Abstract
Objectives:
This study aimed to explore deep breathing exercise education receiving and performing status of patients undergoing abdominal surgery and the relation between them.
Methodology:
This descriptive and cross-sectional study was conducted at the surgical ward of a university hospital with 130 patients between August 17 and October 15, 2015. A patient information form and a deep breathing exercise questionnaire were used for data collection. The patients were visited in their rooms after their surgeries and were asked to answer these questions through face-to-face interviews. Descriptive statistics, the Mann–Whitney U test, Spearman’s correlation, and Pearson’s Chi-squared test were used for analyzing the data.
Results:
Of the patients, 56.2% of the patients received education about deep breathing exercises, and 51.5% of them performed it. A total of 60.3% of the patients received their education from nursing students. Furthermore, 54.8% of them received this education after surgery. A strong correlation was found between the status of receiving education and performing statuses of patients (P < 0.001).
Conclusion:
The study results indicated that the surgical patients did not receive adequate education about deep breathing exercises and most of them received this education after their surgeries. As a good finding, receiving education affected patients’ exercise performing statuses positively. It is advised from this study that clinical nurses should receive in-service education on the importance of pre-operative deep breathing exercise education to improve the exercise application rate among surgical patients.
Keywords: Breathing exercises, general surgery, nursing care, patient education
Introduction
Pre-operative education provides health-related information for patients, prepares them for surgery and helps to minimize the development of post-operative complications.[1-3] According to a review, post-operative pulmonary complications are more common than other complications.[4] The incidence of post-operative pulmonary complications following major surgery is reported to be between 2 and 40%, associated with increased hospital stay, morbidity, and mortality.[5-7]
Deep breathing exercises are used to decrease the incidence and severity of pulmonary complications, such as pneumonia, atelectasis, and hypoxemia.[8] During exercise education, the nurse explains and demonstrates how to take a deep, slow breath, and how to exhale slowly, 3 to 5 times every 1 or 2 h. In a study by Westerdahl et al.,[9] the patients who performed deep breathing exercises had better pulmonary function compared to the performing no exercise groups. In their study, Mathew and D’silva[10] detected that in patients with chronic airflow limitation, the practice of deep breathing exercises reduced the respiratory rate and increased alveolar ventilation.
One goal of pre-operative nursing care is to educate the patient about exercises. According to a study conducted in Turkey,[11] it was detected that the 25% of nurses educated the patient preoperatively about exercises. In another study, Gürlek and Yavuz[1] found 77.8% of the nurses did not provide any deep breathing, leg, and turning exercise education to patients during the pre-operative period, and a deficiency was also found in applying the education. In a review, it was mentioned that research in the field of pre-operative education is weak.[12]
Patients may have deficits in understanding the importance of deep breathing through the absence of education and limited knowledge may affect patients’ ability to exercise participation.[13,14] According to a study, by providing adequate education, nurses can enhance patient participation in exercise interventions.[15] At the surgical ward of this study, there is not any exercise education protocol to follow after surgeries about deep breathing exercises and nurses educate patients according to their own surgical nursing skills.
This study aimed to explore deep breathing exercise education receiving and performing status of patients undergoing abdominal surgery.
The specific study questions were as follows:
Do surgical patients receive any education about deep breathing exercises?
Do patients perform deep breathing exercises?
How does receiving education about deep breathing exercises effect patients’ status of performing these exercises?
Methods
Study design and sample
This descriptive and cross-sectional study was conducted at the surgical ward of a university hospital in Turkey including 130 patients from August 17 to October 15, 2015. The patients included in this study had undergone upper abdominal surgery, were between 18 and 65 years of age, were able to communicate, and volunteer to participate. The sampling calculation was carried out using the main outcome variable of a study[16] based on giving deep breathing and coughing information to patients in the surgical ward at a 95% confidence interval. The necessary sample size was estimated as 130 patients.
Data collection
A patient information form and a deep breathing exercise questionnaire were used for data collecting. The researcher visited patients in their rooms after their surgeries. Information was given with regard to the purpose and method of this study, and verbal permission was obtained from the patients who agreed voluntarily to participate. The patients were asked to answer these questions through face-to-face interviews, and this took approximately 20 min for each patient.
Patient information form
The researchers developed this form to perform information about the characteristics of the patients, including data about their age, gender, knowledge level, presence of chronic respiratory system diseases, length of hospitalization, and post-operative days.
