermenstrual bleeding, menorrhagia, post-coital bleeding, dyspareunia, post-menopausal bleeding, increase vaginal discharge, and loss of weight were evaluated. In Table 2, the mean scores of all of the clinical manifestation of CC failed to reach 4 (P < 0.05), thus implied that public had less awareness on this aspect of CC. The results were statistically significant.
In Table 3, the mean score for Pap smear did not achieve 4 (P > 0.05), it indicated a weak public awareness on this area, it rejected the null hypothesis, and probably the public had some degree of good awareness. Similarly to tissue biopsy, despite its mean score showed a good awareness (P > 0.05), it also rejected the null hypothesis, and the public might have a misunderstanding and misinterpretation on this aspect.
Table 3.
Diagnosis, treatment, and prevention of CC
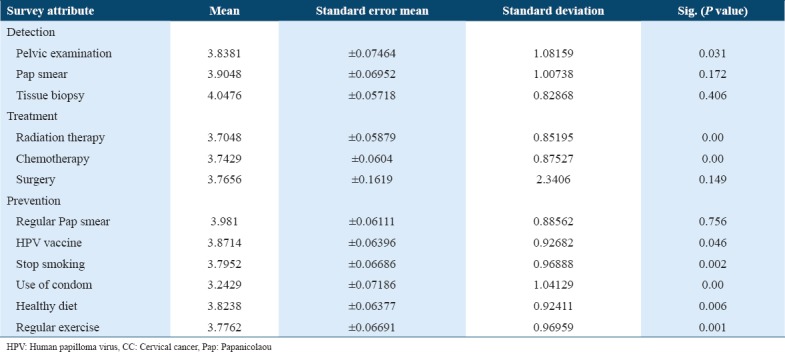
Prevention, early diagnosis and treatment are proven to decrease death from CC. Many nations significantly decrease their CC morbidity and mortality by deploying CC screening program and early intervention. CC can be divided into four stages. Each stage is treated according to its severity. The treatments are chemotherapy, radiation therapy, chemoradiation therapy, and surgery. In Table 3, the mean scores of radiation therapy, chemotherapy, and chemoradiation therapy failed to achieve 4 (P < 0.05), these indicated that public had less awareness on them, this result was statistically significant. For surgery, despite its mean score showed a good awareness (P > 0.05), it rejected the null hypothesis, and the public might have misinterpretation and misunderstanding on this aspect.
In Table 3, despite the mean score of regular Pap smear has reached 4 (P > 0.05), it implied a good awareness but it rejected the null hypothesis, and the public might have misinterpretation and misunderstanding on this aspect. The mean scores of all the other prevention methods such as HPV vaccination, cessation of smoking, use of condom, healthy diet, and regular exercise were under 4; these indicated that the women in Malaysia have very minimal awareness on the CC preventive methods (P < 0.05). On obtaining all the results, our next discussion section will create a good insight on our study.
Discussion
Most women with CC are diagnosed before the age of 50. According to the Centers for Disease Control and Prevention (CDC), CC is usually diagnosed at younger ages than other HPV associated cancers (CDC, 2012).[19] The median age is 49 years old. However, undeniable that older women are remain as the one who is at the highest risk, but in this study, most of the respondents are women below the age of 30. In terms of education, marital status and employment, it shows that educated, married, and employed women have less awareness on CC. The possible explanation could be either lack of enforcement toward the knowledge and attitude of this disease or ignorant.
In this study, several risk factors were indicated to increase the risk of having CC. The factors such as multiparity, multiple sexual partners, smoking, immune-suppression, STD, obesity, high calories intake, early sexual intercourse, inheritance disease, using of oral contraceptive pills, and IUDs could lead to CC. There is a widely accepted hypothesis that multiparity is one of those risk.[20,21] For instance, Italian women with age <45 and three or more deliveries possess an escalated the risk of 8.1 compared with nulliparous women,[22] but the spreading of this information is yet to be asserted into public awareness. It implies that our women in Malaysia have weak awareness on multiparity as one of the causes for CC. In this study, women in Malaysia are aware that multiple sex partners can cause CC. According to some of them, media is the one to play a big role in this. The number of sexual partners is associated with the development of CC.[23]
Smoking is another cause of CC; smokers have an excess risk of CC. In our study, Malaysian women are still lack of awareness on this aspect. Smokers perceive a relative greater risk of heart disease than that of non-smokers, they do not expect to be similar in the case of CC.[24]
STD is actually proven to be one of the causes.[25] In this study, it implies that women in Malaysia may have some degree of awareness on this aspect. More than 90% school-attending adolescents with age between 13 and 20 years old usually have better awareness on HIV and AIDS but low awareness for HPV. People are alert on STD as a factor for CC, but not all STD are known by them.[26]
World Health Organization recommends frequent physical exercise and upkeep of a healthy body weight, along with a healthy diet, because it will definitely decrease cancer risk. For instance, the mean body mass index is higher in patients with CC than in control patients with CIN (P < 0.01),[27] but in our study people are not aware of this. Most of them believe that obesity or overweight does not have any correlation with CC.
Based on the result of this study, it showed that women in Malaysia have less awareness of the risk factor of CC. Similarly, despite the high prevalence of CC, studies implied that women’s knowledge on HPV, CC, and cervical screening is still inadequate. Insufficient of awareness on risk factors and symptoms for malignancy may result in a late diagnosis and bad prognosis. Similarly, the explanations for the high incidence and mortality from CC in sub-Saharan Africa involve insufficient of awareness of CC among the population, health-care providers and policymakers, limited access to high-quality health-care services and cervical screening programs and a shortage of functional referral systems. All these proceed to advanced stage at diagnoses.[28]
Early sexual activity is known to cause CC. Associated factors with CC include a history of multiple sexual partners and copulation at the age of 17 or earlier. Women without any sexual activity are at lower risk for developing CC.[29] Early sexual initiation is recognized to be a risk factor by up to44.3% of women.[30] Unfortunately, in our study, women’s awareness on this aspect is yet to be strengthened.
Oral contraceptive pills are the contributing factor for CC, women taking oral contraceptives with at least 5 years are subjected to a two-fold risk of developing CC,[31] some women are still unaware about this. In Togo, only 23.7% of women are aware on this.[30] Lack of awareness on oral contraceptive pills is one of the risk factors of CC. Surprisingly, IUD help in preventing CC. It does not reduce HPV infection but decrease the probability of HPV induced CC; its users are proven to have a lesser risk of developing CC.[32]
Family history plays a key role in contributing to CC. Women have a first degree relative with CC are at greater risk for acquiring it. In our study, our society is still unaware about this. In Pakistan, only 8% of the population is aware about the risk factor of family history would lead to CC. Therefore, ameliorating public awareness of the program to enhance their knowledge by alerting women on risk factors of CC is vital. The role of media campaign should be contemplated as these are known to work best in advertising CC screening, multiple media is desirable. Ameliorating the acceptability of screening to women by giving accessible and precise information with reduced waiting times during screenings, results and treatment are greatly preferable.[32]
In our study on the causes of CC, awareness on this expect was low (P < 0.05), thus this indicated that Malaysian women had low awareness on HPV and genital warts. This awareness level is still not up to expectation after years of health campaign CC in Malaysia; this shows there is still space for improvement on the awareness campaign and advertisement. Women are motivated to be responsible for their own health and be active in the screening program instead of depending on the health-care professional’s proposal for Pap smear screening. Respondents are ignorant on HPV infection and its link to CC. In the United States, 40% of women aged 18–75 are alert on HPV, but only 20% are aware of its link to CC.[33] There is necessary to teach Malaysian women on the role of HPV in the etiology of CC and its prevention. The implication of health-care professional and the mass media should apprise the population to decrease the burden of CC in Malaysia and its mortality. In addition, the use of local celebrities as role models to campaign the uptake of Pap smear screening is effective; it improves public attention and influences behavioral change in screening practices among women.