Deep breathing exercise questionnaire
The researchers prepared this questionnaire with the guidance of literature research[17,18] to assess the status of receiving education about deep breathing exercises and the exercise performing statuses of patients. A total of five questions were created related to whether the patient had received any deep breathing exercise education, the source of education, the time of education (pre-operative or post-operative), the status of performing exercises, and the periods of exercises.
Ethical consideration
Ethical permission was approved for this study (2015/161-decision number 15/07), and permission to conduct the study was obtained from the directory of hospital. All patients were informed about this study, and their informed consent was obtained verbally.
Data analysis
The data were expressed as mean ± standard deviation and numbers (with percentages). Descriptive statistics, the Mann–Whitney U test, Spearman’s correlation, and Pearson’s Chi-squared test were used for data analyze. Non-parametric tests were used for the not normally distributed data, and P < 0.05 was considered significant. The SPSS 21.0 software package was used for coding and analyzing the data.
Results
Of the patients, 56.2% were female, 86.9% had no chronic respiratory system disease and the mean age was 54.1 ± 10.2 years. The average number of post-operative days was 6.43 ± 9.8 days, and there was no statistically significant difference between demographics and exercise performing status of patients (P > 0.05) [Table 1].
Table 1.
Characteristics of the patients and comparison with exercise performing status (n: 130)
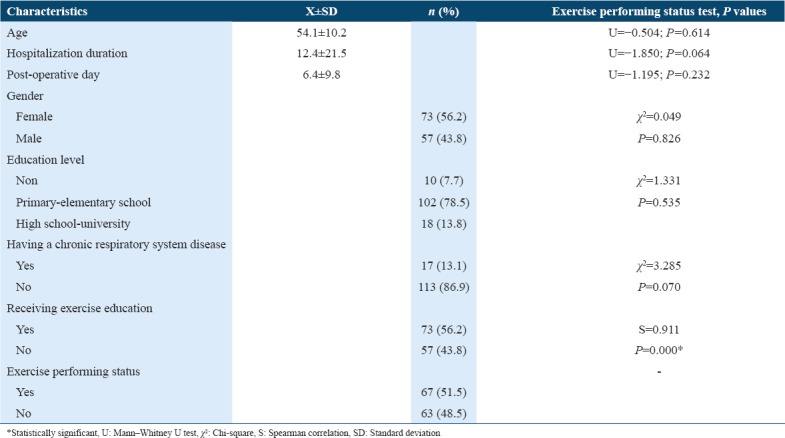
Seventy-three of the patients received education about deep breathing exercises, and 51.5% of them performed it. A strong correlation was found between the status of receiving education and exercise performing statuses of patients (P < 0.001)[Table 1].
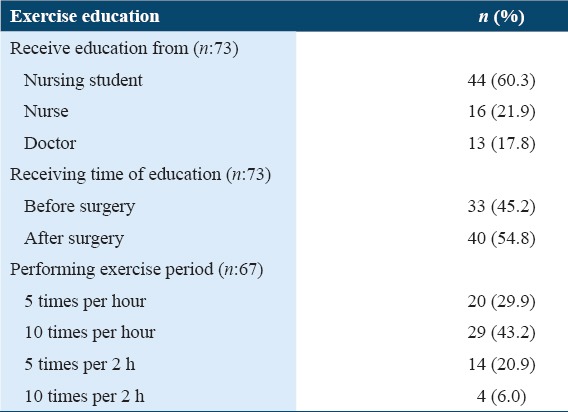
A total of 54.8% of the patients received deep breathing exercise education after surgery and 43.2% of them performed the exercises 10 times per hour [Table 2].
Table 2.
The features of exercise information given
Discussion
In patient education, defining the patient’s characteristics, especially education level and age, is important in light of the educating-learning process. Previous studies showed that old age affected the exercise practice of patients negatively.[19,20] In the present study, the characteristics did not affect the performing deep breathing exercise status of patients.
One of the most important findings of this study was that a strong positive correlation was found between receiving education and performing exercises. This means, receiving education effects patients’ exercise performing statuses positively. In a study,[21] one of the reasons of not performing regular exercises was found to be the lack of information, and the possibility of performing exercises was found to be 7.96 times greater among patients who received information about exercises than among those who did not. Sanaz et al.[22] also mentioned the importance of education and its positive impacts on behavioral improvement. Onat et al.[23] found that educating patients about the significance of exercises was important for the success of treatment. For the future, focusing on the positive effect of educating the patient, effects of organized clinical exercise protocols to be followed after surgeries may be studied.