As regarding to all of the clinical manifestations of CC, all their mean scores indicated that women in Malaysia have less awareness with statistically significant. Despite awareness campaign and advertisement conducted by MOH, women are lack of good knowledge on the clinical manifestations of CC. Low level of knowledge on clinical manifestations of CC can be one of the reasons reducing participation in CC prevention programs and the screening test. The explanations for skipping the screening test in spite of a desire to pursue are mainly lack of awareness on disease or symptoms, knowledge on initialing the test, peer involvement and reinforcement of thought.[34] Occasionally women fail to acknowledge the significance of preventive health check-up in the absence of symptoms.[35]
In our study, women in Malaysia have inadequate awareness on pelvic examination to diagnose CC. Most of the women identify pelvic examinations as a major origin of apprehensiveness, loss of privacy and mortification.[36] Due to religious and cultural beliefs, Muslim women are at ease with a female health-care professional; they are not keen to involve in screening due to perceived inaccessibility of female health-care professional. In fact, they prefer female health-care professional to conduct physical examination on intimate body parts and are significantly chagrined with male health-care professional, female health-care professional have a higher chance of accomplishing a Pap smear.[37,38]
A predicted pain and discomfort during the procedure is another obstacle to screening among these women. Denunciation of pelvic examinations among women leads to exposure to sensationalized tales by peers. Perceived pain as described by peers is an obstacle to pursuing pelvic examination. Exchange of personal health information among public influences the efficient of referral system in health care.[39] Accurate health-care information and communication by health-care professional is important to eliminate the gap between women’s subculture and that of health professionals; it eradicates the feelings of stigma and pain perception toward pelvic examination. One-third of our respondents value their own health as secondary to family and social responsibilities; many women treat their daily domestic housework and family needs as priority than prevention of disease.[37,40]
In our study, public has some degree of good awareness on Pap smear to diagnose CC, the procedure is easy and cheap with good sensitivity and specificity.[41] Knowledge of both cancer of the cervix and Pap smear can be enhanced significantly if more women are aware of the disease, the intervention and Pap smear.[41,42]
As regarding to tissue biopsy, our public may actually have a misinterpretation on this aspect. They may understand the nature of this procedure, but this does not imply that tissue biopsy is fully understood by them in relation to CC. The actual concept of tissue biopsy is unclear among women in Malaysia which makes a large gap in attitude and knowledge about it. In fact, <5% of women in developing nations are screened for CC per year as compare with almost half of women in developed countries, the considerable differences in CC incidence rates are due to a very low screening coverage in developing nations.[43]
Our public has less awareness on the treatment options in CC except for surgery; they may actually have some degree of good knowledge on this aspect. The three most common identified treatment options for CC are hysterectomy, chemotherapy, and radiotherapy.[44] Our awareness level is still far from ideal expectation after health campaign in CC for a few years in Malaysia. Many women believe to be helpless if CC is diagnosed, they prefer to ignore rather than accept, but generally they have a fairly good knowledge on the treatment of CC.
Poverty of awareness and access to preventive methods link closely to the relatively high levels of CC. Malaysians are less aware of the importance of having regular Pap smear done due to various reasons, Pap smear is yet to reach a broad coverage because it is only done opportunistically and insufficient awareness among women. It is simple, cheap, safe, and readily acceptable by Malaysian women, Pap smear is still unpopular. Human factors including the negative attitude of women and health-care professional and unsatisfactory service are part of the reasons of insufficient coverage, Malaysian women still had inadequate knowledge and awareness of CC and screening.[37]
Non-compliance is another reason for poor prevention. Malaysian women are non-compliance to subsequent visits or follow on Pap smear. Women with less awareness believe Pap smear screening is not important and they take it for granted. They only do it when they are told by the doctors and been called directly to be reminded of the screening. Hence, this might be proof that there is awareness but yet been neglected.[36] Cultural beliefs and religion mask health beliefs among these women, they induce confusion, hesitance, and obstacle to screening.[45]
In our study, the public is unaware of the importance of healthy lifestyle as a part of CC prevention, they prefer activities with immediate effects, and they believe that healthy lifestyle cannot prevent CC. There are multiple ways in preventing CC; prevention of CC requires the HPV infection of the genital tract de novo or precluding constant infection of the cervix with HPV. The genital HPV is transmitted by sexual contact; possible methods of primary prevention should be included abstinence, mutual monogamy, condom, and a good practice for safe sex.[46]
The acceptance of HPV vaccine is relatively high along with two factors such as the knowledge of cervical screening and risk factors of CC. There are many reasons for vaccine refusal, unresolved doubts on the vaccine’s safety and efficacy, the perceived embarrassment of receiving a STD vaccine; adverse drug reaction or the side effects of the vaccine are possible explanations. Living in a country with Muslims as the highest number of the population residing in Malaysia, the “halal” status of the vaccine is definitely an issue among those uncertain. Some of the Muslim physicians consider cultural sensitivity is an issue to recommend HPV vaccines because it may imply prevention against STD rather than CC, this creates a stigma among the society.[46]
Conclusion
In a nutshell, CC is preventable. In this study, it clearly shows that women in Malaysia only have a good awareness that having multiple sexual partners and STD are among the risk factors for CC. Meanwhile, they are also aware that regular Pap smear and surgery can diagnose and treat CC. Besides that, the other findings suggest that there is still lacking of knowledge and information about CC among women in Malaysia. It can be due to insufficient communication by a health-care professional that leads to women’s poor attendance and insufficient awareness regarding CC. Even with adequate knowledge, this was not put into practice. Therefore, in conclusion, it shows that there is a large gap in knowledge, attitude, and practices among Malaysian women on CC. Hence, health education, barrier-specific counseling and outreach and community-based interventions should be ideal to provide an opportunity and to enhance the awareness of having cervical screening done. Methods should be implemented in such a way that knowledge and awareness are put into action and practice. Educating women is equal to educating a generation and the nation in a whole.
References
- 1.Cervical Cancer, Human Papillomavirus (HPV), and HPV Vaccines. WHO. World Health Organization. [[Last cited on 2017 Oct 04]]. Available from: http://www.who.int/reproductivehealth/publications/cancers/RHR_08_14/en .
- 2.Garland S, Park SN, Ngan HY, Frazer I, Tay EH, Chen CJ, et al. The need for public education on HPV and cervical cancer prevention in Asia. Opinions of experts at the AOGIN conference. Vaccine. 2008;26:5435–40. doi: 10.1016/j.vaccine.2008.07.077. [DOI] [PubMed] [Google Scholar]
- 3.Chye GL, Yahaya H. Second Report of the National Cancer Registry:Cancer Incidence in Malaysia;2003. National Cancer Registry. 2004 [Google Scholar]
- 4.Monga A, Dobbs SP. Gynecology by Ten Teachers. London: CRC Press; 2011. [Google Scholar]
- 5.Myers ER, McCrory DC, Nanda K, Bastian L, Matchar DB. Mathematical model for the natural history of human papillomavirus infection and cervical carcinogenesis. Am J Epidemiol. 2000;151:1158–71. doi: 10.1093/oxfordjournals.aje.a010166. [DOI] [PubMed] [Google Scholar]
- 6.Salati SA, Al Kadi A. Anal cancer - a review. Int J Health Sci (Qassim) 2012;6:206–30. doi: 10.12816/0006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortega-Cervantes L, Aguilar-Lemarroy A, Rojas-García AE, Barrón-Vivanco BS, Vallejo-Ruiz V, León DC, et al. Human papilloma virus genotypes in women from Nayarit, Mexico, with squamous intraepithelial lesions and cervical cancer. Int J Health Sci (Qassim) 2016;10:327–38. [PMC free article] [PubMed] [Google Scholar]
- 8.Cheah PL. Human papillomavirus related diseases in Malaysians. Malays J Pathol. 1994;16:15–7. [PubMed] [Google Scholar]
- 9.Sichanh C, Quet F, Chanthavilay P, Diendere J, Latthaphasavang V, Longuet C, et al. Knowledge, awareness and attitudes about cervical cancer among women attending or not an HIV treatment center in lao PDR. BMC Cancer. 2014;14:161. doi: 10.1186/1471-2407-14-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma D, Sandhu SV, Bansal H, Gupta S. Distinct perturbations of oral squamous cell carcinoma patients:A quantitative cytomorphometric analysis. Int J Health Sci (Qassim) 2015;9:283–91. [PMC free article] [PubMed] [Google Scholar]
- 11.Peto J, Gilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet. 2004;364:249–56. doi: 10.1016/S0140-6736(04)16674-9. [DOI] [PubMed] [Google Scholar]
- 12.Saha A, Chaudhury AN, Bhowmik P, Chatterjee R. Awareness of cervical cancer among female students of premier colleges in Kolkata, India. Asian Pac J Cancer Prev. 2010;11:1085–90. [PubMed] [Google Scholar]
- 13.Price JH, Easton AN, Telljohann SK, Wallace PB. Perceptions of cervical cancer and pap smear screening behavior by women's sexual orientation. J Community Health. 1996;21:89–105. doi: 10.1007/BF01682301. [DOI] [PubMed] [Google Scholar]
- 14.Gebremariam T. Human papillomavirus related cervical cancer and anticipated vaccination challenges in Ethiopia. Int J Health Sci (Qassim) 2016;10:137–43. [PMC free article] [PubMed] [Google Scholar]
- 15.Ralston JD, Taylor VM, Yasui Y, Kuniyuki A, Jackson JC, Tu SP, et al. Knowledge of cervical cancer risk factors among Chinese immigrants in Seattle. J Community Health. 2003;28:41–57. doi: 10.1023/a:1021381105325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaidya A, Aryal UR, Krettek A. Cardiovascular health knowledge, attitude and practice/behavior in an urbanizing community of Nepal:A population-based cross-Sectional study from Jhaukhel-Duwakot health demographic surveillance site. [[Last cited on 2017 Oct 04]];BMJ Open. 2013 3:e002976. doi: 10.1136/bmjopen-2013-002976. Available from: http://www.bmjopen.bmj.com/content/bmjopen/3/10/.e002976.full.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dandash KF, Al-Mohaimeed A. Knowledge, attitudes, and practices surrounding breast cancer and screening in female teachers of Buraidah, Saudi Arabia. Int J Health Sci (Qassim) 2007;1:61–71. [PMC free article] [PubMed] [Google Scholar]
- 18.HPV and Cancer. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 2017. [[Last cited on 2017 Oct 04]]. Available from: http://www.cdc.gov/cancer/hpv/statistics/age.htm .