Although the patient education is an important nursing intervention, a number of studies showed that surgical patients receive information mostly from doctors[1,16,24,25] and in the following from nurses.[26-28] In the present study, most of the patients received education about deep breathing exercises from nursing students. This result shows that nursing students adopt their roles and carry out their educating roles more effectively during their nursing education and training periods.
The findings of the present study highlighted that over half of the patients had received education about deep breathing exercises and most of them received this education after their surgeries. Educating patients improves their knowledge and sense of empowerment if it is given preoperatively.[29] A systematic review indicated that 61.3% of 31 studies reported that surgery patient education sessions were performed preoperatively and that 21.1% were conducted postoperatively.[30] Şahin et al.[17] reported that 53.6% of patients received information about deep breathing and coughing exercises before surgery, while Kutlu and Çetinkaya[16] cited that 9.3% of nurses educated patients about deep breathing and coughing exercises during the pre-operative period. In addition, Gürlek and Yavuz[1] reported that 38% of patients were taught such exercises preoperatively with Dolgun and Dönmez[26] citing 31.9%. Similarly, İzveren and Dal[11] determined that 25% of patients were educated about post-operative exercises during the early postoperational period. The results demonstrated that a deficiency exists in the education of patients undergoing surgery. Although the rate was not found to be much lower in this study, considering the potential complications after surgery, clinical nurses should pay more attention to educate patients preoperatively.
In this study, the exploration of deep breathing exercise education receiving, performing status of surgical patients was limited with one university hospital in Turkey. Thus, results cannot be generalized to other populations. Future research may include wider surgical units of university hospitals.
Conclusion
This study gained an insight into the status of the receiving deep breathing exercise education and performing statuses of surgical patients. The results indicated that the surgical patients did not receive adequate education about deep breathing exercises and most of them received this education after their surgeries. As a good finding, receiving education affected patients’ exercise performing statuses positively. It is advised from this study that clinical nurses should receive in-service education on the importance of pre-operative deep breathing exercise education to improve the exercise application rate among surgical patients.
Acknowledgments
The authors are grateful to all patients involved in the study.
References
- 1.Gürlek Ö, Yavuz M. Application cases of preoperative education of patients by nurses working in surgical clinicals. J Anatol Nurs Health Sci. 2013;16:8–15. [Google Scholar]
- 2.Lee DS, Lee SS. Pre-operative teaching:How does a group of nurses do it? Contemp Nurse. 2000;9:80–8. doi: 10.5172/conu.2000.9.1.80. [DOI] [PubMed] [Google Scholar]
- 3.Erdil F. Surgical nursing (perioperative nursing) In: Erdil F, Elbaş NO, editors. Surgical Nursing. 6th ed. Ankara: Aydoğdu Ofset; 2010. pp. 108–10. [Google Scholar]
- 4.Smetana GW. Preoperative pulmonary evaluation. Engl J Med. 1999;340:937–44. doi: 10.1056/NEJM199903253401207. [DOI] [PubMed] [Google Scholar]
- 5.Canet J, Gallart L, Gomar C, Paluzie G, Valles J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:1338–50. doi: 10.1097/ALN.0b013e3181fc6e0a. [DOI] [PubMed] [Google Scholar]
- 6.Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat MS, Rajesh PB, et al. Postoperative pulmonary complications following thoracic surgery:Are there any modifiable risk factors? Thorax. 2010;65:815–8. doi: 10.1136/thx.2009.123083. [DOI] [PubMed] [Google Scholar]
- 7.Mazo V, Sabaté S, Canet J, Gallart L, de Abreu MG, Belda J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219–31. doi: 10.1097/ALN.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy HL. Preoperative nursing management. In: Smeltzer SC, Bare BG, Hinkle JL, Cheever KH, editors. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. 12th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. pp. 425–41. [Google Scholar]