- 19.Gawande V, Wahab SN, Zodpey SP, Vasudeo ND. Parity as a risk factor for cancer cervix. Indian J Med Sci. 1998;52:147–50. [PubMed] [Google Scholar]
- 20.Harris GR. Long-term Effects of Multiparity on Cervical and Ovarian Cancer. 2017. [[Last cited on 2017 Oct 04]]. Available from: http://www.digitalcommons.pcom.edu/biomed/41 .
- 21.Hinkula M, Kauppila A, Näyhä S, Pukkala E. Cause-specific mortality of grand multiparous women in Finland. Am J Epidemiol. 2006;163:367–73. doi: 10.1093/aje/kwj048. [DOI] [PubMed] [Google Scholar]
- 22.Liu ZC, Liu WD, Liu YH, Ye XH, Chen SD. Multiple sexual partners as a potential independent risk factor for cervical cancer:A Meta-analysis of epidemiological studies. Asian Pac J Cancer Prev. 2015;16:3893–900. doi: 10.7314/apjcp.2015.16.9.3893. [DOI] [PubMed] [Google Scholar]
- 23.Marteau TM, Hankins M, Collins B. Perceptions of risk of cervical cancer and attitudes towards cervical screening:A comparison of smokers and non-smokers. Fam Pract. 2002;19:18–22. doi: 10.1093/fampra/19.1.18. [DOI] [PubMed] [Google Scholar]
- 24.Sexually Transmitted Infections (STIs) World Health Organization. World Health Organization. [[Last cited on 2017 Oct 04]]. Available from: http://www.who.int/mediacentre/factsheets/fs110/en .
- 25.Samkange-Zeeb FN, Spallek L, Zeeb H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe:A systematic review of published literature. [[Last cited on 2017 Oct 04]];BMC Public Health. 2011 11:727. doi: 10.1186/1471-2458-11-727. Available from: https://www.elib.suub.uni-bremen.de/edocs/00103368-1.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JK, So KA, Piyathilake CJ, Kim MK. Mild obesity, physical activity, calorie intake, and the risks of cervical intraepithelial Neoplasia and cervical cancer. [[Last cited on 2017 Oct 04]];PloS One. 2013 8:e66555. doi: 10.1371/journal.pone.0066555. Available from: http://www.journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0066555&type=printable . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mwaka AD, Orach CG, Were EM, Lyratzopoulos G, Wabinga H, Roland M. Awareness of cervical cancer risk factors and symptoms:Cross-sectional community survey in post-conflict northern Uganda. Health Expectations. 2016;19:854–67. doi: 10.1111/hex.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zandberg DP, Bhargava R, Badin S, Cullen KJ. The role of human papillomavirus in nongenital cancers. CA Cancer J Clin. 2013;63:57–81. doi: 10.3322/caac.21167. [DOI] [PubMed] [Google Scholar]
- 29.Moore AR, Driver N. Knowledge of cervical cancer risk factors among educated women in Lomé, Togo:Half-truths and misconceptions. [[Last cited on 2017 Oct 04]];Sage Open. 2014 4:1–8. Available from: http://www.journals.sagepub.com/doi/pdf/10.1177/2158244014557041 . [Google Scholar]
- 30.Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers:A systematic review. Cancer Epidemiol Biomarkers Prev. 2013;22:1931–43. doi: 10.1158/1055-9965.EPI-13-0298. [DOI] [PubMed] [Google Scholar]
- 31.Raza SA, Franceschi S, Pallardy S, Malik FR, Avan BI, Zafar A, et al. Human papillomavirus infection in women with and without cervical cancer in Karachi, Pakistan. Br J Cancer. 2010;102:1657–60. doi: 10.1038/sj.bjc.6605664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. Know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007;16:288–94. doi: 10.1158/1055-9965.EPI-06-0756. [DOI] [PubMed] [Google Scholar]
- 33.Aswathy S, Quereshi MA, Kurian B, Leelamoni K. Cervical cancer screening:Current knowledge and practice among women in a rural population of Kerala, India. Indian J Med Res. 2012;136:205–10. [PMC free article] [PubMed] [Google Scholar]
- 34.Roy B, Tang TS. Cervical cancer screening in Kolkata, India:Beliefs and predictors of cervical cancer screening among women attending a women's health clinic in Kolkata, India. J Cancer Educ. 2008;23:253–9. doi: 10.1080/08858190802189105. [DOI] [PubMed] [Google Scholar]
- 35.Wong LP, Wong YL, Low WY, Khoo EM, Shuib R. Cervical cancer screening attitudes and beliefs of Malaysian women who have never had a pap smear:A qualitative study. Int J Behav Med. 2008;15:289–92. doi: 10.1080/10705500802365490. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen TT, McPhee SJ, Nguyen T, Lam T, Mock J. Predictors of cervical pap smear screening awareness, intention, and receipt among vietnamese-american women. Am J Prev Med. 2002;23:207–14. doi: 10.1016/s0749-3797(02)00499-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holroyd E, Twinn S, Adab P. Socio-cultural influences on Chinese women's attendance for cervical screening. J Adv Nurs. 2004;46:42–52. doi: 10.1111/j.1365-2648.2003.02964.x. [DOI] [PubMed] [Google Scholar]
- 38.Suls JM, Goodkin F. Good Gossip. Lawrence: University press of Kansas; 1994. Medical Gossip and Rumor:Their Role in the Lay Referral System; pp. 85–99. [Google Scholar]
- 39.Dabash R, Vajpayee J, Jacob M, Dzuba I, Lal N, Bradley J, et al. Strategic Assessment of Cervical Cancer Prevention and Treatment Services in 3 Districts of Uttar Pradesh, India:Reproductive Health. 2005. [[Last cited on 2017 Oct 04]]. Available from: https://www.reproductive-health-journal.biomedcentral.com/track/pdf/10.1186/1742-4755-2-11?site=reproductive-health-journal.biomedcentral.com . [DOI] [PMC free article] [PubMed]
- 40.Zaridah S. A review of cervical cancer research in Malaysia. Med J Malaysia. 2014;69(Suppl A33-41) [PubMed] [Google Scholar]
- 41.Parhizkar S, Latiff LA, Afshari M. Disseminating cervical cancer knowledge:Impact of a public seminar. Int J Learn Dev. 2013;3:203–11. [Google Scholar]
- 42.Chirenje ZM, Rusakaniko S, Kirumbi L, Ngwalle EW, Makuta-Tlebere P, Kaggwa S, et al. Situation analysis for cervical cancer diagnosis and treatment in east, central and southern African countries. Bull World Health Organ. 2001;79:127–32. [PMC free article] [PubMed] [Google Scholar]
- 43.Wong LP. Physicians'experiences with HPV vaccine delivery:Evidence from developing country with multiethnic populations. Vaccine. 2009;27:1622–7. doi: 10.1016/j.vaccine.2008.11.107. [DOI] [PubMed] [Google Scholar]
- 44.Islam N, Kwon SC, Senie R, Kathuria N. Breast and cervical cancer screening among south Asian women in new york city. J Immigr Minor Health. 2006;8:211–21. doi: 10.1007/s10903-006-9325-y. [DOI] [PubMed] [Google Scholar]
- 45.Manhart LE, Koutsky LA. Do condoms prevent genital HPV infection, external genital warts, or cervical neoplasia?A meta-analysis. Sex Transm Dis. 2002;29:725–35. doi: 10.1097/00007435-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 46.Wong LP. Knowledge and attitudes about HPV infection, HPV vaccination, and cervical cancer among rural Southeast Asian women. Int J Behav Med. 2011;18:105–11. doi: 10.1007/s12529-010-9104-y. [DOI] [PubMed] [Google Scholar]