- 9.Westerdahl E, Lindmark B, Eriksson T, Hedenstierna G, Tenling A. The immediate effects of deep breathing exercises on atelectasis and oxygenation after cardiac surgery. Scand Cardiovasc J. 2003;37:363–7. doi: 10.1080/14017430310014984. [DOI] [PubMed] [Google Scholar]
- 10.Mathew J, D'silva F. A study on effectiveness of deep breathing exercise on pulmonary function among patients with chronic airflow limitation. Int J Nurs Educ. 2011;3:34–7. [Google Scholar]
- 11.İzveren AÖ, Dal Ü. The early period complications in patients who were performed abdominal surgery intervention and the nursing practices for these complications. Hacettepe Univ Fac Health Sci Nursing J. 2011;18:36–46. [Google Scholar]
- 12.Shuldham C. Pre-operative education-a review of the research design. Int J Nurs Stud. 1999;36:179–87. doi: 10.1016/s0020-7489(99)00011-5. [DOI] [PubMed] [Google Scholar]
- 13.O'Connor CJ. Pain relief and pulmonary morbidity after cardiac surgery. Crit Care Med. 1999;27:2314–6. doi: 10.1097/00003246-199910000-00055. [DOI] [PubMed] [Google Scholar]
- 14.Eber MR, Laxminarayan R, Perencevich EN, Malani A. Clinical and economic outcomes attributable to health care-associated sepsis and pneumonia. Arch Intern Med. 2010;170:347–53. doi: 10.1001/archinternmed.2009.509. [DOI] [PubMed] [Google Scholar]
- 15.McTier L, Botti M, Duke M. Patient participation in pulmonary interventions to reduce postoperative pulmonary complications following cardiac surgery. Aust Crit Care. 2016;29:35–40. doi: 10.1016/j.aucc.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Kutlu AK, Çetinkaya AÇ. Preoperative and postoperative interventions of nurses working in surgical units:Manisa sample. Hemşirelik Forum Derg. 2004;7:68–77. [Google Scholar]
- 17.Şahin A, Ayhan F, Öcal HS, Çayır A. An assessment of the preoperative information given to patients in the province of Karaman. J Hum Sci. 2015;12:1111–9. [Google Scholar]
- 18.Avşar G, Mağfiret K. Evaluation of patient education provided by clinical nurses in Turkey. Int J Nurs Pract. 2011;17:67–71. doi: 10.1111/j.1440-172X.2010.01908.x. [DOI] [PubMed] [Google Scholar]
- 19.Kattainen E, Merilainen P, Jokela V. CABG and PTCA patients'expectations of informational support in health related quality of life themes and adequacy of information in year follow-up. Eur J Cardiovasc Nurs. 2004;3:149–63. doi: 10.1016/j.ejcnurse.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Gentz GA. Perceived learning needs of the patient undergoing coronary angioplasty:An integrative review of the literature. Heart Lung. 2000;29:161–72. doi: 10.1067/mhl.2000.106002. [DOI] [PubMed] [Google Scholar]
- 21.Akça NK, Doğan A. Benefits of home-based exercising ability in patients with osteoarthritis. Turk J Phys Med Rehabil. 2012;58:288–93. [Google Scholar]
- 22.Sanaz S, Zahra MB, Saffari M. The impact of education on performing postpartum exercise based on health belief model. Med J Mashhad Univ Med Sci. 2014;57:776–84. [Google Scholar]
- 23.Onat ŞŞ, Delialioğlu SÜ, Uçar D. Exercises in the treatment of elderly patients with knee osteoarthritis:Factors affecting the efficiency of patient education. Turk J Geriatr. 2013;16:166–71. [Google Scholar]
- 24.Tok A, Çelik SŞ. Post-discharge problems experienced by the patients who undergone the coronary angioplasty and intra coronary stenting. Turk Klin J Nurs Sci. 2009;1:47–55. [Google Scholar]
- 25.Doğu Ö. Meeting the needs of education and training in patients with planned surgery preparation psychological effects of individual patient-Sakarya sample. J DU Health Sci Inst. 2013;3:10–3. [Google Scholar]
- 26.Dolgun E, Dönmez YC. Determination of patient's knowledge requirements belonging to preoperative period. J Nurs Sci Art. 2010;3:10–6. [Google Scholar]
- 27.Aygül S, Ulupınar S. Patient's opinions about nurse's role of patient education. J Anatol Nurs Health Sci. 2012;15:1–9. [Google Scholar]
- 28.Babacan E, Ulupınar S. Nurses'opinions and activities of patient education. J Educ Res Nurs. 2008;5:29–36. [Google Scholar]
- 29.Johansson K, Nutila L, +Virtanen H, Katajisto J, Salantera S. Preoperative education for orthopaedic patients:Systematic review. Adv Nurs. 2005;50:212–23. doi: 10.1111/j.1365-2648.2005.03381.x. [DOI] [PubMed] [Google Scholar]
- 30.Ronco M, Iona L, Fabbro C, Bulfone G, Palese A. Patient education outcomes in surgery:A systematic review from 2004 to 2010. Int J Evid Based Healthcare. 2012;10:309–23. doi: 10.1111/j.1744-1609.2012.00286.x. [DOI] [PubMed] [Google Scholar]


